Abstract
Introduction
Serum vitamin D concentration is a major contributing factor for increasing the risk of fall and fall-related injuries in older adults. However, when prescribed and supplemented for these populations, the outcomes are controversial, and in several cases no improvement has been reported in reducing the risk of recurrent falls. This study aimed to examine the association between serum vitamin D concentration and recurrent falls in Iranian older adults.
Methods
This cohort study was conducted in the emergency departments of two university hospitals. A cohort of 82 elderly participants aged over 60 and suffered from an unintentional episode of falling was evaluated six months after their first ED visit. A structured, self-administered checklist was developed to obtain the participants’ demographic and clinical information. Participants also were asked about any recurrent fall experience during follow-up.
Results
The mean (SD) age of the study population was 75 (8). Over half of the participants were male (57.3%). The mean (median) serum 25-hydroxyvitamin D (25 (OH)D) concentration was 38 (34) ng/ml. Mean serum 25(OH)D levels varied slightly between gender groups (p=0.450). An inverse but insignificant association was found between the age of participants and their serum 25(OH)D levels (r=−0.03, p=0.7). A small but insignificant association also was found between the mean serum 25(OH)D level and the number of recurrent falls in elderly patients irrespective of their age, gender, or physical activity groups (OR=1.008, p=0.992).
Conclusion
In contrast to previous studies, no significant association of serum 25(OH)D concentration was found with recurrent falls in Iranian older adults.
Keywords: 25-hydroxyvitamin D, falls, Vitamin D insufficiency, Iran, Elderly
1. Introduction
Falls are the leading cause of injury and deaths among older adults worldwide with an estimated 424,000 cases reported each year (1). Over 30% of those aged over 65 or older and 40–50% of those over 80 currently are treated for fall-related injuries (2). Recurrent falls among older adults have a significant financial, social, psychological, and health-related burden on society, particularly on the health care system. Since falls and fall-related injuries result in the loss of over 17 million disability-adjusted life years (DALYs), they are considered to be a major public health challenge across the world that calls for global action. In this context, the rapidly increasing number of older adults and the associated risk of fall-related injuries underlines ongoing concerns about the quality of life, costs of care, and demands for support services and preventive programs for vulnerable populations. Serum Vitamin D insufficiency has been implemented as a major risk factor for osteoporosis, muscle weakness (3), falls(2, 4), fractures(5, 6) and even mortality (7–9). The association between vitamin D insufficiency and the risk of fracture and injuries has been estimated in several studies (5, 6, 10, 11). Most of the studies have investigated the effect of serum 25-hydroxyvitamin D (25(OH)D) concentration, which is the best indicator of vitamin D status, on bone mineral density (BMD) changes (6, 12, 13). Therefore, it has been suggested that vitamin D is a major determinant of bone health. It also has been indicated that low 25(OH)D levelshave been associated with low BMD in older white adults (12, 14). In this regard, further investigations indicated a positive association between serum 25(OH)D and BMD of the hip(5, 6, 11)and spine in men. Some other studies have suggested that vitamin D has a protective effect on fractures by improving muscle functions and reduced risk of falling (2–4, 8). In these studies, low 25(OH)D was found to be associated with poor grip strength, an indicator of muscle strength, balance, and increased risk of mortality in elderly patients. Despite its well-documented protective effects, serum 25(OH)D concentration is likely to be one of the most globally-considered contributing factors to BMD changes, muscle strength, fractures, and falls. Serum 25(OH)D supplementation has been prescribed repeatedly as a preventive drug for older people, yet there are surprising small number of well-documented randomized, controlled trials measuring its efficacy and potential to reduce the risk of fractures and falls (15). Prescription of vitamin D supplementation for older people is based on clinical experience rather than well documented, randomized trials that involve an extensive population with different outcomes (15). While a great body of the literature suggests vitamin D supplementation as the major contributing factors for reducing the risk of falls and fractures in elderly people, it is unclear whether its efficacy and potential performance leads to better results. Therefore, further efforts are needed to investigate the effect of serum 25(OH)D concentration on the risk of falls in older populations. Recent data have failed to find any protective effect of 25(OH)D on the risk or rates of falling in older people, yet the association between 25(OH)D concentration level and the risk of falling in older adults has been a topic of heavy debate among healthcare professionals, and, therefore, more investigations are needed to provide evidence of how 25(OH)D status is associated with the risk of recurrent falls. In an attempt to address these challenges, the present study aimed to conduct a preliminary investigation of the association between serum 25(OH)D levels and the risk of recurrent falls in the elderly Iranian population.
