Abstract
Background:
Surgery for hypertrophied breasts represents a challenge for plastic surgeons. The search for a good post-surgical cosmetic breast has led to the development of many techniques. Objectives for reduction mammoplasty are to achieve elevated, symmetrical breasts, a round shape, good projection, small cicatrices that are not very perceptible, and a lasting result.
Patients and Methods:
This study was carried out on sixty cases who had done reduction mammoplasty from January 2009 to December 2014. All patients were examined and were asked for late post-operative results and overall patients' satisfaction.
Results:
Long-term projection and contour of the breast were more satisfactory among patients who had superomedial pedicle with a statistically significant difference. No statistically significant difference was observed between patients underwent either superomedial or inferior pedicle reduction mammoplasty with regard to breast shape symmetry, nipple symmetry and sensation. The mean score for satisfaction was higher among patients who underwent superomedial pedicle rather than the inferior pedicle method.
Conclusion:
The superomedial pedicle shows better long-term cosmetic results.
KEY WORDS: Bottoming out, inferior pedicle, patients’ satisfaction, reduction mammoplasty, superomedial pedicle
INTRODUCTION
The female breast is the strongest feminine feature. For many women, breast reduction is a solution for the functional and aesthetic problems associated with large breasts.[1]
Surgery for hypertrophied breast represents a challenge for plastic surgeons. The search for a good cosmetic breast has led to the development of many techniques. The objective of a reduction procedure is primarily to reduce the size of the hypertrophic breast with appropriate re-draping of the skin envelope while maintaining a viable nipple-areola complex (NAC). Secondary objectives are to achieve elevated, symmetrical breasts, with round shape, good projection, small cicatrices that are not very perceptible, and a lasting result.[2]
Breast reduction procedures have been modified over time, with different methods employed for skin and glandular resection. The ‘inverted-T scar’ described by Wise in 1956 is based on a key-hole technique, with periareolar, vertical and infra-mammary fold scars.[3] This technique has been widely used ever since with a variety of associated NAC pedicles. The ‘vertical scar’ was originally designed by Lassus (1970) and is also used in the Lejour technique and is aimed to reduce the amount of scarring and the complication of T-junction skin necrosis.[3,4,5,6,7]
Reduction mammoplasty techniques differ in the way the NAC is transposed to its new higher position. During the past two decades, the trend was towards using a combination of dermal and glandular pedicles.[8]
The inferior pedicle technique, originally described in the mid-1970s in separate publications by Ribeiro, Courtiss and Goldwyn and Robbins, has perhaps become the most popular technique of reduction mammoplasty in North America. This technique gives consistent, reproducible results, with excellent survival of the NAC.[9,10,11,12]
However, it has the major disadvantage of late loss of conical projection due to sagging of lower breast tissue.[13,14]
The superomedial pedicle technique, described by Orlando and Guthrie in 1975, was able to produce a long-lasting projection of the breast with good reliability regarding NAC viability and sensibility.[15] It was developed to include more breast parenchyma beneath the pedicle, aimed to preserve both the vascularity and innervation to the NAC.[16,17]
The aim of this study is to evaluate the long-term follow-up outcome for reduction mammoplasty cases comparing both the inferior pedicle and the superomedial pedicle techniques as regard breast aesthetics, nipple sensation, scar acceptance and patient satisfaction.
PATIENTS AND METHODS
This study included sixty cases who had undergone reduction mammoplasty in the period from January 2009 to December 2014. All the surgeries were done by one surgeon.
The operative records for every patient were checked for the type of pedicle that was used either inferior pedicle or superomedial pedicle reduction mammoplasty, with the same ‘inverted-T’ skin incision type.
All patients were examined and asked for late post-operative results at least 1 year postoperatively as regards:
Long-term breast projection and contour
Breast symmetry
Recurrence of breast ptosis
Nipple position and sensation
Scar acceptance
Overall patient's satisfaction score. The satisfaction scale ranged from excellent = 5 to very poor = 1 (excellent = 5, good = 4, fair = 3, poor = 2 and very poor = 1).
Statistical analysis
Data were analysed and expressed in tables as mean values ± standard deviation. SPSS 19.0 (IBM Corp. Armonk, NY) program was used for data processing. Chi-square test was used to compare number and percentages between different groups. Values were considered statistically significant when P ≤ 0.05.
RESULTS
This study was done on female patients who had done reduction mammoplasty operation in our institution in the period from January 2009 to December 2014.
