Abstract
BACKGROUND
Understanding the differences in care-seeking pattern is key in designing interventions aimed at improving health-care service delivery, including prevention and control of noncommunicable diseases. The aim of this study was to identify the differences and determinants of care-seeking patterns of urban and rural residents in Abia State in southeast Nigeria.
METHODS
This was a cross-sectional, community-based, study involving 2999 respondents aged 18 years and above. Data were collected using the modified World Health Organization’s STEPS questionnaire, including data on care seeking following the onset of illness. Descriptive statistics and logistic regressions were used to analyze care-seeking behavior and to identify differences among those seeking care in urban and rural areas.
RESULTS
In both urban and rural areas, patent medicine vendors (73.0%) were the most common sources of primary care following the onset of illness, while only 20.0% of the participants used formal care. Significant predictors of difference in care-seeking practices between residents in urban and rural communities were educational status, income, occupation, and body mass index.
CONCLUSIONS
Efforts should be made to reduce barriers to formal health-care service utilization in the state by increasing health insurance coverage, strengthening the health-care system, and increasing the role of patent medicine vendors in the formal health-care delivery system.
Keywords: health care, behavior, formal care, informal care, patent medicine vendors, Nigeria
Introduction
Over the past two decades, significant declines in mortality associated with noncommunicable diseases (NCDs) have been reported in developed countries. Available evidence suggests that this decline is attributable to both population-wide primary prevention and individual health-care interventions, including improvement in care-seeking behavior.1 Health-care-seeking behavior has been defined as any action undertaken by individuals who perceive themselves to have a health problem for the purpose of finding an appropriate remedy2 or as a sequence of remedial actions that individuals undertake to rectify perceived ill health.3 It can also be described as the process of remedial actions that individuals accept for improvement of their perceived disease.4,5 Health-care-seeking behavior is believed to be a summation of individual characteristics, the nature of the environment in which a person lives, and the interaction between individual and environmental factors. It includes issues of whether, when, and from where care is sought for an illness.6
An NCD is defined as a medical condition or disease that is noninfectious and non-transmissible among people.7 There are four main types of NCDs, which include cardiovascular diseases, cancers, respiratory diseases, and diabetes. Currently, NCDs are the leading causes of death and disease burden worldwide, accounting for nearly 38 million (68.0%) deaths out of 58 million deaths in 2012. Sixteen million (40%) of these deaths are considered premature, occurring in those aged less than 70 years. Furthermore, almost 75% of all NCDs-related deaths and majority of the premature deaths (82%) occur in low- and middle-income countries (LMICS). Risk factors for NCDs include smoking, alcohol use, physical inactivity, poor diet, and obesity.1
Care-seeking behavior is a key factor influencing health-care service utilization. It is also a major determinant of health outcomes, in that the timing of the initiation of care, the place where care is sought, and the type of treatment received often determine the duration, prognosis, and outcome of an illness. Delay in correctly and promptly diagnosing a disease and initiating appropriate treatment has been associated with increased disease morbidity and mortality.5,8
Individual health-seeking behavior is crucial for personal, societal, and national development.9 Understanding care-seeking practices in a given society and determining the factors influencing care seeking should enable health systems to adapt strategies to respond to specific community perceptions about health and care. In addition, knowing a community’s first treatment option is of crucial importance. That knowledge should help create and strengthen a care resource in the community, which can be used as a patient recruitment and referral point.4 Furthermore, understanding community health-care-seeking behavior should help in the optimization of allocation of health resources and distribution by supporting the planning and implementation of appropriate interventions to improve care-seeking practices in the community.10–12
A number of studies have reported differences in health-care-seeking behavior between urban and rural communities and the factors associated with those differences. These factors include internal and external factors.5 They include patient sociodemographic and socioeconomic characteristics such as gender, age, income, educational status, marital status, health literacy, and illness type and severity.8,13 Other indicators are community-related and health-system-related factors such as the presence of significant others, including spouses and other family members, access and cost of health-care services, availability of heath resources and services, attitude of health-care staff, convenience, payment mechanism, satisfaction with health-care services provided, community perception of a disease, and health belief model (HBM).3–5,8,13,14
The HBM assumes that health behavior is determined by personal beliefs or perceptions about a disease and the measures available to reduce its occurrence. Originally, there were four main constructs of the model, perceived seriousness of the problem, perceived susceptibility of the problem to a remedy, perceived benefits of treatment, and perceived barriers to treatment. More recently, the model has been expanded to accommodate other constructs such as cues to action, motivating factors, and self-efficacy. It is believed that each of these can either individually or in combination with others influence health behavior.15
Mechanic David had earlier identified a wide range of cultural and social factors influencing how people respond to illness, among which are the following16:
Visibility or recognizability of symptoms
Perceived seriousness of symptoms
Extent to which symptoms disrupt family, work, and other social activities
Frequency of the appearance of symptoms, their persistence, or frequency of recurrence
Tolerance threshold of those who are exposed to and evaluate the deviant signs and symptoms
Available information, knowledge, and cultural assumptions and understandings of the evaluator
Needs competing with illness response
Competing possible interpretations that can be assigned to the symptoms once they are recognized
The availability of treatment resources, physical proximity, and psychological and monetary costs of taking action
Both the HBM and Mechanic’s work clearly emphasize that interventions aimed at improving health status of individuals, and communities should be focused at addressing factors influencing individuals’ willingness to engage in health-care-seeking behavior.
