Abstract
Background:
Fingertip injury requiring flap cover is very common in the modern era. The ideal cover should fulfill both functional and aesthetic improvement.
Materials and Methods:
From June 2015 to April 2016, we performed seven free toe pulp flaps for finger defect reconstruction. All patients were males. Five flaps were done in emergency post-traumatic cases, and two were done in elective set up. The cases included reconstruction of three thumbs, one index and one ring finger in an emergency set up and two ring fingers in the elective. Thumb reconstruction was done with great toe lateral pulp and the other digits reconstructed with second toe pulp flap. Follow-up evaluation included both functional and aesthetic assessment.
Results:
Five flaps survived completely, one suffered partial loss, and one flap failed completely. The median follow-up period was 9 months. The median duration of surgery was 255 min (range 210 to 300 min). The median two-point discrimination was 6.5 mm (range 4–8 mm). There was the return of temperature sensation in all patients; two had cold intolerance. The Semmes-Weinstein monofilament score varied from 3.61 to 5.07 (median filament index value 4.31/pressure value of 2 g/mm2). Three patients had delayed donor site wound healing.
Conclusions:
The free toe pulp flap is an efficient choice for fingertip and volar finger defects reconstruction with an excellent tissue match.
KEY WORDS: Finger defect, free toe pulp flap, pulp defect, reconstruction, volar defect
INTRODUCTION
The functional and the aesthetic importance of the hand in day to day life is unquestionable. Reconstruction of finger defects requires improvement of functional outcome with an acceptable aesthesis. The options of reconstruction vary with the requirement and the size of the defect. The options extend from simple grafting, local flaps[1] to complex microsurgical procedures. The ideal reconstruction is one which gives the best aesthetic as well as the functional outcome. The toe pulp is considered to be the most suitable for finger pulp and volar defect reconstruction due to its tissue match.[2] The improvement in microsurgical techniques nowadays makes this option very viable for the finger reconstruction. The advantages of the free pulp transfer are the tissue match and the sensory recovery when compared to the other local options. The simultaneous harvesting of the bone, joint or tendon along with the skin paddle is feasible with the toe pulp flap.[3] Some of the local options such as cross finger flap[4] and the thenar flap[5] mandate to keep the fingers immobilised, resulting in stiffness, especially in elderly patients.
MATERIALS AND METHODS
From June 2015 to April 2016, we performed free toe pulp flaps in seven patients. We included patients with finger defects with exposed bone, tendon or joints which require flap cover for the management. The patients who were willing for the surgery after discussing about the pros and cons and financial details were included in the study. The written informed consent was taken before the procedure. All the patients were operated by a single surgeon. Five patients were operated on an emergency basis, of which, two sustained injury by finger getting in motorcycle chain and the rest by machine crush in the workplace. The other two toe pulp flaps were carried out in an elective set up for the correction of finger deformity. Three had involvement of the thumb; one patient had involvement of the index finger and three had involvement of the ring finger. The size of the flaps was measured at the time of surgery. The donor site was closed with skin graft taken from the instep of the sole in all the patients. The sensation was assessed by Semmes-Weinstein monofilament test and the two point discrimination test. The sensitivity to cold was assessed by the Cold Intolerance Symptom Severity Questionnaire. The aesthesis of the finger was assessed with the visual analogue scale. The donor site healing was also assessed during the study. All the post-operative evaluation was done by an independent observer.
Surgical method
All the surgeries were performed by a single surgeon including recipient dissection, flap elevation to the anastomosis. Pre-operative handheld Doppler assessment of both the donor and the recipient sites were done, and the arteries marked. The veins were marked over the dorsum of the digit with keeping a venous tourniquet before the surgery [Figure 1]. The procedures were done under regional anaesthesia, axillary and the wrist block for the recipient site and ankle block for the flap elevation. The tourniquet was applied before the surgery with moderate exsanguination for the visualisation of the veins. Intravenous sedation was administered in all the patients. All the surgeries were done under microscope magnification of ×20. The finger defect was made into a template, and the flap was planned in reverse.
Figure 1.

