Abstract
Objectives
This study aims to: (1) test whether the minority stressors disclosure of sexual orientation; and (2) internalized heterosexism are predictive of chronic physical health conditions; and (3) depression; (4) to test direct and indirect relationships between these variables; and (5) whether chronic physical health conditions are further predictive of depression, net of disclosure of sexual orientation and internalized heterosexism.
Methods
Secondary analysis of national, community-based surveys of 2349 lesbian, gay, and bisexual adults aged 50 and older residing in the US utilizing structural equation modeling.
Results
Congruent with minority stress theory, disclosure of sexual orientation is indirectly associated with chronic physical health conditions and depression, mediated by internalized heterosexism with a suppressor effect. Internalized heterosexism is directly associated with chronic physical health conditions and depression, and further indirectly associated with depression mediated by chronic physical health conditions. Finally, chronic physical health conditions have an additional direct relationship with depression, net of other predictor variables.
Conclusion
Minority stressors and chronic physical health conditions independently and collectively predict depression, possibly a synergistic effect. Implications for depression among older sexual minority adults are discussed.
Keywords: Sexual orientation, depression, older adults, minority stress, structural equation modeling
Introduction
The World Health Organization (WHO) has characterized depression as a serious public health issue (World Health Organization, 2012). Current annual health care expenditures for the treatment of depression in the US alone exceed $22 billion (Soni, 2012). In addition, the annual per capita health care costs for older Americans with depression exceed $20,000, which is more than double the cost of those who do not (Unützer et al., 2009). Untreated depression typically becomes chronic in nature (Chapman, Perry, & Strine, 2005; Fiske, Wetherell, & Gatz, 2009), negatively impacting quality of life (Chapman et al., 2005; Fiske et al., 2009), the treatment of co-occurring chronic physical health conditions (Centers for Disease Control and Prevention and National Association of Chronic Disease Directors, 2009), and potentially decreasing life expectancy by 5–10 years (Chapman et al., 2005). Depression is recognized as the most common, treatable chronic mental health condition among older adults (Centers for Disease Control and Prevention, 2015). Population-based prevalence estimates of depression among Americans aged 50 and older in the general population are typically reported to range from 1% to 5% (Centers for Disease Control and Prevention, 2015). National Survey on Drug Use and Health (NSDUH) and Behavioral Risk Factor Surveillance System (BRFSS) data indicate prevalences among adults aged 50 and older ranging from about 6% (Substance Abuse and Mental Health Services Administration, 2013) to about 8%, respectively (Centers for Disease Control and Prevention and National Association of Chronic Disease Directors, 2009). Clinically significant depressive symptomatology among older community-dwelling adults may be as high as 15% (Fiske et al., 2009).
Census projections suggest that the number of Americans aged 50 and older will grow to more than 130 million by 2030, and will approach 164 million by 2060 (U.S. Census Bureau, 2015). Current national estimates suggest that 2.6–4.9 million of these will self-identify as lesbian, gay, and bisexual (LGB) (Gates & Newport, 2012). Our knowledge of the health and well-being of LGB older adults remains a significant shortcoming in health disparities research (Centers for Disease Control and Prevention, 2011; Fredriksen-Goldsen, Emlet, et al., 2013). Yet, LGB Americans aged 50 and older have been found to be a health disparate population, evidencing higher rates of poor mental health as well as other physical health problems than heterosexual older adults (Fredriksen-Goldsen, Kim, Barkan, Muraco, & Hoy-Ellis, 2013; Wallace, Cochran, Durazo, & Ford, 2011). In large community-based samples, 29% of LGB older adults (Fredriksen-Goldsen, Emlet, et al., 2013) and 47% of transgender older adults (Fredriksen-Goldsen, Cook-Daniels, et al., 2013) have been found to have clinically significant depressive symptomatology. While poor mental health outcomes among lesbian, gay, bisexual, or transgender (LGBT) older adults are being recognized, the underlying processes tend to be less understood (Institute of Medicine, 2011). A major goal of the Healthy People 2020 initiative is to improve the health and well-being of LGB communities, including reducing the incidence of major depression among LGB adults as a targeted objective (U.S. Department of Health and Human Services, 2013). Meeting this objective will require a better understanding of depression among LGB older adults so that culturally responsive intervention and prevention efforts can be developed and implemented.
Depression is not a part of the normative aging process. According to the diathesis-stress perspective, depression due to genetic diathesis is more common among younger adults; disruptions resulting from significant life events and cumulative social, psychological, and biological stressors are more likely to result in depression among older adults (Blazer & Hybels, 2005; Fiske et al., 2009; Zuckerman, 1999). General stressors that increase the risk for depression in older adulthood are common to both LGB and heterosexual older adults. These include financial challenges, decreased social interactions, social isolation, bereavement, and other negative life events (Fiske et al., 2009). Numerous chronic medical conditions have been linked to depression among older adults (Blazer, 2003; Chapman et al., 2005; Fiske et al., 2009; Yang, 2007). Adults in the general population living with chronic health conditions, particularly those aged 40–59 years old have a significantly increased risk for developing depression (Pratt & Brody, 2008). Just under 80% of Americans aged 50 and older have at least one chronic health condition (AARP Public Policy Institute, 2010; Centers for Disease Control and Prevention, 2013). Chronic health conditions most often associated with depression include asthma, arthritis, cardiovascular disease (CVD), diabetes, and obesity (Chapman et al., 2005; Fiske et al., 2009). Emerging evidence indicates that compared to their heterosexual counterparts, LGB adults aged 50 and older are also at heightened risk for a variety of chronic physical health conditions, including CVD, obesity, and asthma among sexual minority women (Fredriksen-Goldsen, Kim, et al., 2013), and hypertension and diabetes among sexual minority men (Wallace et al., 2011). These conditions are among the most prevalent associated with increased risk of developing or exacerbating the course of depressive disorders (Chapman et al., 2005; Fiske et al., 2009).
LGB older adults also experience additional stressors unique to their sexual orientation, which stem from living in a heterosexist society and are theorized to contribute to their ‘excess’ rates of depression (Centers for Disease Control and Prevention, 2013). Heterosexism can be described as the collective constellation of societal prejudice, attitudes, stereotypes, and beliefs that cast heterosexuality as normative and any other form of human sexual identity, attraction, and/or behavior as abnormal (Herek & Garnets, 2007). The minority stress model identifies processes by which heterosexist-related minority stressors negatively impact the mental health of LGB people (Meyer, 2003). Internals of minority stressors, internalized heterosexism and concealment of sexual orientation, are the most chronic and inescapable (Meyer, 2003) and, thus, may play a crucial role in heightened risk for depression among older LGB adults. Internalized heterosexism refers to early and ongoing socialization processes by which people internalize society’s prejudicial attitudes, stereotypes, and beliefs regarding non-heterosexuality. Consciously and unconsciously, LGB people may apply such internalized representations to themselves and to other LGB people (Meyer, 2003). Internalized heterosexism has been associated with increased risk for depression among LGB older adults (Fredriksen-Goldsen, Emlet, et al., 2013).
