Abstract
According to the 36-Item Short Form Health Survey questionnaire developers, a global measure of health-related quality of life such as the “SF-36 Total/Global/Overall Score” cannot be generated from the questionnaire. However, studies keep on reporting such measure. This study aimed to evaluate the frequency and to describe some characteristics of articles reporting the SF-36 Total/Global/Overall Score in the scientific literature. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses method was adapted to a scoping review. We performed searches in PubMed, Web of Science, SCOPUS, BVS, and Cochrane Library databases for articles using such scores. We found 172 articles published between 1997 and 2015; 110 (64.0%) of them were published from 2010 onwards; 30.0% appeared in journals with Impact Factor 3.00 or greater. Overall, 129 (75.0%) out of the 172 studies did not specify the method for calculating the “SF-36 Total Score”; 13 studies did not specify their methods but referred to the SF-36 developers’ studies or others; and 30 articles used different strategies for calculating such score, the most frequent being arithmetic averaging of the eight SF-36 domains scores. We concluded that the “SF-36 Total/Global/Overall Score” has been increasingly reported in the scientific literature. Researchers should be aware of this procedure and of its possible impacts upon human health.
Keywords: Epidemiology/public health, bias (epidemiology), medical ethics, health status indicators, quality of life, questionnaires
Introduction
In the era of globalization, researchers play an important role in the “industrialization” of academy and “collegialization” of research. Academic organizations work with enterprises and industries to increase the commercialization of scientific research and methods. Access to knowledge no longer belongs to the public sphere but to the private one.1 Research tools that have been developed, validated, and patented by enterprises or by the academy must be used according to the specifications of their developers. The Medical Outcomes Trust, Health Assessment Lab, QualityMetric Incorporated, and Optum Incorporated, the organizations that hold all SF-36 copyrights and trademarks, have developed common policies for granting permissions for the use of SF-36 form. These organizations offer their licensing programs for both scholarly research and commercial applications that evaluate completeness of data, consistent responses and internal consistency, and assure the accuracy of data scoring and proper interpretation as well.2
The 36-Item Short Form Health Survey questionnaire (SF-36)3 is a very popular instrument for evaluating Health-Related Quality of Life. A PubMed search using the term “SF-36 health survey” found 9722 items.4
The SF-36 measures eight scales: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). Component analyses showed that there are two distinct concepts measured by the SF-36: a physical dimension, represented by the Physical Component Summary (PCS), and a mental dimension, represented by the Mental Component Summary (MCS). All scales do contribute in different proportions to the scoring of both PCS and MCS measures.3 The correct calculation of SF-36 summary measures PCS and MCS requires the use of special algorithms, which are strictly controlled by a private company.5
The SF-36 Scoring Manual3 doesn’t provide support to calculate a single measure of health-related quality of life, such as a “SF-36 Total/Global/Overall Score.” According to its developers, it is pointless trying to combine the two SF-36 summary measures to produce an overall score of health-related quality of life.6 Despite this, some researchers continue to use and to extrapolate erroneously from such measures.
This study evaluates the frequency and some characteristics of articles reporting single scores of health-related quality of life (the SF-36 Total/Global/Overall Score) in scientific literature.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method7 was adapted to this scoping review. While a systematic review may include few study designs, the scoping review allows the inclusion of several study designs.8 We included studies that have mentioned the use of a SF-36 Total/Global/Overall Score.
Search strategy
We conducted searches for articles and reviews in PubMed, Web of Science, SCOPUS, BVS, and Cochrane Library electronic databases, from 1990 to 2015, with any restrictions of language, date, and so on. The following queries were used for SF-36 Total Score: “sf-36 total score” OR “sf36 total score” OR “sf 36 total score”; and for SF-36 Global Score: “sf-36 global score” OR “sf36 global score” OR “sf 36 global score.” The PubMed search using the query “sf-36 overall score” OR “sf36 overall score” OR “sf 36 overall score” did not work well, probably because of the term “overall.” We then performed the search for SF-36 Overall Score using the following syntax: sf-36[All Fields] AND (“overall score”[All Fields] OR “overall scores”[All Fields] OR “overall scoring”[All Fields] OR “overall scoring system”[All Fields]).
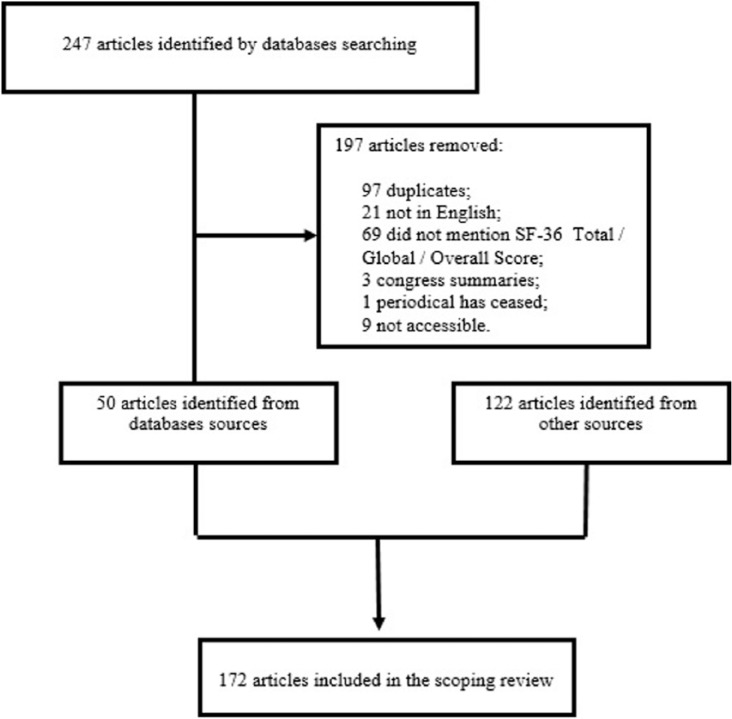
Two researchers analyzed the full-text of all the studies listed in the databases and selected them for deeper analysis. Subsequently, the studies were submitted to the inclusion and exclusion criteria (Figure 1).
Figure 1.
Flow chart: selection of papers in the scoping review.
Eligibility criteria
Articles in English language only: presence of the terms SF-36 total score, SF-36 global score, or SF-36 overall score in title, abstract, or full-text screening.
Data collection and classification, and study quality
Two independent researchers analyzed the relevant studies, classified the study design and identified the procedures for calculating SF-36 Total Score. We did not use any scoring method to assess the methodological quality of papers because our objective was just to demonstrate the misuse of a measure. Each study was classified according to the most recent evaluation of the Journal Citation Reports (JCR) Impact Factor of the periodical in which it was published and stratified as Impact Factor < 3.00 or with Impact Factor ⩾ 3.00.
Results
The PubMed search retrieved 131 studies (26 SF-36 Total Score, 41 SF-36 Global Score, and 64 SF-36 Overall Score); the Web of Science search retrieved 27 studies (23 SF-36 Total Score, 2 SF-36 Global Score, and 2 SF-36 Overall Score); the SCOPUS search retrieved 49 studies (42 SF-36 Total Score, 3 SF-36 Global Score, and 4 SF-36 Overall Score); the BVS search retrieved 29 studies (25 SF-36 Total Score, 2 SF-36 Global Score, and 2 SF-36 Overall Score); and the Cochrane Library search retrieved 11 studies (9 SF-36 Total Score, 1 SF-36 Global Score, and 1 SF-36 Overall Score).
Comparing the five databases searches, 247 articles which were considered potentially relevant were submitted to the inclusion and exclusion criteria. In total, 197 articles were excluded from our database because 97 were duplicates, 69 did not mention SF-36 Total/Global/Overall Score, 21 were not written in English (9 Chinese, 5 French, 2 Spanish, 1 German, 1 Portuguese, 1 Russian, 1 Japanese, and 1 Italian), 3 were not full-text articles but summaries presented in scientific events, and 10 articles could not be accessed: one because the publication of the respective periodical had ceased, and the other nine because access to the periodical was paid. By reviewing reference lists of the remaining 50 full-text articles, we obtained other 122 relevant citations. The final sample consisted of 172 articles, published between 1997 and 2015.
The study designs were cross-sectional (41), randomized clinical trial (35), non-randomized clinical trial (22), non-controlled clinical trial (9), diagnostic accuracy (25), cohort (19), case-control (4), systematic review (5), case series (11), and case report (1).
