Abstract
Objective
Occupational stress can have a harmful effect on the individual both physically and psychologically. In Korea, occupational stress of physician is rarely demonstrated. Although it is well reported that physicians tend to have a high incidence of minor psychiatric disorders, the magnitude of the problem remains unclear. Interns and residents are thought to be under substantial amount of stress, and tend to have psychiatric disorder. In this paper, we aimed to evaluate the relationship between the occupational stress and depression of residents.
Methods
The participants of this study were surgical and medical residents in a tertiary hospital in Korea. For measurement of occupational stress, we used an occupational stress scale. In addition, to evaluate the prevalence of depression, we used the Beck Depression Inventory.
Results
Female doctors showed higher degree of occupational stress than the males. The interns and chief residents showed higher degree of occupational stress than the other residents. Interestingly, in this study, most of the participants experienced a depressive mood. Compared with the general population, job demand and culture of workplace were high. Occupational stress was the only significant predictor of a depressive mood.
Conclusion
Hospital residents experience a high degree of occupational stress leading to a depressed mood due to various risk factors. Therefore, it is essential to recognize the occupational stress of residents early, to encourage positive competition and peer and social support, and to help improve the residents’ ability to cope with stress.
Keywords: Occupational stress, Internship and residency, Depression
INTRODUCTION
Occupational stress was defined by the National Institute for Occupational Safety and Health as the set of harmful physical and emotional responses that occur when the requirements of a worker’s job does not match his or her capabilities, resources, or needs [1]. Occupational stress has drawn academic attention since the 1960s, and French et al. [2] pointed out that it can have a negative effect on the worker such as influencing his or her physical, emotional, and psychological health. Furthermore, if the occupational stress exceeds the individual’s ability to cope with it, the individual tends to experience physical (ischemic cardiomyopathy, cardiac arrhythmia, thrombosis, or sudden death) and psychological (exhaustion, depression, or burn-out) harmful effects [1-3].
There are several theories on occupational stress. An earlier theory was presented as a cognitive stress model and embodied in the physiologic stress theory. Since then, however, integrated cognitive models of occupational stress, such as Karasek’s demandcontrol model, have been presented as alternative models that reflect the diversity of the modern society. As demonstrated in the study conducted by Karasek [4], physicians can be categorized as high-demand or high-control. When making decisions, physicians demonstrate highly active autonomy. In other words, when physicians are deprived of autonomy, their job itself can become a huge stressor for them.
Many hospitals at present are influenced by the characteristics of modern society, such as structuralization, specialization, and diversification. Moreover, the competition between hospitals and the needs of patients have greatly increased. Due to these and various other factors, including the changes observed in the organization of health services, occupational stress among physicians is growing, thereby increasing the prevalence of mental distress [5-7].
Although it is well documented that health service staff tends to have a high level of minor psychiatric disorders, the scale and nature of the problem remain unclear. In Korea, occupational stress of physicians is rarely demonstrated. In some studies on physicians’ occupational stress, the level of occupational stress was much higher in residents than in senior or oriental medical doctors [8-10].
Residency is a transitional phase of a physician’s career that forms the work habits of the future physician, and that can strongly influence self-care behaviors [11]. Medical interns and residents are very vulnerable to stress and tend to incur various psychiatric disorders. Their overwhelming workload and responsibilities combined with their lack of experience render residents more susceptible to occupational stress, depression, and burnout. Fahrenkopf et al. [12] reported that the depressed residents made six times more medical errors than the non-depressed residents. Thus, without proper recognition and intervention, the occupational stress of residents can become a huge problem not only in the medical field but also in the field of social health services [13].
In this study, the occupational stress of interns and residents and the relationship between the occupational stress and depression of physicians are investigated to reveal potential factors that contribute to stress in this particular population. To our knowledge, such a study has not been conducted in Korean residents. Recognizing stress and mental health problems in residents is crucial, as they can have serious effects on the quality of health care.