Self-concealment of personal information and secrets of a distressing nature have been consistently linked to physiological symptoms in the general population (Uysal, Lin, & Knee, 2010). Concealing one’s non-heterosexual orientation may provide a degree of short-term protection by making oneself a less visible target for victimization, but continued concealment over time is psychologically stressful (Meyer, 2003), negatively impacting neuroendocrine functioning (Meyer, 2003) associated with the development of chronic health conditions (Cole, Kemeny, Taylor, & Visscher, 1996). A sample of HIV-negative gay men in the Natural History of AIDS Psychosocial Study who concealed their sexual orientation developed cancer at significantly higher rates relative to gay men who disclosed their sexual orientation (Cole et al., 1996). Recent epigenetic research has identified chronic stress as playing a role in the expression of the ATF3 gene in breast cancer metastasis (Wolford et al., 2013). Alternately, disclosure of one’s LGB sexual orientation is posited to counteract the negative impacts of chronic minority stress by providing individual and group-level coping resources (Meyer, 2003). Research findings regarding the role of concealment and disclosure of sexual orientation and risk of depression among older LGB adults have been mixed. Data from the Urban Men’s Health Study (UMHS) indicated that disclosure is associated with greater risk for depression among gay men aged 50–59, but not for those aged 60 and older (Rawls, 2004). Another study found that disclosure of sexual orientation among older LGB adults is associated with lower levels of depression, but that relationship is indirectly working through internalized heterosexism (Hoy-Ellis, 2015). Yet, a different study found no relationship between concealment or disclosure of sexual orientation and depression, when controlling for demographic characteristics and other risk and protective factors (Fredriksen-Goldsen, Emlet, et al., 2013).
The significance of the current study is that it examines the relative roles of the most internal of minority stressors, internalized heterosexism and concealment or disclosure of sexual orientation, and chronic health conditions in depression among older LGB adults. It also seeks to explore if disparities in certain chronic physical health conditions identified in this population may contribute to disparities in poor mental health. Specifically, this study aims to test the following hypothesized relationships:
Disclosure of sexual orientation is directly and inversely related to internalized heterosexism, chronic health conditions, and depression.
Disclosure of sexual orientation is inversely and indirectly associated with chronic health conditions and depression through internalized heterosexism.
Internalized heterosexism is directly and positively related to chronic physical health conditions and depression.
Internalized heterosexism is positively and indirectly associated with depression via chronic physical health conditions.
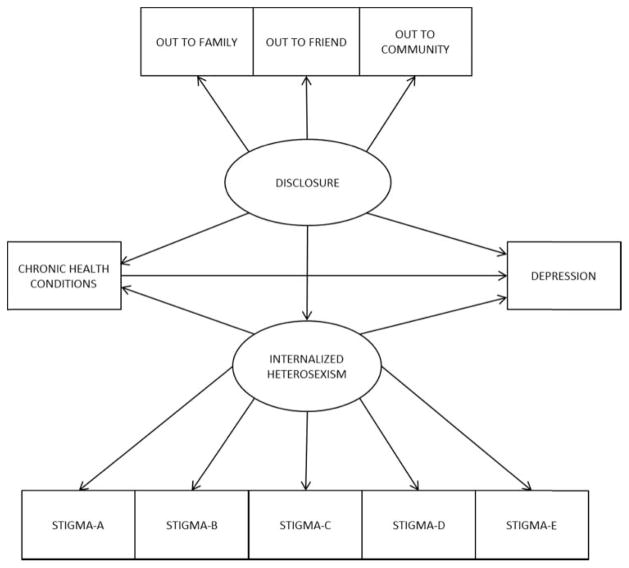
Chronic physical health conditions have an additional positive relationship with depression among LGB older adults, net of disclosure of sexual orientation and internalized heterosexism (see Figure 1 for model to be tested).
Figure 1.
Structural equation model to be tested.
Note: Model showing direct and indirect relationships between latent variables concealment and internalized heterosexism; and observed variables chronic health conditions and depression.
Methods
Sample and procedure
This study is a secondary analysis of data from the National Health, Aging, & Sexuality Study: Caring & Aging with Pride Over Time (NHAS), the first of its kind national study to investigate the health and well-being of LGB older adults as a population distinct from both their younger LGB peers and older heterosexual adult counterparts. The Institute for Multigenerational Health at the University of Washington, Seattle, partnered with 11 agencies across the US, which provide programming and services specific to LGB older adults. A survey was developed and distributed via agency mailing lists from June through November of 2010. The survey included questions to assess standard sociodemographic information, as well as sexual orientation and gender identity. Also included in the survey were items particularly relevant to LGB experience, such as disclosure of sexual orientation or gender identity, and measures of physical and mental health. Inclusion criteria for the NHAS required that (1) potential participants be 50 years old or older at the time of the survey distribution and (2) self-identify as LGBT. Along with standard informed consent and anonymity protocols, participants were offered an opportunity to enter a raffle to win one of five $500 gift cards for their time, winners to be chosen randomly. The University of Washington Institutional Review Board approved all study materials, procedures, and safeguards for the protection of human participants; many partnering agencies conducted their own internal reviews. The final dataset was comprised of surveys completed by 2560 LGBT adults aged 50–95 years old. For a fuller description of the NHAS, see Fredriksen-Goldsen, Kim and associates (2013).
The sample for the current study (n = 2349) consisted of 829 self-identified bisexual and lesbian women (35%) and 1520 bisexual and gay men. Transgender participants were excluded and studied elsewhere. Sample participants ranged in age from 50 to 95 years old (M = 66.9; SD = 9.0), most identified as lesbian or gay (95%), and were predominantly non-Hispanic white (87.0%). Although the majority (92%) had at least some college education, about half (52%) reported annual household incomes of $49,999. See Table 1 for sample sociodemographic characteristics.
Table 1.