2. Material and Methods
2.1. Study Setting and Participants
This cohort study was conducted in the emergency departments (EDs) of Rasoul Akram and Sina Hospitals during March 2012–January 2013. A cohort of elderly participants over 60 who suffered from an unintentional episode of falling was evaluated six months after of their first ED visit. Of all 120 patients invited to participate in the study, 82 ultimately remained to the end of the study. Exclusion criteria were the use of vitamin D supplements, anti-seizure medications, or glucocorticoids.
2.2. Data collection and Follow-up
A structured, self-administered checklist was developed to obtain the participants’ demographic and clinical information. The questionnaire included demographic information (age, gender, level of education, marital status), past medical history, and serum 25(OH)D concentration of included participants at the time of hospitalization. This checklist was completed during admission and in a six-month of follow up through telephone calls to the patients, their family, or caregivers who were aware of the patients’ conditions. We also asked about any recurrent fall experience during the six-month follow-up. Those who reported recurrent falls were asked about the frequency of their falls.
2.3. 25(OH)D Analysis and Statistical analysis
A valid serum 25(OH)D sample was obtained from all of the patients who participated in the study. Non-fasting blood samples were collected from participants during their first visit to the clinic. The serum concentration of 25(OH)D was measured by separating the serum from 5 cm3of clotted blood taken from the participants. All samples were stored at −20°C and then transferred to the Reference Laboratory. The serum 25(OH)D concentration was measured using the Enzyme-Linked Immunosorbent Assay (ELISA) method. Data analysis was performed using Stata version 12 (Stata Corp., College Station, TX). Descriptive statistics (mean, median, SD and range) were used to present the overall characteristics of the participants. Spearman’s regression coefficient was used to measure the associations between the quantitative variables. In order to compare the mean serum 25(OH)D concentration between different categorical variables, the Mann-Whitney U and Kruskal-Wallis tests were used.
2.4. Ethics Approval and Informed Consent
All participants gave written informed consent. Ethical approval was granted by the Iran University of Medical Sciences’ Research Ethics Committee.
3. Results
3.1. Characteristics of Participants
The mean (SD) age of the study population was 75 (8). Over half of the participants were male (57.3%), and about 80% lived in private homes. Table 1 presents the participants’ characteristics according to the three levels of serum 25(OH)D studied.
Table 1.
Descriptive Characteristics of Participants, Aged 60 and Older Living in the Community According to Serum 25(OH)D Level
| Variables | Characteristics | n (%) | 25(OH)D; Mean (median) | <30 ng/ml (%) | 30–100 ng/ml (%) | 100–150 ng/ml (%) |
|---|---|---|---|---|---|---|
| Gender | Male | 47 (57.3) | 39.1 (36) | 16 (45.7) | 30(66.7) | 1 (50) |
| Female | 35 (42.7) | 36.8 (28) | 19 (54.3) | 15 (33.3) | 1 (50) | |
| Marital state | Married | 52 (63.4) | 38.5 (36) | 21 (60) | 30 (66.7) | 1 (50) |
| Widow | 26 (31.7) | 37.3(39) | 13 (37.1) | 12 (26.7) | 1(50) | |