METHODS
Study population
The study participants were interns and residents with medical qualifications who were trained in a tertiary hospital in Seoul, Korea. Those who already had a psychiatric or physical disorder based on a DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) diagnosis that could be affected by further exposure to stress were excluded from the study. A total of 200 physicians, who were employed in the authors’ hospital in 2014, participated in this study; 42 were interns and 158 were residents.
Measurement tool
The Korean Occupational Stress Scale invented and validated in 2006 by the Korean Occupational Safety and Health Agency (KOSHA) was used to measure levels and sources of occupational stress. It is composed of 43 items categorized into 8 subscales: occupational environment (3 items), job demand (8 items), job autonomy (5 items), relationships (4 items), job instability (6 items), the organization system (7 items), improper rewards (6 items), and the culture of their workplace (4 items). The scale uses a 4-point Likert scale with higher scores indicating higher occupational stress. The degree of reliability of this scale as expressed by Cronbach’s α was 0.51 to 0.825.
To evaluate the prevalence of depression, the Korean version of the Beck Depression Inventory, validated by Lee [6] was used. It consists of 21 self administered items, each scored item categorized into 8 subscales.
Data collection and ethical approval
With the permission of the institutional review board of the authors’ hospital, data collection was performed between November and December 2014. Before data collection using the self-report questionnaires described above, the study’s purpose and the study subject anonymity, were explained to those who agreed to participate in the study by providing written informed consent.
Data analysis
Statistical analyses were conducted using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). The descriptive statistics present the study participants’ demographic characteristics. Demographic differences were analyzed with t-tests, chi-squares, or Pearson’s correlation. Multiple regression analyses were performed to examine the relationship between individual stress and depressive symptoms.
RESULTS
The baseline characteristics of the study participants are presented in Table 1. The total number of residents was 200, and 104 participants were included in this study. All the hospital interns (n=42) responded to the survey questionnaire, a fraction of the residents did so. The mean occupational stress scores are also presented in Table 1. According to KOSHA guidelines, the mean scores of occupational stress should be divided by sex. Our data confirmed that female doctors showed a higher degree of occupational stress than did male doctors. Interns and chief residents also showed a higher degree of occupational stress than did the other residents. Surprisingly, all participants reported a moderate depressive mood, and moreover, 84% of the residents had a severe depressive mood. None of participants reported a minimal, or mild depressive mood.
Table 1.
Baseline characteristics of participants (n=104)
| Characteristics | n (%) | Occupational stress | Moderate depression | Severe depression |
|---|---|---|---|---|
| Sex | ||||
| Male | 24 (23.1) | 43.26 ± 3.51 | 4 (3.9) | 20 (19.2) |
| Female | 80 (76.9) | 44.72 ± 3.80 | 13 (12.5) | 67 (64.4) |
| Age (yr) | ||||
| <30 | 57 (54.8) | 44.6 ± 3.98 | 14 (13.5) | 43 (41.4) |
| 30–9 | 47 (45.2) | 44.11 ± 3.52 | 3 (2.9) | 44 (42.3) |
| Grade | ||||
| Intern | 42 (40.4) | 45.04 ± 4.38 | 7 (6.7) | 35 (33.7) |
| R1 | 22 (21.2) | 43.43 ± 3.44 | 4 (3.9) | 18 (17.3) |
| R2 | 19 (18.3) | 42.92 ± 3.22 | 2 (1.9) | 17 (16.4) |
| R3 | 18 (17.3) | 44.64 ± 1.95 | 4 (3.9) | 14 (13.5) |
| R4 | 3 (2.9) | 49.75 ± 2.26 | 0 (0) | 3 (2.9) |
Values are presented as n (%) or mean±SD.
R1, 1st year residents; R2, 2nd year residents; R3, 3rd year residents; R4, chief residents.