In Nigeria, few studies have investigated health-care utilization patterns in relation to care-seeking behavior, and most of these efforts focused on reproductive health and NCDs.17–22 However, the rising prevalence of NCD-related morbidity and mortality in the country1 underlines the need to assess individual’s care-seeking practices in relation to NCD prevention and control. Anecdotal evidence suggests that people affected by NCDs often do not often seek appropriate care in the early stages of an NCD, because the onset of most NCDs is insidious and progression is slow.
Furthermore, lack of access to NCD screening services in many communities means that most patients present to health facilities in the later stages of such diseases, after complications have arisen.23 A review of literature showed that few studies have examined differences in health-seeking behavior among urban and rural communities, as it relates to NCDs in LMICS. This study therefore aimed at identifying urban–rural differences in health-care-seeking behavior and its implications in the control of NCDs among residents of a single state in an African nation.
Methods
Data
The research was carried out in Abia State in southeast Nigeria as part of the study of NCDs in the state. A survey emphasizing NCDs and their risk factors was conducted between August 2011 and April 2012. The estimated population of the state as of 2015 was 3,601,916, based on the 2006 population and an annual estimated growth rate of 2.8%.24 The study population consisted of all individuals aged 18 years and above, who had been a resident in the state for at least six months prior to the time of the survey.
This was a community-based, cross-sectional study. The final, estimated minimum required sample size for the study was 2800 participants aged 18–78 years, after adjusting for design effect and age–sex estimates. This target sample size was further adjusted upward to 3200 in anticipation of a 10% nonresponse rate.
Pregnant women were excluded because of pregnancy-related changes in anthropometry, blood pressure, and biochemical parameters. Chronically ill and debilitated individuals who lacked the physical and mental ability to live independently were excluded from the study because of their inability to consent to or participate in the survey.
Study participants were selected using a multistaged sampling technique. The state is statutorily divided into 3 senatorial zones and has 17 Local Government Areas (LGAs) (Fig. 1). The LGAs in the state were stratified by senatorial zone and locality. From each senatorial zone, a representative urban and rural LGAs were selected by simple random sampling. In Nigeria, an urban area is defined as an area with a population size of ≥20,000 people, with basic social and physical infrastructure and so designated through a legal or administrative instruments.25 This strategy was used in the present study to identify urban and rural areas for inclusion in the survey.
Figure 1.
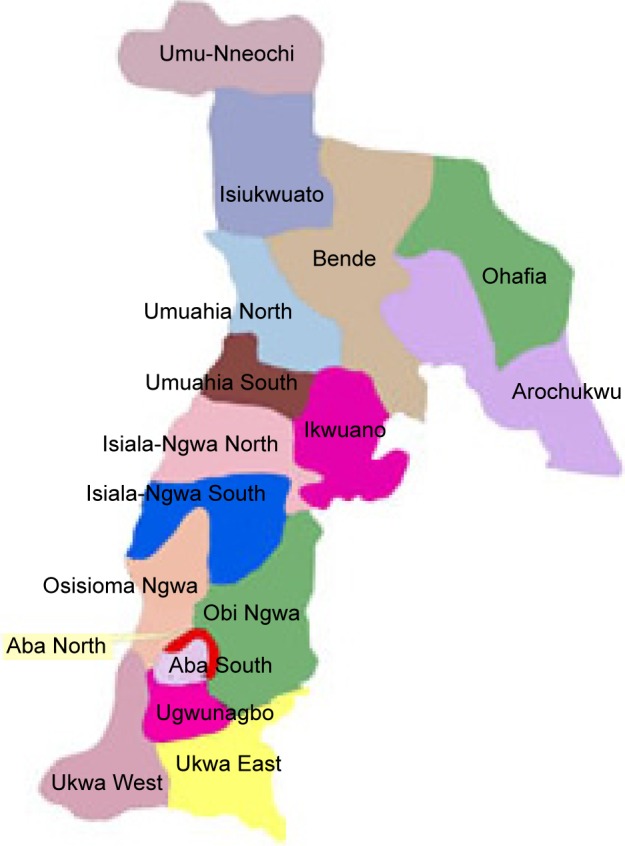
Map of Abia State showing the 17 local government areas.
From each LGA, four enumeration areas (EAs) were selected by simple random sampling technique from the list of EAs in the LGAs. The maps and previous listing of houses/households in each selected EAs were updated with the help of the staff of the National Population Commission. From a prominent landmark in a selected EA, households were identified and eligible respondents were recruited moving in a clockwise direction. Not more than two eligible participants of opposite sex were selected from each household until a total of 120 participants were selected from each EA.