Sample sociodemographic characteristics.
| Variable | (%) | (n) |
|---|---|---|
| Age M (SD) | 66.9 (9.0) | 2372 |
| Gender | ||
| Women | 35.4 | 840 |
| Men | 64.6 | 1531 |
| Sexual orientation | ||
| Lesbian/gay | 94.6 | 2217 |
| Bisexual | 5.4 | 124 |
| Race/ethnicity | ||
| Hispanic/non-Hispanic, non-white | 13.0 | 343 |
| Non-Hispanic white | 87.0 | 2198 |
| Education | ||
| Grade 1–8 | 0.2 | 4 |
| Grade 9–11 | 0.8 | 19 |
| Grade 12 or GED | 6.7 | 158 |
| College 1–3 years | 18.2 | 427 |
| College 4 years or more | 74.2 | 1744 |
| Annual household income | ||
| <$20,000 | 18.2 | 399 |
| $20,000–$24,999 | 8.3 | 186 |
| $25,000–$34,999 | 11.7 | 269 |
| $35,000–$49,999 | 14.3 | 329 |
| $50,000–$74,999 | 17.0 | 396 |
| $75,000 or more | 30.6 | 721 |
Measures
Covariates income and education were controlled for, as the robust associations between these variables and chronic health conditions and depression have been widely established (Marmot & Wilkinson, 2006; World Health Organization, 2003). Age was also treated as a covariate as it has been related to disclosure of sexual orientation and internalized heterosexism (David & Knight, 2008). Annual household income was coded across six categories: <$20,000; $20,000–$24,999; $25,000–$34,999; $35,000–$49,999; $50,000–$74,999; and $75,000 or more. Educational attainment was categorized as: kindergarten or none; grade 9–11; grade 12 or GED (General Educational Development Test, a certification that is equivalent to a high school diploma); college of 1–3 years; and college of 4 years or more. Age was calculated from reported year of birth.
A latent variable to assess the degree of disclosure of the participants’ sexual orientation was constructed from a modified version of the 12-item Outness Inventory (Mohr & Fassinger, 2000), which assesses sexual orientation disclosure in three primary social domains. Participants indicated the likelihood that family members (e.g. parent, sibling), community members (e.g. neighbors, faith community), and a best friend know or have known their sexual orientation on a 4-point Likert scale (1 = definitely do not know through 4 = definitely do know). Factor analyses indicated that the three indicators (out to friend, family, community) loaded well onto a single factor (.63–.91, p < .001). Internal consistency was acceptable, Cronbach’s α = .71. Higher scores indicate higher levels of disclosure of sexual orientation.
A separate latent variable with five indicators was constructed to capture internalized heterosexism, utilizing the Homosexual Self-Stigma subscale (Liu, Feng, & Rhodes, 2009). Participants indicated their level of agreement with five statements such as ‘I wish I weren’t lesbian, gay, bisexual, or transgender’ coded on a 4-point Likert scale (1 = strongly agree through 4 = strongly disagree). Factor analyses indicated that all five items loaded well onto a single latent factor (.48–.79, p < .001), with acceptable internal consistency (Cronbach’s α = .79). Responses were then reverse-coded so that higher scores indicated higher levels of internalized heterosexism.
Chronic health conditions were treated as an observed variable based on participants’ endorsement (‘mark all that apply’) of whether they had ever been told by a physician that they had any of the following nine chronic health conditions identified in the literature as being associated with depression: angina, arthritis, congestive heart failure, diabetes, heart attack, high cholesterol, hypertension, osteoporosis, and stroke. A number of conditions were summed, producing a range of 0–9, with higher numbers indicating the presence of more chronic health conditions.
Depression was assessed via the Center for Epidemiological Studies Depression Scale 10-item short form (CESD-10) (Radloff, 1977), which has well-established validity and reliability in screening for major depression across populations (Grzywacz, Hovey, Seligman, Arcury, & Quandt, 2006; Zhang et al., 2012), including among community-dwelling older adults (Andresen, Malmgren, Carter, & Patrick, 1994; Boey, 1999; Irwin, Artin, & Oxman, 1999). Depression was treated as an observed variable, making for a more parsimonious the model; model fit decreases as the number of variables increases (Kenny, 2014). The CESD-10 calls for participants to indicate how many days during the past week (0 = <1 day, 1 = 1–2 days; 2 = 3–4 days; 3 = 5–7 days) they had felt or acted in certain ways; for example, ‘I felt depressed,’ and ‘everything I did was an effort.’ Internal consistency was good, Cronbach’s α = 0.88. On a range of 0–30, a score ≥10 is an indicator of depressive symptoms that meet clinically significant levels (Andresen et al., 1994; Zhang et al., 2012).
Statistical analyses
Structural equation modeling (SEM) using Stata v. 12 was employed for all analyses. SEM is a confirmatory statistical technique useful for testing a priori theorized models (Bollen, 1989). A sample variance–covariance matrix is computed and compared to an estimated population variance–covariance matrix; if the difference between the two matrices is close to zero, the model is considered to be a good fit to the data (Bollen, 1989). In SEM, the measurement model provides information as to how well indicators load onto latent variables (i.e. confirmatory factor analysis); the structural model provides information on the relationships between variables. SEM has some advantages over more traditional multiple regression techniques. Standard regression models assume ‘perfect measurement’ which produces biased estimates (Baron & Kenny, 1986); SEM accounts for measurement error (Bollen, 1989), and is more sensitive to detecting suppressor effects (Cheung & Lau, 2008) and mediation effects (Iacobucci, Saldhana, & Deng, 2007). Total effects can be decomposed into their direct and indirect components, allowing inferences about mediation effects to be made (Duncan, 1975). Because equations are estimated simultaneously, standard errors are smaller and more consistent (Iacobucci et al., 2007).
In this study, the Maximum Likelihood estimator with pairwise deletion was used for model-testing. The data were not normally distributed, therefore, bootstrapping, resampling with replacement (500 replications), was employed to derive a sampling distribution for more precise standard errors and accurate confidence intervals (CI) (Cheung & Lau, 2008). A Variance Inflation Factor (VIF) was computed to assess for possible issues of multicollinearity, which preliminary analyses indicated was not an issue; VIF = 1.07, well below the acceptable upper bound of 10 (StataCorp, 2011). Hooper, Coughlan, and Mullen (2008) recommend assessing an array of post-estimation goodness-of-fit (GOF) statistics to examine model fit. The model χ2 is typically reported, yet, with very large sample sizes (i.e. ≥200); this statistic will almost always be significant (Matsueda, 2012), requiring rejection of the null hypothesis. However, a non-significant difference between the sample and estimated population variance–covariance matrices is indicative of a good model fit. Of other test statistics endorsed by Hooper et al. (2008), the Comparative Fit Index (CFI) is minimally affected by sample size, thus, addressing the issue of model χ2 significance. It contrasts the null model against the sample covariance matrix and calculates a statistic that ranges from 0 to 1; a value >.90 suggests a good model fit. Among the most revealing of fit statistics, the Root Mean Square Error of Approximation (RMSEA) identifies the closeness of fit between the population covariance matrix and sample parameters; a value <.06 indicates a good fit between the model and the data (Hooper et al., 2008). The Standardized Root Mean Square Residual (SRMR) is a measure of the difference between the standardized square root residuals of the sample and hypothesized population covariance matrices. While an SRMR < .08 is considered adequate, a value <.05 suggests a better model fit (Hooper et al., 2008). In addition, a CI close to zero implies that the sample and hypothesized population covariance matrices do not differ significantly.
