Abstract
We present the first documented case of erythema multiforme following campylobacter gastroenteritis.
Keywords: Clinical, dermatology, gastroenterology, infectious diseases, microbiology, pathology
Case report
A 57-year-old gentleman presented to hospital with a widespread itchy, rash. He had a three-day history of watery diarrhoea up to six times a day, intermittent, crampy abdominal pain and fever. This illness developed a day after he had eaten crab cakes, which were out of date. On examination, he was dehydrated with dry mucous membranes. Abdomen was mostly tender in the umbilical and epigastric region but there were no signs of peritonism. The rash was well defined with circular target lesions on his upper and lower limbs. The remainder of physical examination was unremarkable. Vital observations on admission were as follows: temperature of 38.2℃, pulse rate of 110, blood pressure 102/68, respiratory rate of 22 and oxygen saturations of 96% on room air.
Initial blood tests revealed normal full blood count (Hb 147 gd/L, WBC 5.3 × 109/L, platelets 142 × 109/L), lipase (10 U/L) and electrolytes (sodium 136 mmol/L, potassium 3.8 mmol/L, magnesium 0.81 mmol/L, phosphate 1.07 mmol/L, adjusted calcium 2.22 mmol/L). However C-reactive protein was raised (83 mg/L), there was acute kidney injury (urea 13.4 mmol/L, creatinine 120 µmol/L, eGFR 34 mls/min/1.73 m2) and liver function tests showed a mixed hepatitic and cholestatic picture (Bilirubin 20 mmol/L, AST 64 U/L, ALT 111 U/L, ALP 155 U/L, GGT 103 U/L and albumin 25). Urinalysis and chest X-ray were unremarkable. He received IV fluids and empirical IV Piperacillin/Tazobactam for sepsis. Stool samples were sent as work up of acute diarrhoea and campylobacter species was isolated. The stool samples were negative for Giardia, Cryptosporidium, Salmonella, Shigella and E. coli. Clostridium difficile toxin was not found in any of the stool samples. Blood cultures were negative. IV antibiotics were stopped upon discussion with microbiology.
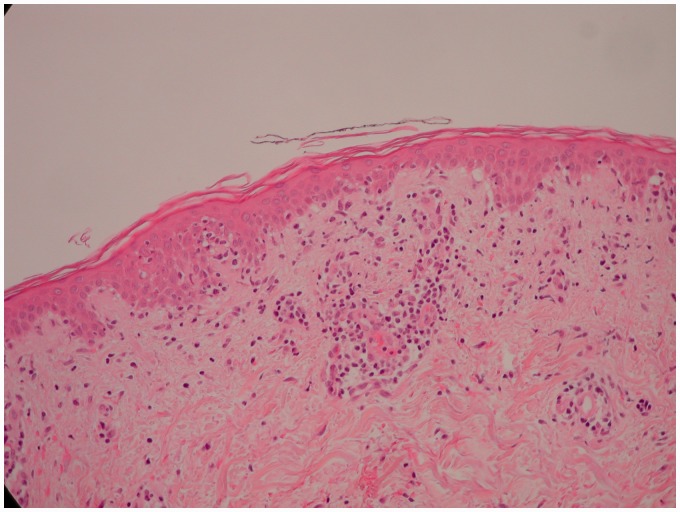
His diarrhoea, abdominal pain and fever resolved over the four days following admission. Renal function and liver function also improved. However, the rash had spread to his chest, neck, back and hands (Figure 1(a) and (b)). Dermatology opinion was sought and erythema multiforme major was diagnosed. Histology of a skin biopsy demonstrated a superficial perivascular chronic inflammatory infiltrate in the dermis with features of an interface dermatitis, i.e. basal vacuolation of the epidermis with lymphocytes involving the basal layer. This is consistent with erythema multiforme (Figure 2). He was treated with Chlorphenamine and topical emollient cream. Over the following five days, the rash slowly resolved.
Figure 1.
Florid erythematous lesions on patient's torso and limbs.
Figure 2.
Histology of skin biopsy.