Ethical approval for the study was obtained from Abia State Ministry of Health, Umuahia, while written consent was obtained from each study participants after explanation of the purpose, procedure, benefits, and risks associated with the survey. In addition, the study was conducted in compliance with Helsinki Declaration.
Measurements
Data were collected by a team of trained health-care workers under the supervision of the survey project team composed of three public health consultants: a nephrologist, a cardiologist, and a health program manager with the State Ministry of Health. Using a modified World Health Organization’s (WHO) STEPS questionnaire,26 responses were elicited from the respondents in both English and Igbo languages on the following: sociodemographic characteristics, income (daily, weekly, or monthly income [in Naira] depending on the nature of occupation), use of alcohol, history of smoking, physical activity, history of diabetes mellitus or hypertension, and places where treatment was sought following the onset of illness.
In addition, anthropometry and blood pressure measurements were performed for all the respondents, and half had their blood sugar measured using ACCU-CHECK glucometer (Roche Diabetes Care Ltd). The interviewers used bathroom scales for weight measurement, while height was measured using stadiometer. Blood pressure was measured digitally twice at five-minute intervals, using Omron M2 Digital Blood Pressure (OMRON Healthcare Europe B.V.). The final blood pressure measurement was an average of the two readings. Average duration of administration of the questionnaire and measurements was 30 minutes.
Hypertension was defined to include individuals with a known history of hypertension and also those diagnosed with hypertension during the survey (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg). Diabetes was also defined as individuals with known history of diabetes and also those diagnosed with diabetes during the survey using fasting blood sugar level of ≥126 mg/dL or random blood sugar of ≥180 mg/dL.
The respondents’ age was estimated in years and was categorized as follows: 18–39, 40–59, and ≥60 years. Income data were analyzed for 2006 (69.3%) respondents who provided information on their income; however, those who did not respond to question on income, students, and those currently unemployed were excluded from the analysis of income. Income status was categorized into low <N100,000/annum and high <N100,000/annum. Body mass index (BMI) was classified into two categories: normal weight <25 kg/m2 and overweight/obesity ≥25 kg/m2. Alcohol use was defined by those with a history of alcohol ingestion in the last 12 months. Physical activity level was first measured in metabolic equivalent of task (MET) minutes per week and was then categorized as follows: ≥600 MET minutes/week as moderate–high level of physical activity and <600 MET minutes/week as low level of physical activity in accordance with WHO’s recommendations on physical activity for health.27
Seeking formal health care was defined as seeking care from trained health-care providers (doctor, nurse, or community health extension workers working in a health facility hospital/clinic or health center). Seeking informal care was defined as seeking help from other individuals such as patent medicine vendors (PMVs), also known as chemists, traditional healers, spiritualists, or self-medication.
Analysis strategy
The data were collected and entered by double entry by two data entry clerks into epi-data26 and were exported to SPSS. Analysis was performed using SPSS version 21.0 (SPSS Inc.). Descriptive and frequency statistics were used to determine the general characteristics of the study population. Association between individual characteristics and differences in health-care seeking between urban and rural areas was evaluated using chi-squared test, with a P-value of <0.05 assumed to be statistically significant.
Multivariate logistic regression analysis was used to identify differences in seeking formal care between individuals living in urban and rural communities in the state. The dependent variable was the site where formal care was sought—urban or rural, while the independent variables included factors that were found to be significantly associated with formal care seeking in the bivariate analysis. They included age, educational status, occupation, income, and BMI. The significance of odds ratio was assessed using 95% confidence intervals (95% CI), adjusted for the use of a multistage sample.
Results
A total of 2999 participants were recruited for the survey. The relevant sections of the instrument were completed by 2983 participants, which was 90% of the original targeted sample size. Table 1 shows the characteristics of the respondents by locality.
Table 1.
General characteristics of the respondents by urban/rural residence.
| CHARACTERISTIC | URBAN n = 1396 (%) |
RURAL n = 1587 (%) |
χ2 | P-VALUE |
|---|---|---|---|---|
| Age (in years) | ||||
| 18–39 | 59.8 | 48.8 | ||
| 40–59 | 24.4 | 27.4 | 42.98 | <0.001 |
| ≥60 | 15.8 | 23.8 | ||
| Mean (SD) | 39. 3 ± 17.4 | 43.9 ± 19.2 | ||
| Gender | ||||
| Male | 50.1 | 46.1 | 4.79 | 0.03 |
| Female | 49.9 | 53.9 | ||
| Marital status | ||||
| Married | 53.7 | 62.3 | 22.73 | <0.001 |
| Not married | 46.3 | 37.7 | ||
| Educational status | ||||
| <Secondary | 26.5 | 43.0 | 88.5 | <0.001 |
| ≥Secondary | 73.5 | 57.0 | ||
| Occupation | ||||
| Professional/skilled | 19.1 | 12.5 | ||
| Semi-skilled | 21.8 | 18.3 | ||
| Unskilled | 28.4 | 43.1 | 92.96 | <0.001 |
| Unemployed/students | 30.7 | 26.1 | ||
| Average annual income (in Naira) | n = 929 | n = 1077 | ||
| <100,0000 | 41.8 | 57.2 | 47.50 | <0.001 |
| ≥100,000 | 58.2 | 42.8 | ||
| Mean (SD); Median | 268,416.45 144,000.00 | 171,118.85 96,000.00 |
As indicated in Table 1, urban dwellers were more likely than those dwelling in rural areas to be more highly educated, younger, more likely to be single, more likely to hold a higher status occupation, and more likely to have a higher annual income.