Results
Overall, 29% of the sample (n = 666) reported clinical symptoms that met the threshold of major depression, scoring ≥10 on the CESD-10 (M = 7.2, SD = 6.2). The average level of disclosure, 3.5 on a scale of 1–4 (SD = .6) was relatively high, and the mean level of internalized heterosexism, 1.5 on a scale of 1–4 (SD = .6) was relatively low. Participants had on average 1.9 chronic health conditions (SD = 1.4). See Table 2 for sample summary statistics and distributions of chronic health conditions.
Table 2.
Sample summary statistics and distribution of chronic health conditions.
| Variable | Range | M (SD) | Chronic conditions | (%) | (n) |
|---|---|---|---|---|---|
| Disclose to friend | 3.9 (0.6) | Angina | 3.9 | 92 | |
| Disclose to family | 1–4 | 3.4 (0.8) | Arthritis | 33.8 | 802 |
| Disclose to community | 3.5 (0.7) | Congestive heart failure | 2.7 | 63 | |
| Disclosure overall | 3.5 (0.6) | Diabetes | 13.7 | 324 | |
| Internalized heterosexism | 1–4 | 1.5 (0.6) | Heart attack | 5.6 | 132 |
| Chronic health conditions | 0–9 | 1.9 (1.4) | High cholesterol | 43.3 | 1027 |
| Depression (CESD) | 0–30 | 7.2 (6.2) | Hypertension | 45.5 | 1079 |
| CESD ≥ 10 | 29.2% | n = 666 | Osteoporosis | 10.2 | 243 |
| Stroke | 3.9 | 92 |
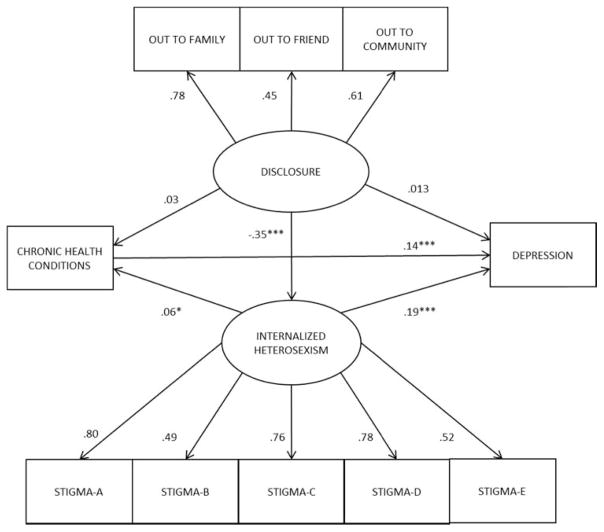
To further assess model fit, a Lagrange Multiplier Test to detect omitted paths and provide estimates of change in model fit was conducted. Adding omitted paths is methodologically sound, provided that such additions are consistent with theory (StataCorp, 2011). Correlated error term paths were added (not shown), which is theoretically sound as indicators of observed measures are themselves typically correlated (see Table 3 for correlation matrix). The final fitted model is shown in Figure 2. With the exception of the χ2-statistic, post-estimation GOF test statistics separately and collectively suggest a very close fit of the model to the data (see Table 4).
Table 3.
Correlations of observed measures.
| Disclosure (D)
|
Internalized heterosexism (IH)
|
Chronic | CESD | Age | Income | Education | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Family | Friend | Community | A | B | C | D | E | ||||||
| D-family | 1.00 | ||||||||||||
| D-friend | .38 | 1.00 | |||||||||||
| D-community | .49 | .45 | 1.00 | ||||||||||
| IH-A | −.18 | −.11 | −.23 | 1.00 | |||||||||
| IH-B | −.11 | −.06 | −.09 | .39 | 1.00 | ||||||||
| IH-C | −.17 | −.13 | −.20 | .71 | .09 | 1.00 | |||||||
| IH-D | −.19 | −.14 | −.22 | .60 | .37 | .59 | 1.00 | ||||||
| IH-E | −.13 | −.08 | −.14 | .38 | .26 | .41 | .53 | 1.00 | |||||
| Chronic | −.08 | −.04 | −.05 | .07 | .04 | .06 | .08 | .04 | 1.00 | ||||
| CESD | −.04 | −.06 | −.05 | .18 | .09 | .14 | .20 | .11 | .18 | 1.00 | |||
| Age | −.31 | −.12 | −.16 | .11 | .02 | .06 | .11 | .06 | .22 | −.02 | 1.00 | ||
| Income | .13 | .10 | .14 | −.10 | .02 | −.05 | −.13 | −.07 | −.17 | −.31 | −.17 | 1.00 | |
| Education | .07 | .10 | .10 | −.04 | .04 | −.01 | −.07 | −.05 | −.12 | −.16 | −.07 | .36 | 1.00 |
Figure 2.
Fitted structural equation model.
Note: Showing direct and indirect relationships between latent variables concealment and internalized heterosexism; and observed variables chronic health conditions and depression. Factor loadings and path coefficients are standardized. *p < .05. **p < .01. ***p < .001.
Table 4.
Model goodness-of-fit statistics.
| Statistical test | Statistical value |
|---|---|
| Model χ2 (df) | 143.64 (42) |
| Root Mean Square Error of Approximation (RMSEA) | 0.035 |
| Confidence interval (CI) (90%) | [.029, .042] |
| Comparative Fit Index (CFI) | 0.981 |
| Standardized Root Mean Square Residual (SRMR) | 0.023 |
| Coefficient of determination (CD) (model R2) | 0.757 |
Factor loadings and path coefficients in Figure 2 are standardized to facilitate interpretation of relationships and effect sizes (Preacher & Kelley, 2011). Initial results initially indicated that disclosure of sexual orientation did not appear to have a significant association with either depression (p = .089) or chronic health conditions (p = .679). However, decomposition of total effects into their direct and indirect components (see Table 5) suggests that the indirect effect of disclosure is significantly related to both depression (p < .001) and chronic health conditions (p = .030). Indirect effects may be significant even though direct and total effects are not, such as the case when the indirect effect has an opposite sign, which may indicate that the mediating variable (i.e. internalized heterosexism) also acts as a suppressor, strengthening or weakening the effect of the independent variable on the dependent variable, thereby, obscuring the total effect (Rucker, Preacher, Tormala, & Petty, 2011). Opposite signs of the indirect coefficients are seen in Table 5. These relationships are in line with minority stress theory in that disclosure of sexual orientation decreases the stressful effects if internalized heterosexism (Meyer, 2003), which in turn, would attenuate the positive associations between internalized heterosexism with depression and chronic health conditions.
