Abstract
Background and objectives
The relationship between HDL cholesterol and all-cause mortality in patients with kidney disease is not clear. We sought to characterize the relationship of HDL cholesterol and risk of death and examine the association by eGFR levels.
Design, setting, participants, & measurements
We built a cohort of 1,764,986 men who were United States veterans with at least one eGFR between October of 2003 and September of 2004 and followed them until September of 2013 or death.
Results
Patients with low HDL cholesterol and low eGFR had a higher burden of comorbid illnesses. Over a median of 9.1 years (interquartile range, 7.7–9.4 years), 26,247 (40.1%), 109,222 (32.3%), 152,625 (29.2%), 113,785 (28.5%), and 139,803 (31.8%) participants with HDL cholesterol ≤25, >25 to <34, ≥34 to ≤42, >42 to <50, and ≥50 mg/dl died. In adjusted survival models, compared with the referent group of patients with low HDL cholesterol (≤25 mg/dl), intermediate HDL cholesterol levels (>25 to <34, ≥34 to ≤42, and >42 to <50 mg/dl) were associated with lower risk of death across all levels of eGFR. The lower risk was partially abrogated in those with high HDL cholesterol (≥50 mg/dl), and the risk of death was similar to the referent category among those with eGFR<30 or ≥90 ml/min per 1.73 m2. Analysis by HDL cholesterol deciles and spline analyses suggest that the relationship between HDL cholesterol and death follows a U-shaped curve. There was a significant interaction between eGFR and HDL cholesterol in that lower eGFR attenuated the salutary association of HDL cholesterol and risk of death (P for interaction <0.01). Presence of coronary artery disease attenuated the lower risk of high HDL cholesterol and all-cause mortality in those with eGFR≥60 ml/min per 1.73 m2 (P for interaction <0.05).
Conclusions
Our results show a U-shaped relationship between HDL cholesterol and risk of all-cause mortality across all eGFR categories. The risk is modified by eGFR and cardiovascular disease.
Keywords: hypercholesterolemia; mortality risk; chronic kidney disease; lipids; mortality; Epidemiology and outcomes; Cardiovascular Diseases; Cholesterol, HDL; coronary artery disease; Humans; United States; Veterans
Introduction
Few studies have evaluated the association between HDL cholesterol (HDL-C) and mortality in patients with kidney disease. Results from numerous experimental and translational studies suggest that, in addition to a relative quantitative HDL-C deficiency, HDL-C antioxidant, anti–inflammatory, and antiatherogenic properties are qualitatively impaired in patients with ESRD on dialysis (1,2). HDL-C obtained from patients with CKD promoted endothelial superoxide production, reduced nitric oxide bioavailability, and increased arterial BP (3). Reduced HDL-C levels or altered functions resulted in reduced or impaired cellular cholesterol efflux and may partly explain the increased cardiovascular disease burden and excess mortality risk in patients with CKD (4).
Zewinger et al. (5) evaluated the relationship of HDL-C and mortality in a cohort of 3307 patients undergoing coronary angioplasty and found that higher HDL-C was not associated with reduced mortality in patients with eGFR<60 ml/min per 1.73 m2. The study cohort was comprised of referred patients with a large burden of coronary artery disease (CAD; 77.9%). Lamprea-Montealegre et al. (6) evaluated the association between plasma lipids—and of relevance here, HDL-C—and subclinical atherosclerosis measured by the common carotid intima-media thickness in a cross-sectional study involving 6752 participants. The investigators found that higher HDL-C was associated with lower intima-media thickness and that this association was more pronounced in patients with eGFR<60 ml/min per 1.73 m2 (6).
Observations from clinical literature are inconsistent largely because of the short duration of follow-up and often, very small sample size (7–9). Whether higher HDL-C is associated with reduced risk of mortality in patients with CKD and whether eGFR modifies the association of HDL-C and risk of death are not clear. Furthermore, the cardiovascular disease burden in people with kidney disease is significant; whether the presence of cardiovascular disease modifies the relationship of HDL-C and risk of all-cause mortality has not been examined in large–scale epidemiologic studies spanning a sufficiently prolonged duration of time (10,11).
Here, we built a cohort of 1,764,986 men who were United States veterans and followed them over a median of 9.1 years (interquartile range [IQR], 7.7–9.4 years) to examine the association of HDL-C and all-cause mortality on the basis of eGFR levels, determine whether eGFR modifies this association, and examine whether the presence of cardiovascular disease modifies the relationship between HDL-C and risk of death.
Materials and Methods
Patients
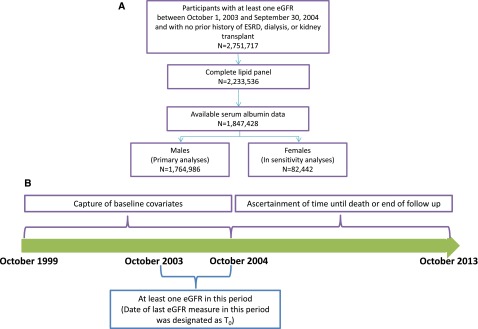
Using administrative data from the US Department of Veterans Affairs (VA), we identified users of the VA Healthcare System who had at least one eGFR value between October 1, 2003 and September 30, 2004 with no prior history of ESRD, dialysis, or kidney transplant (n=2,751,717); the date of last eGFR during this period was designated as time 0 (T0). Cohort participants were additionally selected for having a complete lipid panel between October 1, 1999 and T0 (n=2,233,536), having serum albumin data (n=1,847,428), and being men (n=1,764,986). The study was approved by the Institutional Review Board of the VA St. Louis Health Care System. A flow chart and timeline for cohort selection are presented in Figure 1.
Figure 1.
Cohort construction. (A) Flow diagram of cohort assembly. (B) Timeline of cohort selection.
Data Sources
We used the Department of VA databases, including outpatient and inpatient medical Statistical Analysis System (SAS) datasets, which include utilization information consisting of all patient encounters within the VA system, to ascertain detailed patient demographic characteristics and comorbidity data on the basis of Current Procedural Terminology (CPT) codes and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic and procedure codes associated with inpatient and outpatient encounters (12–15). The VA Managerial Cost Accounting System Laboratory Results, a comprehensive dataset that includes VA-wide results for select laboratory tests obtained in the clinical setting, provided data on outpatient and inpatient serum creatinine, HDL-C, LDL cholesterol, triglycerides, serum albumin, and microalbumin-to-creatinine ratio (12,13,16). The VA Corporate Data Warehouse (CDW) Production Outpatient Pharmacy domain provided information on statins, angiotensin–converting enzyme inhibitors (ACEIs), and angiotensin receptor blockers (ARBs). The CDW Vital Signs domain provided data on height and weight, which was used to calculate body mass index (BMI) and body surface area. The VA Vital Status and Beneficiary Identification Records Locator Subsystem files provided demographic characteristics and death follow-up through September 30, 2013 (12,13). The CDW Laboratory Chemistry domain provided data on C-reactive protein (CRP). Data were assessed from October 1, 1999 to September 30, 2013.