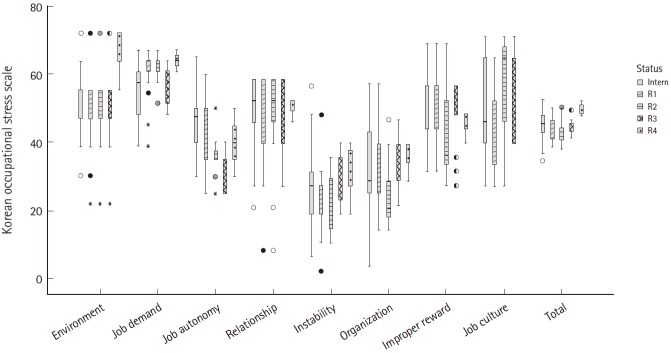
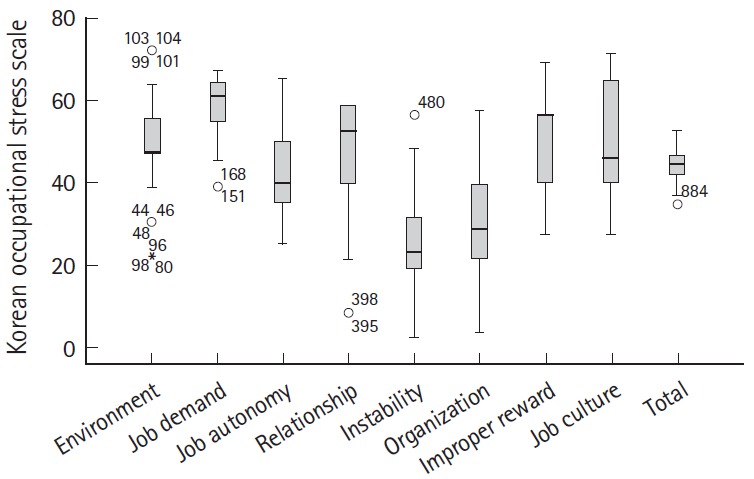
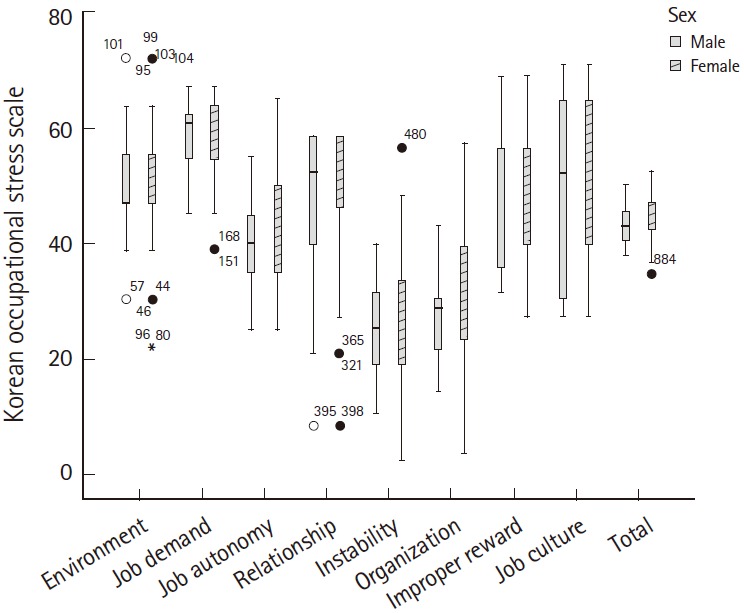
Fig. 1 shows the specific survey variables (occupational environment, job demand, job autonomy, relationship, job instability, organization system, inappropriate rewards, and job culture) and the total occupational stress scores. Job demand, job environment, and job culture showed relatively higher scores than did the other variables while job instability and organization system showed the lowest scores. The male and female physicians showed similar results for all the survey variables (Fig. 2). Job-demand- and job-autonomy-related stress showed a tendency to be higher among interns and second-year residents than third-year residents, and was the highest among the chief residents. Other variables, such as relationships, job organization, and inappropriate rewards, showed similar results. Job instability was shown to increase upon promotion to senior resident (Fig. 3). No significant difference was shown in any of the survey variables by age.
Fig. 1.
Comparison between specific topics of occupational stress in physicians (interns and residents). Dots and asterisks represent extreme abnormal values.
Fig. 2.