Table 5.
Decomposition of total, direct, and indirect effects.
| Depression
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| b* | se Direct | p > z | b* | se Indirect | p > z | b* | se Total | p > z | |
| Disclosure | .013 | .326 | .683 | −.064 | .168 | <.001 | −.051 | .309 | .089 |
| Internalized heterosexism | .186 | .418 | <.001 | .009 | .050 | .022 | .195 | .424 | <.001 |
| Chronic health conditions | .143 | .103 | <.001 | (No path) | .143 | .103 | <.001 | ||
| Internalized heterosexism | |||||||||
| Disclosure | −.354 | .048 | <.001 | (No path) | −.354 | .048 | <.001 | ||
| Chronic health conditions | |||||||||
| Disclosure | .032 | .064 | .249 | −.021 | .023 | .030 | .011 | .060 | .679 |
| Internalized heterosexism | .060 | .079 | .022 | (No path) | .060 | .079 | .022 | ||
Note: b*= Standardized coefficient; se = bootstrapped standard error.
Significant direct positive associations were found between internalized heterosexism and both depression and chronic health conditions, as well as an additional indirect association with depression via chronic health conditions; chronic health conditions have an additional positive direct association with depression (see Table 5). The cumulative direct, indirect, and total effects of concealment of sexual orientation, internalized heterosexism, and chronic health conditions indicate that these variables account for just under 76% of the variance in depression.
Discussion
Emerging research suggests that LGB older adults have a significantly greater risk for depression and several chronic health conditions (Fredriksen-Goldsen, Kim, et al., 2013; Valanis et al., 2000; Wallace et al., 2011). Concealment of sexual orientation (Hoy-Ellis, 2015) and internalized heterosexism may increase the risk for depression (Fredriksen-Goldsen, Emlet, et al., 2013; Hoy-Ellis, 2015) among LGB older adults (Fredriksen-Goldsen, Emlet, et al., 2013). The results reported here suggest that disparities in chronic health conditions documented among LGB older adults may explain some of the disparity in their rates of depression, aligning with research in the general older adult population linking chronic health conditions with increased risk for depression (Blazer & Hybels, 2005; Chapman et al., 2005; Fiske et al., 2009). Findings also provide additional evidence that minority stressors are cumulative in their effects on mental health outcomes (Meyer, 2003), and that pathways of risk are complex and may be obscured (Institute of Medicine, 2011). Disclosure of sexual orientation appears to be related to lower levels of internalized heterosexism, thereby, reducing the positive associations between both internalized heterosexism and chronic health conditions on depression. Internalized heterosexism and chronic health conditions may have additional impacts on depression, net of disclosure of sexual orientation, suggesting that social, psychological, and physical factors be considered in tandem when examining depression among LGB older adults.
The finding that higher levels of disclosure of sexual orientation are inversely related to internalized heterosexism and indirectly with depression mediated by internalized heterosexism is consistent with the minority stress model. Long-term concealment of a significant aspect of the self is psychologically costly (Meyer, 2003), which can be attributed to potential negative consequences of disclosure, shame, guilt, and distorted thinking that related to internalized heterosexism (Pachankis, 2007). Through disclosure of sexual orientation, important individual and group-level coping processes are activated reducing levels of internalized heterosexism (Meyer, 2003). When available, coping resources are deemed to be adequate to meet perceived threat through secondary appraisals (Lazarus & Folkman, 1984); the stress response and risk for depression are significantly diminished (Juster, McEwen, & Lupien, 2010). Consistent with social comparison theory (Hogg, Terry, & White, 1995) at the individual level, disclosure diminishes feelings of shame and guilt (Pachankis, 2007), and through subsequent positive comparisons of the self with other LGBs, replacing hitherto negative comparisons with heterosexuals, distorted cognitions regarding the self are ameliorated (Meyer, 2003).
The indirect relationship between concealment and chronic health conditions, mediated via internalized heterosexism and the additional direct effect of internalized heterosexism on both chronic health conditions and depression, is consistent with social stress theory broadly, and the minority stress framework in particular. Decades of social stress research have demonstrated that chronic psychosocial stressors ‘gets under the skin’ to become embodied and consequently manifest in chronic disease (Ferraro & Shippee, 2009; Krieger, 1999), such as CVD, diabetes (Juster et al., 2010), hypertension, and asthma (Katon, 2011), particularly among socially marginalized groups (Aneshensel, 2009). The internalization of stigma associated with marginalized social status has been characterized as a chronic stressor in and of itself (Hatzenbuehler, Phelan, & Link, 2013). The hypothalamic-pituitary-adrenal (HPA) axis is central to neuroendocrine processes that are activated in response to stressors (Juster et al., 2010; McEwen, 1998). Cortisol and adrenaline are primary hormones released in this response process. When stressors are acute and relatively sporadic, the release of these hormones may enhance survival. When stressors are chronic, repeated over-activation of the HPA-axis results in allostatic load (AL) (Juster et al., 2010; McEwen, 1998). Among other negative physiological effects, AL has been linked to metabolic dysfunctions such as hyperlipidemia and insulin resistance, which are associated with diabetes, hypertension, and CVD (Juster et al., 2010; McEwen, 1998). Regions of the brain involved in threat appraisal processes are also negatively impacted by AL, resulting in decreased perceived coping resources and increased risk for depression (McEwen, 2006).
Chronic health conditions also have an additional direct association with depression, net of all other relationships. Having chronic health conditions increases the risk for developing depression or exacerbating existent depression (Chapman et al., 2005; Katon, 2011; Wolkowitz, Reus, & Mellon, 2011). There is also a direct relationship between increasing numbers of chronic health conditions and increased risk of developing or worsening depression (Chapman et al., 2005). It is, thus, plausible that the heightened risk of chronic health conditions identified among LGB older adults (Fredriksen-Goldsen, Kim, et al., 2013; Wallace et al., 2011) plays an important role in the disparately high rates of depression documented in this population. The relationship between chronic health conditions and depression is also consistent with the broader social stress literature. LGB older adults are marginalized both by their sexual orientation and their age (Fredriksen-Goldsen, Hoy-Ellis, Goldsen, Emlet, & Hooyman, 2014), resulting in social exclusion and lower social standing. Findings from the Whitehall studies have advanced our understanding of the relationship between lower social standing, chronic health conditions, and poor mental health outcomes by showing that the underlying mechanism of risk is decreased control over important aspects of the social environment that accompanies lower social standing (Marmot et al., 1991; Marmot & Wilkinson, 2006). The presence of chronic health can also limit control over key aspects of one’s life (Blazer, 2003; Katon, 2011).