Primary Predictor Variable.
The primary predictor variable for all survival analyses was HDL-C level. The value for HDL-C was taken as the outpatient HDL-C value before and most proximal to T0. HDL-C was then categorized using the following criteria (as outlined in the work by Zewinger et al. [5]): ≤25, >25 to <34, ≥34 to ≤42, >42 to <50, and ≥50 mg/dl. For additional analysis of the relationship of HDL-C and risk of death, values were also categorized into deciles.
Outcomes.
The primary outcome in survival analyses consisted of time until death, with follow-up from time of cohort entry (T0) until September 30, 2013.
Covariates
Baseline covariates were ascertained from October 1, 1999 until cohort entry (T0). Covariates included eGFR, age, race, diabetes mellitus, hypertension, CAD, congestive heart failure (CHF), peripheral artery disease, cancer, cerebrovascular disease, chronic lung disease, hepatitis C, HIV, dementia, LDL cholesterol, triglycerides, serum albumin, ACEI/ARB use, statin use, BMI, body surface area, microalbumin-to-creatinine ratio, and CRP. Race/ethnicity was categorized as white, black, or other (Latino, Asian, Native American, or other racial/ethnic minority groups). T0 eGFR was categorized into groups as >90, 90 to <60, 60 to <45, 45 to <30, and 30 to <15 ml/min per 1.73 m2. To minimize residual confounding, we also controlled for eGFR within each eGFR category as a time-varying covariate. Dialysis, kidney transplant status, and statin use were also assessed as time varying. Microalbumin-to-creatinine ratio was categorized into groups of <20, 20 to <300, and ≥300 mg/g. BMI was categorized into underweight, normal weight, overweight, and obese categories. Body surface area was calculated using the DuBois and DuBois equation (17). Patients were considered ACEI or ARB users if the total days of prescription during the period before T0 was ≥90. Covariates were treated as continuous variables where appropriate and unless otherwise indicated. Comorbidities were assigned on the basis of relevant ICD-9-CM diagnostic and procedures codes and CPT codes in the VA Medical SAS datasets (18–22).
Statistical Analyses
Cox proportional hazard regression models were used in the assessment of survival in the overall cohort and within each eGFR category. The proportional hazard assumption was assessed through use of log–negative log plots and met. Multiple models were built to assess the relation between HDL-C level and the outcome while sequentially controlling for different covariates. A bar chart showing hazard ratios of the risk of all-cause mortality by HDL-C levels grouped by eGFR category, with error bars representing 95% confidence intervals, is presented. Quadratic spline analyses were performed in adjusted Cox proportional hazard regression models to assess the relationship between HDL and risk of all-cause mortality within each eGFR category and in the overall cohort (20). Knots were placed at quintiles. To account for potential highly influential values, those with HDL-C values below the 1st percentile and above the 99th percentile within each eGFR strata were excluded. For all splines, an HDL-C value of 41 mg/dl, the median value within the overall cohort, was used as the reference. To assess potential effect modification of HDL-C level and risk of death by eGFR category, an interaction term between the two variables was added to a nonstratified model. The P value for the type 3 test of the overall effect of the interaction is presented. For assessment of potential effect modification by cardiovascular disease, interaction terms between HDL-C level and CAD, CHF, and a three–level cardiovascular disease variable (defined as neither CAD nor CHF, either CAD or CHF, and both CAD and CHF) were added to separate eGFR stratified models. In survival analyses, a 95% confidence interval of a hazard ratio that does not include unity was considered statistically significant. In all analyses, a P value of ≤0.05 was considered statistically significant. Missing data were not imputed. All analyses were performed and all graphs were made using SAS Enterprise Guide, version 6.1 and SAS 9.2 (SAS Institute Inc., Cary, NC).
Sensitivity Analyses
We evaluated the consistency of study findings by undertaking a number of sensitivity analyses, where we (1) conducted analyses in a separate cohort of women (n=82,422), (2) examined the association in a subcohort where data on microalbumin-to-creatinine ratio were available (n=134,321), (3) additionally controlled for body surface area, (4) additionally controlled for CRP in a subcohort where data were available (n=65,112), and (5) also used different cutoff points to define HDL-C categories, where HDL-C was categorized into four groups: <30, ≥30 to <40, ≥40 to <60, and ≥60 mg/dl (data not shown).
Results
The demographic and clinical characteristics of the overall cohort (n=1,764,986) and according to HDL-C levels are presented in Table 1; patients with lower HDL-C had lower eGFR and higher burden of comorbid diseases. Characteristics according to eGFR category are presented in Supplemental Table 1; patients with low eGFR had lower HDL-C and higher burden of comorbid illnesses. Among cohort participants, 1,456,328 had more than one HDL-C measure at or before T0, with a median number of measures of 4 (IQR, 3–7) and a mean (SD) coefficient of variation of 11.7% (7.0).
Table 1.