Table 2 shows the distribution of NCDs and associated risk factors among the respondents by place of residence. Overall prevalence of NCDs and associated risk factors were: diabetes, 3.6%; hypertension, 39.7%; smoking, 13.3%; overweight/obesity, 39.9%; physical inactivity, 51.3%; and alcohol use, 47.0%. Residents in urban communities were more likely to have higher prevalence of hypertension (63.5% vs 57.5%), overweight/obesity (44.8% vs 35.7%), and higher level of physical activity (50.7% vs 46.9%) than those in rural areas. There was no significant difference in the prevalence of diabetes, smoking, and alcohol use between urban and rural areas.
Table 2.
Distribution of prevalence of NCDs and associated risk factors for respondents in urban and rural areas.
| NCDS/RISK FACTOR | URBAN n = 1396 (%) |
RURAL n = 1587 (%) |
TOTAL n = 2983 (%) |
χ2 | P-VALUE |
|---|---|---|---|---|---|
| Diabetes | |||||
| No | 95.9 | 96.8 | 96.4 | 1.05 | 0.31 |
| Yes | 4.1 | 3.2 | 3.6 | ||
| Hypertension | |||||
| No | 63.5 | 57.5 | 60.3 | ||
| Yes | 36.5 | 42.5 | 39.7 | 10.94 | 0.001 |
| Smoking status | |||||
| Yes | 13.2 | 13.5 | 13.3 | 0.06 | 0.81 |
| No | 86.8 | 86.5 | 86.7 | ||
| BMI | |||||
| Normal | 55.2 | 64.3 | 60.1 | 21.87 | <0.001 |
| Overweight/obese | 44.8 | 35.7 | 39.9 | ||
| Alcohol use | |||||
| Yes | 49.2 | 45.9 | 47.0 | 1.57 | 0.21 |
| No | 51.6 | 54.1 | 53.0 | ||
| Physical activity level (MET mins/week) | |||||
| <600 | 49.3 | 53.1 | 51.3 | 3.84 | 0.05 |
| ≥600 | 50.7 | 46.9 | 48.7 | ||
| Mean (SD);Median | 978.5 (946.5); 685.7 | 1056.3 (901.0); 822.9 | 1020.5 (881.7); 728.9 |
Figure 2 shows care-seeking practices of the respondents following the onset of an episode of illness. The majority of respondents in both urban and rural areas were most likely to utilize the services of PMVs: 73.0%; following the onset of illness, followed by hospital/clinic, 12.4%; and primary health center, 6.6%. Utilization of formal health-care services— hospital/clinic or health centers—was almost the same in both urban (21.1%) and rural areas (20.1%). However, more respondents in urban areas (17.2%) visited a hospital/clinic following the onset of illness compared to 11.1% in rural areas, while more respondents in rural areas (9.0%) were more likely to visit primary health centers than urban residents (3.9%). However, these differences in formal care seeking were not statistically significant.
Figure 2.
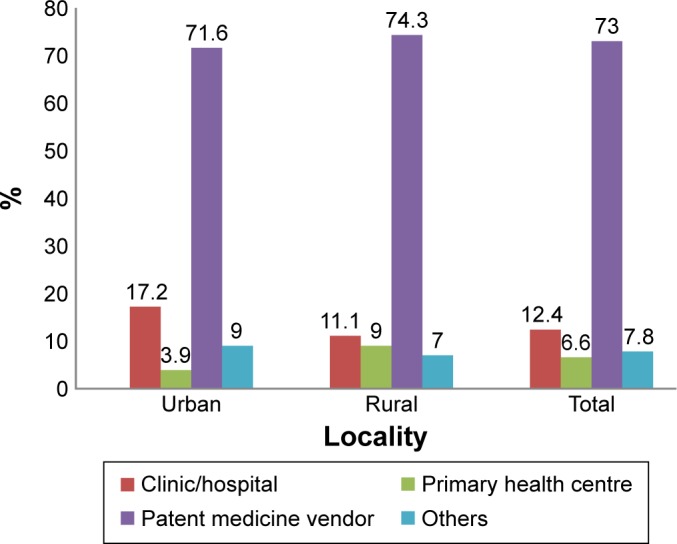
Places where care was sought following the onset of illness.
Residents seeking formal health care was 294 (21.1%) and 319 (20.1%) in urban and rural areas, respectively.
Table 3 shows respondents’ characteristics associated with bivariate differences in the use of formal health-care services in urban and rural communities. As indicated in the table, those seeking formal care in urban or rural areas differed along a number of dimensions. There were significant differences in age, educational status, occupation, income, and BMI status of respondents utilizing formal health-care services in urban and rural areas. Those who sought formal care in urban areas were significantly more likely to be older and more highly educated, with higher status occupations and higher incomes. Interestingly, in the bivariate analyses, those identified as having an NCD and living in an urban area did not differ from those with an NCD in rural areas in their use of formal care.