Implications
There is a dearth of research that attends to midlife and older LGB adults as a population distinct from both midlife and older heterosexual adults, and from younger adult and adolescent sexual minorities. The little research that has made such comparisons indicates that there are important differences between these respective groups (Fredriksen-Goldsen, Kim, et al., 2013; Kertzner, Meyer, Frost, & Stirratt, 2009; Wallace et al., 2011). Today’s LGB older adults are more likely to conceal their sexual orientation than their younger LGB counterparts (Floyd & Bakeman, 2006). Within-group differences by age are also beginning to emerge. For example, LGB adults aged 50–64 years old report higher rates of discrimination and victimization than their counterparts aged 65 and older, yet, the latter age group evidences higher levels of internalized heterosexism and is more likely to conceal their sexual orientation than the former (Fredriksen-Goldsen, Kim, Shiu, Goldsen, & Emlet, 2014). Fearing discrimination by staff, and harassment and isolation from other clients, even LGB older adults who are open about their sexual orientation believe that they will need to conceal their identity in order to access mainstream aging services – at the very time when advancing age increases the likelihood of needing such services (National Senior Citizens Law Center, 2011). Yet, these findings suggest that to do so, may place LGB older adults at increased risk for depression.
This study makes a significant contribution to our knowledge regarding the health and well-being of older LGB adults by identifying how minority stress risk factors and chronic health conditions are associated with each other and with depression. Identifying that chronic health conditions play a role in the minority stress process may enhance our understanding of why rates of depression remain alarmingly high as LGB individuals get older (Fredriksen-Goldsen, Kim, et al., 2013; Wallace et al., 2011), while rates of depression decline noticeably in the general population as it ages (Blanchflower & Oswald, 2008; Blazer, 2003; Yang, 2007). Furthermore, results may also contribute to clarifying the theoretical relationship between internal minority stressors of concealing LGB sexual orientation and internalized heterosexism, and depression. Identifying and understanding the complex interactions of minority stress processes as they relate to health will be central to developing culturally sensitive and effective interventions for LGB older adults living with depression.
There is evidence that the relationship between chronic health conditions and depression is recursive (Chapman et al., 2005; Katon, 2011; Pinquart & Sorenson, 2007). Many chronic health conditions that begin to manifest around the age of 50 may be rooted in chronic stress that begins in earlier life experience (Kuzawa & Sweet, 2009; Murgatroyd & Spengler, 2011; Seeman, Singer, Ryff, Dienberg Love, & Levy-Storms, 2002; Wolkowitz et al., 2011). The corrosive effects of internalized heterosexism that surfaces earlier in life when one begins to realize a non-heterosexual orientation would fall squarely in the category of ‘chronic stress that begins in earlier life experience.’ The same array of complex neurobiological patterns found between chronic social stress and HPA-axis dysregulation and AL is found in the relationship between chronic health conditions and depression (Chapman et al., 2005; Katon, 2011; Wolkowitz et al., 2011). Primary and secondary appraisals of threat and available coping resources are mediated by the brain (Lazarus & Folkman, 1984; McEwen, 1998). The ongoing dilemma of whether, when, where, how, and under what circumstances one conceals or discloses sexual orientation, coupled with attempting to gauge potential consequences is a primary appraisal process. If the individual chooses to continue concealing her or his sexual orientation, then concealment itself may be an additional chronic stressor (Meyer, 2003). On the other hand, disclosure may over time provide additional coping resources, reduce levels of internalized heterosexism, and buffer the impact of stress processes on health. Still, it is possible that those with depression are more likely to report having been diagnosed with chronic health conditions. Longitudinal research will be needed to clarify this relationship among LGB older adults.
This study has also practice implications for addressing depression related to sexual orientation among LGB older adults. Individual appraisals of stressors are central to social stress processes (Pearlin, Mullan, Semple, & Skaff, 1990). Subjective appraisals of stressors are more strongly related to poor health outcomes, including depression (Mittelman, Roth, Haley, & Zarit, 2004) than objective stressors (Zarit, Todd, & Zarit, 1986). Accurate assessment is foundational to effective treatment of depression among older adults (Zarit & Zarit, 2007). Therapeutic interventions to address the damaging effects of internalized heterosexism have typically focused on supporting the process of disclosure (Herek & Garnets, 2007). While such an approach can positively influence the stress appraisal process, it also runs the risk of blaming the individual for their poor mental health (Meyer, 2003). On the other hand, if the social environment is less threatening, it is likely to be appraised as less threatening, which would benefit LGB older adults with depression who do not have access to LGB-affirmative therapy.
Effectively addressing depression among LGB older adults that is related to factors associated with sexual orientation goes beyond intervening with current depression; it also requires prevention efforts. More than two decades ago, Albee and Ryan-Finn (1993) proposed that the occurrence of mental distress stemming from societal oppression can be described as a function of elements in the social environment that promote marginalization divided by the capacity of individuals and groups to resist marginalization. Taking such a social justice approach to primary prevention requires empowering LGB older adults to develop and strengthen their capacity to resist societal heterosexism, and that researchers identify and work toward dismantling heterosexist social structures and institutions (Kenny & Hage, 2009; Matthews & Adams, 2009). Such an approach would serve to ameliorate existent depression among today’s LGB older adults, and contribute to preventing the development of depression among the next generation of LGB older adults.
Limitations
In addition to its cross-sectional design, this study has other limitations. Surveys were distributed via agency mailing lists; participants who responded may differ in important ways from those who did not. For example, LGB older adults with higher levels of internalized heterosexism may be less likely to participate in research. Similarly, LGB older adults who are not connected with these service agencies may differ in significant ways from those who are, for example, differing levels of concealment and disclosure. The ways in which individuals came to be on agency mailing lists may also be an issue, as the majority of respondents in this sample (70.6%) were not utilizing services at the time that surveys were distributed. While there is representation across the country, the findings reported here cannot be generalized. Most participants were concentrated on the West Coast, Eastern Seaboard, and parts of the Central US in major metropolitan areas. Urban-dwelling LGB older adults likely have experiences that vary from their rural-dwelling counterparts. These limitations may have skewed findings. It is possible that LGB older adults who are connected with agencies may differ on both mental and physical health measures, which if true, likely biases these results.
The psychometric properties of the CESD-10 are well established; measures to assess internalized heterosexism and concealment/disclosure are less so. The Outness Inventory (Mohr & Fassinger, 2000) requires subjective interpretations of other likely perceptions, rather than whether participants have actively or passively disclosed or concealed their sexual orientation. The adapted version of the Homosexuality Stigma Scale (Liu et al., 2009) may not differentiate well between current and previous levels of internalized heterosexism. For example, ‘I have tried not to be LGB’ can refer to previous decades or current experience.