The studies came from 36 countries: the United States (25), Iran (15), Israel (13), the United Kingdom (12), Italy (11), Turkey (9), Canada (8), The Netherlands (7), Korea (6), China (6), Australia (5), Spain (5), France (5), Greece (5), Serbia (5), Sweden (4), Taiwan (3), Brazil (3), India (3), Switzerland (2), United Arab Emirates (2), Norway (2), Germany (2), Malaysia (2), Russia (1), Belgium (1), Mexico (1), Tunisia (1), Poland (1), Slovak Republic (1), Austria (1), Portugal (1), Jamaica (1), Saudi Arabia (1), Thailand (1), and Japan (1).
In total, 110 (64.0%) out of the 172 articles were published from 2010 onwards (Table 1).
Table 1.
Number of articles reporting SF-36 Total Score according to year of publication.
| Year | Articles (n) |
|---|---|
| 1997 | 2 |
| 1998 | 1 |
| 1999 | 1 |
| 2000 | 2 |
| 2001 | 5 |
| 2002 | 3 |
| 2003 | 8 |
| 2004 | 4 |
| 2005 | 7 |
| 2006 | 5 |
| 2007 | 4 |
| 2008 | 10 |
| 2009 | 10 |
| 2010 | 14 |
| 2011 | 22 |
| 2012 | 14 |
| 2013 | 18 |
| 2014 | 26 |
| 2015 | 16 |
| Total | 172 |
Fifty-one (30.0%) out of the 172 studies were published in journals with Impact Factor 3.00 or greater.
In total, 129 (75.0%) out of the 172 studies did not specify the method used for calculating the “SF-36 Total/Global/Overall Score.” Overall, 13 studies specified their methods, referring to articles published by the SF-36 developers at the beginning of the nineties or other authors. The remaining 30 articles were grouped into five different strategies for calculating the SF-36 Total Score, the most common being the arithmetic averaging of the eight SF-36 domains scores (Table 2).
Table 2.
Methods for calculating SF-36 Total/Global/Overall Score in 172 articles.
| Method for calculating SF-36 Total Score | n | Reference |
|---|---|---|
| Not specified | 129 | 9–137 |
| Not specified, but referred to studies by the SF-36 developers or others | 13 | 138,a 139,b 140,c 141,d 142,e,f 143,g 144,h 145,b 146,b 147,i 148,b 149,j 150k,l |
| Sum of the eight SF-36 domain scores | 7 | 151–157 |
| Sum of the two domains | 1 | 158 m |
| Sum of the eight SF-36 domains and the health transition item scores | 1 | 159 |
| “Sum of subcategories scores functional status, well being and overall health evaluation” | 1 | 160 |
| Arithmetic averaging | ||
| (a) The eight SF-36 domains | 16 | 161,n 162,o 163–176 |
| (b) The Physical and Mental Component Summaries | 3 | 177,e 178,p 179 |
| Adding a third second-order factor (well-being) to the eight SF-36 domains and to the Physical and Mental Component Summaries | 1 | 180 |
Cited Kosinski et al.181
Cited Ware and Sherbourne.182
Cited Ware.184
Cited Ware and Gandek.185
Cited Ware et al.186
Cited Kalantar-Zadeh et al.167
Cited Hays and Sherbourne.187
Cited Alonso et al.188
Cited Ware et al.189
Cited Brazier et al.190
Cited Brazier et al.191
Cited Zabel et al.192
Cited Brazier et al.193
Cited Bronfort and Bouter.159
Cited Ware et al.194
Some studies summed the scores of the eight SF-36 domains yielding Total Scores above 100, such as 524.4,151 482,152 and 110.4.153 Other studies still reported that the SF-36 Total Score “was found to have a high internal consistency,” as measured by Cronbach’s α = 0.91,20 α = 0.94,74 and α = 0.93.89
Discussion
The SF-36 developers state categorically,
The components analyses showed that there are two distinct concepts measured by the SF-36®—a physical dimension and a mental dimension. Therefore, it is not appropriate to try and come up with one overall score; thus instead the two summary scores are used.6
Analogously, the WHOQOL-BREF questionnaire does not recommend the calculation of a single index of quality of life. The instrument comprises a four domain structure: Physical health, Psychological, Social relationships, and Environment. Each particular domain is individually scored and interpreted. The calculation of a single/total/global/overall score of quality of life is not recommended (www.who.int/mental_health/media/en/76.pdf).
In the early nineties, it was questioned whether SF-36 scores could be used to generate a valid single index of health-related quality of life.193 The SF-6D provides a single index for use in economic evaluation or for determination of quality adjusted life years, derived from seven of the eight health domains of the SF-36. The GH domain is excluded; and the RP and the RE are combined in only one domain.190,191 The SF-6D is a single utility measure, widely validated in several studies,195 but it cannot be considered as a single index of health-related quality of life, strictly speaking.
Questionnaires addressing health-related quality of life can measure a single or multiple constructs and be classified as unidimensional or multidimensional, accordingly. This classification can be made after empirical demonstration, using adequate statistical techniques, such as confirmatory factor analysis or Rasch analysis. Once unidimensionality is proved, the items that compose the questionnaire can be added in order to yield a single/total score. Dealing with indexes derived from multidimensional questionnaires remains as a controversial issue. Some researchers argue that if the questionnaire is multidimensional, the items gathered into different scales must be scored and interpreted separately. This interpretation respects the questionnaire theoretical structure. However, other researchers feel no constraint in creating a total/global/overall score from a multidimensional questionnaire, using factor analysis or preference-based methods. Because this procedure doesn’t respect the different natures of the components dimensions, it can be criticized as an “adding apples and oranges” practice.
The exact balance between the physical and the mental components and their contributions to the health-related quality of life probably will remain unknown. Some studies177-179 we reviewed in this article have calculated a single index by averaging the physical and mental components. By doing so, they intrinsically assumed that the best (100%) measure of our health-related quality of life would result from a “perfect equilibrium” between the physical (50%) and the mental (50%) components.
Statistical strategies must be critically and parsimoniously used in the evaluation of health measures. Analyses of SF-36 dimensionality denote cross-loadings from the eight domains (https://campaign.optum.com/content/dam/optum/resources/Manual%20Excerpts/SF-36v2-Health-Survey-Measurement-Model.pdf) and also between the Physical and the Mental Component Summaries.185,197,198 These findings would suggest the existence of unidimensionality that would support the calculation of a single index of health-related quality of life. A review of the studies addressing SF-36 unidimensionality would be welcome.
A study74 calculated SF-36 Global Score even after a factor analysis has extracted two main dimensions (physical and mental).
In 2005, a study180 used structural equation model analysis to investigate the SF-36 structure in a population-based sample of adults older than 18 years living in Athens, Greece. The full model included the eight first-order factors (PF, RP, BP, GH, VT, SF, RE, and MH), three second-order factors (PCS, MCS, and “well-being,” based on GH and VT domain scores), and a third-order factor. This third-order factor would correspond to an SF-36 Overall Score, “indicating that all SF-36 responses address a single underlying phenomenon: health.” This study confirmed the multidimensional structure of the SF-36, but did not recommend the use of a SF-36 Overall Score. Instead, the authors recommended the use of the eight SF-36 domains together with the second-order factors (PCS, MCS, and “well-being”) for measuring health-related quality of life.
Presently, some instruments recommend the calculation of a single index of quality of life, such as the PedsQL (Pediatric Quality of Life Inventory (http://www.pedsql.org/score.html)), EuroQuol-5D (http://www.euroqol.org/), and the 15-D (http://www.15d-instrument.net/15d). Commenting on the adequacy of these instruments validation and interpretation of their total indexes is beyond the scope of this article.
SF-36 questionnaire aimed at two different constructs to measure health-related quality of life: the Physical Component and the Mental Component. In the end of the 1990s, after an exhaustive and sophisticated validation process, the SF-36 developers concluded that their questionnaire was adequate for measuring these two constructs of the health-related quality of life.185 However, they have never proposed but, in fact, they disapproved the use of SF-36 for building a single index of health-related quality of life. Subsequently, analyses of the SF-36 dimensionality conducted in general populations confirmed the extraction of these two main factors (Physical and Mental).74,196,199,200
Fairly high fees should be paid for each administered SF-36 questionnaire5 and applications of the scoring software.2,3 Researchers from low-income countries could have limited possibilities to pay for these fees. However, the great majority (72.4%) of 174 studies which we identified have come from high-income countries, classified according to the World Bank criteria: Gross National Income per capita of US$12,736 or more (http://data.worldbank.org/about/country-and-lending-groups#High_income).