Table 3.
Respondents’ characteristics associated with differences in the use of formal health care between urban and rural areas.
| CHARACTERISTIC | URBAN N = 294 (%) |
RURAL N = 319 (%) |
χ2 | P-VALUE |
|---|---|---|---|---|
| Age (in years) | ||||
| 18–39 | 18.6 | 30.7 | 15.56 | <0.001 |
| 40–59 | 25.8 | 27.8 | ||
| ≥60 | 55.7 | 41.5 | ||
| Gender | ||||
| Male | 44.2 | 37.6 | 2.76 | 0.10 |
| Female | 55.8 | 62.4 | ||
| Marital status | ||||
| Married | 64.2 | 69.5 | 1.96 | 0.16 |
| Not married | 35.8 | 30.5 | ||
| Educational status | ||||
| ≥Secondary | 79.5 | 60.4 | ||
| <Secondary | 20.5 | 39.6 | 26.39 | <0.001 |
| Occupation | ||||
| Professional/skilled | 33.2 | 21.5 | ||
| Semiskilled | 17.0 | 10.8 | ||
| Unskilled | 20.1 | 38.6 | 29.30 | <0.001 |
| Unemployed/students | 29.8 | 29.1 | ||
| Annual income (in Naira) | ||||
| <100,0000 | 38.1 | 57.2 | ||
| ≥100,000 | 61.9 | 42.8 | 15.21 | <0.001 |
| Diabetes | ||||
| Yes | 9.0 | 6.1 | ||
| No | 91.0 | 93.9 | 1.13 | 0.29 |
| Hypertension | ||||
| Yes | 40.1 | 46.7 | ||
| No | 59.9 | 53.3 | 2.69 | 0.10 |
| Alcohol use | ||||
| Yes | 60.2 | 64.6 | 1.25 | 0.26 |
| No | 39.8 | 35.4 | ||
| Smoking status | ||||
| Yes | 11.9 | 10.0 | ||
| No | 88.1 | 90.0 | 0.55 | 0.46 |
| BMI | ||||
| Normal | 47.1 | 56.9 | 4.69 | 0.03 |
| Overweight/obesity | 52.9 | 43.1 | ||
| Physical activity level (MET mins/week) | ||||
| <600 | 42.7 | 43.7 | 0.05 | 0.83 |
| ≥600 | 57.3 | 56.3 |
Multivariate logistic regression analysis was used to identify significant predictors of urban–rural differences in formal health-care service utilization as shown in Table 4. Only those who sought formal health-care services were included in the model, and the dependent variable reflected whether they lived in an urban or a rural area. Those seeking formal care in an urban area, in comparison to those seeking formal care in a rural area, were more likely to have at least secondary education, adjusted odds ratio (AOR; 95% CI) = 1.38 (1.05–1.82); less likely to be unemployed or a student, AOR (95% CI) = 0.59 (0.38–0.90); more likely to be earning income ≥N100,000, AOR (95% CI) = 1.40 (1.11–1.76); and more likely to be overweight/obese, AOR (95% CI) = 1.43 (1.14–1.80).
Table 4.
Logistic regression predicting the use of formal health services in urban and rural areas.
| VARIABLES | AOR (95% C.I.) |
|---|---|
| Age (in years) | |
| 18–39 | – |
| 40–59 | 1.26 (0.88–1.81) |
| ≥60 | 1.22 (0.86–1.73) |
| Educational status | |
| <Secondary | – |
| ≥Secondary | 1.38 (1.05–1.82)* |
| Occupation | |
| Professional/skilled | – |
| Semiskilled | 1.30 (0.78–2.18) |
| Unskilled | 0.97 (0.63–1.51) |
| Unemployed/students | 0.59 (0.38–0.90)* |
| Annual income (in Naira) | |
| <100,0000 | – |
| ≥100,000 | 1.40 (1.11–1.76)* |
| BMI | |
| Normal | – |
| Overweight/obesity | 1.43 (1.14–1.80)* |
Notes: –, reference category.
Statistically significant.
Discussion
This study population exhibited relatively higher prevalence of hypertension and diabetes and associated risk factors— obesity, smoking, alcohol consumption, and physical inactivity compared to previous studies.28–30 Rising prevalence of NCDs has been reported in a number of LMICS, despite the existing high burden of communicable diseases. This phenomenon has been described as a double burden of disease that is not faced in higher income countries with their lower prevalence of infectious diseases.31
Changes in lifestyle such as dietary habits, increasing sedentary activity, and transition from agrarian to urbanized society are among the factors identified as being responsible for rising prevalence of NCDs.1 However, it is worthy to note that these changes are taking place in both rural and urban communities in Abia State though at different rate, as there was no significant difference in the prevalence of NCDs and associated risk factors in both localities except for hypertension and overweight/obesity. Higher prevalence of hypertension was reported in rural communities than in urban communities, and this is probably due to higher proportion of older people in rural than in urban areas. The prevalence of overweight/obesity reported in urban areas was higher than that in rural areas, which could be attributed to lower level of physical activity among urban residents. Since urban and rural communities in the state are largely equally affected by NCDs, measures to reduce its burden in the state should target both urban and rural communities.