Nonetheless, this study has valuable strengths. It is one of the few to specifically examine LGB older adults as a distinct population, and to apply the minority stress framework to this population. In addition to providing support for the minority stress model in general, it also suggests that internal minority stressors may play a role in physical as well as mental health outcomes (e.g. depression), and that it is important to attend to both. Through the use of SEM, this study provides further evidence that may help to clarify the relationships between disclosure of sexual orientation, internalized heterosexism, chronic health conditions, and depression, particularly the role of internalized heterosexism as mediator suppressor of disclosure in both physical and mental health.
Conclusion
We must begin to think in terms of health equity and move toward targeting interventions upstream at community and policy levels. Health equity means that every person, regardless of social characteristics (including sexual orientation), has a right to the best possible health, which necessitates that any barriers to health that marginalized groups experience must be addressed (Braveman & Gruskin, 2003). Health disparities are the gauge by which progress toward health equity can be assessed; for LGB older adults to attain mental health equity in the form of resolving disparately high rates of depression, we must attend to the unique barriers that they experience (Fredriksen-Goldsen et al., 2014). Both the perceived and still all too often real need to conceal an LGB identity – it is still legal to discriminate based on sexual orientation in the majority of states (Human Rights Campaign, 2015) – and internalized heterosexism are barriers to LGB older adults’ mental health equity. Recognizing that these barriers are ultimately rooted in societal heterosexism requires that we must also calibrate interventions at community and policy levels to address macro-level heterosexism that fosters internalized heterosexism and the perceived need to conceal one’s sexual orientation, which eventually manifests downstream in disparately high rates depression.
Acknowledgments
Some research reported in this publication was supported in part by grants from the National Institute on Aging of the National Institutes of Health under Award Numbers R01AG026526 and 2R01AG026526-03A1 (Fredriksen-Goldsen, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, National Institute of Aging, the University of Utah, or the University of Washington.
Funding
National Institute on Aging of the National Institutes of Health [award number R01AG026526], [award number 2R01AG026526-03A1].
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- AARP Public Policy Institute. Chronic care: A call to action for health reform. 2010 Retrieved from http://assets.aarp.org/rgcenter/health/beyond_50_hcr.pdf.
- Albee GW, Ryan-Finn KD. An overview of primary prevention. Journal of Counseling and Development. 1993;72:115–123. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Aneshensel CS. Toward explaining mental health disparities. Journal of Health and Social Behavior. 2009;50(4):377–394. doi: 10.1177/002214650905000401. [DOI] [PubMed] [Google Scholar]
- Baron R, Kenny D. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Social Science & Medicine. 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003;58(3):249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Hybels CF. Origins of depression in later life. Psychological Medicine. 2005;35(9):1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. International Journal of Geriatric Psychiatry. 1999;14(8):608–617. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [Google Scholar]
- Braveman P, Gruskin S. Theory and methods: Defining equity in health. Journal of Epidemiology and Community Health. 2003;57:254–258. doi: 10.1136/jech.57.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC Health disparities and inequalities report – United States, 2011. MMWR 2011. 2011;60(Suppl):1–116. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The state of aging and health in America 2013. 2013 Retrieved from http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf.
- Centers for Disease Control and Prevention. Aging and depression. Healthy Aging. 2015 Retrieved from http://www.cdc.gov/aging/mentalhealth/depression.htm.
- Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. The state of mental health and aging in America – issue brief 2: Addressing depression in older adults: Selected evidence-based programs. 2009:1–12. Retrieved from http://www.cdc.gov/aging/pdf/mental_health_brief_2.pdf.
- Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Preventing Chronic Disease. 2005;2(1):1–10. [PMC free article] [PubMed] [Google Scholar]
- Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables: Bootstrapping with structural equation models. Organizational Research Methods. 2008;11(2):296–325. doi: 10.1177/1094428107300343. [DOI] [Google Scholar]
- Cole SW, Kemeny ME, Taylor SE, Visscher BR. Elevated physical health risk among gay men who conceal their homosexual identity. Health Psychology. 1996;15(4):243–251. doi: 10.1037//0278-6133.15.4.243. [DOI] [PubMed] [Google Scholar]
- David S, Knight BG. Stress and coping among gay men: Age and ethnic differences. Psychology and Aging. 2008;23(1):62–69. doi: 10.1037/0882-7974.23.1.62. [DOI] [PubMed] [Google Scholar]
- Duncan OD. Introduction to structural equation models. New York: Academic Press; 1975. Recursive models; pp. 25–66. [Google Scholar]
- Ferraro KF, Shippee TP. Aging and cumulative inequality: How does inequality get under the skin? The Gerontologist. 2009;49(3):333–343. doi: 10.1093/geront/gnp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annual Review of Clinical Psychology. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd FJ, Bakeman R. Coming out across the life course: Implications of age and historical context. Archives of Sexual Behavior. 2006;35(3):287–296. doi: 10.1007/s10508-006-9022-x. [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, Erosheva EA, Emlet CA, Hoy-Ellis CP, … Muraco A. Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist. 2013;54(3):488–500. doi: 10.1093/geront/gnt021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Emlet CA, Kim HJ, Muraco A, Erosheva EA, Goldsen J, Hoy-Ellis CP. The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. The Gerontologist. 2013;53(4):664–675. doi: 10.1093/geront/gns123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Hoy-Ellis CP, Goldsen J, Emlet CA, Hooyman NR. Creating a vision for the future: Key competencies and strategies for culturally competent practice with lesbian, gay, bisexual, and transgender (LGBT) older adults in the health and human services. Journal of Gerontological Social Work. 2014;57:80–107. doi: 10.1080/01634372.2014.890690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay male and bisexual older adults: Results from a population-based study. American Journal of Public Health. 2013;103(10):1802–1809. doi: 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Shiu C, Goldsen J, Emlet CA. Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. The Gerontologist. 2014;55(1):154–168. doi: 10.1093/geront/gnu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Simoni JM, Kim HJ, Lehavot K, Walters KL, Yang J, … Muraco A. The health equity promotion model: Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. American Journal of Orthopsychiatry. 2014;84(6):653–663. doi: 10.1037/ort0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates GJ, Newport F. Special report: 3.4% of U.S. adults identify as LGBT. Inaugural gallup findings based on more than 120,000 interviews. 2012 Retrieved from http://www.gallup.com/poll/158066/special-report-adults-identify-lgbt.aspx.