Comparison of specific aspects of occupational stress between male and female physicians. Dots and asterisks represent extreme abnormal values.
Fig. 3.
Comparison between specific topics of occupational stress and physicians’ grade. R1 stands for 1st year of residents, R2 for 2nd year, R3 for 3rd year, and R4 for chief residents. Dots and asterisks represent extreme abnormal values.
Depressive mood was further evaluated and compared with other factors, including sex, age, year level (interns and first year residents versus other year residents), and occupational stress using multiple logistic regression. Depressive mood was categorized by the Beck Depression Inventory score, as follows: scores below 16 were considered minimal or mild depressive mood and scores 16 or above 16 were considered moderate or severe depressive mood. As mentioned above, we used the mean scores based on the KOSHA stress scale and divided level of occupational stress into two groups, below and above the mean score. These evaluation results are presented in Table 2. Only occupational stress showed a statistically significant association with depression (P<0.05).
Table 2.
Multiple logistic regression of the relation between depressive mood and occupational stress, sex, age, and year level of interns and residents
| P-value | Odds ratio | 95% confidence interval |
||
|---|---|---|---|---|
| Lower | Upper | |||
| Sex | 0.83 | 0.87 | 0.23 | 3.27 |
| Age | 0.16 | 1.12 | 0.96 | 1.30 |
| Occupational stress | 0.04 | 1.34 | 1.01 | 1.79 |
| Grade | 0.27 | 0.73 | 0.42 | 1.28 |
Age was divided into two groups, under and over 30 years. Depressive mood was categorized by Beck Depression Inventory scores (scores below 16 were considered minimal or mild depressive mood, and scores 16 or above 16 were considered moderate or severe depressive mood).
DISCUSSION
Previous studies have confirmed that occupational stress proved to be higher in physicians than in the general population due to physicians’ excessive workload, decision-making responsibilities, on-call duty, financial problems, medical errors, medico-legal problems, and relationships with their patients [14-21], although it has been reported that the prevalence of mental health problems decreases among senior residents [22,23]. The excessive occupational stress of physicians can eventually adversely affect their patients’ safety and the quality of the medical service they provide [24].
Internship and residency are transitional periods during which medical students turn into physicians. They are considered tremendously stressful phases due to the presence therein of many stressors, such as shifting from being a medical student without clinical responsibilities to being a physician with numerous responsibilities. During their internship and residency, physicians are susceptible to various kinds of stress, which tend to facilitate the development of psychiatric problems such as depression and burnout. There are various factors that can lead to mental health problems such as occupational stress and depression among residents, such as job stressors, the dynamics in the medical education culture, the patients’ demands, the behaviors modeled by the clinical supervisors, sleep deprivation, and the residents’ personal characteristics [11].
Compared with the general population, the overall reported occupational stress of the hospital residents in this study, both male and female, was in the middle range. As expected, job environment and relationships were also in the middle range. Job demand and workplace culture were in the first upper quartile. This indicates that compared with the general population, physicians have a higher workload and are required to have greater patience to cope with the harsh workplace culture. On the contrary, some variables, including job autonomy, job instability, job organization, and inappropriate rewards, were in the lower quartile. This could be interpreted in a way that physicians, even interns and residents, are more capable of working with autonomy and within a concrete organization than are other workers.
This study demonstrated that the occupational stress of residents is not influenced by age and sex but by their year level. It was speculated that both job demand and job autonomy decline as the resident advances in year level, but it was shown that job demand and job autonomy increased until the second year of residency, declined during the third year of residency, and increased again during the chief resident year. This may be because chief residents already have full responsibility for their patients and junior residents, which can affect their job demand and job autonomy. On the other hand, job instability tends to increase among senior residents due to their anxiety about the future.
Under-recognition of how stress induces mental health problems and the low rate of treatment seeking may be the reasons for the high prevalence of psychiatric problems among young doctors. In one study, it was found that physicians tend to ignore their mental health problems, such as stress and burnout. In response to stress, physicians often neglect or avoid it, which leads to their maladaptation and their adoption of improper coping strategies, including substance abuse, unrecognized depression, and even suicide [25].