Demographic and clinical characteristics according to HDL cholesterol levels
| Characteristic | Overall | HDL-C≤25 mg/dl | HDL-C>25 to <34 mg/dl | HDL-C≥34 to ≤42 mg/dl | HDL-C>42 to <50 mg/dl | HDL-C≥50 mg/dl |
|---|---|---|---|---|---|---|
| No. (%) | 1,764,986 | 65,431 (3.7) | 338,327 (19.2) | 522,373 (29.6) | 399,303 (22.6) | 439,552 (24.9) |
| Median HDL-C (IQR), mg/dl | 41.0 (34.0–49.5) | 23.0 (21.6–25.0) | 30.0 (28.1–32.0) | 37.9 (36.0–39.5) | 45.0 (43.0–47.0) | 57.0 (53.0–65.0) |
| Race (%) | ||||||
| White | 1,503,312 (85.2) | 58,598 (89.6) | 299,469 (88.5) | 452,934 (86.7) | 338,073 (84.7) | 354,238 (80.6) |
| Black | 224,785 (12.7) | 5626 (8.6) | 31,649 (9.4) | 58,008 (11.1) | 52,670 (13.2) | 76,832 (17.5) |
| Other | 36,889 (2.1) | 1207 (1.8) | 7209 (2.1) | 11,431 (2.2) | 8560 (2.1) | 8482 (1.9) |
| Median age (IQR), yr | 64.1 (56.1–72.6) | 61.8 (55.1–71.4) | 63.1 (55.7–72.0) | 64.0 (56.1–72.4) | 64.8 (56.3–72.9) | 65.0 (56.3–73.1) |
| Cancer (%) | 248,058 (14.1) | 9567 (14.6) | 45,499 (13.5) | 71,324 (13.7) | 55,676 (13.9) | 65,992 (15.0) |
| Cerebrovascular accident (%) | 11,633 (0.7) | 613 (0.9) | 2704 (0.8) | 3643 (0.7) | 2412 (0.6) | 2261 (0.5) |
| Coronary artery disease (%) | 576,589 (32.7) | 28,484 (43.5) | 132,693 (39.2) | 181,056 (34.7) | 122,458 (30.7) | 111,898 (25.5) |
| Congestive heart failure (%) | 146,203 (8.3) | 10,055 (15.4) | 37,141 (11.0) | 44,195 (8.5) | 28,235 (7.1) | 26,577 (6.1) |
| Chronic lung disease (%) | 384,971 (21.8) | 15,966 (24.4) | 73,546 (21.7) | 107,299 (20.5) | 82,971 (20.8) | 105,189 (23.9) |
| Diabetes mellitus (%) | 557,235 (31.6) | 31,039 (47.4) | 138,205 (40.9) | 179,777 (34.4) | 113,751 (28.5) | 94,463 (21.5) |
| Dementia (%) | 61,308 (3.5) | 2438 (3.7) | 11,563 (3.4) | 17,766 (3.4) | 13,831 (3.5) | 15,710 (3.6) |
| HIV (%) | 119,926 (6.8) | 6277 (9.6) | 26,114 (7.7) | 35,227 (6.7) | 25,030 (6.3) | 27,278 (6.2) |
| Hypertension (%) | 1,278,661 (72.5) | 50,986 (77.9) | 258,782 (76.5) | 385,445 (73.8) | 283,880 (71.1) | 299,568 (68.2) |
| Hepatitis C (%) | 81,256 (4.6) | 5312 (8.1) | 16,527 (4.9) | 21,527 (4.1) | 16,189 (4.1) | 21,701 (4.9) |
| Peripheral artery disease (%) | 60,387 (3.4) | 3302 (5.1) | 14,210 (4.2) | 18,337 (3.5) | 12,246 (3.1) | 12,292 (2.8) |
| Average eGFR at T0 (SD), ml/min per 1.73 m2 | 74.8 (19.3) | 71.7 (21.6) | 72.6 (20.0) | 73.9 (19.2) | 75.2 (18.7) | 77.7 (18.6) |
| eGFR at T0 (%), ml/min per 1.73 m2 | ||||||
| ≥90 | 25,249 (1.4) | 2085 (3.2) | 7150 (2.1) | 7640 (1.5) | 4462 (1.1) | 3912 (0.9) |
| ≥60 to <90 | 98,720 (5.6) | 5972 (9.1) | 25,157 (7.4) | 31,263 (6.0) | 19,746 (5.0) | 16,582 (3.8) |
| ≥45 to <60 | 272,441 (15.4) | 11,479 (17.5) | 57,977 (17.1) | 85,344 (16.3) | 60,612 (15.2) | 57,029 (13.0) |
| ≥30 to <45 | 954,680 (54.1) | 31,176 (47.7) | 176,095 (52.1) | 283,942 (54.4) | 222,440 (55.7) | 241,027 (54.8) |
| ≥15 to <30 | 413,896 (23.5) | 14,719 (22.5) | 71,948 (21.3) | 114,184 (21.9) | 92,043 (23.1) | 121,002 (27.5) |
| Dialysis during follow-up (%) | 27,157 (1.5) | 1727 (2.6) | 6961 (2.1) | 8144 (1.6) | 5152 (1.3) | 5173 (1.2) |
| Kidney transplant during follow-up (%) | 11,515 (0.7) | 761 (1.2) | 2897 (0.9) | 3357 (0.6) | 2175 (0.5) | 2325 (0.5) |
| Average LDL-C (SD), mg/dl | 109.79 (33.8) | 93.16 (33.9) | 104.40 (33.3) | 110.88 (33.6) | 113.73 (33.6) | 111.54 (33.5) |
| Average triglycerides (SD), mg/dl | 160.81 (114.3) | 252.55 (194.2) | 204.98 (132.5) | 171.69 (108.0) | 145.35 (94.2) | 114.25 (78.3) |
| Average serum albumin (SD), g/dl | 4.09 (0.7) | 3.88 (0.7) | 4.00 (0.6) | 4.08 (0.7) | 4.13 (0.7) | 4.16 (0.8) |
| Body mass index (%) | ||||||
| Underweight | 17,671 (1.0) | 378 (0.6) | 1308 (0.4) | 2604 (0.5) | 3252 (0.8) | 10,129 (2.3) |
| Normal | 345,569 (19.6) | 8,507 (13.0) | 41,815 (12.4) | 78,388 (15.0) | 79,063 (19.8) | 137,796 (31.4) |
| Overweight | 689,296 (39.6) | 23,492 (35.9) | 126,130 (37.3) | 207,027 (39.6) | 167,046 (41.8) | 179,755 (40.9) |
| Obese | 703,450 (39.9) | 33,054 (50.5) | 169,074 (50.0) | 234,354 (44.9) | 149,942 (37.6) | 111,872 (25.5) |
| Average body surface area (SD), m2 | 2.1 (0.2) | 2.1 (0.2) | 2.1 (0.2) | 2.1 (0.2) | 2.1 (0.2) | 2.0 (0.2) |
| Statin use during follow-up (%) | 1,282,527 (72.7) | 45,963 (70.3) | 256,950 (76.0) | 397,119 (76.0) | 295,012 (73.9) | 287,483 (65.4) |
| ACEI/ARB use | 876,615 (49.7) | 38,709 (59.2) | 189,971 (56.2) | 270,522 (51.8) | 189,658 (47.5) | 187,755 (42.7) |
| Median follow-up time (IQR), yr | 9.1 (7.7–9.4) | 9.1 (5.4–9.3) | 9.1 (7.3–9.3) | 9.1 (8.1–9.4) | 9.2 (8.3–9.4) | 9.1 (7.4–9.4) |
| Death during follow-up (%) | 541,682 (30.7) | 26,247 (40.1) | 109,222 (32.3) | 152,625 (29.2) | 113,785 (28.5) | 139,803 (31.8) |
| Microalbumin-to-creatinine ratio (%),a mg/g | ||||||
| 0–<20 | 93,696 (69.8) | 4133 (65.5) | 21,558 (67.8) | 30,232 (69.5) | 20,322 (71.4) | 17,451 (72.0) |
| 20–<300 | 36,687 (27.3) | 1902 (30.2) | 9168 (28.9) | 12,030 (27.6) | 7429 (26.1) | 6158 (25.4) |
| ≥300 | 3938 (2.9) | 272 (4.3) | 1053 (3.3) | 1264 (2.9) | 709 (2.5) | 640 (2.6) |
| Average C–reactive proteinb (SD), mg/dl | 2.0 (4.4) | 2.4 (4.7) | 2.2 (4.7) | 2.0 (4.4) | 1.9 (4.2) | 1.9 (4.3) |
HDL-C, HDL cholesterol; IQR, interquartile range; LDL-C, LDL cholesterol; ACEI, angiotensin–converting enzyme inhibitor; ARB, angiotensin receptor blocker.