The total number of patients was sixty patients with a mean age of 29.2± 5.9 years [Table 1].
Table 1.
Age and marital status according to the type of procedure
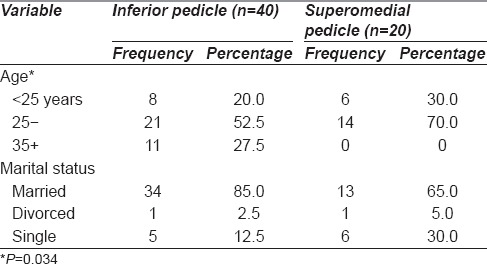
Records showed that reduction mammoplasty was done via superomedial or inferior pedicle in 33.3% (twenty patients) and 66.7% (forty patients), respectively. Studied patients who had superomedial pedicle were younger in age than those who had inferior pedicle, nearly one-fourth of the patients who had reduction mammoplasty via inferior pedicle were above 35 years of age with a statistically significant difference. However, no statistically significant difference was observed between the two groups concerning the marital status [Table 1].
Long-term post-operative assessment results of the patients' satisfaction concerning breast symmetry, long-term breast projection, recurrence of ptosis, nipple position and sensation, scar acceptance and overall satisfaction were as follows: Concerning the breast symmetry; records showed that breast symmetry was recorded in 58.3% of cases. Long-term projection and contour were satisfactory in 55.0% of cases, whereas recurrence of breast ptosis was recorded in nearly one-fourth of the cases (26.7%, n = 16). As for the nipple position, it was symmetrical in 58.3% of cases. Nipple sensation was decreased in 16 cases (26.7%) and lost in 3 cases (5.0%), whereas normal nipple sensation was recorded in 68.3% of cases [Table 2].
Table 2.
Post-operative characteristics of the reduction mammoplasty
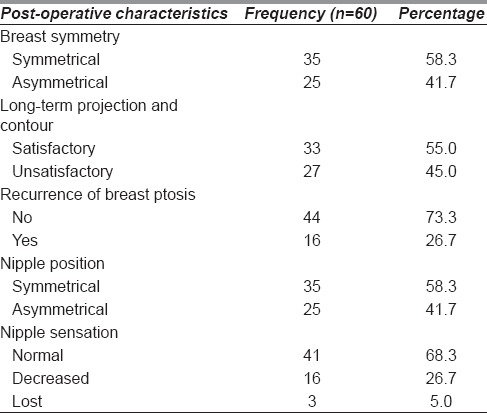
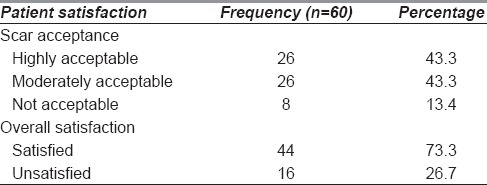
Post-operative scar was accepted by the majority of the patients (86.6%, n = 52), whereas non-acceptability of the scar was reported in 13.4% (n = 8). Moreover, the overall satisfaction was reported in nearly three-fourth of the cases (73.3%, n = 44) [Table 3].
Table 3.
Post-operative patient satisfaction
Comparing the two groups of patients according to the pedicle type, we found that patients' satisfaction about the long-term projection and contour of the breast was higher among patients who had superomedial pedicle with a statistically significant difference (P < 0.01) [Figure 1a and b].
Figure 1.
(a and b) Late post-operative patient who had superomedial pedicle reduction mammoplasty showing good
In addition, a lesser percentage of recurrence of breast ptosis was recorded among those who had superomedial pedicle compared to those who had inferior pedicle with a statistically significant difference (P = 0.007) [Figure 2a and b].
Figure 2.

(a and b) Late post-operative patient who had inferior pedicle reduction mammoplasty showing recurrence of glandular breast ptosis (bottoming out)
As for scar acceptance, higher acceptance was reported by patients who had reduction mammoplasty via superomedial pedicle compared to inferior pedicle with a statistically significant difference (P < 0.001). The overall satisfaction about the operation was higher among patients who had superomedial pedicle compared to those who had inferior pedicle with a statistically significant difference (P = 0.007). The mean score of satisfaction was higher among patients who had superomedial pedicle than inferior pedicle [Table 4].
Table 4.