This review has identified a high number of studies that have worked the “SF-36 Total/Global/Overall Score” out. These studies came from countries all over the world; 29.3% of them were published in high impact-factor journals and 63.8% were published in the last 6 years.
Calculating or not a SF-36 Total Score could be taken as a matter of different standpoints. However, we can argue against this position. Only a tiny proportion of the published papers uses the SF-36 Total Score. Applying our data to the 9722 papers found in a PubMed search using the query “SF36 health survey,” we have found that only 1.8% (172/9722) calculated SF-36 Total Score. Even considering that a certain proportion out of these 9722 papers were not interested in calculating a global measure of health-related quality of life, it is reasonable to assume that this different standpoint is not in the mainstream of the scientific community practice. Besides, papers reporting the SF-36 Total Score did not provide scientific arguments to support this measure.
This review has identified at least nine different ways of calculating this SF-36 Total Score (Table 2). It is difficult to conceive that all nine ways of calculation would provide the same (and valid) measure. If this different standpoint still applies, another question arises—which would be the correct way of calculating the SF-36 Total Score?
In our opinion, calculating a SF-36 Total/Global/Overall Score is a measurement bias (a systematic error) that can lead to a measure with poor validity, considering the latter as “the degree to which a health related-patient reported outcomes (HR-PRO) instrument measures the construct(s) it purports to measure.”201
If calculating a SF-36 Total/Global/Overall Score is an error, this might contribute to the building of a body of knowledge without the necessary scientific basis. The identification of any real implications of such error on decision making in clinical practice, developing guidelines, and on patients’ life lies beyond the scope of this study. However, researchers should be aware of this fact and of its possible impacts upon human health.
Study results based on a measure (SF-36 Total Score) with questionable validity may produce negative effects on individual and community health and waste public and private resources. It is difficult to evaluate the magnitude of the impact of the methodological errors in the studies we identified. In our scoping review, we identified five systematic reviews that aimed to consolidate knowledge produced about the quality of life of patients with critical conditions such as acute coronary syndrome,33 pain after spine surgery,164 in treatment for iron-deficiency anemia,43 osteoarthritis,100 and with movement disorders, undergoing deep brain stimulation.63 However, these five studies considered a SF-36 Total/Global Score, a measure that needs a more consistent scientific basis. Researchers, editors, and reviewers of scientific periodicals should take responsibility for the trustworthiness of their research and for the preservation of research integrity.
Strengths and limitations
This review was limited because the queries “SF-36 total score,” “SF-36 global score,” and “SF-36 overall score” are not indexed in all the databases we used. This can partially explain the scarcity of articles retrieved from these databases when compared to the number of articles obtained by consulting article references or by accessing the Internet. Another limitation is that our study was restricted to five databases. Despite these limitations, our review was able to identify a substantial number of studies dealing with the SF-36 Total/Global/Overall Score.
Conclusion
The SF-36 Total/Global/Overall Score, a global measure of health-related quality of life, has been increasingly reported in the scientific literature. Many studies using this measure were published in highly prestigious journals. However, its validity as a measure of total health-related quality of life can be questioned. Such total measure may contribute to build a biased body of knowledge.
Acknowledgments
We would like to thank Flávia Catarino Conceição Ferreira, librarian from the Reference Sector, Unified Health Library, Federal University of Bahia, for technical help in planning the scientific literature searches. We also thank Prof. Kionna Oliveira Bernardes Santos, from Federal University of Bahia, for useful criticisms to the final version of the manuscript.
Footnotes
Declaration of Conflicting Interests: The authors declare no financial or non-financial competing interests with organizations that hold copyrights and trademarks of questionnaires, particularly the SF-36. The findings of this study were not discussed with the SF-36 developers or with the SF-36 organization.
Ethical approval: Ethical approval was not sought for this study because it did not deal with human beings directly but with public data, already published.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:F.M.C. received a research fellowship from Brazilian National Research Council—CNPq (304563/2014-5).
Informed consent: Informed consent was not sought for this study because it did not deal with human beings directly.
References
- 1. Kleiman DL, Vallas SP. Science, capitalism, and the rise of the “knowledge worker”: the changing structure of knowledge production in the United States. Theor Soc 2001; 30: 451–492. [Google Scholar]
- 2. OPTUM. Scoring services, http://www.webcitation.org/6cfeMyJiW (accessed 30 October 2015).
- 3. Saris-Baglama RN, Dewey CJ, Chisholm GB, et al. QualityMetric health outcomes™ scoring software 4.0. Lincoln, RI: QualityMetric Incorporated, 2010, p. 138. [Google Scholar]
- 4. National Center for Biotechnology Information, U.S. National Library of Medicine, http://www.ncbi.nlm.nih.gov/pubmed (accessed 30 October 2015).
- 5. Optum. SF-36 health survey, http://www.webcitation.org/6cfdiZOJI (accessed 30 October 2015).
- 6. SF-36.org. FAQ: is there one summary score that is a combined score for the various subscales in the SF-36® so that a single score could be used for each patient? http://www.webcitation.org/6cfeefPkf (accessed 30 October 2015).
- 7. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 9. Asnani MR, Lipps GE, Reid ME. Utility of WHOQOL-BREF in measuring quality of life in Sickle Cell Disease. Health Qual Life Outcomes 2009; 7: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moura A, Madureira J, Alija P, et al. Predictors of health-related quality of life perceived by end-stage renal disease patients under online hemodiafiltration. Qual Life Res. Epub ahead of print 8 November 2014. DOI: 10.1007/s11136-014-0854-x. [DOI] [PubMed] [Google Scholar]
- 11. Pekmezovic T, Popovic A, Tepavcevic DK, et al. Factors associated with health-related quality of life among Belgrade University students. Qual Life Res 2011; 20: 391–397. [DOI] [PubMed] [Google Scholar]
- 12. Akashiba T, Kawahara S, Akahoshi T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 2002; 122: 861–865. [DOI] [PubMed] [Google Scholar]
- 13. Alishiri GH, Bayat N, Salimzadeh A, et al. Health-related quality of life and disease activity in rheumatoid arthritis. J Res Med Sci 2011; 16: 897–903. [PMC free article] [PubMed] [Google Scholar]
- 14. Ayoub AM, Hijjazi KH. Quality of life in dialysis patients from the United Arab Emirates. J Family Community Med 2013; 20: 106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beberashvili I, Sinuani I, Azar A, et al. Serum uric acid as a clinically useful nutritional marker and predictor of outcome in maintenance hemodialysis patients. Nutrition 2015; 31: 138–147. [DOI] [PubMed] [Google Scholar]
- 16. Birring SS, Prudon B, Carr AJ, et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 2003; 58: 339–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bouman EA, Theunissen M, Bons SA, et al. Reduced incidence of chronic postsurgical pain after epidural analgesia for abdominal surgery. Pain Pract 2014; 14: E76–E84. [DOI] [PubMed] [Google Scholar]