Results for a subset of the cohort (n=134,321).
Results for a subset of the cohort with available C–reactive protein data (n=65,112).
Association between HDL-C Levels and All-Cause Mortality in Overall Cohort and by eGFR Category
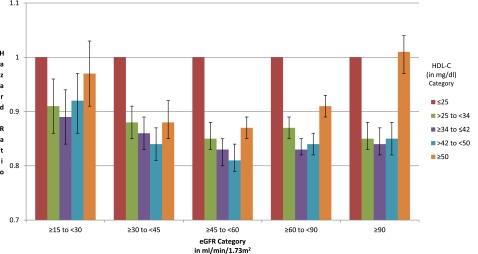
During a median follow-up of 9.1 years (IQR, 7.7–9.4 years), 541,682 (30.7%) study participants died in the overall cohort; 26,247 (40.1%), 109,222 (32.3%), 152,625 (29.2%), 113,785 (28.5%), and 139,803 (31.8%) were in HDL-C≤25, >25 to <34, ≥34 to ≤42, >42 to <50, and ≥50 mg/dl groups, respectively. In a series of nested models adjusting for demographics, eGFR, comorbid conditions, lipid parameters, BMI, statins, serum albumin, ACEI/ARB use, and cardiovascular disease, compared with the referent group of patients with low HDL-C (≤25 mg/dl), higher HDL-C levels were associated with lower risk of all-cause mortality in the overall cohort (Table 2). Compared with the referent category (HDL-C≤25 mg/dl), intermediate HDL-C levels (>25 to <34, ≥34 to ≤42, and >42 to <50 mg/dl) exhibited reduced risk of death across all levels of eGFR (Figure 2, Table 2). HDL-C≥50 mg/dl was not associated with reduced risk of all-cause mortality in the lowest and highest eGFR categories (eGFR<30 and ≥90 ml/min per 1.73 m2) (Table 2). Adjusted models of all-cause mortality by HDL-C in each eGFR category are presented in Table 2; the nested models are presented in Supplemental Table 2. Formal interaction analyses were undertaken and show a significant interaction between eGFR category and HDL-C in that lower GFR modified (attenuated) the salutary association of HDL-C and risk of death (P for interaction <0.01). However, even in the lowest eGFR group, there was still a significant association between HDL-C and risk of death in HDL-C groups with >25 to <34, ≥34 to ≤42, and >42 to <50 mg/dl (Supplemental Table 3).
Table 2.
Risk of all-cause mortality by HDL cholesterol levels in overall cohort and by eGFR category
| eGFR, ml/min per 1.73 m2 | Hazard Ratio (95% Confidence Interval) | ||||
|---|---|---|---|---|---|
| HDL-C≤25 mg/dl | HDL-C>25 to <34 mg/dl | HDL-C≥34 to ≤42 mg/dl | HDL-C>42 to <50 mg/dl | HDL-C≥50 mg/dl | |
| Overall | 1.00 | 0.87 (0.86 to 0.88) | 0.84 (0.83 to 0.85) | 0.84 (0.82 to 0.85) | 0.92 (0.91 to 0.93) |
| ≥15 to <30 | 1.00 | 0.91 (0.86 to 0.96) | 0.89 (0.84 to 0.94) | 0.92 (0.86 to 0.97) | 0.97 (0.91 to 1.03) |
| ≥30 to <45 | 1.00 | 0.88 (0.85 to 0.91) | 0.86 (0.83 to 0.89) | 0.84 (0.81 to 0.87) | 0.88 (0.85 to 0.92) |
| ≥45 to <60 | 1.00 | 0.85 (0.83 to 0.88) | 0.83 (0.80 to 0.85) | 0.81 (0.79 to 0.84) | 0.87 (0.85 to 0.89) |
| ≥60 to <90 | 1.00 | 0.87 (0.85 to 0.89) | 0.83 (0.82 to 0.85) | 0.84 (0.82 to 0.86) | 0.91 (0.89 to 0.93) |
| ≥90 | 1.00 | 0.85 (0.83 to 0.88) | 0.84 (0.82 to 0.87) | 0.85 (0.82 to 0.88) | 1.01 (0.97 to 1.04) |
Models were adjusted for age, race, cancer, cerebrovascular accident, chronic lung disease, diabetes mellitus, dementia, hepatitis C, HIV, hypertension, body mass index, LDL cholesterol, triglycerides, serum albumin, angiotensin–converting enzyme inhibitor/angiotensin receptor blocker use, coronary artery disease, congestive heart failure, and peripheral artery disease. Models were additionally adjusted for eGFR, dialysis, kidney transplant, and statin use as time varying. P for interaction of HDL-C and eGFR category is <0.01. HDL-C, HDL cholesterol.
Figure 2.
Risk of all-cause mortality by HDL cholesterol (HDL-C) levels in each eGFR category. Error bars represent 95% confidence intervals.