Currently, there is no coordinated response in the state to reduce the burden of NCDs and associated risk factors. Hence, the prevalence of these conditions is likely to remain high and potentially increase, until programs and policies are put in place to reverse the trend. This study showed that overall utilization of formal health-care services following the onset of illness was low (20.0%). In general, PMVs were the most common sources of primary care following the onset of illness. Previous research indicates that PMVs play a significant role in health-care delivery in Nigeria.32–34
Highlighting the danger of patronizing PMVs, Onah and Govender32 pointed out that these care providers are more likely to provide substandard care to their clients because their activities in the country are unregulated. While others have reported their positive role in health-care service delivery and suggested that they might be reoriented and integrated into the country’s health-care system considering their high accessibility and the high level of confidence they enjoy from community members.12,13,33 Given the dominant role played by PMVs in both urban and rural areas, training and integration of these care providers into the formal health-care system, possibly as source of information on disease prevention and referrals to formal health-care providers, might be a useful avenue for reform.
Low utilization of formal health sector in the state as observed in this study could be attributed to the following: nonavailability of basic equipment and drugs, attitude of health-care workers, unavailability of services, costs, distance, incessant strikes by health workers, weak health system, poor funding of the health sector, and payment mechanism which is predominantly out of pocket payments.35,36 An assessment of 40 primary health-care facilities in the state on provision of youth-friendly services showed that 80% of them had a functional sphygmomanometer for measuring blood pressure while none had a glucometer.37
In realization of the need to improve utilization of formal health-care services in Nigeria, a national health act was enacted in 2014. The goal of the act was to ensure universal health coverage for all Nigerians by addressing inequities in access to health care. This legislation intends to achieve greater equity in access by increased funding of the health sector, removing barriers to health services through expansion of health insurance coverage and strengthening the health-care systems.38 Increased funding of the health sector will help address deficiency in equipment and supplies including drugs required to prevent and control NCDs.
Removing barriers to accessing health-care services and improving the quality of health-care services will help improve utilization of formal health-care services including prevention and control services of NCDs. Screening, diagnosis, and management of NCDs in the state are currently limited to tertiary and some secondary health facilities. Therefore, establishment of comprehensive NCD services involving the primary health-care centers in the state will improve the uptake of formal health-care services.
While no significant urban–rural difference was observed in the rates at which formal health-care services were used, there were significant differences in respondents’ characteristics that influenced utilization of formal health-care services in both localities. Most of these factors were socioeconomic: educational status, income, and occupation. High income and high educational status were associated with higher utilization of formal health care in urban areas.
Overall utilization of formal health-care services was low, with no difference observed between residents in urban and rural communities. Therefore, the effects of the current efforts of the Nigerian government to increase access to quality health-care services through universal health coverage may not vary across urban and rural settings. The state on its part should develop policies and programs aimed at increasing the availability of prevention and control services of NCDs in formal care settings so that the anticipated increase in the uptake of formal health-care services will translate into reduction of the burden of NCDs.
Educational status, income level, occupation, and BMI status were found to have significantly influenced the differences in health-care service utilization between urban and rural communities in the state. Therefore, interventions to address differences in care-seeking behavior of urban and rural communities in the state should take into consideration measures to reduce socioeconomic barriers to seeking formal health care. In addition, as some researchers have recommended increasing the role for PMVs in the management of disease conditions such as malaria, STIs, and tuberculosis,21,39–41 the same can be argued for NCDs even though management of NCDs is complex and challenging, requiring regular monitoring and follow-up. PMVs can be trained on screening for hypertension and diabetes using electronic sphygmomanometer and glucometer respectively and referring identified cases to formal health-care facilities for continuing care. They can also be trained on monitoring blood pressure and blood glucose of patients already on treatment, identifying non-adherent/poorly adherent patients, and providing health education on NCDs. Involving PMVs in screening and monitoring of patients with hypertension and diabetes will increase community members’ access to these services.
Like most studies, this effort has limitations. Because this was a cross-sectional study, causal inferences could not be ascertained. In addition, the study did not examine community-related and health facility-related factors influencing care-seeking behavior among the respondents.