| Single | 4 (4.9) | 37.7 (40.5) | 1 (2.9) | 3 (6.7) | 0 (0) | |
| Residence | Private home | 65 (79.3) | 37.06 (34) | 28 (80) | 36 (80) | 1 (50) |
| Children’s home | 17 (20.7) | 42.2 (34) | 7 (20) | 9 (20) | 1 (50) | |
| Age (year) | 60–70 | 29 (35.4) | 36.3 (33) | 14 (40) | 14 (31.1) | 1 (50) |
| 71–80 | 34 (41.5) | 43.4 (37) | 14 (40) | 19 (42.2) | 1 (50) | |
| 81–90 | 16(19.5) | 34.2 (34.5) | 4 (11.4) | 12 (26.7) | 0 (0) | |
| >90 | 3(3.7) | 15.3 (10) | 3 (8.6) | 0 (0) | 0 (0) | |
| Past medical history | DM | 16 (19.5) | 41.3(30) | 8 (22.9) | 7 (15.6) | 1 (50) |
| HTN | 23 (28.1) | 36.5 (36) | 8 (22.9) | 14 (31.1) | 1 (50) | |
| HLP | 13 (15.8) | 34 (36) | 5 (14.3) | 8 (17.8) | 0 | |
| CAD | 18 (21.9) | 39.1 (29) | 10 (28.6) | 8 (17.8) | 0 | |
| CVA | 12 (14.6) | 39.8 (36.5) | 4 (11.4) | 8 (17.8) | 0 | |
| BMI (kg/M2) | <20 | 8 (9.8) | 42.7 (29) | 4 (11.4) | 3 (6.7) | 1 (50) |
| 20–24.9 | 38(46.3) | 37.7 (36) | 14 (40) | 23 (51.1) | 1 (50) | |
| 25–29.9 | 31(37.8) | 38(33) | 15 (42.9) | 16 (35.6) | 0 (0) | |
| >30 | 5 (6.1) | 33.6 (31) | 2 (5.7) | 3 (6.7) | 0 (0) | |
| Physical activity | <80 | 75(91.5) | 36.2 (32) | 39 (86.7) | 1 (50) | |
| >80 | 7 (8.5) | 58.8 (42) | 6 (13.3) | 1 (50) | ||
| Muscle weakness | Yes | 6 (7.3) | 34.1 (32) | 2 (5.7) | 4 (8.9) | 0 (0) |
| No | 76 (92.7) | 38.4 (34.5) | 33 (94.3) | 41 (91.1) | 2 (100) | |
| Dynamic balance | Good | 39 (47.6) | 36.7 (36) | 16 (45.7) | 23 (51.1) | 0 (0) |
| Poor, not completed | 43 (52.4) | 39.3 (33) | 19 (54.3) | 22 (48.9) | 2 (100) |
3.2. Distribution of Serum 25(OH)D Concentration
The mean (median) serum 25(OH)D concentration was 38 (34) ng/ml. Mean serum 25(OH)D levels varied little according to gender groups, men had higher levels of 25(OH)D rather than women (39.1 vs. 36.8, respectively, p=0.450). In addition, mean serum 25(OH)D levels differed between the age groups, ranging from 15.3 ng/ml in those aged over 90 to 43.4 ng/ml in those aged 71–80. According to this finding, an inverse, but insignificant, association was found between the age of participants and their serum 25(OH)D levels (r=−0.03, p=0.7). Table 1 indicates that the mean serum 25(OH)D levels decreased according to BMI categories (from 42.7 to 33.6 ng/ml, P=0.986). Mean serum 25(OH)D level was significantly higher in the group with physical activity of more than 80 min per week (P=0.03). However, the mean serum 25(OH)D level was found to have no significant association with muscle weakness(p=0.979) or dynamic balance scores(p=0.90).
3.3. The Effect of Serum 25(OH)D Concentration on Falls
Figure 1 indicates the distribution of serum 25(OH)D according to recurrent falls and gender categories. According to this figure, the median serum 25(OH)D concentration was higher in men than in women. Besides, the median serum 25(OH)D concentration was decreased insignificantly in line with the increasing number of recurrent falls. However, in women, the median of the serum 25(OH)D concentration followed a different pattern, in which women who experienced recurrent falls had higher scores of serum 25(OH) than others (p=0.643). According to these findings, a small but insignificant association was found between the mean serum 25(OH)D level and the number of recurrent falls in elderly patients irrespective of their age, gender, or physical activity groups (OR=1.008, p=0.992).