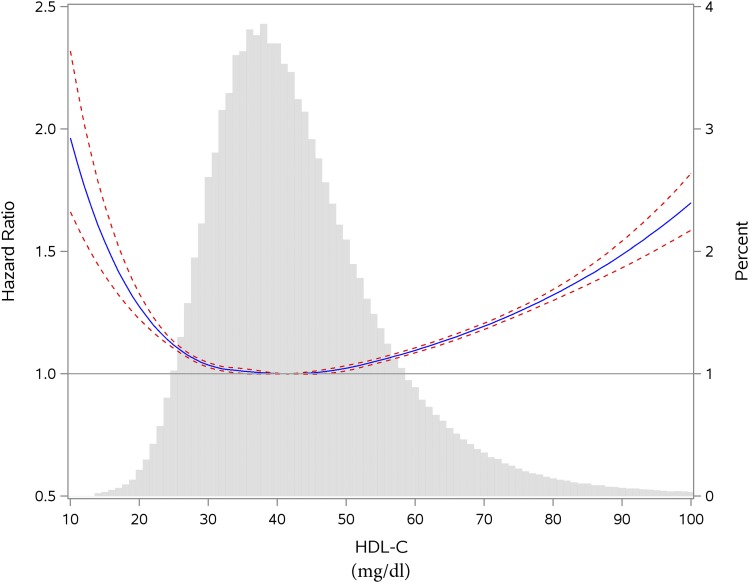
We then divided HDL-C into deciles and examined the relationship of HDL-C and risk of death in each eGFR category. In the overall cohort and compared with those in the lowest decile (decile 1), higher deciles (deciles 2–9) were associated with reduced risk of death, whereas decile 10 was associated with increased risk of death. In analyses by eGFR categories, the results suggest that, compared with the lowest HDL-C decile (decile 1), higher deciles (deciles 2–7) have reduced risk of death in all eGFR categories. Risk of death was increased in decile 10 among those with eGFR<30, ≥60 to <90, and ≥90 ml/min per 1.73 m2 (Table 3). However, in each eGFR category, the risk was lowest in the middle deciles and highest in deciles 1 and 10. Spline analyses suggest that—in the overall cohort and all eGFR categories—the relationship between HDL-C and mortality is not linear and exhibits a U-shaped association, where risk is lowest in the middle and elevated in low and high ends of HDL-C values spectrum (Figure 3, Supplemental Figure 1).
Table 3.
Risk of all-cause mortality by HDL cholesterol deciles in eGFR category
| HDL-C Decile | Median (IQR) | All-Cause Mortality Hazard Ratio (95% Confidence Interval) | |||||
|---|---|---|---|---|---|---|---|
| Overall | eGFR≥15 to <30 ml/min per 1.73 m2 | eGFR≥30 to <45 ml/min per 1.73 m2 | eGFR≥45 to <60 ml/min per 1.73 m2 | eGFR≥60 to <90 ml/min per 1.73 m2 | eGFR≥90 ml/min per 1.73 m2 | ||
| Decile 1 (low HDL-C) | 27.0 (24.0–28.0) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Decile 2 | 32.0 (31.0–32.9) | 0.92 (0.91 to 0.93) | 0.92 (0.88 to 0.97) | 0.94 (0.92 to 0.97) | 0.90 (0.88 to 0.92) | 0.93 (0.91 to 0.94) | 0.92 (0.90 to 0.95) |
| Decile 3 | 34.0 (34.0–35.0) | 0.91 (0.90 to 0.93) | 0.93 (0.88 to 0.99) | 0.90 (0.87 to 0.93) | 0.92 (0.90 to 095) | 0.91 (0.89 to 0.93) | 0.92 (0.89 to 0.95) |
| Decile 4 | 37.0 (36.0–38.0) | 0.91 (0.90 to 0.92) | 0.91 (0.87 to 0.96) | 0.92 (0.89 to 0.95) | 0.89 (0.87. 0.91) | 0.91 (0.89 to 0.92) | 0.92 (0.89 to 0.94) |
| Decile 5 | 40.0 (39.0–41.0) | 0.90 (0.89 to 0.91) | 0.91 (0.86 to 0.96) | 0.94 (0.91 to 0.97) | 0.88 (0.86 to 0.90) | 0.89 (0.87 to 0.90) | 0.91 (0.89 to 0.94) |
| Decile 6 | 43.0 (42.0–44.0) | 0.90 (0.89 to 0.91) | 0.99 (0.94 to 1.05) | 0.89 (0.86 to 0.92) | 0.88 (0.86 to 0.90) | 0.90 (0.89 to 0.92) | 0.91 (0.88 to 0.94) |
| Decile 7 | 46.0 (45.0–47.0) | 0.91 (0.90 to 0.92) | 0.89 (0.84 to 0.96) | 0.92 (0.88 to 0.95) | 0.89 (0.86 to 0.91) | 0.91 (0.90 to 0.93) | 0.92 (0.89 to 0.95) |
| Decile 8 | 50.0 (48.9–51.0) | 0.92 (0.91 to 0.93) | 0.97 (0.91 to 1.03) | 0.91 (0.87 to 0.94) | 0.89 (0.86 to 0.91) | 0.91 (0.90 to 0.93) | 0.98 (0.95 to 1.01) |
| Decile 9 | 56.0 (54.0–58.0) | 0.94 (0.93 to 0.95) | 0.95 (0.89 to 1.02) | 0.95 (0.91 to 0.98) | 0.90 (0.88 to 093) | 0.93 (0.91 to 0.95) | 1.01 (0.98 to 1.04) |
| Decile 10 (high HDL-C) | 68.1 (64.0–77.0) | 1.09 (1.08 to 1.11) | 1.07 (1.00 to 1.15) | 0.99 (0.96 to 1.04) | 1.01 (0.98 to 1.04) | 1.08 (1.06 to 1.09) | 1.22 (1.18 to 1.25) |
Models were adjusted for age, race, cancer, cerebrovascular accident, chronic lung disease, diabetes mellitus, dementia, hepatitis C, HIV, hypertension, body mass index, LDL cholesterol, triglycerides, serum albumin, angiotensin–converting enzyme inhibitor/angiotensin receptor blocker use, coronary artery disease, congestive heart failure, and peripheral artery disease. Models were additionally adjusted for eGFR, dialysis, kidney transplant, and statin use as time varying. IQR, interquartile range; HDL-C, HDL cholesterol.
Figure 3.
Spline analyses of all-cause mortality by HDL cholesterol (HDL-C) levels in the overall cohort, where median HDL-C was used as a reference and the HDL-C probability distribution histogram is represented in gray bars in the background. Dashed red lines represent 95% confidence intervals.