The flap marking- with artery marked red colour and dorsal vein in blue
While elevating the flap the initial dissection was done proximal to the flap to identify the subcutaneous vein and the connection of the vein to the flap was kept intact. The incision was extended into the web space or the dorsum of the foot for harvesting adequate length of vessels. Following which the flap was elevated from the dorsal incision, then to the distal most part of the flap. The incision was deepened to the extensor tendon layer not injuring it and started elevating from distal to proximal fashion by cutting the septa. At most care was given to keep the incision little away from the nail matrix to prevent deformity of the nail. While elevating, the digital artery and the digital nerve were identified, and the elevation continued proximally. The flap was left to perfuse for at least 5 min before dividing the flap. The recipient vessels were the digital artery and the volar vein of the injured digit, and they were dissected by putting a zigzag incision extending from the defect proximally. After division of the flap, the anastomosis was done in end to end fashion in both the artery and the vein. For the initial two cases of thumb reconstruction, the flaps were planned according to the defect from the lateral great toe pulp and the artery was dissected to the dorsalis pedis artery. The recipient vessel was the radial artery in the anatomical snuff box. The venous anastomosis was done to the dorsal hand veins in both the cases. For anastomosis, we used 10–0, 11–0 nylon sutures according to the size of the vessels (the size of dorsals pedis artery and vein were 2–3 mm, which matched with radial artery and the dorsal vein in the anatomical snuff box. The size of the digital artery was 1–1.5 mm and the dorsal veins were 0.5–1 mm in all the other cases; both donor as well as the recipient). The digital nerve was harvested along with the vessels, and they were co-opted with the digital nerve of the injured digit. In one patient, there was a bone defect for which a small piece of vascularised bone was harvested from the middle phalanx along with the second toe pulp flap. The flaps were monitored by clinical assessment of the colour, turgor, temperature and the capillary refill time. Adequate hydration of the patients was done using intravenous fluid administration for 5 days post-surgery. The donor defects were closed with full thickness/partial thickness skin graft harvested from the instep of the same foot. One patient had a little bulky flap which was thinned 2 months after the initial surgery.
RESULTS
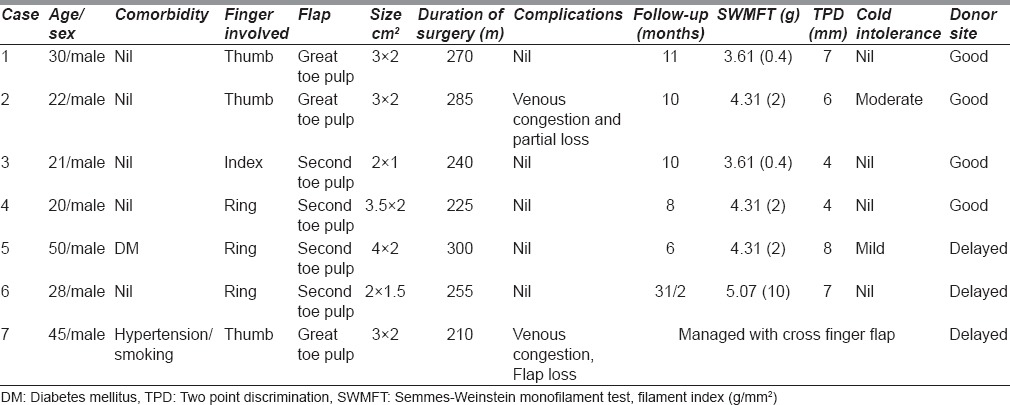
A total of seven patients underwent free toe pulp flap [Table 1] of which one flap completely failed. The flap size ranged from 2 cm × 1 cm to 4 cm × 2 cm in dimensions. The median duration of surgery was 255 min (range 210 min to 300 min). The vessel size of dorsalis pedis artery and vena comitantes was 2–3 mm. The digital artery size was 1–1.5 mm and the dorsal/volar vein 0.5–1 mm. The median age of the patients was 28 years (range 18–45 years). The maximum follow-up period was 11 months and the minimum 3½ months (median follow-up 9 months). The Semmes-Weinstein Sensitivity score varied from 3.61 to 5.07 (median filament index value 4.31/pressure value of 2 g/mm2), and the median static two-point discrimination was 6.5 mm (range 4–8 mm). There was mild cold intolerance in one patient and moderate cold intolerance in another one. The flap which failed was the great toe lateral pulp flap for the thumb. The flap looked well perfused over a period of 48 h after that it developed venous congestion and re-exploration could not save the flap. The defect was closed with a cross finger flap. The patient was a chronic smoker in that case. One flap developed post-operative venous congestion which was salvaged by re-exploration, but suffered a partial flap loss. There was delayed wound healing in the donor site in three patients. None of the patients had any proximal joint stiffness due to the flap dissection.