Figure 1.
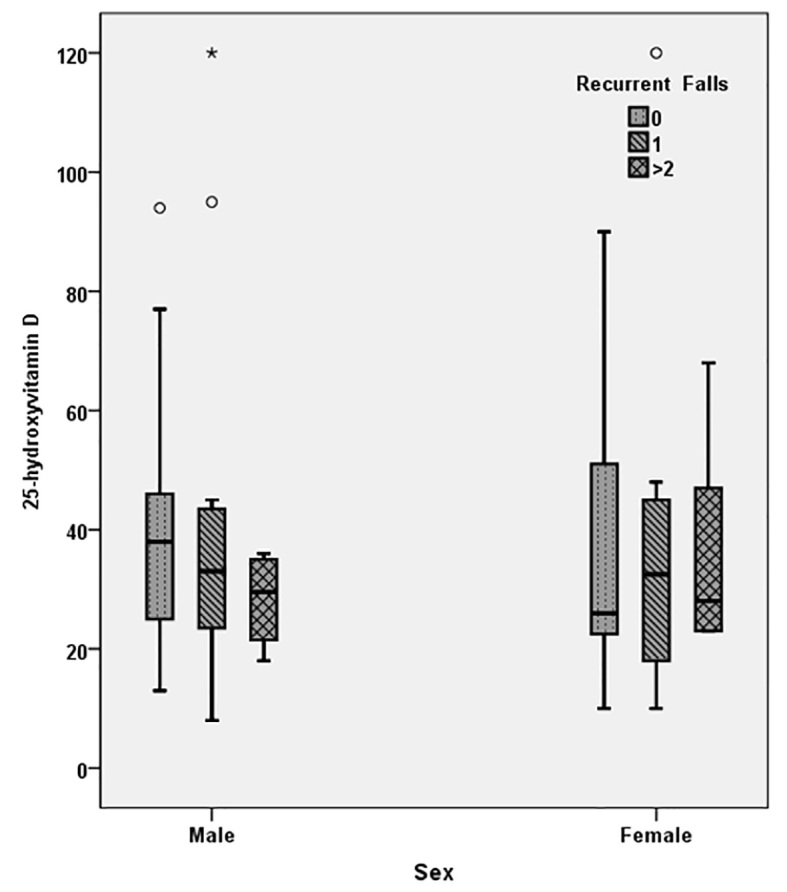
Distribution of Serum 25(OH)D according to recurrent falls and gender categories in participants aged 60 and older in the community
4. Discussion
In this prospective cohort study of elderly people that were treated in emergency rooms for injuries from falls, no significant association was observed between their serum 25(OH)D concentration and recurrent falls. In addition, mean serum 25(OH)D concentration was not associated with muscle weakness and balance in older adults. In this study, no significant association of 25(OH)D was found with incidence of one or more recurrent falls. In contrast to previous reports, our findings did not support the argument that vitamin D concentration reduces the risk of recurrent falls in elderly people. Similar to our findings, in a survey by Faulkner et al., the relationship between serum concentration of vitamin D metabolites and falls in older women in the United States was examined, and it was reported that the risk of falling only decreased with high serum 1,25(OH)2D3 concentration, whereas higher 25(OH)D level was not associated with lower risk (16). Serum 1,25(OH)2D3 concentration was not assessed in participants in our study because of laboratory limitations, but our findings confirmed the second result of this study in that is showed that there was no association between 25(OH) D levels and falls. In a meta-analysis of randomized controlled trials, the efficacy of the administration of vitamin D and calcium supplements in elderly people to reduce the frequency of falls was examined, but the results found no efficacy (10). The findings of previous studies have suggested that low vitamin D status is associated with increased risk of falling and fractures. Therefore, vitamin D supplementation has been implemented as a strategy in increasing BMD and reducing the risk of fractures or falls in older people. Vitamin D concentration has been suggested repeatedly to be the contributing factor for BMD changes, falls, fractures, and physical performance in older people, but emerging evidence highlights ongoing debates on the protective effect of vitamin D concentration on falls and fractures. While prescribing vitamin D for preventing unfavorable outcomes of bone resorption and turnover is based on clinical practice and cohort studies, there is now evidence that failed to identify any protective effect of vitamin D supplementation on the risk or rate of falling in older people (both in healthcare facilities or hospitals and in the community) (15, 17, 18). Our findings also indicated no significant association of 25(OH)D concentration and muscle weakness in older adults. This result was consistent with the findings of a systematic review and meta-analysis that examined the effect of vitamin D concentration on muscle strength in adults (19). According to this evidence, vitamin D supplementation showed no significant effect on grip strength, knee flexion strength, or knee extension strength in adults with baseline 25(OH)D >25 nmol/L. These results provided further evidence that the function, metabolism, and absorption of vitamin D may differ among individuals and even across diverse populations (15). However, limited early investigations have suggested an increase in proximal muscle strength in adults with vitamin D deficiency (3). In this