- 18. Buemi M, Caccamo C, Floccari C, et al. Correlation between quality of life assessment and a personality neurobiologic model in dialyzed patients. J Nephrol 2003; 16: 895–902. [PubMed] [Google Scholar]
- 19. Cabral DL, Laurentino GEC, Damascena CG, et al. Comparisons of the Nottingham Health Profile and the SF-36 health survey for the assessment of quality of life in individuals with chronic stroke. Rev Bras Fisioter 2012; 16: 301–308. [DOI] [PubMed] [Google Scholar]
- 20. Canetti L, Elizur Y, Karni Y, et al. Health-related quality of life changes and weight reduction after bariatric surgery vs. a weight-loss program. Isr J Psychiatry Relat Sci 2013; 50: 194–200. [PubMed] [Google Scholar]
- 21. Heller B, Tarricone R. Oxaprozin versus diclofenac in NSAID-refractory periarthritis pain of the shoulder. Curr Med Res Opin 2004; 20: 1279–1290. [DOI] [PubMed] [Google Scholar]
- 22. Keuthen NJ, Dougherty DD, Franklin ME, et al. Quality of life and functional impairment in individuals with trichotillomania. J Appl Res 2004; 4: 186–197. [Google Scholar]
- 23. Lee JS, Shin JK, Son SM, et al. Validation of the quality-of-life questionnaire of the European foundation for osteoporosis (QUALEFFO-26) in Korean population. Rheumatol Int 2014; 34: 919–927. [DOI] [PubMed] [Google Scholar]
- 24. Lee JS, Suh KT, Kim JI, et al. Validation of the Korean version of the neck pain and disability scale. Asian Spine J 2013; 7: 178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mamani M, Majzoobi MM, Ghahfarokhi SM, et al. Assessment of health-related quality of life among patients with tuberculosis in Hamadan, Western Iran. Oman Med J 2014; 29: 102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Monticone M, Baiardi P, Nido N, et al. Development of the Italian version of the neck pain and disability scale NPDS-I: cross-cultural adaptation, reliability, and validity. Spine 2008; 33: E429–E434. [DOI] [PubMed] [Google Scholar]
- 27. Noohi S, Karami GR, Lorgard-Dezfuli-Nejad M, et al. Are all domains of quality of life poor among elderly kidney recipients? Transplant Proc 2007; 39: 1079–1081. [DOI] [PubMed] [Google Scholar]
- 28. Peric S, Stojanovic VR, Basta I, et al. Influence of multisystemic affection on health-related quality of life in patients with myotonic dystrophy type 1. Clin Neurol Neurosurg 2013; 115: 270–275. [DOI] [PubMed] [Google Scholar]
- 29. Queen RM D, Sparling TL, Butler RJ, et al. Patient-reported outcomes function, and gait mechanics after fixed and mobile-bearing total ankle replacement. J Bone Joint Surg Am 2014; 96: 987–993. [DOI] [PubMed] [Google Scholar]
- 30. Rakhshani T, Shojaiezadeh D, Lankarani KB, et al. The association of health-promoting lifestyle with quality of life among the Iranian elderly. Iran Red Crescent Med J 2014; 16: e18404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rathod R, Baig MS, Khandelwal PN, et al. Results of a single blind, randomized, placebo-controlled clinical trial to study the effect of intravenous L-carnitine supplementation on health-related quality of life in Indian patients on maintenance hemodialysis. Indian J Med Sci 2006; 80: 143–153. [PubMed] [Google Scholar]
- 32. Sakkas GK, Karatzaferi C, Zintzaras E, et al. Liver fat, visceral adiposity, and sleep disturbances contribute to the development of insulin resistance and glucose intolerance in nondiabetic dialysis patients. Am J Physiol Regul Integr Comp Physiol 2008; 295: R1721–R1729. [DOI] [PubMed] [Google Scholar]
- 33. Silva SA, Passos SLR, Carballo MT, et al. Quality of life assessment after acute coronary syndrome: systematic review. Arq Bras Cardiol 2011; 97: 526–540. [DOI] [PubMed] [Google Scholar]
- 34. Tuchner M, Meiner Z, Parush S, et al. Relationships between sequelae of injury, participation, and quality of life in survivors of terrorist attacks. OTJR 2010; 30: 29–38. [Google Scholar]
- 35. Vukojevic Z, Pekmezovic T, Nikolic A, et al. Correlation of clinical and neurophysiological findings with health-related quality of life in patients with diabetic polyneuropathy. Vojnosanit Pregl 2014; 71: 833–838. [PubMed] [Google Scholar]
- 36. Wokhlu A, Monahan KH, Hodge DOI, et al. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J Am Coll Cardiol 2010; 55: 2308–2316. [DOI] [PubMed] [Google Scholar]
- 37. Rodrigues GH, Gebara OC, Gerbi CC, et al. Depression as a clinical determinant of dependence and low quality of life in elderly patients with cardiovascular disease. Arq Bras Cardiol 2014; 104: 443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Almeida OP, Lautenschlager NT, Vasikaran S, et al. A 20-week randomized controlled trial of estradiol replacement therapy for women aged 70 years and older: effect on mood, cognition and quality of life. Neurobiol Aging 2006; 27: 141–149. [DOI] [PubMed] [Google Scholar]
- 39. Andersen BL, Woods XA, Copeland LJ. Sexual self-schema and sexual morbidity among gynecologic cancer survivors. J Consult Clin Psychol 1997; 65: 221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Assari S, Lankarani MM, Khodabakhsh A. Comorbidity influences multiple aspects of well-being of patients with ischemic heart disease. Int Cardiovasc Res J 2013; 7: 118–123. [PMC free article] [PubMed] [Google Scholar]
- 41. Assari S, Soroush MR, Vishteh HRK, et al. Marital relationship and its associated factors in veterans exposed to high dose chemical warfare agents. J Fam Plann Reprod Health Care 2008; 2: 69–74. [Google Scholar]
- 42. Ayoub A, Nelson K, Wood P, et al. The relationship between laboratory values and quality of life of dialysis patients in the United Arab Emirates. Renal Soc Australas J 2014; 10: 12–20. [Google Scholar]
- 43. Bailie GR. Efficacy and safety of ferric carboxymaltose in correcting iron-deficiency anemia: a review of randomized controlled trials across different indications. Arzneimittelforschung 2010; 60: 386–398. [DOI] [PubMed] [Google Scholar]
- 44. Bakhtiari M, Falaknazi K, Lotfi M, et al. The relationship between Personality Traits, Anxiety and Depression, in Life Quality of patients under treatment by Hemodialysis (HD). Nov Biomed 2013; 1: 1–7. [Google Scholar]
- 45. Baldini M, Colasanti A, Orsatti A, et al. Neuropsychological functions and metabolic aspects in subclinical hypothyroidism: the effects of L-thyroxine. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 854–859. [DOI] [PubMed] [Google Scholar]
- 46. Barbat-Artigas S, Filion ME, Dupontgand S, et al. Effects of tai chi training in dynapenic and nondynapenic postmenopausal women. Menopause 2011; 18: 974–979. [DOI] [PubMed] [Google Scholar]
- 47. Bar-Ziv Y, Beer Y, Ran Y, et al. A treatment applying a biomechanical device to the feet of patients with knee osteoarthritis results in reduced pain and improved function: a prospective controlled study. BMC Muscoskel Disord 2010; 11: 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Baskov AV, Borshchenko IA, Shekhter AB, et al. Long term clinical results in laser reconstruction of spine discs. J Spine 2015; 4: 210. [Google Scholar]
- 49. Berner E, Qvigstad E, Myrvold AK, et al. Pain reduction after total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy among women with dysmenorrhoea: a randomised controlled trial. BJOG 2015; 122: 1102–1111. [DOI] [PubMed] [Google Scholar]
- 50. Bilgic A, Akman B, Sezer S, et al. Daytime sleepiness and quality of life in peritoneal dialysis patients. Ther Apher Dial 2011; 15: 565–571. [DOI] [PubMed] [Google Scholar]
- 51. Bross R, Zitterkoph J, Pithia J, et al. Association of serum total iron-binding capacity and its changes over time with nutritional and clinical outcomes in hemodialysis patients. Am J Nephrol 2009; 9: 571–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Calvet X, Gallardo O, Coronas R, et al. Remission on thiopurinic immunomodulators normalizes quality of life and psychological status in patients with Crohn’s disease. Inflamm Bowel Dis 2006; 12: 692–699. [DOI] [PubMed] [Google Scholar]
- 53. Cookson MS, Dutta SC, Chang SS, et al. Health related quality of life in patients treated with radical cystectomy and urinary diversion for urothelial carcinoma of the bladder: development and validation of a new disease specific questionnaire. J Urol 2003; 170: 1926–1930. [DOI] [PubMed] [Google Scholar]