Association between HDL-C Levels and All-Cause Mortality Is Modified by Presence of Cardiovascular Disease
Formal interaction analyses were undertaken to examine whether presence of cardiovascular disease modifies the association of HDL-C and risk of death. The results suggest that presence of CAD attenuated the lessened risk of high HDL-C and all-cause mortality in those with eGFR≥60 ml/min per 1.73 m2 (Table 4). The magnitude and direction of risk were modified by the presence of CAD in those with eGFR≥90 ml/min per 1.73 m2 and HDL-C≥50 mg/dl (Table 4). Interaction models, where we tested effect modification by the presence of CHF (Supplemental Table 4A), the presence of either CAD or CHF, or both, yielded consistent results (Supplemental Table 4B).
Table 4.
Effect modification of the relationship between HDL cholesterol and risk of death by presence of coronary artery disease
| eGFR (ml/min per 1.73 m2) with or without Coronary Artery Disease | Hazard Ratio (95% Confidence Interval) | ||||
|---|---|---|---|---|---|
| HDL-C≤25 mg/dl | HDL-C>25 to <34 mg/dl | HDL-C≥34 to ≤42 mg/dl | HDL-C>42 to <50 mg/dl | HDL-C≥50 mg/dl | |
| ≥15 to <30 | |||||
| Without | 1.00 | 0.92 (0.83 to 1.02) | 0.92 (0.83 to 1.02) | 0.96 (0.86 to 1.07) | 0.97 (0.87 to 1.09) |
| With | 1.00 | 0.91 (0.85 to 0.97) | 0.88 (0.82 to 0.93) | 0.89 (0.83 to 0.96) | 0.98 (0.91 to 1.05) |
| ≥30 to <45 | |||||
| Without | 1.00 | 0.84 (0.79 to 0.89) | 0.82 (0.77 to 0.87) | 0.81 (0.76 to 0.86) | 0.85 (0.80 to 0.91) |
| With | 1.00 | 0.90 (0.86 to 0.93) | 0.87 (0.84 to 0.91) | 0.85 (0.81 to 0.89) | 0.89 (0.85 to 0.93) |
| ≥45 to <60 | |||||
| Without | 1.00 | 0.84 (0.80 to 0.88) | 0.81 (0.77 to 0.84) | 0.80 (0.77 to 0.84) | 0.85 (0.81 to 0.89) |
| With | 1.00 | 0.86 (0.83 to 0.89) | 0.84 (0.81 to 0.87) | 0.82 (0.79 to 0.85) | 0.88 (0.85 to 0.92) |
| ≥60 to <90 | |||||
| Without | 1.00 | 0.84 (0.82 to 0.87) | 0.80 (0.78 to 0.83) | 0.81 (0.79 to 0.84) | 0.88 (0.86 to 0.91) |
| With | 1.00 | 0.89a (0.87 to 0.92) | 0.86a (0.84 to 0.89) | 0.87a (0.84 to 0.89) | 0.93a (0.90 to 0.96) |
| ≥90 | |||||
| Without | 1.00 | 0.81 (0.78 to 0.85) | 0.80 (0.77 to 0.83) | 0.80 (0.77 to 0.84) | 0.96 (0.92 to 1.00) |
| With | 1.00 | 0.93a (0.87 to 0.98) | 0.92a (0.87 to 0.98) | 0.94a (0.88 to 0.99) | 1.08a (1.02 to 1.14) |
Models were adjusted for age, race, cancer, cerebrovascular accident, chronic lung disease, diabetes mellitus, dementia, hepatitis C, HIV, hypertension, body mass index, LDL cholesterol, triglycerides, serum albumin, angiotensin–converting enzyme inhibitor/angiotensin receptor blocker use, coronary artery disease, congestive heart failure, and peripheral artery disease. Models were additionally adjusted for eGFR, dialysis, kidney transplant, and statin use as time varying. HDL-C, HDL cholesterol.
Significant (<0.05) P value for interaction between HDL-C level and coronary artery disease status.
Sensitivity Analyses
We evaluated the consistency of study findings by undertaking a number of sensitivity analyses as described in Materials and Methods. The results were consistent with those shown in the primary analyses (Supplemental Tables 5–8).
Discussion
In a longitudinal national cohort study of 1,764,986 United States veterans spanning almost a decade (median follow-up of 9.1 years), we show that, compared with low HDL-C (≤25 mg/dl), intermediate HDL-C levels (HDL-C between 25 and 50 mg/dl) were associated with reduced risk of all-cause mortality and that risk of death in patients with high HDL-C (≥50 mg/dl) was comparable with that of patients with low HDL-C (≤25 mg/dl). Analyses where HDL-C was categorized in deciles and spline analyses further support the assessment that the association between HDL-C and risk of death is not linear and follows a U-shaped relationship (where risk is highest in those with very low and very high HDL-C levels). Furthermore, we show that risk is modified by eGFR and presence of cardiovascular disease.
Zewinger et al. (5) studied the association of HDL-C and mortality in a cohort of 3307 patients with significant burden of CAD (77.9%) who underwent coronary angioplasty and concluded that higher HDL-C was not associated with reduced mortality in patients with kidney dysfunction (eGFR<60 ml/min per 1.73 m2). Our results support a more nuanced conclusion: specifically, the association between HDL-C and risk of death follows a U-shaped curve, and lower eGFR attenuated the salutary effect of HDL-C; however, the associations remained significant in patients with advanced kidney disease. We also show that presence of cardiovascular disease attenuates the association of HDL-C and all-cause mortality.
The observation that the association between HDL-C and risk of death follows a U-shaped curve was not expected, and the mechanism underpinning the association of high HDL-C and mortality is not clear. Our study did not examine the cause of death; however, we note that prevalence of diabetes, hypertension, and cardiovascular diseases was lower among those with high HDL-C, suggesting perhaps that cardiovascular events are not likely to explain the increased risk of death in this group. We also note the slightly higher percentage of patients with cancer and that average CRP was higher among those with high HDL-C. Whether cancer or conditions associated with increased CRP (infections and chronic inflammation) explain the increased risk of death among patients with high HDL-C merits additional investigation.