context, universal recommendations on the use of vitamin D supplementation to improve muscle strength and physical performance of older adults’ require further evidence. Our study was limited in several aspects. First, the design of our study did not allow us to investigate the causality effect of vitamin D and recurrent falls. Also, we did not consider important covariates, including body mass index, education, smoking, use of alcohol, and health status when we analyzed the potential associations between serum vitamin D concentration and recurrent falls in older people. In addition, a single baseline measurement of serum vitamin D, was used to categorize the participants, and this could have led to misclassification of the participants, because single baseline measurements may not have reflected their long-term biochemical status. We excluded those subjects who took vitamin D supplements during the six-month follow-up. The efficacy of vitamin D supplements in reducing recurrent falls was not investigated in our study. Despite these limitations, this study has several unique strengths. First, this is the first population-based study to examine the incidence of recurrent fractures with serum vitamin D concentration in the Iranian population. Therefore, these findings provide further evidence of the effect of vitamin D on recurrent falls in people with diverse ethnic backgrounds. Second, this study used direct serum measures of vitamin D instead of other indirect measures, including questionnaire-based scales or food frequency intakes of vitamin D-rich foods. In summary, our study findings failed to support the argument that vitamin D concentration is associated with the reduced risk of falling in older adults. No significant association of vitamin D was found with incidence of recurrent falls, muscle activity, and balance.
5. Conclusions
The association between vitamin D insufficiency and the risk of fracture and injuries has been investigated repeatedly, but the results remain controversial across different populations. Therefore, this study aimed to investigate the protective role of vitamin D concentration against falls in the elderly Iranian population. By using serum vitamin D concentration as a direct measure of vitamin D, this study failed to support the argument that vitamin D concentration is associated with the reduced risk of falling in older adults. According to our findings, no significant association was observed between serum vitamin D concentration and recurrent falls, muscle activity, and balance. Our findings provided further evidence that the function, metabolism, and absorption of vitamin D may differ among individuals and even across diverse populations. Yet, the results are still incomplete, and further trials are needed to reach conclusive decisions.
Acknowledgments
This work supported in part by the Iran University of Medical Sciences with research grant number 18050. The authors thank the staff of the Deputy for Research at the Iran University of Medical Sciences for their financial support.
Footnotes
iThenticate screening: March 02, 2016, English editing: May 19, 2016, Quality control: July 04, 2016
Conflict of Interest:
There is no conflict of interest to be declared.
Authors’ contributions:
All authors contributed to this project and article equally. All authors read and approved the final manuscript.