Footnotes
ACADEMIC EDITOR: Charles Phillips, Editor in Chief
PEER REVIEW: Eight peer reviewers contributed to the peer review report. Reviewers’ reports totaled 3142 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: OSO, UUO, OOM, AUU, IIC, AOM. Analyzed the data: UUO. Wrote the first draft of the manuscript: UUO. Contributed to the writing of the manuscript: OSO, IIC. Agree with manuscript results and conclusions: OSO, UUO, IIC. Jointly developed the structure and arguments for the paper: OOM, AUU, AOM. Made critical revisions and approved final version: UUO, OSO. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.World Health Organisation . Global Status Report on Noncommunicable Diseases 2010. Geneva: WHO Press, World Health Organisation; 2011. [Google Scholar]
- 2.Olenja J. Health seeking behaviour in context. East Afr Med J. 2003;80(2):61–62. doi: 10.4314/eamj.v80i2.8689. [DOI] [PubMed] [Google Scholar]
- 3.Fomundam H, Abraham Tesfay A, Andrew Maranga A, Lucia Chanetsa L, Vieira Muzoola V, Frederick Oyaro F. Identifying treatment and healthcare seeking behavior as a means of early HIV/AIDS intervention in Africa. World J AIDS. 2012;2:165–173. [Google Scholar]
- 4.Bahrami MA, Atashbahar O, Shokohifar M, Montazeralfaraj R. Developing a valid tool of treatment seeking behavior survey for Iran. J Novel Appl Sci. 2014;3(6):651–660. [Google Scholar]
- 5.Atashbahar O, Bahrami MA, Asqari R, Fallahzadeh H. An examination of treatment seeking behaviour affecting factors: a qualitative study in Iran. World Appl Sci J. 2013;25(5):774–781. [Google Scholar]
- 6.Chomi EN, Mujinja PGM, Enemark U, Hansen K, Kiwara AD. Health care seeking behaviour and utilisation in a multiple health insurance system: does insurance affiliation matter? Int J Equity Health. 2014;13:25. doi: 10.1186/1475-9276-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HC, Oh SM. Noncommunicable diseases: current status of major modifiable risk factors in Korea. J Prev Med Public Health. 2013;46(4):165–172. doi: 10.3961/jpmph.2013.46.4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uddin MJ, Alam N, Sarma H, et al. Consequences of hypertension and chronic obstructive pulmonary disease, healthcare-seeking behaviors of patients, and responses of the health system: a population-based cross-sectional study in Bangladesh. BMC Public Health. 2014;14:547. doi: 10.1186/1471-2458-14-547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chauhan RC, Manikandan Purty AJ, Samuel A, Singh Z. Determinants of health care seeking behavior among rural population of a coastal area in South India. Int J Sci Rep. 2015;1(2):118–122. [Google Scholar]
- 10.van der Hoeven M, Kruger A, Greeff M. Differences in health care seeking behaviour between rural and urban communities in South Africa. Int J Equity Health. 2012;11:31. doi: 10.1186/1475-9276-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah T, Patel M, Shah V. Health care seeking behaviour of urban and rural community in Ahmedabad district. Int J Med Sci Public Health. 2013;2:908–911. [Google Scholar]
- 12.MacKian S. A Review of Health Seeking Behaviour: Problems and Prospects. Health Systems Development Programme. Manchester: University of Manchester; 2003. [Google Scholar]
- 13.Kahi HA, Abi Rizk GY, Hlais SA, Adib SM. Health-care-seeking behaviour among university students in Lebanon. East Mediterr Health J. 2012;18(6):598–606. doi: 10.26719/2012.18.6.598. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal G, Keshri K. Morbidity patterns and health care seeking behavior among older widows in India. PLoS One. 2014;9(4):e94295. doi: 10.1371/journal.pone.0094295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayden JA. Health Belief Model. Chapter 4. Introduction to Health Behavior Theory. Second ed. Burlington, MA: Jones & Bartlett Learning; 2013. pp. 31–44. [Google Scholar]
- 16.PHPR Illness Behavior and the Sick Role. 2016. [Accessed July 10, 2016]. Available at: www.phpr.purdue.edu/~phad/./illnessbehaviorandthesickrole.pdf.