Comparison of risk in high–HDL-C vis-à-vis low–HDL-C groups, where the risk relationship might not be linear and risk may be increased at both ends of the HDL-C values spectrum, might mask the presence of an association where one exists (23). Our results suggest that, regardless of eGFR category, the lower risk of death associated with HDL-C was most pronounced in the middle deciles and that risk is elevated in lowest and highest deciles (a U-shaped relationship). These results reconcile with findings from recent Mendelian randomization analyses showing that genetic mechanisms that raise plasma HDL-C do not lower risk of myocardial infarction (24). Experimental evidence suggests that HDL-C may have a biphasic effect (at low and high concentrations) and that, at high concentrations, HDL-C paradoxically enhanced senescence and impaired endothelial progenitor cell tube formation and angiogenesis, suggesting loss of protective effect (25). Furthermore, pharmaceutic intervention studies (those involving cholesterol ester transfer protein inhibitors or niacin) aimed at increasing HDL-C levels did not result in amelioration of cardiovascular outcomes or mortality (26–28). The constellation of findings from these studies supports the notion that there may be a range of HDL-C values where HDL-C may have a salutary effect, beyond which higher HDL-C may not be beneficial and may be associated with untoward outcomes. Identification of HDL-C levels where risk is highest (and the corollary identification of levels where risk is lowest) and which groups of patients are most likely to favorably respond to interventions aimed at increasing HDL-C levels may be useful in informing patient selection, design, and implementation of such trials and help develop a definitive answer to the question of whether therapeutics aimed at ameliorating HDL-C levels may improve clinical outcomes (29). The results from our studies, however, also suggest that risk of death varies very little for the vast majority of participants in this large cohort, which highlights the challenge of identifying populations where interventions might lead to amelioration of risk of death and may limit the potential public health effect of potential pharmaceutic interventions.
Our study has a number of limitations. Although our study included data on HDL-C levels and other lipid parameters, our data do not allow for qualitative assessment of HDL-C size, composition, functional capacity, or HDL-C subclasses (i.e., HDL2, which is generally associated with improved cardiovascular outcomes) (30,31). Low HDL-C may be present in the context of increased oxidative stress, insulin resistance, poor physical activity, smoking, and alcohol consumption. Our datasets did not include information on these parameters. We also note that there are significant baseline differences in demographic and health characteristics among cohort participants according to eGFR and HDL-C levels (Table 1, Supplemental Table 1) and that those with low eGFR and those with low HDL-C had much higher burden of comorbid illnesses (Table 1, Supplemental Table 1); these observations suggest that HDL-C is a heavily confounded measure, which might challenge its validity as an independent predictor of clinical outcomes. Additionally, although we accounted for several known covariates in our models, we cannot completely eliminate the possibility of residual confounding, the notion that there might be factors, either unmeasured or unknown, that might partially or fully explain the reported associations and that HDL-C may be more of a surrogate marker rather than an independent driver of clinical outcomes. Regardless, we show that quantitative assessment of HDL-C informs risk of all-cause mortality across levels of eGFR and by presence of cardiovascular disease. Our data did not include information on the cause of mortality. The cohort consisted of mainly older white men who were United States veterans and sought and obtained care at the VA; thus, the observed associations may not be generalizable to a broader population. Additionally, cohort selection required participants to have at least an eGFR, a complete lipid panel, and serum albumin to qualify for cohort entry, and as such, this might represent a selection bias. The nature of administrative data and the retrospective design of the study may also lead to sampling bias, errors in measurement, and misclassification of exposure or predictor variables. To minimize such measurement bias, we used definitions that have been validated for use in VA administrative data. We performed a number of sensitivity analyses, where we tested robustness of findings to changes in epidemiologic design and specification of statistical models, and the results were consistent.
Disclosures
None.
Supplementary Material
Acknowledgments
This work was funded by a grant from the US Department of Veterans Affairs (to Z.A.-A.).
The contents do not represent the views of the US Department of Veterans Affairs or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.00730116/-/DCSupplemental.
References
- 1.Yamamoto S, Yancey PG, Ikizler TA, Jerome WG, Kaseda R, Cox B, Bian A, Shintani A, Fogo AB, Linton MF, Fazio S, Kon V: Dysfunctional high-density lipoprotein in patients on chronic hemodialysis. J Am Coll Cardiol 60: 2372–2379, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trevisan R, Dodesini AR, Lepore G: Lipids and renal disease. J Am Soc Nephrol 17[Suppl 2]: S145–S147, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Speer T, Rohrer L, Blyszczuk P, Shroff R, Kuschnerus K, Kränkel N, Kania G, Zewinger S, Akhmedov A, Shi Y, Martin T, Perisa D, Winnik S, Müller MF, Sester U, Wernicke G, Jung A, Gutteck U, Eriksson U, Geisel J, Deanfield J, von Eckardstein A, Lüscher TF, Fliser D, Bahlmann FH, Landmesser U: Abnormal high-density lipoprotein induces endothelial dysfunction via activation of Toll-like receptor-2. Immunity 38: 754–768, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Jacek R, Anna G, Danilo F, Timo S, Andrzej W: Chronic kidney disease - different role for HDL? Curr Med Chem 21: 2910–2916, 2014 [DOI] [PubMed] [Google Scholar]
- 5.Zewinger S, Speer T, Kleber ME, Scharnagl H, Woitas R, Lepper PM, Pfahler K, Seiler S, Heine GH, März W, Silbernagel G, Fliser D: HDL cholesterol is not associated with lower mortality in patients with kidney dysfunction. J Am Soc Nephrol 25: 1073–1082, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamprea-Montealegre JA, Astor BC, McClelland RL, de Boer IH, Burke GL, Sibley CT, O’Leary D, Sharrett AR, Szklo M: CKD, plasma lipids, and common carotid intima-media thickness: Results from the multi-ethnic study of atherosclerosis. Clin J Am Soc Nephrol 7: 1777–1785, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaziri ND, Navab M, Fogelman AM: HDL metabolism and activity in chronic kidney disease. Nat Rev Nephrol 6: 287–296, 2010 [DOI] [PubMed] [Google Scholar]