References
- 1.World Health organization. Falls. World Health Organization; 2012. [Google Scholar]
- 2.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of vitamin D on falls: a meta-analysis. JAMA. 2004;291(16):1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 3.Barker T, Henriksen VT, Martins TB, Hill HR, Kjeldsberg CR, Schneider ED, et al. Higher serum 25-hydroxyvitamin D concentrations associate with a faster recovery of skeletal muscle strength after muscular injury. Nutrients. 2013;5(4):1253–75. doi: 10.3390/nu5041253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murad MH, Elamin KB, Abu Elnour NO, Elamin MB, Alkatib AA, Fatourechi MM, et al. Clinical review: The effect of vitamin D on falls: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96(10):2997–3006. doi: 10.1210/jc.2011-1193. [DOI] [PubMed] [Google Scholar]
- 5.Holvik K, Ahmed LA, Forsmo S, Gjesdal CG, Grimnes G, Samuelsen SO, et al. Low serum levels of 25-hydroxyvitamin D predict hip fracture in the elderly: a NOREPOS study. J Clin Endocrinol Metab. 2013;98(8):3341–50. doi: 10.1210/jc.2013-1468. [DOI] [PubMed] [Google Scholar]
- 6.Steingrimsdottir L, Halldorsson T, Siggeirsdottir K, Cotch MF, Einarsdottir BO, Eiriksdottir G, et al. Hip fractures and bone mineral density in the elderly--importance of serum 25-hydroxyvitamin D. PloS One. 2014;9(3) doi: 10.1371/journal.pone.0091122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Durup D, Jørgensen HL, Christensen J, Schwarz P, Heegaard AM, Lind B. A reverse J-shaped association of all-cause mortality with serum 25-hydroxyvitamin D in general practice: the CopD study. J Clin Endocrinol Metab. 2012;97(8):1–9. doi: 10.1210/jc.2012-1176. [DOI] [PubMed] [Google Scholar]
- 8.Hirani V, Cumming RG, Naganathan V, Blyth F, Le Couteur DG, Handelsman DJ, et al. Associations Between Serum 25-Hydroxyvitamin D Concentrations and Multiple Health Conditions, Physical Performance Measures, Disability, and All Cause Mortality: The Concord Health and Ageing in Men Project. J Am Geriatr Soc. 2014;62(3):417–25. doi: 10.1111/jgs.12693. [DOI] [PubMed] [Google Scholar]
- 9.Chowdhury R, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, et al. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ. 2014;348(g1903):2–13. doi: 10.1136/bmj.g1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354(7):669–83. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 11.Wang Xg, Yang B, Wang Yh, Cui Ly, Luo Jp. Serum Levels of 25-hydroxyvitamin D and Functional Outcome in Older Patients with Hip Fracture. J Arthroplasty. 2015;30(5):891–4. doi: 10.1016/j.arth.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Hannan MT, Litman HJ, Araujo AB, McLennan CE, McLean RR, McKinlay JB, et al. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J Clin Endocrinol Metab. 2013;93(1):40–6. doi: 10.1210/jc.2007-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hwang YC, Ahn HY, Jeong IK, Ahn KJ, Chung HY. Optimal serum concentration of 25-hydroxyvitamin D for bone health in older Korean adults. Calcif Tissue Int. 2013;92(1):68–74. doi: 10.1007/s00223-012-9669-3. [DOI] [PubMed] [Google Scholar]
- 14.Lips P, Duong TU, Oleksik A, Black D, Cummings S, Cox D, et al. A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trial. J Clin Endocrinol Metab. 2001;86(3):1212–21. doi: 10.1210/jcem.86.3.7327. [DOI] [PubMed] [Google Scholar]
- 15.Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JPA. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348(g2035):2–19. doi: 10.1136/bmj.g2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faulkner KA, Cauley JA, Zmuda JM, Landsittel DP, Newman AB, Studenski SA, et al. Higher 1, 25-dihydroxyvitamin D3 concentrations associated with lower fall rates in older community-dwelling women. Osteoporos Int. 2006;17(9):1318–28. doi: 10.1007/s00198-006-0071-8. [DOI] [PubMed] [Google Scholar]
- 17.Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD005465.pub3. [DOI] [PubMed] [Google Scholar]
- 18.Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2(CD007146) doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Stockton KA, Mengersen K, Paratz JD, Kandiah D, Bennell KL. Effect of vitamin D supplementation on muscle strength: a systematic review and meta-analysis. Osteoporos Int. 2011;22(3):859–71. doi: 10.1007/s00198-010-1407-y. [DOI] [PubMed] [Google Scholar]