- 54. Daenen L, Nijs J, Roussel N, et al. Sensorimotor incongruence exacerbates symptoms in patients with chronic whiplash associated disorders: an experimental study. Rheumatology 2012; 51: 1492–1499. [DOI] [PubMed] [Google Scholar]
- 55. Dalat F, Trouillet F, Fessy MH, et al. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: retrospective study of 54 cases. Orthop Traumatol Surg Res 2014; 100: 761–766. [DOI] [PubMed] [Google Scholar]
- 56. Davis AH, Figueredo AJ, Fahy BF, et al. Reliability and validity of the Exercise Self-Regulatory Efficacy Scale for individuals with chronic obstructive pulmonary disease. Heart Lung 2007; 36: 205–216. [DOI] [PubMed] [Google Scholar]
- 57. Deary IJ, Wilson JA, Carding PN, et al. The dysphonic voice heard by me, you and it: differential associations with personality and psychological distress. Clin Otolaryngol Allied Sci 2003; 28: 374–378. [DOI] [PubMed] [Google Scholar]
- 58. Debi R, Mor A, Segal G, et al. Correlation between single limb support phase and self-evaluation questionnaires in knee osteoarthritis populations. Disabil Rehabil 2011; 33: 1103–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Demirel R, Genc A, Ucok K, et al. Do patients with mild to moderate psoriasis really have a sedentary lifestyle? Int J Dermatol 2013; 52: 1129–1134. [DOI] [PubMed] [Google Scholar]
- 60. Desmarchelier R, Besse J-L, Fessy M-H, et al. Scarf osteotomy versus metatarsophalangeal arthrodesis in forefoot first ray disorders: comparison of functional outcomes. Orthop Traumatol Surg Res 2012; 98(6 suppl): 77S–84S. [DOI] [PubMed] [Google Scholar]
- 61. Di Donato N, Montanari G, Benfenati A, et al. The impact of socioeconomic and anamnestic characteristics on quality of life and sexual function in women with endometriosis. J Endometr Pelvic Pain Disord 2013; 5: 159–165. [Google Scholar]
- 62. Di Maio S, Akagami R. Prospective comparison of quality of life before and after observation, radiation, or surgery for vestibular schwannomas. J Neurosurg 2009; 111: 855–862. [DOI] [PubMed] [Google Scholar]
- 63. Diamond A, Jankovic J. The effect of deep brain stimulation on quality of life in movement disorders. J Neurol Neurosurg Psychiatry 2005; 76: 1188–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Doria A, Rinaldi S, Ermani M, et al. Health-related quality of life in Italian patients with systemic lupus erythematosus. II. Role of clinical, immunological and psychological determinants. Rheumatology 2004; 43: 1580–1586. [DOI] [PubMed] [Google Scholar]
- 65. Dowson AJ, Tepper SJ, Baos V, et al. Identifying patients who require a change in their current acute migraine treatment: the Migraine Assessment of Current Therapy (Migraine ACT) Questionnaire. Curr Med Res Opin 2004; 20: 1125–1135. [DOI] [PubMed] [Google Scholar]
- 66. Drapier S, Raoul S, Drapier D, et al. Only physical aspects of quality of life are significantly improved by bilateral subthalamic stimulation in Parkinson’s disease. J Neurol 2005; 252: 583–588. [DOI] [PubMed] [Google Scholar]
- 67. Drexler M, Segal G, Lahad A, et al. A non-invasive foot-worn biomechanical device for patients with hip osteoarthritis. Surg: Curr Res 2013; 3: 153. [Google Scholar]
- 68. Elbaz A, Mor A, Segal G, et al. APOS therapy improves clinical measurements and gait in patients with knee osteoarthritis. Clin Biomech 2010; 25: 920–925. [DOI] [PubMed] [Google Scholar]
- 69. El-Salhy M, Lillebø E, Reinemo A, et al. Effects of a health program comprising reassurance, diet management, probiotics administration and regular exercise on symptoms and quality of life in patients with irritable bowel syndrome. Gastroenterol Insights 2010; 2: 21–26. [Google Scholar]
- 70. Fabbri M, Superbo M, Defazio G, et al. Quality of life in patients with craniocervical dystonia: italian validation of the “Cervical Dystonia Impact Profile (CDIP-58)” and the “Craniocervical Dystonia Questionnaire (CDQ-24).” Neurol Sci 2014; 35: 1053–1058. [DOI] [PubMed] [Google Scholar]
- 71. George A, Wilson D, Abas A, et al. Safety and efficacy of a Labisia pumila var alata water extract on sexual well being and lipid profile of pre- and postmenopausal women: a randomized double-blind pilot study. Afr J Biotechnol 2014; 13: 768–777. [Google Scholar]
- 72. Gilron I, Bailey JM, Tu D, et al. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: a double-blind, randomised controlled crossover trial. Lancet 2009; 374: 1252–1261. [DOI] [PubMed] [Google Scholar]
- 73. Golish SR, Hanna LS, Bowser RP, et al. Outcome of lumbar epidural steroid injection is predicted by assay of a complex of fibronectin and aggrecan from epidural lavage. Spine 2011; 36: 1–6. [DOI] [PubMed] [Google Scholar]
- 74. Guermazi M, Allouch C, Yahia M, et al. Translation in Arabic, adaptation and validation of the SF-36 Health Survey for use in Tunisia. Ann Phys Rehabil Med 2012; 5: 388–403. [DOI] [PubMed] [Google Scholar]
- 75. Gupta R, Abosala A, Lovell M, et al. Does the ability of a patient to perform straight leg raise early postoperatively affect the outcome of total knee replacement? Internet J Orthop Surg 2008; 11: 1–7. [Google Scholar]
- 76. Halpern J, Cohen M, Kennedy G, et al. Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med 2014; 20: 37–46. [PubMed] [Google Scholar]
- 77. Harts CC, Helmhout PH, Bie RA, et al. A high-intensity lumbar extensor strengthening program is little better than a low-intensity program or a waiting list control group for chronic low back pain: a randomised clinical trial. Aust J Physiother 2008; 54: 23–31. [DOI] [PubMed] [Google Scholar]
- 78. Hassan IS, Bannister BA, Akbar A, et al. A study of the immunology of the chronic fatigue syndrome: correlation of immunologic parameters to health dysfunction. Clin Immunol Immunopathol 1998; 87: 60–67. [DOI] [PubMed] [Google Scholar]
- 79. Herman A, Chechik O, Segal G, et al. The correlation between radiographic knee OA and clinical symptoms: do we know everything? Clin Rheumatol 2015; 34: 1955–1960. [DOI] [PubMed] [Google Scholar]
- 80. Hwang H. Quality of life and surgical outcomes following laparoscopic surgery for refractory gastroesophageal reflux disease in a regional hospital. Can J Surg 2012; 55: 41–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Jarema M, Konieczynska Z. Quality of life in schizophrenia: impact of psychopathology, patient’s gender and antipsychotic treatment. Int J Psychiatry Clin Pract 2001; 5: 19–26. [DOI] [PubMed] [Google Scholar]
- 82. Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis 2010; 6: 361–366. [DOI] [PubMed] [Google Scholar]
- 83. Judson MA, Highland KB, Kwon S, et al. Ambrisentan for sarcoidosis associated pulmonary hypertension. Sarcoidosis Vasc Diffuse Lung Dis 2011; 28: 139–145. [PubMed] [Google Scholar]
- 84. Kerr JR, Petty R, Burke B, et al. Gene expression subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis. J Infect Dis 2008; 197: 1171–1184. [DOI] [PubMed] [Google Scholar]
- 85. Kerr JR, Burke B, Petty R, et al. Seven genomic subtypes of chronic fatigue syndrome/myalgic encephalomyelitis: a detailed analysis of gene networks and clinical phenotypes. J Clin Pathol 2008; 61: 730–739. [DOI] [PubMed] [Google Scholar]
- 86. Kerr JR. Gene profiling of patients with chronic fatigue syndrome/myalgic encephalomyelitis. Curr Rheumatol Rep 2008; 10: 482–491. [DOI] [PubMed] [Google Scholar]
- 87. Keynan O, Mirovsky Y, Dekel S, et al. Safety and efficacy of dietary agmatine sulfate in lumbar disc-associated radiculopathy. An open-label, dose-escalating study followed by a randomized, double-blind, placebo-controlled trial. Pain Med 2010; 11: 356–368. [DOI] [PubMed] [Google Scholar]
- 88. Koh MJ, Park SY, Park EJ, et al. The effect of education on decreasing the prevalence and severity of neck and shoulder pain: a longitudinal study in Korean male adolescents. Korean J Anesthesiol 2014; 67: 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Krokavcova M, Nagyova I, Rosenberger J, et al. Employment status and perceived health status in younger and older people with multiple sclerosis. Int J Rehabil Res 2012; 35: 40–47. [DOI] [PubMed] [Google Scholar]