- 17.Abdulraheem IS. Health needs assessment and determinants of health-seeking behaviour among elderly Nigerians: a household survey. Ann Afr Med. 2007;6(2):58–63. doi: 10.4103/1596-3519.55715. [DOI] [PubMed] [Google Scholar]
- 18.Emelumadu OF, Ukegbu AU, Ezeama NN, Kanu OO, Ifeadike CO, Onyeonoro UU. Socio-demographic determinants of maternal health-care service utilization among rural women in Anambra State, South East Nigeria. Ann Med Health Sci Res. 2014;4(3):374–382. doi: 10.4103/2141-9248.133463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iyalombe GBS, Iyalomhe SI. Health-seeking behavior of rural dwellers in Southern Nigeria: implications for health care professionals. Int J Trop Dis Health. 2012;2(2):62–71. [Google Scholar]
- 20.Mmari KN, Oseni O, Fatusi AO. STI treatment-seeking behaviors among youth in Nigeria: are there gender differences? Int Perspect Sex Reprod Health. 2010;36(2):72–79. doi: 10.1363/ipsrh.36.072.10. [DOI] [PubMed] [Google Scholar]
- 21.Okeibunor JC, Onyeneho NG, Chukwu JN, Post E. Where do tuberculosis patients go for treatment before reporting to DOTS clinics in southern Nigeria? Tanzan Health Res Bull. 2007;9(2):94–101. doi: 10.4314/thrb.v9i2.14310. [DOI] [PubMed] [Google Scholar]
- 22.Uzochukwu BSC, Onwujekwe OE. Socio-economic differences and health seeking behaviour for the diagnosis and treatment of malaria: a case study of four local government areas operating the Bamako initiative programme in south-east Nigeria. Int J Equity Health. 2004;3:6. doi: 10.1186/1475-9276-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aguocha BU, Ukpabi JO, Onyeonoro UU, Njoku P, Ukegbu AU. Pattern of diabetic mortality in a tertiary health facility in south-eastern Nigeria. Afr J Diabetes Med. 2013;21(1):14–16. [Google Scholar]
- 24.Allen AA, Adekola PO. Spatio-temporal factors and dynamics of population growth in Ondo State Nigeria 1970–2010. Int J Innovat Sci Res. 2015;17(1):43–50. [Google Scholar]
- 25.Ofem BI. A review of the criteria for defining urban areas in Nigeria. J Hum Ecol. 2012;37(3):167–171. [Google Scholar]
- 26.World Health Organisation . WHO STEPS Surveillance Manual. Geneva: World Health Organisation; 2008. [Accessed August 10 2011]. Available at: http://www.who.int/chp/steps/manual/en/index5.html. [Google Scholar]
- 27.World Health Organisation . Global Physical Activity Questionnaire (GPAQ): Analysis Guide. Surveillance and Population-Based Prevention. Geneva: Prevention of Non communicable Diseases Department World Health Organization; 2014. [Accessed April 12 2014]. Available at: www.who.int/chp/steps. [Google Scholar]
- 28.Ogah OS, Okpechi I, Chukwuonye II, et al. Blood pressure, prevalence of hypertension and hypertension related complications in Nigerian Africans; a review. World J Cardiol. 2012;4(12):327–340. doi: 10.4330/wjc.v4.i12.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iloh GUP, Amadi AN, Nwankwo BO, Ugwu VC. Obesity in adult Nigerians: a study of its pattern and common primary co-morbidities in a rural Mission General Hospital in Imo state, south-eastern Nigeria. Niger J Clin Pract. 2011;14(2):212–218. doi: 10.4103/1119-3077.84019. [DOI] [PubMed] [Google Scholar]
- 30.Adamu H, Makusidi AM, Liman HM, Isah MD, Jega MR, Chijioke A. Prevalence of obesity, diabetes type 2 and hypertension among a sampled population from Sokoto metropolis-Nigeria. Br J Med Med Res. 2014;4(10):2065–2080. [Google Scholar]
- 31.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191–199. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 32.Onah MN, Govender V. Out-of-pocket payments, health care access and utilisation in South-Eastern Nigeria: a gender perspective. PLoS One. 2014;9(4):e93887. doi: 10.1371/journal.pone.0093887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mamodesan O. Improving access to health care in rural communities by reorienting and integrating patent medicine sellers into primary health care service delivery in Nigeria. S Am J Pub Health. 2015;3(2):98–115. [Google Scholar]
- 34.Osamor PE. Health care seeking for hypertension in South West Nigeria. Med Sociol Online. 2011;6(1):54–69. [Google Scholar]
- 35.Oluwatayo IB. Health care services delivery system and households welfare status in urban south west Nigeria. J Hum Ecol. 2015;50(2):181–187. [Google Scholar]
- 36.Onwujekwe O, Hanson K, Uzochukwu B, Ezeoke O, Soludo E, Dike N. Geographic-inequities in provision and utilization of malaria treatment services in south east Nigeria: diagnosis, providers and drugs. Health Policy. 2010;94:144–149. doi: 10.1016/j.healthpol.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 37.Onyeonoro UU, Oluoha C, Borke O, Nwamoh UN. A rapid assessment of youth friendly reproductive health services in Abia State; its implications on universal health coverage; A Conference Paper Presented at Association of Public Health Physicians of Nigeria 32nd National Scientific & Annual General Meeting; Abuja. 14th–18th March, 2016. [Google Scholar]
- 38.Uzochukwu BSC, Ughasoro MD, Etiaba E, Okwuosa C, Envuladu E, Onwujekwe OE. Health care financing in Nigeria: implications for achieving universal health coverage. Niger J Clin Pract. 2015;18(4):437–444. doi: 10.4103/1119-3077.154196. [DOI] [PubMed] [Google Scholar]
- 39.Goodman C, Brieger W, Unwin A, Mills A, Meek S, Greer G. Medicine sellers and malaria treatment in sub Saharan Africa: what do they do and how can their practice be improved? Am J Trop Med Hyg. 2007;77(6 suppl):203–218. [PMC free article] [PubMed] [Google Scholar]
- 40.Beyeler N, Liu J, Sieverding M. A systematic review of the role of proprietary and patent medicine vendors in health care provision in Nigeria. PLoS One. 2015;10(1):e0117165. doi: 10.1371/journal.pone.0117165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okonkwo AD, Okonkwo UP. Patent medicine vendors, community pharmacists and STI management in Abuja, Nigeria. Afr Health Sci. 2010;10(3):253–265. [PMC free article] [PubMed] [Google Scholar]