Post-operative characteristics and patient satisfaction according to the type of pedicle
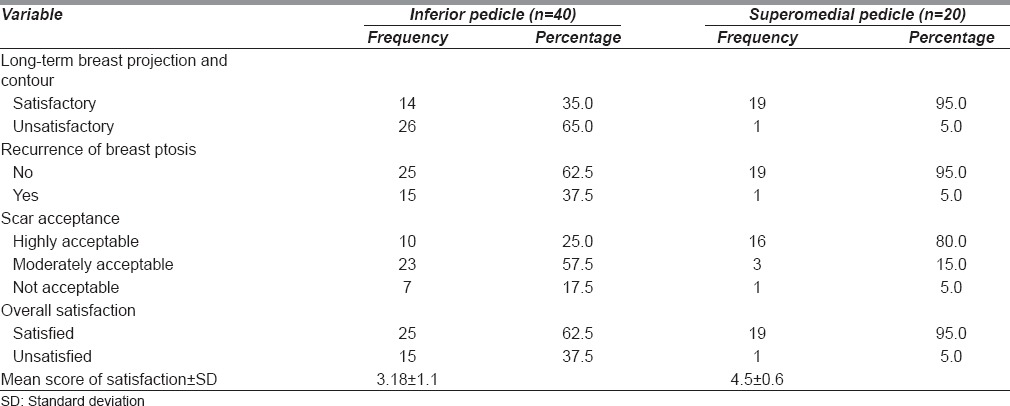
On the other hand, no statistically significant difference was observed between patients, concerning breast symmetry, nipple symmetry and sensation, who had either type of operation.
DISCUSSION
The search for the ideal technique to reduce the size of large breasts has continued for decades. The objective of a reduction procedure is primarily to reduce the size of the hypertrophic breast with appropriate re-draping of the skin envelope while maintaining a viable NAC.[2]
Criticisms of a procedure always include the loss of long-term projection, quality and length of scars, development of ‘bottoming out’. Several techniques have appeared over the years, and modifications of the basic principles have been published, but till now, there is no single technique that appears to fulfil all the criteria of excellence.[18]
In this study, comparing the long-term follow-up of the inferior pedicle and superomedial pedicle reduction mammoplasty, we found that patients' satisfaction about the long-term projection and contour of the breast was higher among patients who had superomedial pedicle. This result was in accordance with Nahabedian et al., 2000, as they have mentioned that the medial and superior-medial techniques give enhancement of the central breast projection.[18]
We also found that lesser percentage of recurrence of breast ptosis was recorded among those who had superomedial pedicle compared to those who had inferior pedicle technique.
Bericout, 1996, stated that, in inferior pedicle reduction mammoplasty, cleavage between the superior skin envelope and the dermoglandular pedicle makes the pedicle more exposed to the effects of gravity, and this increases the risk of secondary ptosis compared to other techniques.[19]
Inferior pedicle reduction mammoplasty is one of the most popular techniques, especially in North America. This technique is safe and can be applied equally to minimally, moderate, and massively enlarged breasts. The vascular basis of this pedicle is the musculocutaneous perforating branches of the internal mammary artery through the pectoralis major muscle and intercostal perforating branches through the muscle. It is very reliable and safe technique. However, the need to preserve and maintain central and lower breast tissue may lead to post-operative bottoming out.[20]
Later, bottoming out of the breast or pseudoptosis was considered an inevitable sequel of the inferior pedicle technique.[21,22,23]
On the other hand, no statistically significant difference was observed between patients that underwent either type of operations concerning breast symmetry, nipple symmetry and sensation.
Inferior pedicle technique was able to achieve a good cosmetic result with a reliable vascular and nerve supply to the NAC.[13,14]
Superomedial technique was able to produce a good aesthetic result with regard to conical breast projection with normal NAC sensation. This is explained by the fact that incorporating a medial component to the superior pedicle preserves the anterior cutaneous branches of the 2nd–5th intercostal nerves.[2]
We found that the overall satisfaction about the operation was higher among patients who underwent superomedial pedicle compared to those who had an inferior pedicle one.