Table 1.
Factors evaluated and results
Case 1
A 31-year-old man presented with an occupational injury to the right thumb with pulp loss [Figure 2a]. The defect was reconstructed with right great toe lateral pulp free flap [Figure 2b and c]. The vessels were traced to the dorsalis pedis artery and the dorsal veins of the foot [Figure 2c]. Radial artery and dorsal hand veins are taken as the recipient vessels on the hand [Figure 2d]. Post-operative results showed a well-settled flap with good sensation and aesthesis [Figure 2e].
Figure 2.

(a) Right thumb pulp loss. (b) Flap design on the lateral aspect right great toe with proximal extension. (c) Flap after division showing the vascular pedicle. (d) Anastomosis with radial artery and the dorsal vein in the recipient site. (e) Well settled flap after 8 months
Case 2
A 21-year-old young adult presented with right index finger pulp defect [Figure 3a]. The injury occurred while cleaning the motorcycle. The defect was covered with second toe pulp free flap [Figure 3b and c]. While giving inset, the area of pedicle was covered with a thin split-thickness graft [Figure 3d]. The final outcome was good after a single stage of proximal flap thinning [Figure 3e and f].
Figure 3.
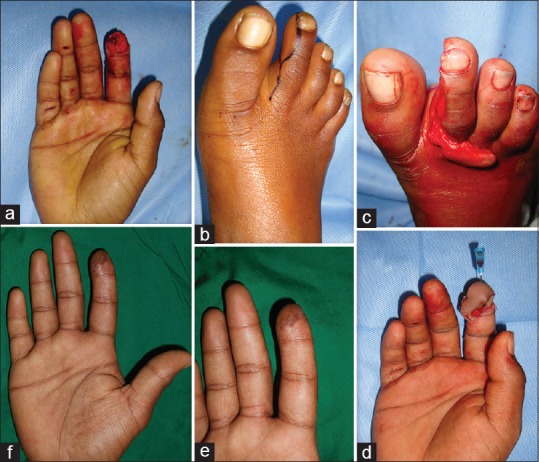
(a) Right index finger pulp defect. (b) Second toe pulp flap marking on right side. (c) Harvesting of the flap. (d) Flap inset showing proximal pedicle covered with a thin split thickness graft. (e and f) Final result after 7 months
Case 3
A 20-year-old young adult sustained an injury to the index, middle, ring and little finger in the form of crush amputation [Figure 4a and 4b]. The amputated parts were replanted, and the middle and ring finger survived completely [Figure 4c]. There was marked arterial insufficiency of the ring finger after a follow-up period of 1 year [Figure 4d]. The second toe pulp flap was done to get more bulk and aesthesis of the digit [Figure 4e–h]. Post-operative result was very good [Figure 4i].
Figure 4.

(a) Crush amputation right index through little finger. (b) Amputated parts showing avulsion elements. (c) The digits after replantation. (d) Arterial insufficiency marked on ring finger. (e and f) Second toe pulp flap markings. (g) Elevated flap. (h) The flap after inset, proximal part covered with a small split thickness graft. (i) 5 months post-operative result showing improved aesthesis
Case 4
A 50-year-old diabetic with an injury to right index, middle, ring and little finger sustained while working in industry. There was bone loss in the distal phalanx of the index finger, volar defect without exposing the tendon or bone of the middle finger and the ring finger had a volar defect with exposed tendon [Figure 5a]. The middle finger was covered with full thickness graft, index finger and little finger primarily closed and the ring finger was managed with second toe pulp flap [Figure 5b–e] and donor site closed with full thickness graft [Figure 5f]. There were no flap-related complication and the flap settled well over time [Figure 5g].
Figure 5.