- 90. Kwiatkowski F, Mouret-Reynier MA, Duclos M, et al. Long term improved quality of life by a 2-week group physical and educational intervention shortly after breast cancer chemotherapy completion. Results of the “Programme of Accompanying women after breast Cancer treatment completion in Thermal resorts” (PACThe) randomised clinical trial of 251 patients. Eur J Cancer 2013; 49: 1530–1538. [DOI] [PubMed] [Google Scholar]
- 91. Kwon JW, Moon JY, Kim SH, et al. Reliability and validity of a korean version of the leicester cough questionnaire. Allergy Asthma Immunol Res 2015; 7: 230–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Löhle M, Hughes D, Milligan A, et al. Clinical prodromes of neurodegeneration in Anderson-Fabry disease. Neurology 2015; 84: 1454–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Mabrouk M, Frascà C, Geraci E, et al. Combined oral contraceptive therapy in women with posterior deep infiltrating endometriosis. J Minim Invasive Gynecol 2011; 18: 470–474. [DOI] [PubMed] [Google Scholar]
- 94. Mabrouk M, Montanari G, Guerrini M, et al. Does laparoscopic management of deep infiltrating endometriosis improve quality of life? A prospective study. Health Qual Life Outcomes 2011; 9: e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Maisto SA, Conigliaro J, McNeil M, et al. An empirical investigation of the factor structure of the AUDIT. Psychol Assess 2000; 12: 346–353. [DOI] [PubMed] [Google Scholar]
- 96. Malekahmadi MR, Rahimzadeh S, Dezfuli Nejad ML, et al. Importance of socioeconomic, clinical, and psychological factors on health-related quality of life in adolescents after kidney transplant. Exp Clin Transplant 2011; 9: 50–55. [PubMed] [Google Scholar]
- 97. Maleki I, Taghvaei T, Barzin M, et al. Validation of the Persian version of the inflammatory bowel disease questionnaire (IBDQ) in ulcerative colitis patients. Caspian J Intern Med 2015; 6: 20–24. [PMC free article] [PubMed] [Google Scholar]
- 98. Manocha R, Black D, Wilson L. Quality of life and functional health status of long-term meditators. Evid Based Complement Alternat Med 2012; 2012: 350674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. MasoudRayyani LM, Forouzi MA, Razban F. Self-care self-efficacy and quality of life among patients receiving hemodialysis in South-East of Iran. Asian J Nur Edu Res 2014; 4: 165–171. [Google Scholar]
- 100. McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 2001; 45: 453–461. [DOI] [PubMed] [Google Scholar]
- 101. Meijer JM, Meiners PM, Vissink A, et al. Effectiveness of rituximab treatment in primary Sjögren’s syndrome: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2010; 62: 960–968. [DOI] [PubMed] [Google Scholar]
- 102. Min M-H, Choi Y-G, Kim Y-J, et al. The Effect of Sa-am acupuncture on Knee Osteoarthritis. J Meridian Acupoint 2009; 26: 53–66. [Google Scholar]
- 103. Mohammadi N, Kian S, Davoudi F, et al. Psychometric evaluation of the Persian version of the quality of life in epilepsy inventory-31. Iran J Neurol 2013; 12: 144–148. [PMC free article] [PubMed] [Google Scholar]
- 104. Mutlu B, Paker N, Bugdayci D, et al. Efficacy of supervised exercise combined with transcutaneous electrical nerve stimulation in women with fibromyalgia: a prospective controlled study. Rheumatol Int 2013; 33: 649–655. [DOI] [PubMed] [Google Scholar]
- 105. Neziri AY, Scaramozzino P, Andersen OK, et al. Reference values of mechanical and thermal pain tests in a pain-free population. Eur J Pain 2011; 15: 376–383. [DOI] [PubMed] [Google Scholar]
- 106. Ozturk O, Yalcin BM, Unal M. The quality of life difference between smoker and non smoker rheumatoid arthritis and ankylosing spondylitis patients. J Addiction Res Ther 2014; 5:1–6. [Google Scholar]
- 107. Paker N, Tekdös D, Kesitas N, et al. Comparison of the therapeutic efficacy of TENS versus intra-articular hyaluronic acid injection in patients with knee osteoarthritis: a prospective randomized study. Adv Ther 2006; 23: 342–353. [DOI] [PubMed] [Google Scholar]
- 108. Rambod M, Bross R, Zitterkoph J, et al. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am J Kidney Dis 2009; 53: 298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ren WH, Lai M, Chen Y, et al. Validation of the mainland Chinese version of the Inflammatory Bowel Disease Questionnaire (IBDQ) for ulcerative colitis and Crohn’s disease. Inflamm Bowel Dis 2007; 13: 903–907. [DOI] [PubMed] [Google Scholar]
- 110. Rousseau MC, Pietra S, Nadji M, et al. Evaluation of quality of life in complete locked-in syndrome patients. J Palliat Med 2013; 16: 1455–1458. [DOI] [PubMed] [Google Scholar]
- 111. Salaffi F, Leardini G, Canesi B, et al. Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthritis Cartilage 2003; 11: 551–560. [DOI] [PubMed] [Google Scholar]
- 112. Salaffi F, Carotti M, Grassi W. Health-related quality of life in patients with hip or knee osteoarthritis: comparison of generic and disease-specific instruments. Clin Rheumatol 2005; 24: 29–37. [DOI] [PubMed] [Google Scholar]
- 113. Sañudo B, Galiano D, Carrasco L, et al. Aerobic exercise versus combined exercise therapy in women with fibromyalgia syndrome: a randomized controlled trial. Arch Phys Med Rehabil 2010; 91: 1838–1843. [DOI] [PubMed] [Google Scholar]
- 114. Scuderi GJ, Cuellar JM, Cuellar VG, et al. Epidural interferon gamma-immunoreactivity: a biomarker for lumbar nerve root irritation. Spine 2009; 34: 2311–2317. [DOI] [PubMed] [Google Scholar]
- 115. Söderman P, Malchau H. Validity and reliability of Swedish WOMAC osteoarthritis index: a self-administered disease-specific questionnaire (WOMAC) versus generic instruments (SF-36 and NHP). Acta Orthop Scand 2000; 71: 39–46. [DOI] [PubMed] [Google Scholar]
- 116. Lahariya C, Khandekar J, Pradhan SK. Effect of impairment and disability on health-related quality of life of elderly: a community-based study from urban India. Indian J Community Med 2012; 37: 223–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Themistocleous GS, Goudelis G, Kyrou I, et al. Translation into Greek, cross-cultural adaptation and validation of the disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH). J Hand Ther 2006; 19: 350–357. [DOI] [PubMed] [Google Scholar]
- 118. Tsonga T, Kapetanakis S, Papadopoulos C, et al. Evaluation of improvement in quality of life and physical activity after total knee arthroplasty in greek elderly women. Open Orthop J 2011; 5: 343–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Tuchner M, Meiner Z, Parush S, et al. Health-related quality of life two years after injury due to terrorism. Isr J Psychiatry Relat Sci 2010; 47: 269–275. [PubMed] [Google Scholar]
- 120. Ünal H, Yildirim D, İrez BG. A study in terms of social marketing approach: the effects of physical activity on quality of life in elderly. J Phys Educ Sport Sci 2014; 8: 83–92. [Google Scholar]
- 121. Vandoninck V, Van Balken MR, Agró EF, et al. Posterior tibial nerve stimulation in the treatment of urge incontinence. Neurourol Urodyn 2003; 22: 17–23. [DOI] [PubMed] [Google Scholar]
- 122. Vercammen A, Morris R, Green MJ, et al. Reduced neural activity of the prefrontal cognitive control circuitry during response inhibition to negative words in people with schizophrenia. J Psychiatry Neurosci 2012; 37: 379–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Wallace DM, Shafazand S, Ramos AR, et al. Insomnia characteristics and clinical correlates in Operation Enduring Freedom/Operation Iraqi Freedom veterans with post-traumatic stress disorder and mild traumatic brain injury: an exploratory study. Sleep Med 2011; 12: 85085–85089. [DOI] [PubMed] [Google Scholar]
- 124. Waters F, Naik N, Rock D. Sleep, fatigue, and functional health in psychotic patients. Schizophr Res Treat 2013; 2013: 425826-1–425826-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Wu SY, Li HY, Tian J, et al. Health-related quality of life and its main related factors among nurses in China. Ind Health 2011; 49: 158–165. [DOI] [PubMed] [Google Scholar]