A study mentioned earlier, reported that the depressed residents made significantly more medical errors than did non-depressed residents [12]. In a previous study, it was revealed that stress could be reduced by consistent cognitive-, behavioral-, mindfulness-based interventions, which could significantly reduce the symptoms of anxiety in physicians [26]. In the present study, all the enrolled residents reported a depressive mood, and most of them reported that they suffered from a severe depressive mood. There are some studies about occupational stress and depressive symptoms [17], but none of them reported a similar finding, that is all residents having moderate or severe depressive mood. Various factors need to be considered to evaluate such a high prevalence of depressive mood. Surgical and medical functions and socioeconomic status as assessed by the self-administered questionnaire were not related to depression. Further investigation about the high incidence of depressive mood in residents is required. Furthermore, the current study found that their depressive mood was influenced by their occupational stress. This shows that without proper counseling and support, residents could be at risk of entering a “vicious cycle.” Thus, without proper recognition of and intervention for the occupational stress and depression of residents, this can become a severe problem not only in the medical field but also in the field of social health services [27].
There are some limitations to be discussed. This study was conducted in a single tertiary hospital that is affiliated with a medical school for women. Thus, our findings cannot be generalized to other hospitals. In a previous study, sex was found to be an important factor influencing depression and stress [28]. Thus, the results of the present study may have some biases. Second, there were few chief residents who responded to the questionnaire survey. As mentioned above, our study consisted of voluntary participants, and the residents could not be obliged to reply to the questionnaires; which resulted in a small number of study participants of certain year levels; this might have influenced the study results.
Third, residents showed an extremely high prevalence of depressive mood in this study. No participants reported having minimal or mild depressive mood. Further investigation about various factors such as sleep deprivation, work load, off-duty time, job culture, and others is required.
Fourth, the study was a single-center study in a tertiary hospital. There may be a need to conduct a multi-center study, and to exert efforts to develop a special screening and evaluation tool for the interns and residents in South Korea.
To summarize, hospital residents due to various risk factors, show a high prevalence of occupational stress, which leads to psychiatric problems. Occupational stress that exceeds the residents’ ability to cope can have physically and psychologically harmful effects on that resident, and can adversely affect patients and the quality of health care. Therefore, it is essential to recognize occupational stress among residents early, to encourage positive competition and social support, and to help improve the residents’ ability to cope with stress.
Capsule Summary
What is already known
Occupational stress can have a negative effect on the worker such as physical, emotional and psychological health. Although it is well reported that health service staff tend to have a high incidence of minor psychiatric disorders, there are only a few studies in Korea. Internship and residency are very vulnerable period of stress and other psychiatric disorders.
What is new in the current study
In this study, we describe occupational stress in interns and residents and the relationship between occupational stress and depression. According to this study, all enrolled residents had depressive mood and moreover, most of them reported that they had a severe depressive mood. Depressive mood was influenced by occupational stress. Therefore, it is essential to recognize occupational stress in residents early, and encourage positive competition, peer and social support, and help improve ability to cope with stress.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health . Occupational stress. Atlanta: Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 2.Saindon-Larose D, Rainville T. Work satisfaction of psychiatric nurses. Can Nurse. 1993;89:47–50. [PubMed] [Google Scholar]