(a) Injury to right index, middle, ring and little finger. Ring finger had exposed tendon, little and index finger had crushed tip and middle finger with superficial volar tissue loss. (b and c) Second toe flap markings. (d) Elevated flap. (e) Toe pulp flap used to cover the ring finger, full thickness graft for the middle finger and primary closure of the little and index finger. (f) Donor site closed with full thickness graft. (g) 4 months post-operative results showing well settled flap
Case 5
A 28-year-old male presented with deformed left ring finger with malunion at the level of the distal interphalangeal (DIP) joint [Figure 6a]. The deformity was corrected with releasing incision on the ulnar aspect resulting in a composite tissue defect including bone [Figure 6b]. The second toe pulp flap was harvested along with a small piece of bone from the middle phalanx of the second toe [Figure 6c–e]. The flap was transferred to the recipient defect and anastomosed to the digital artery and the volar vein [Figure 6f and g]. After the bone was united, the K-wire was removed, and the flap settled well. There was a little excess of the flap which may require trimming later on [Figure 6h]. The donor site healed well, even though there was early wound dehiscence [Figure 6i].
Figure 6.

(a) Post-traumatic malunited left ring finger with ulnar deviation. (b) Defect over the medial and the volar ring finger post-release. (c) Second toe pulp flap marking. (d and e) Flap harvesting showing a small piece of bone taken as composite flap from the middle phalanx. (f and g) Flap inset immediate post-operative. (h) Well settled flap 1½ months post-surgery. (i) Well healed donor site
The donor site settled well in all the cases except for the hypertrophic scar in the dorsum of foot in the initial two cases. The avoidance of proximal dissection gave better aesthesis in all the other cases [Figure 7].
Figure 7.

(a) Donor big toe after 10 months post-operatively, showing well settled big toe scar with hypertrophic scar on the dorsum. (b and c) Well settled donor in case of second toe pulp flap after 7 months post-operatively with negligible scar. Since the dissection stopped at the web space there is no donor scar in the dorsum foot. (d) Well settled great toe 11 months post-operative with ugly scar on the dorsum foot due to proximal dissection. (e and f) Very good donor site, 6 months post-operatively in case of second toe pulp flap
DISCUSSION
Fingertip injuries with exposed bone, tendon or neurovascular bundle is frequently encountered in the plastic surgery emergency department. The ideal cover is one which gives the best aesthesis along with best functional outcome. Re-plantation of the amputated thumb was successfully done by Komatsu and Tamai in 1968.[6] Following which the dimension of the digital reconstruction was changed drastically. The use of toes for reconstruction of the fingers was next in the queue, followed by the toe pulp for the fingertip injuries. The progress of microsurgery and evolution of super microsurgery plays a critical role in the improved outcome of hand injuries.
The options for reconstruction vary from local flaps to free tissue transfer in finger pulp and volar defects. The local flaps usually performed for the digital reconstruction are cross finger flap, thenar flap, first dorsal metacarpal artery (FDMA) flap, reverse dorsal metacarpal artery flap and reverse homodigital island flap. The main disadvantages of these flaps are the inferior sensory recovery and the scar over the nearby visible donor area. The use of neurotization in FDMA[7] and cross finger flap[8] improves the sensory recovery, but the donor scar and colour texture match are still poor. Digital artery perforator flap is another option which gives tissue match with donor site scar which is still poor.[9] With the revolutionary changes in microsurgery, the reconstruction is nearing the ideal. The options are free great toe pulp flap, second toe pulp flap, medial plantar artery perforator flap[10] and freestyle perforator flap depending on the defect size.
Morrison et al., in early 80's had done extensive work on the use of wrap-around flap and partial toe flap for the thumb and finger reconstruction. They proposed that the use of toenail along with nail matrix could be used for reconstruction of both finger and thumbnail.[11,12,13,14,15]
One of the large series of toe pulp transfer is from Korea by Lee et al.[16] Over a period of 7 years they performed 929 partial second toe pulp flaps in 854 patients, of which 57 patients had two finger defect and 9 had three finger defects. The overall survival in this series was 99.7% and 59% cases had donor site morbidity in the form of wound hematoma or wound separation. They could achieve a mean static two-point discrimination of 8 mm. They harvested flaps with shorter pedicle and saved the duration of surgery. In this study, in the initial two cases, we took a longer pedicle till the dorsalis pedis artery for extra pedicle length and the rest of the cases we took the flap with the digital artery and the dorsal vein in the web space. Keeping a long pedicle causes extra time for dissection and chance of compression of the pedicle in the case of tunneling. One of our patients had venous congestion post-surgery with resulting partial flap loss which was tackled with a small full thickness graft harvested from the instep. Zheng et al.[17] in their experience has faced flap loss in a chronic smoker and cautions over doing pulp transfer in chronic smokers, diabetes mellitus patients and individuals with peripheral vascular disease. They analysed great toe lateral pulp free flap for finger pulp reconstruction and came out with conclusion promoting the use of the same in finger reconstruction. We experienced a complete flap loss in a patient after 2 days of surgery who was a chronic smoker. He developed venous congestion, in spite of flap re-exploration, frequent puncturing and letting out blood eventually the flap failed. The raw area was tackled with cross finger flap from the index finger. Yoon and Lee[18] in a series of patients tried free toe pulp transfer for fingertip reconstruction without venous anastomosis and came out with good results. In the study group, post-surgery venous decompression was done with needle puncture method, every 2 hourly in the first 24 h and every 4 h thereafter. The blood loss calculated was around 0.2 ml for each needle puncture. The long-term follow-up showed no flap atrophy or any other untoward outcomes.