- 126. Xu J, Lin H, Feng X, et al. Different therapeutic approaches on quality of life in patients with inflammatory bowel disease. BMC Gastroenterol 2014; 14: 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Yalcinkaya H, Ucok K, Ulasli AM, et al. Do male and female patients with chronic neck pain really have different health-related physical fitness, depression, anxiety and quality of life parameters? Int J Rheum Dis. Epub ahead of print 9 May 2014. DOI: 10.1111/1756-185X.12389. [DOI] [PubMed] [Google Scholar]
- 128. Yekta Z, Pourali R, Ghasemi-Rad M. Comparison of demographic and clinical characteristics influencing health-related quality of life in patients with diabetic foot ulcers and those without foot ulcers. Diabetes Metab Syndr Obes 2011; 4: 393–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Lee SW, Chang C-S, Lien H-C, et al. Impact of overlapping functional gastrointestinal disorders on the presentation and quality of life of patients with erosive esophagitis and nonerosive reflux disease. Med Princ Pract 2015; 24: 491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Borg T, Hernefalk B, Carlsson M, et al. Development of a pelvic discomfort index to evaluate outcome following fixation for pelvic ring injury. J Orthop Surg 2015; 23: 146–149. [DOI] [PubMed] [Google Scholar]
- 131. Demircioglu DT, Paker N, Erbil E, et al. The effect of neuromuscular electrical stimulation on functional status and quality of life after knee arthroplasty: a randomized controlled study. J Phys Ther Sci 2015; 27: 2501–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Benda NMM, Seeger JPH, Stevens GGCF, et al. Effects of high-intensity interval training versus continuous training on physical fitness, cardiovascular function and quality of life in heart failure patients. PLoS ONE 2015; 10: e0141256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. De Rango P, Verzini F, Parlani G, et al. ; Comparison of surveillance vs. Aortic Endografting for Small Aneurysm Repair (CAESAR) Investigators. Quality of life in patients with small abdominal aortic aneurysm: the effect of early endovascular repair versus surveillance in the CAESAR trial. Eur J Vasc Endovasc Surg 2011; 41: 324–331. [DOI] [PubMed] [Google Scholar]
- 134. Link A, Treiber G, Peters B, et al. Impact of endoscopy-based research on quality of life in healthy volunteers. World J Gastroenterol 2010; 16: 467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Sheikh KA, El-setouhy M, Yagoub U, et al. Khat chewing and health related quality of life: cross-sectional study in Jazan region, Kingdom of Saudi Arabia. Health Qual Life Outcomes 2014; 12: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Pellegrini MJ, Schiff AP, Adams SB, Jr, et al. Conversion of tibiotalar arthrodesis to total ankle arthroplasty. J Bone Joint Surg Am 2015; 97: 2004–2013. [DOI] [PubMed] [Google Scholar]
- 137. Angthong C. Validity and reliability of Thai version of the Foot and Ankle Outcome Score in patients with arthritis of the foot and ankle. Foot Ankle Surg. Epub ahead of print 13 October 2015. DOI: 10.1016/j.fas.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 138. Debbi EM, Agar G, Fichman G, et al. Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee: a randomized controlled study. BMC Complement Altern Med 2011; 11: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Lioni L, Vlachos K, Letsas KP, et al. Differences in quality of life, anxiety and depression in patients with paroxysmal atrial fibrillation and common forms of atrioventricular reentry supraventricular tachycardias. Indian Pacing Electrophysiol J 2014; 14: 250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Qin Z, Zhang L, Sun F, et al. The Chinese Parkinson Study Group. Depressive symptoms impacting on health-related quality of life in early Parkinson’s disease: results from Chinese L-dopa exposed cohort. Clin Neurol Neurosurg 2009; 111: 733–737. [DOI] [PubMed] [Google Scholar]
- 141. Varma GR, Kusuma YS, Babu BV. Health-related quality of life of elderly living in the rural community and homes for the elderly in a district of India. Z Gerontol Geriatr 2010; 43: 259–263. [DOI] [PubMed] [Google Scholar]
- 142. Aslani J, Mirzamani SM, AzizAbadi-Farahani M, et al. Health-related quality of life in chronic obstructive pulmonary disease: are disease-specific and generic quality of life measures correlated? Tanaffos 2008; 7: 28–35. [Google Scholar]
- 143. Brandes M, Ringling M, Winter C, et al. Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res 2011; 63: 328–334. [DOI] [PubMed] [Google Scholar]
- 144. Garcia-Peña C, Wagner FA, Sánchez-Garcia S, et al. Depressive symptoms among older adults in Mexico City. J Gen Intern Med 2008; 23: 1973–1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Pinar R. A study on the reliability and validity of the Turkish version of the MQOLS-CA2 in people with cancer. Turk J Cancer 2002; 32: 148–163. [Google Scholar]
- 146. Polderman MCA, Huizinga TWJ, Le Cessie S, et al. UVA-1 cold light treatment of SLE: a double blind, placebo controlled crossover trial. Ann Rheum Dis 2001; 60: 112–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Sañudo B, Carrasco L, de Hoyo M, et al. Effects of exercise training and detraining in patients with fibromyalgia syndrome: a 3-yr longitudinal study. Am J Phys Med Rehabil 2012; 91: 561–569. [DOI] [PubMed] [Google Scholar]
- 148. Sañudo B, Hoyo M, Carrasco L, et al. The effect of a 6-week exercise programme and whole body vibration on strength and quality of life in women with fibromyalgia: a randomised study. Clin Exp Rheumatol 2010; 28: 40S–45S. [PubMed] [Google Scholar]
- 149. Berk C, Carr J, Sinden M, et al. Thalamic deep brain stimulation for the treatment of tremor due to multiple sclerosis: a prospective study of tremor and quality of life. J Neurosurg 2002; 97: 815–820. [DOI] [PubMed] [Google Scholar]
- 150. de Vries M, Ouwendijk R, Kessels AG, et al. Comparison of generic and disease-specific questionnaires for the assessment of quality of life in patients with peripheral arterial disease. J Vasc Surg 2005; 41: 261–268. [DOI] [PubMed] [Google Scholar]
- 151. Su C-T, Ng H-S, Yang A-L, et al. Psychometric evaluation of thr Short Form 36 Health Surveu (SF-36) and the World Health organization Quality of Life Scale Brief Version (WHOQOL-BREF) for patients with schizophrenia. Psychol Assess 2014; 26: 980–989. [DOI] [PubMed] [Google Scholar]
- 152. Cusano NE, Rubin MR, McMahon DJ, et al. PTH(1-84) is associated with improved quality of life in hypoparathyroidism through 5 years of therapy. J Clin Endocrinol Metab 2014; 99: 3694–3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Kulnigg S, Stoinov S, Simanenkov V, et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT) randomized controlled trial. Am J Gastroenterol 2008; 103: 1182–1192. [DOI] [PubMed] [Google Scholar]
- 154. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev 2005; 42: 535–546. [DOI] [PubMed] [Google Scholar]
- 155. Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet 2012; 380: 1583–1589. [DOI] [PubMed] [Google Scholar]
- 156. Wu GL, Li TY, Fan YS, et al. Therapeutic effect of Chinese herbal medicine for strengthening qi, nourishing yin, and removing stasis on serum osteopontin and quality of life of patients with primary Sjogren’s syndrome. Chin J Integr Med 2011; 17: 710–714. [DOI] [PubMed] [Google Scholar]
- 157. Yuhong H, Qian L, Yu L, et al. An n-of-1 trial service in clinical practice: testing the effectiveness of Liuwei Dihuang decoction for kidney-yin deficiency syndrome. Evid Based Complement Alternat Med 2013; 2013: 827915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Sahathevan S, Se CH, Ng SH, et al. Assessing protein energy wasting in a Malaysian haemodialysis population using self-reported appetite rating: a cross-sectional study. BMC Nephrol 2015; 16: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Bronfort G, Bouter LM. Responsiveness of general health status in chronic low back pain: a comparison of the COOP charts and the SF-36. Pain 1999; 83: 201–209. [DOI] [PubMed] [Google Scholar]