- 3.Hwang CK, Koh SB, Chang SJ, et al. Occupational stress in relation to cerebrovascular and cardiovascular disease: longitudinal analysis from the NSDSOS project. Korean J Occup Environ Med. 2007;19:105–14. [Google Scholar]
- 4.Karasek RA. Healthy work: stress, productivity, and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 5.Sutherland VJ, Cooper CL. Job stress, satisfaction, and mental health among general practitioners before and after introduction of new contract. BMJ. 1992;304:1545–8. doi: 10.1136/bmj.304.6841.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SM. The effect of job characteristics and personal factors on work stress, job satisfaction and turnover intention. J Nurs Acad Soc. 1995;25:790–806. [Google Scholar]
- 7.Kim JK, Kim YJ, Seo KS, et al. Job stress, job satisfaction and occupational commitment among Korean emergency physicians. J Korean Soc Emerg Med. 2010;21:246–58. [Google Scholar]
- 8.Kang YS, Kam S, Lee SW, Chun BY, Yeh MH. Job stress and its related factors in south Korean doctors. Korean J Prev Med. 2001;34:141–8. [Google Scholar]
- 9.Kang MK, Kang YS, Kim JR, et al. The levels of psychosocial stress, job stress and related factors of medical doctors practicing at local clinics. J Prev Med Public Health. 2007;40:177–84. doi: 10.3961/jpmph.2007.40.2.177. [DOI] [PubMed] [Google Scholar]
- 10.Jin DG, Kam S, Kang YS, et al. Professional job perception, job stress and job satisfaction of doctors practicing in local clinic in Daegu city. Korean J Prev Med. 2003;36:153–62. [PubMed] [Google Scholar]
- 11.Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45:541–9. [PubMed] [Google Scholar]
- 12.Bowman MA. Stress and women physicians. New York: Springer-Verlag; 1985. [Google Scholar]
- 13.Tyssen R, Vaglum P. Mental health problems among young doctors: an updated review of prospective studies. Harv Rev Psychiatry. 2002;10:154–65. doi: 10.1080/10673220216218. [DOI] [PubMed] [Google Scholar]
- 14.Coombs RH. Mastering medicine: professional socialization in medical school. New York: Free Press; 1978. [Google Scholar]
- 15.McCue JD. The effects of stress on physicians and their medical practice. N Engl J Med. 1982;306:458–63. doi: 10.1056/NEJM198202253060805. [DOI] [PubMed] [Google Scholar]
- 16.Gerber LA. Married to their careers and family dilemmas in doctor’s lives. New York: Tavistock; 1983. [Google Scholar]
- 17.Kinnunen-Amoroso M, Liira J. Management of work related stress by Finnish occupational physicians. Occup Med (Lond) 2013;63:361–4. doi: 10.1093/occmed/kqt046. [DOI] [PubMed] [Google Scholar]
- 18.Hawk J. A case of family medicine: sources of stress in residents of health professionals. New York: Vruner/Mazel; 1986. [Google Scholar]
- 19.Mawardi BH. Satisfactions, dissatisfactions, and causes of stress in medical practice. JAMA. 1979;241:1483–6. [PubMed] [Google Scholar]
- 20.McCue JD. The distress of internship: causes and prevention. N Engl J Med. 1985;312:449–52. doi: 10.1056/NEJM198502143120725. [DOI] [PubMed] [Google Scholar]
- 21.Charles SC, Wilbert JR, Franke KJ. Sued and nonsued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry. 1985;142:437–40. doi: 10.1176/ajp.142.4.437. [DOI] [PubMed] [Google Scholar]
- 22.Hsu K, Marshall V. Prevalence of depression and distress in a large sample of Canadian residents, interns, and fellows. Am J Psychiatry. 1987;144:1561–6. doi: 10.1176/ajp.144.12.1561. [DOI] [PubMed] [Google Scholar]
- 23.Reuben DB. Depressive symptoms in medical house officers: effects of level of training and work rotation. Arch Intern Med. 1985;145:286–8. [PubMed] [Google Scholar]
- 24.Baldwin PJ, Dodd M, Wrate RM. Young doctors’ health: II. Health and health behaviour. Soc Sci Med. 1997;45:41–4. doi: 10.1016/s0277-9536(96)00307-3. [DOI] [PubMed] [Google Scholar]
- 25.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–21. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 26.Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014;202:353–9. doi: 10.1097/NMD.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 27.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–91. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hochberg MS, Berman RS, Kalet AL, Zabar SR, Gillespie C, Pachter HL. The stress of residency: recognizing the signs of depression and suicide in you and your fellow residents. Am J Surg. 2013;205:141–6. doi: 10.1016/j.amjsurg.2012.08.003. [DOI] [PubMed] [Google Scholar]