Koshima et al., in their study evaluated 133 toe transfers done over a period of 17 years.[19] Out of which 56 cases were done for fingertip reconstruction requiring bone, soft tissue, nail in different proportions. They evaluated the sensation and functional recovery of the fingers and came out with the positive result of the superior quality of the toe pulp flap with or without nail and bone or nail alone as a free tissue transfer.
Cho et al., in their institution-based study evaluated the use of the second toe pulp free flap for the volar finger defects.[20] They used the flaps to cover the defects over the interphalangeal joint with or without harvesting the digital nerve according to the requirements. The histological tissue match along with the option of harvesting the digital nerve makes this procedure superior to other local options. There is no need for prolonged immobilisation of the fingers like in case of the thenar or cross finger flap. One of our patients had deformed ring finger, angulation to the ulnar side due to destroyed DIP joint and deformed distal phalanx. The deformity was corrected by putting releasing incision on the ulnar side of the digit, which extended from the volar to dorsum and there was a bony deficit on the ulnar aspect. We harvested second toe pulp flap with a vascularised bone piece and digital nerve along with the flap, and reconstruction of the defect was done. Arthrodesis of the DIP joint was done. The digital nerve was neurotized to the side of the ulnar side digital nerve. There was bony stabilisation and sensory recovery without cold intolerance in this patient.
The functional outcome post toe pulp transfer was studied in detail by Lin et al., by analysing the sensory recovery, pinch strength and subjective pain and discomfort evaluation.[21] They noticed that the sensory recovery in terms of sensory threshold was equal to the donor toes, and the pinch strength was comparable to the uninvolved hand. Cold intolerance and hyperaesthesia were noted in subjective evaluation especially in those with recent fingertip reconstruction. In our series, the longest follow-up was 11 months and shortest follow-up was 3½ months. The patient with the longest follow-up had good recovery in terms of sensation as well as tolerance to cold. The short follow-up patient also regained two-point discrimination of 7 mm and good sensory recovery without much cold intolerance.