- 8.Vaziri ND: Causes of dysregulation of lipid metabolism in chronic renal failure. Semin Dial 22: 644–651, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang F, Zheng J, Ye P, Luo L, Bai Y, Xu R, Sheng L, Xiao T, Wu H: Association of high-density lipoprotein cholesterol with the estimated glomerular filtration rate in a community-based population. PLoS One 8: e79738, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baragetti A, Norata GD, Sarcina C, Rastelli F, Grigore L, Garlaschelli K, Uboldi P, Baragetti I, Pozzi C, Catapano AL: High density lipoprotein cholesterol levels are an independent predictor of the progression of chronic kidney disease. J Intern Med 274: 252–262, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Muntner P, Coresh J, Smith JC, Eckfeldt J, Klag MJ: Plasma lipids and risk of developing renal dysfunction: The atherosclerosis risk in communities study. Kidney Int 58: 293–301, 2000 [DOI] [PubMed] [Google Scholar]
- 12.Murphy PA, Cowper DC, Seppala G, Stroupe KT, Hynes DM: Veterans Health Administration inpatient and outpatient care data: An overview. Eff Clin Pract 5[Suppl]: E4, 2002 [PubMed] [Google Scholar]
- 13.Oddone EZ, Eisen S: Veterans Affairs Research and Development: Using science to improve health care for veterans. N C Med J 69: 35–37, 2008 [PubMed] [Google Scholar]
- 14.US Department of Veterans Affairs : VIReC Research User Guide: VHA Medical SAS Outpatient Datasets FY2006, Hines, IL, US Department of Veterans Affairs VA Information Resource Center, 2007
- 15.US Department of Veterans Affairs : VIReC Research User Guide: VHA Medical SAS Inpatient Datasets FY2006, Hines, IL, US Department of Veterans Affairs VA Information Resource Center, 2007
- 16.US Department of Veterans Affairs : VIReC Research User Guide: Veterans Health Administration Decision Support System Clinical National Data Extracts, Hines, IL, US Department of Veterans Affairs VA Information Resource Center, 2009
- 17.Du Bois D, Du Bois EF: A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5: 303–311, 1989 [PubMed]
- 18.Xie Y, Bowe B, Xian H, Balasubramanian S, Al-Aly Z: Rate of kidney function decline and risk of hospitalizations in stage 3A CKD. Clin J Am Soc Nephrol 10: 1946–1955, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA: Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43: 1130–1139, 2005 [DOI] [PubMed] [Google Scholar]
- 20.Xie Y, Bowe B, Li T, Xian H, Balasubramanian S, Al-Aly Z: Proton pump inhibitors and risk of incident CKD and progression to ESRD [published online ahead of print April 14, 2016]. J Am Soc Nephrol [DOI] [PMC free article] [PubMed]
- 21.Xie Y, Bowe B, Xian H, Balasubramanian S, Al-Aly Z: Estimated GFR trajectories of people entering CKD stage 4 and subsequent kidney disease outcomes and mortality [published online ahead of print March 4, 2016]. Am J Kidney Dis doi:10.1053/j.ajkd.2016.02.039 [DOI] [PubMed] [Google Scholar]
- 22.Xie Y, Bowe B, Xian H, Balasubramanian S, Al-Aly Z: Renal function trajectories in patients with prior improved eGFR slopes and risk of death. PLoS One 11: e0149283, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bowe B, Xie Y, Xian H, Balasubramanian S, Al-Aly Z: Low levels of high-density lipoprotein cholesterol increase the risk of incident kidney disease and its progression. Kidney Int 89: 886–896, 2016 [DOI] [PubMed]
- 24.Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, Hindy G, Hólm H, Ding EL, Johnson T, Schunkert H, Samani NJ, Clarke R, Hopewell JC, Thompson JF, Li M, Thorleifsson G, Newton-Cheh C, Musunuru K, Pirruccello JP, Saleheen D, Chen L, Stewart A, Schillert A, Thorsteinsdottir U, Thorgeirsson G, Anand S, Engert JC, Morgan T, Spertus J, Stoll M, Berger K, Martinelli N, Girelli D, McKeown PP, Patterson CC, Epstein SE, Devaney J, Burnett MS, Mooser V, Ripatti S, Surakka I, Nieminen MS, Sinisalo J, Lokki ML, Perola M, Havulinna A, de Faire U, Gigante B, Ingelsson E, Zeller T, Wild P, de Bakker PI, Klungel OH, Maitland-van der Zee AH, Peters BJ, de Boer A, Grobbee DE, Kamphuisen PW, Deneer VH, Elbers CC, Onland-Moret NC, Hofker MH, Wijmenga C, Verschuren WM, Boer JM, van der Schouw YT, Rasheed A, Frossard P, Demissie S, Willer C, Do R, Ordovas JM, Abecasis GR, Boehnke M, Mohlke KL, Daly MJ, Guiducci C, Burtt NP, Surti A, Gonzalez E, Purcell S, Gabriel S, Marrugat J, Peden J, Erdmann J, Diemert P, Willenborg C, König IR, Fischer M, Hengstenberg C, Ziegler A, Buysschaert I, Lambrechts D, Van de Werf F, Fox KA, El Mokhtari NE, Rubin D, Schrezenmeir J, Schreiber S, Schäfer A, Danesh J, Blankenberg S, Roberts R, McPherson R, Watkins H, Hall AS, Overvad K, Rimm E, Boerwinkle E, Tybjaerg-Hansen A, Cupples LA, Reilly MP, Melander O, Mannucci PM, Ardissino D, Siscovick D, Elosua R, Stefansson K, O’Donnell CJ, Salomaa V, Rader DJ, Peltonen L, Schwartz SM, Altshuler D, Kathiresan S: Plasma HDL cholesterol and risk of myocardial infarction: A Mendelian randomisation study. Lancet 380: 572–580, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang CY, Lin FY, Shih CM, Au HK, Chang YJ, Nakagami H, Morishita R, Chang NC, Shyu KG, Chen JW: Moderate to high concentrations of high-density lipoprotein from healthy subjects paradoxically impair human endothelial progenitor cells and related angiogenesis by activating Rho-associated kinase pathways. Arterioscler Thromb Vasc Biol 32: 2405–2417, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJ, Bittner V, Fruchart JC; Treating to New Targets Investigators : HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med 357: 1301–1310, 2007 [DOI] [PubMed] [Google Scholar]
- 27.Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, Chaitman BR, Holme IM, Kallend D, Leiter LA, Leitersdorf E, McMurray JJ, Mundl H, Nicholls SJ, Shah PK, Tardif JC, Wright RS; dal-OUTCOMES Investigators : Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 367: 2089–2099, 2012 [DOI] [PubMed] [Google Scholar]
- 28.Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B; ILLUMINATE Investigators : Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 357: 2109–2122, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Kalil RS, Wang JH, de Boer IH, Mathew RO, Ix JH, Asif A, Shi X, Boden WE: Effect of extended-release niacin on cardiovascular events and kidney function in chronic kidney disease: A post hoc analysis of the AIM-HIGH trial. Kidney Int 87: 1250–1257, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Boer IH, Brunzell JD: HDL in CKD: How good is the “good cholesterol?”. J Am Soc Nephrol 25: 871–874, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Müller-Deile J, Schmitt R: HDL in CKD: Not protective any longer? Kidney Int 85: 712, 2014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.