Discussion
Campylobacter species are Gram negative, microaerophillic, motile bacilli. It colonises the intestinal tract in animals without causing illness and is typically transmitted via contaminated food and water. In humans, campylobacter species commonly cause a self-limiting enteritis lasting for a few days,1 usually without any complication. Post infection complications are rare with campylobacter. However, there are case reports of Guillain–Barré syndrome, acute pancreatitis, meningitis, haemolytic anaemia and septic arthritis associated with campylobacter infection.2 Acute hepatitis has also been associated with campylobacter infection, causing transaminases to rise over 50-fold.3 In our patient, liver function was only mildly deranged. We believe it was secondary to sepsis.
Cutaneous manifestations with campylobacter infection are very rare. So far, erythema nodosum4 and more recently, a case of sweet syndrome5 has been reported in literature.
Erythema multiforme is an acute, florid mucocutaneous condition characterised by skin, ocular and oral lesions. The unique ‘target-like’ skin rash is pathognomonic of this condition.6 Erythema multiforme is believed to be a sequela of infective and drug triggers. Case reports indicate that 70% of cases were precipitated by a preceding herpes simplex virus infection.7 Mycoplasma pneumonia and fungal infection are other commonly reported associations.8 Drugs most often associated with this condition are penicillins, nonsteroidal anti-inflammatory drugs, sulphonamides and barbiturates.9 However, our patient did not have any history of oro-genital herpes simplex, fungal infection and was not on any of the above medications.
Erythema multiforme is usually diagnosed clinically, but a skin biopsy may be of value. Biopsies show intraepithelial and intracellular oedema with eosinophilic necrotic keratinocytes. There may be lymphocytic infiltration in the subepithelial connective tissue and occasionally they aggregate into a dense mass around a vessel.10
The appearance of the skin rash in our case was pathognomonic of erythema multiforme and the skin biopsy histology was typical of this condition. To our knowledge, this is the first documented case of erythema multiforme associated with campylobacter infection. In conclusion, we would like to suggest that campylobacter infection should be considered as a possible cause in a patient with erythema multiforme following an acute diarrhoeal illness.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
Written informed consent for publication was obtained from the patient.
Guarantor
AM
Contributorship
All authors contributed equally to the planning of the manuscript, the review of the literature and the writing and editing of the original and final manuscript.
Provenance
Not commissioned; peer-reviewed by Anastasios Koulaouzidis and Kieran Fernando
References
- 1.Cover TL, Blaser MJ. The pathobiology of Campylo bacter infections in humans. Ann Rev Med 1989; 40: 269–285. [DOI] [PubMed] [Google Scholar]
- 2.Allos BM. Campylobacter jejuni infections: update on emerging issues and trends. Clin Infect Dis 2001; 32: 1201–1206. [DOI] [PubMed] [Google Scholar]
- 3.Korman TM, Varley CC, Spelman DW. Acute hepatitis associated with Campylobacter jejuni bacteremia. Eur J Clin Microbiol Infect Dis 1997; 16: 678–681. [DOI] [PubMed] [Google Scholar]
- 4.Ellis ME, Pope J, Mokashi A, et al. Campylobacter colitis associated with erythema nodosum. Br Med J (Clin Res Ed) 1982; 285: 937–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pai S, Rytina E, Sterling J, Karas JA, Aliyu SH. Campylobacter gastroenteritis associated with Sweet's syndrome. J Med Microbiol 2012; 61(Pt 10): 1473–5644. [DOI] [PubMed] [Google Scholar]
- 6.Huff JC, Weston WL, Tonnesen MG. Erythema multiforme: a critical review of characteristics, diagnostic criteria, and causes. J Am Acad Dermatol 1983; 8: 763–765. [DOI] [PubMed] [Google Scholar]
- 7.Sun Y, Chan RK, Tan SH, Ng PP. Detection and genotyping of human herpes simplex viruses in cutaneous lesions of erythema multiforme by nested PCR. J Med Virol 2003; 71: 423–428. [DOI] [PubMed] [Google Scholar]
- 8.Ayangco L, Rogers RS., III Oral manifestations of erythema multiforme. Dermatol Clin 2003; 21: 195–205. [DOI] [PubMed] [Google Scholar]
- 9.Volcheck GW. Clinical evaluation and management of drug hypersensitivity. Immunol Allergy Clin North Am 2004; 24: 357–371. [DOI] [PubMed] [Google Scholar]
- 10.Huang YF, Yang HW, Yang JH. Erythema multiforme – case report. J Dent Sci 2006; 1: 94–97. [Google Scholar]