- 160. Kim W, Lim SK, Chung EJ, et al. The effect of cognitive behavior therapy-based psychotherapy applied in a forest environment on physiological changes and remission of major depressive disorder. Psychiatry Investig 2009; 6: 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Arefnasab Z, Ghanei M, Noorbala AA, et al. Effect of mindfulness based stress reduction on quality of life (SF-36) and spirometry parameters, in chemically pulmonary injured veterans. Iran J Public Health 2013; 42: 1026–1033. [PMC free article] [PubMed] [Google Scholar]
- 162. Jensen IB, Bergström G, Ljungquist T, et al. A 3-year follow-up of a multidisciplinary rehabilitation programme for back and neck pain. Pain 2005; 115: 273–283. [DOI] [PubMed] [Google Scholar]
- 163. Cheng SP, Lee JJ, Liu TP, et al. Parathyroidectomy improves symptomatology and quality of life in patients with secondary hyperparathyroidism. Surgery 2014; 155: 320–328. [DOI] [PubMed] [Google Scholar]
- 164. DeVine J, Norvell DC, Ecker E, et al. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery. Spine 2011; 36: 69S–74S. [DOI] [PubMed] [Google Scholar]
- 165. Fallahzadeh H, Mirzaei H. Health-related quality of life and associated factors among Iranian university students. J Community Health Res 2012; 1: 122–130. [Google Scholar]
- 166. He JQ, Chan-Yeung M, Carlsten C. Airway hyperresponsiveness and quality of life in Western red cedar asthmatics removed from exposure. PLoS ONE 2012; 7: e50774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Kalantar-Zadeh K, Kopple JD, Block G, et al. Association among SF36 quality of life measures and nutrition, hospitalization, and mortality in hemodialysis. J Am Soc Nephrol 2001; 12: 797–806. [DOI] [PubMed] [Google Scholar]
- 168. Latas M, Stojkovic T, Ralic T, et al. Medical students’ health-related quality of life—a comparative study. Vojnosanit Pregl 2014; 71: 751–756. [DOI] [PubMed] [Google Scholar]
- 169. Angst F, Goldhahn J, Pap G, et al. Cross-cultural adaptation, reliability and validity of the German Shoulder Pain and Disability Index (SPADI). Rheumatology 2007; 46: 87–92. [DOI] [PubMed] [Google Scholar]
- 170. Ariza-Ariza R, Hernández-Cruz B, Navarro-Sarabia F. Physical function and health-related quality of life of Spanish patients with ankylosing spondylitis. Arthritis Rheum 2003; 15: 483–487. [DOI] [PubMed] [Google Scholar]
- 171. Beaton DE, Hogg-Johnson S, Bombardier C. Evaluating changes in health status: reliability and responsiveness of five generic health status measures in workers with musculoskeletal disorders. J Clin Epidemiol 1997; 50: 79–93. [DOI] [PubMed] [Google Scholar]
- 172. Boccard SG, Pereira EA, Moir L, et al. Deep brain stimulation of the anterior cingulate cortex: targeting the affective component of chronic pain. Neuroreport 2014; 22: 83–88. [DOI] [PubMed] [Google Scholar]
- 173. Boi R, Racca L, Cavallero A, et al. Hearing loss and depressive symptoms in elderly patients. Geriatr Gerontol Int 2012; 12: 440–445. [DOI] [PubMed] [Google Scholar]
- 174. Tidermark J, Bergström G, Svensson O, et al. Responsiveness of the EuroQol (EQ 5-D) and the SF-36 in elderly patients with displaced femoral neck fractures. Qual Life Res 2003; 2: 1069–1079. [DOI] [PubMed] [Google Scholar]
- 175. Li R, Louie MK, Lee HJ, et al. Prospective randomized trial of three different methods of nephrostomy tract closure after percutaneous nephrolithotripsy. BJU Int 2011; 107: 1660–1665. [DOI] [PubMed] [Google Scholar]
- 176. Vetter TR, Bridgewater CL, McGwin G., Jr. An observational study of patients versus parental perceptions of health-related quality of life in children and adolescents with a chronic pain condition: who should the clinician believe? Health Qual Life Outcomes 2012; 10: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Barnett CT, Vanicek N, Polman RCJ. Temporal adaptations in generic and population-specific quality of life and falls efficacy in men with recent lower-limb amputations. J Rehabil Res Dev 2013; 50: 437–448. [DOI] [PubMed] [Google Scholar]
- 178. Pekmezovic T, Jecmenica-Lukic M, Petrovic I, et al. Quality of life in patients with progressive supranuclear palsy: one-year follow-up. J Neurol 2015; 262: 2042–2048. [DOI] [PubMed] [Google Scholar]
- 179. Md Yusop NB, Yoke Mun C, Shariff ZM, et al. Factors associated with quality of life among hemodialysis patients in Malaysia. PLoS ONE 2013; 8: e84152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Anagnostopoulos F, Niakas D, Pappa E. Construct validation of the Greek SF-36 Health Survey. Qual Life Res 2005; 14: 1959–1965. [DOI] [PubMed] [Google Scholar]
- 181. Kosinski M, Keller SD, Ware JE, et al. The SF-36 health survey as a generic outcome measure in clinical trials of patients with osteoarthritis and rheumatoid arthritis: relative validity of scales in relation to clinical measures of arthritis severity. Med Care 1999; 37: MS23–MS39. [DOI] [PubMed] [Google Scholar]
- 182. Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483. [PubMed] [Google Scholar]
- 183. McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993; 31: 247–263. [DOI] [PubMed] [Google Scholar]
- 184. Ware JE. Measuring patients’ views: the optimum outcome measure. BMJ 1993; 306: 1429–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Ware JE, Gandek B. Overview of the SF-36 health survey and the International Quality of Life Assessment (IQOLA) project. J Clin Epidemiol 1998; 51: 903–912. [DOI] [PubMed] [Google Scholar]
- 186. Ware JE, Kosinski M, Keller SK. Physical and mental health summary scales. A user’s manual. Boston, MA: The Health Institute, 1994. [Google Scholar]
- 187. Hays RD, Sherbourne CD. RAND 36-item health survey 1.0 scoring manual. Santa Monica, CA: The RAND Corporation, 1992. [Google Scholar]
- 188. Alonso J, Prieto L, Antó JM. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Med Clin 1995; 104: 771–776 (in Spanish). [PubMed] [Google Scholar]
- 189. Ware JE, Snow KK, Kosinski M. SF-36 health survey manual and interpretation guide. Boston, MA: New England Medical Center, The Health Institute, 1997. [Google Scholar]
- 190. Brazier J, Usherwood T, Harper R, et al. Deriving a preference-based single index from the UK SF-36 Health Survey. J Clin Epidemiol 1998; 51: 1115–1128. [DOI] [PubMed] [Google Scholar]
- 191. Brazier JE, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002; 21: 271–292. [DOI] [PubMed] [Google Scholar]
- 192. Zabel R, Ash S, King N, et al. Relationships between appetite and quality of life in hemodialysis patients. Appetite 2012; 59: 194–199. [DOI] [PubMed] [Google Scholar]
- 193. Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992; 305: 160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Ware JE, Snow KK, Kosinski M. The SF-36 health survey manual and interpretation guide. Boston, MA: Nimrod Press, 1993. [Google Scholar]
- 195. Strand V, Crawford B, Singh J, et al. Use of “spydergrams” to present and interpret SF-36 health-related quality of life data across rheumatic diseases. Ann Rheum Dis 2009; 68: 1800–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Li L, Wang W, Shen Y. Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health 2003; 57: 259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Taft C, Karlsson J, Sullivan M. Do SF-36 summary component scores accurately summarize subscale scores? Qual Life Res 2001; 10: 395–404. [DOI] [PubMed] [Google Scholar]
- 198. Farivar SS, Cunningham WE, Hays RD. Correlated physical and mental health summary scores for the SF-36 and SF-12 Health Survey, V.I. Health Qual Life Outcomes 2007; 5: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Anagnostopoulos F, Niakas D, Tountas Y. Comparison between exploratory factor-analytic and SEM-based approaches to constructing SF-36 summary scores. Qual Life Res 2009; 18: 53–63. [DOI] [PubMed] [Google Scholar]
- 200. Grassi M, Nucera A; European Community Respiratory Health Study Quality of Life Working Group. Dimensionality and summary measures of the SF-36 v1.6: comparison of scale- and item-based approach across ECRHS II adults population. Value Health 2010; 13: 469–478. [DOI] [PubMed] [Google Scholar]
- 201. Porta M. (ed.) A dictionary of epidemiology. 6th ed. Oxford: Oxford University Press, 2014, pp. 180–181. [Google Scholar]