CONCLUSIONS
The free toe pulp flap is an efficient choice for fingertip and volar finger defects reconstruction with excellent tissue match.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Papatheodorou LK, Dailiana ZH, Varitimidi SE, Hantes ME, Basdekis GK, Malizos KN. Digital coverage with flaps from the same or neighboring digits. Hippokratia. 2011;15:153–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Yan H, Ouyang Y, Chi Z, Gao W, Zhang F, Fan C. Digital pulp reconstruction with free neurovascular toe flaps. Aesthetic Plast Surg. 2012;36:1186–93. doi: 10.1007/s00266-012-9949-3. [DOI] [PubMed] [Google Scholar]
- 3.Wang ZT, Sun WH. Cosmetic reconstruction of the digits in the hand by composite tissue grafting. Clin Plast Surg. 2014;41:407–27. doi: 10.1016/j.cps.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Woon CY, Lee JY, Teoh LC. Resurfacing hemipulp losses of the thumb: The cross finger flap revisited: Indications, technical refinements, outcomes and long term neurosensory recovery. Ann Plast Surg. 2008;61:385–91. doi: 10.1097/SAP.0b013e3181640873. [DOI] [PubMed] [Google Scholar]
- 5.Flatt AE. The thenar flap. J Bone Joint Surg Br. 1957;39B:80–5. doi: 10.1302/0301-620X.39B1.80. [DOI] [PubMed] [Google Scholar]
- 6.Komatsu S, Tamai S. Successful replantation of a completely cut off thumb. Plast Reconstr Surg. 1968;42:374–7. [Google Scholar]
- 7.Wang H, Chen C, Li J, Yang X, Zhang H, Wang Z. Modified first dorsal metacarpal Island flap for sensory reconstruction of thumb pulp defects. J Hand Surg Eur. 2016;41:177–84. doi: 10.1177/1753193415610529. [DOI] [PubMed] [Google Scholar]
- 8.Lee NH, Pae WS, Roh SG, Oh KJ, Bae CS, Yang KM. Innervated cross-finger pulp flap for reconstruction of the fingertip. Arch Plast Surg. 2012;39:637–42. doi: 10.5999/aps.2012.39.6.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koshima I, Urushibara K, Fukuda N, Ohkochi M, Nagase T, Gonda K, et al. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg. 2006;118:1579–84. doi: 10.1097/01.prs.0000232987.54881.a7. [DOI] [PubMed] [Google Scholar]
- 10.Yoon ES, Kim DW, Chun D, Dhong ES, Koo SH, Park SH, et al. An anatomic study and clinical application of medial pedis flap in Asians. Ann Plast Surg. 2007;58:517–22. doi: 10.1097/01.sap.0000244929.93375.34. [DOI] [PubMed] [Google Scholar]
- 11.Morrison WA, O’Brien BM, MacLeod AM. Thumb reconstruction with a free neurovascular wrap-around flap from the big toe. J Hand Surg Am. 1980;5:575–83. doi: 10.1016/s0363-5023(80)80110-9. [DOI] [PubMed] [Google Scholar]
- 12.Morrison WA, O’Brien B. Surgical opportunism in emergency hand surgery. World J Surg. 1991;15:439–45. doi: 10.1007/BF01675638. [DOI] [PubMed] [Google Scholar]
- 13.Morrison WA. Microvascular nail transfer. Hand Clin. 1990;6:69–76. [PubMed] [Google Scholar]
- 14.Morrison WA, O’Brien BM, MacLeod AM. Experience with thumb reconstruction. J Hand Surg Br. 1984;9:223–33. doi: 10.1016/0266-7681(84)90030-5. [DOI] [PubMed] [Google Scholar]
- 15.Morrison WA, MacLeod AM, O’Brien BM. Digital reconstruction in the mutilated hand. Ann Plast Surg. 1982;9:392–9. doi: 10.1097/00000637-198211000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Lee DC, Kim JS, Ki SH, Roh SY, Yang JW, Chung KC. Partial second toe pulp free flap for fingertip reconstruction. Plast Reconstr Surg. 2008;121:899–907. doi: 10.1097/01.prs.0000299945.03655.0d. [DOI] [PubMed] [Google Scholar]
- 17.Zheng H, Liu J, Dai X, Machens HG, Schilling AF. Free lateral great toe flap for the reconstruction of finger pulp defects. J Reconstr Microsurg. 2015;31:277–82. doi: 10.1055/s-0034-1396754. [DOI] [PubMed] [Google Scholar]
- 18.Yoon WY, Lee BI. Fingertip reconstruction using free toe tissue transfer without venous anastomosis. Arch Plast Surg. 2012;39:546–50. doi: 10.5999/aps.2012.39.5.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koshima I, Inagawa K, Urushibara K, Okumoto K, Moriguchi T. Fingertip reconstructions using partial-toe transfers. Plast Reconstr Surg. 2000;105:1666–74. doi: 10.1097/00006534-200004050-00011. [DOI] [PubMed] [Google Scholar]
- 20.Cho YJ, Roh SY, Kim JS, Lee DC, Yang JW. Second toe plantar free flap for volar tissue defects of the fingers. Arch Plast Surg. 2013;40:226–31. doi: 10.5999/aps.2013.40.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin CH, Lin YT, Sassu P, Lin CH, Wei FC. Functional assessment of the reconstructed fingertips after free toe pulp transfer. Plast Reconstr Surg. 2007;120:1315–21. doi: 10.1097/01.prs.0000279476.29055.5f. [DOI] [PubMed] [Google Scholar]