Studies have shown that the choice of reduction mammoplasty technique has a considerable influence on the durability of the aesthetic result. This was attributed to the gradual increase in the length of the vertical infra-areolar scar (bottoming out effect) which was maximum in the inferior pedicle and minimum in the superior pedicle. Thus, the superior-medial pedicle shows the better long-term cosmetic result.[24]
CONCLUSION
From this study, comparing the long-term follow-up of the inferior pedicle and superomedial pedicle reduction mammoplasty, we concluded that the superomedial pedicle shows better long-term aesthetics, projection and contour of the breast in addition to the diminished incidence of glandular ptosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Guyuron B. Indications, Operations and Outcomes. St. Louis: Mosby; 2000. Plastic Surgery; p. 2709. [Google Scholar]
- 2.Finger RE, Vasquez B, Drew GS, Given KS. Superomedial pedicle technique of reduction mammaplasty. Plast Reconstr Surg. 1989;83:471–80. doi: 10.1097/00006534-198903000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Lassus C. A technique for breast reduction. Int Surg. 1970;53:69–72. [PubMed] [Google Scholar]
- 4.Lassus C. Breast reduction: Evolution of a technique – a single vertical scar. Aesthetic Plast Surg. 1987;11:107–12. doi: 10.1007/BF01575495. [DOI] [PubMed] [Google Scholar]
- 5.Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97:373–80. doi: 10.1097/00006534-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94:100–14. doi: 10.1097/00006534-199407000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Lejour M, Abboud M, Declety A, Kertesz P. Reduction of mammaplasty scars: From a short inframammary scar to a vertical scar. Ann Chir Plast Esthet. 1990;35:369–79. [PubMed] [Google Scholar]
- 8.McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245–52. doi: 10.1097/00006534-197203000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59:64–7. doi: 10.1097/00006534-197701000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500–7. [PubMed] [Google Scholar]
- 11.Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55:330–4. [PubMed] [Google Scholar]
- 12.Hidalgo DA, Elliot LF, Palumbo S, Casas L, Hammond D. Current trends in breast reduction. Plast Reconstr Surg. 1999;104:806–15. [PubMed] [Google Scholar]
- 13.Mizgala CL, MacKenzie KM. Breast reduction outcome study. Ann Plast Surg. 2000;44:125–33. doi: 10.1097/00000637-200044020-00001. [DOI] [PubMed] [Google Scholar]
- 14.Bohmert H, Gabka CJ. A Surgical Atlas. Stuttgart, New York: Thieme; 1997. Plastic and Reconstructive Surgery of the Breast; p. 37. [Google Scholar]
- 15.Orlando JC, Guthrie RH., Jr The superomedial dermal pedicle for nipple transposition. Br J Plast Surg. 1975;28:42–5. doi: 10.1016/s0007-1226(75)90149-6. [DOI] [PubMed] [Google Scholar]
- 16.Hauben DJ. Experience and refinements with the supero-medial dermal pedicle for nipple-areola transposition in reduction mammoplasty. Aesthetic Plast Surg. 1984;8:189–94. doi: 10.1007/BF01597524. [DOI] [PubMed] [Google Scholar]
- 17.Hugo NE, McClellan RM. Reduction mammaplasty with a single superiorly-based pedicle. Plast Reconstr Surg. 1979;63:230–4. doi: 10.1097/00006534-197902000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Nahabedian MY, McGibbon BM, Manson PN. Medial pedicle reduction mammaplasty for severe mammary hypertrophy. Plast Reconstr Surg. 2000;105:896–904. doi: 10.1097/00006534-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Bricout N. Breast Surgery. Paris: Springer-Verlag; 1996. [Google Scholar]
- 20.Nahai F. The Art of Aesthetic Surgery. Missouri: Quality Medical Publishing, Inc.; 2005. Clinical decision-making in Breast surgery; pp. 1817–58. [Google Scholar]
- 21.Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29:379–91. doi: 10.1016/s0094-1298(02)00008-1. [DOI] [PubMed] [Google Scholar]
- 22.Reus WF, Mathes SJ. Preservation of projection after reduction mammaplasty: Long-term follow-up of the inferior pedicle technique. Plast Reconstr Surg. 1988;82:644–52. doi: 10.1097/00006534-198810000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Karp NS. Medial pedicle/vertical breast reduction made easy: The importance of complete inferior glandular resection. Ann Plast Surg. 2004;52:458–64. doi: 10.1097/01.sap.0000124390.27129.b5. [DOI] [PubMed] [Google Scholar]
- 24.White DJ, Maxwell GP. Reduction mammoplasty. In: Achauer BM, Eriksson E, Guymon B, Coleman JJ III, Russell RC, Nander Kolh A, et al., editors. Plastic Surgery Indications, Operations, and Outcomes. St Louis: Mosby; 2000. pp. 2705–43. [Google Scholar]