- Grzywacz JG, Hovey JD, Seligman LD, Arcury TA, Quandt SA. Evaluating short-form versions of the CES-D for measuring depressive symptoms among immigrants from Mexico. Hispanic Journal of Behavioral Sciences. 2006;28(3):404–424. doi: 10.1177/0739986306290645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Garnets LD. Sexual orientation and mental health. Annual Review of Clininical Psychology. 2007;3:353–375. doi: 10.1146/annurev.clinpsy.3.022806.091510. [DOI] [PubMed] [Google Scholar]
- Hogg MA, Terry DJ, White KM. A tale of two theories: A critical comparison of identity theory with social identity theory. Social Psychology Quarterly. 1995;58(4):255–269. [Google Scholar]
- Hooper D, Coughlan J, Mullen MR. Structural equation modeling: Guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6(1):53–60. [Google Scholar]
- Hoy-Ellis CP. Concealing concealment: The mediating role of internalized heterosexism in psychological distress among lesbian, gay, and bisexual older adults. Journal of Homosexuality. 2015;63(4):487–506. doi: 10.1080/00918369.2015.1088317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Rights Campaign. Why the equality act? 2015 Retrieved from http://www.hrc.org//resources/entry/why-the-equality-act.
- Iacobucci D, Saldhana N, Deng X. A meditation on mediation: Evidence that structural equations models perform better than regressions. Journal of Consumer Psychology. 2007;12(2):139–153. doi: 10.1016/S1057-7408(07)70020-7. [DOI] [Google Scholar]
- Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159(15):1701–1174. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues in Clinical Neuroscience. 2011;13(1):7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA. Measuring model fit. 2014 Retrieved from http://davidakenny.net/cm/fit.htm.
- Kenny ME, Hage SM. The next frontier: Prevention as an instrument of social justice. Journal of Primary Prevention. 2009;30(1):1–10. doi: 10.1007/s10935-008-0163-7. [DOI] [PubMed] [Google Scholar]
- Kertzner RM, Meyer IH, Frost DM, Stirratt MJ. Social and psychological well-being in lesbians, gay men, and bisexuals: The effects of race, gender, age, and sexual identity. American Journal of Orthopsychiatry. 2009;79(4):500–510. doi: 10.1037/a0016848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: Developmental origins of US racial disparities in cardiovascular health. American Journal of Human Biology. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- Liu H, Feng T, Rhodes AG. Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections. 2009;85(1):65–69. doi: 10.1136/sti.2008.032714. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Stansfeld S, Patel C, North F, Head J, White I, … Smith GD. Health inequalities among British civil servants: The Whitehall II study. The Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Wilkinson RG. Social determinants of health. 2. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Matsueda RL. Key advances in the history of structural equation modeling. In: Hoyle RH, editor. Handbook of structural equation modeling. New York, NY: The Guilford Press; 2012. pp. 17–42. [Google Scholar]
- Matthews CR, Adams EM. Using a social justice approach to prevent the mental health consequences of heterosexism. Journal of Primary Prevention. 2009;30(1):11–26. doi: 10.1007/s10935-008-0166-4. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease. allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators: Central role of the brain. Dialogues in Clinical Neuroscience. 2006;8(4):367–381. doi: 10.31887/DCNS.2006.8.4/bmcewen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittelman MS, Roth DL, Haley WE, Zarit SH. Effects of a caregiver intervention on negative caregiver appraisals of behavior problems in patients with Alzheimer’s disease: Results of a randomized trial. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2004;59B(1):P27–P34. doi: 10.1093/geronb/59.1.p27. [DOI] [PubMed] [Google Scholar]
- Mohr J, Fassinger R. Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development. 2000;33(2):66–90. [Google Scholar]
- Murgatroyd C, Spengler D. Epigenetic programming of the HPA axis: Early life decides. Stress. 2011;14(6):581–589. doi: 10.3109/10253890.2011.602146. [DOI] [PubMed] [Google Scholar]
- National Senior Citizens Law Center. LGBT older adults in long-term care facilities: Stories from the field. 2011 Retrieved from http://www.lgbtlongtermcare.org/authors/
- Pachankis JE. The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychological Bulletin. 2007;133(2):328–345. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorenson S. Correlates of physical health of informal caregivers: A meta-analysis. Journal of Gerontology. 2007;62B(2):P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Pratt LA, Brody DJ. Depression in the United States household population, 2005–2006. NCHS Data Brief. 2008;(7):1–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19389321. [PubMed]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rawls TW. Disclosure and depression among older gay and homosexual men: Findings from the Urban Men’s Health Study. In: Herdt G, de Vries B, editors. Gay and lesbian aging: Research and future directions. New York, NY: Springer; 2004. pp. 117–41. [Google Scholar]
- Rucker DD, Preacher KJ, Tormala ZL, Petty RE. Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass. 2011;5(6):359–371. doi: 10.1111/j.1751-9004.2011.00355.x. [DOI] [Google Scholar]
- Seeman TE, Singer BH, Ryff CD, Dienberg Love G, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosomatic Medicine. 2002;64(3):395–406. doi: 10.1097/00006842-200205000-00004. [DOI] [PubMed] [Google Scholar]
- Soni A. Trends in use and expenditures for depression among U.S. adults age 18 and older, civilian noninstitutionalized population, 1999 and 2009. 2012 Retrieved from http://meps.ahrq.gov/data_files/publications/st377/stat377.pdf.
- StataCorp. Stata: Release 12. College Station, TX: StataCorp LP; 2011. (Vol. Stata) [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 national survey on drug use and health: Mental health findings. 2013 Retrieved from http://www.samhsa.gov/data/sites/default/files/2k12MH_Findings/2k12MH_Findings/NSDUHmhfr2012.htm#sec2-3. [PubMed]
- U.S. Census Bureau. 2014 National population projections: Summary tables. Table 9. Projections of the population by age and sex for the United States: 2015 to 2060. 2015 Retrieved from https://www.census.gov/population/projections/data/national/2014/summarytables.html.
- U.S. Department of Health and Human Services. Lesbian, gay, bisexual, and transgender health. 2020 Topics & Objectives. 2013 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health/objectives.
- Unützer J, Schoenbaum M, Katon WJ, Fan MY, Pincus HA, Hogan D, Taylor J. Healthcare costs associated with depression in medically Ill fee-for-service medicare participants. Journal of the American Geriatric Society. 2009;57(3):506–510. doi: 10.1111/j.1532-5415.2008.02134.x. [DOI] [PubMed] [Google Scholar]
- Uysal A, Lin HL, Knee CR. The role of need satisfaction in self-concealment and well-being. Personality and Social Psychology Bulletin. 2010;36(2):187–199. doi: 10.1177/0146167209354518. [DOI] [PubMed] [Google Scholar]
- Valanis BG, Bowen DJ, Bassford T, Whitlock E, Charney P, Carter RA. Sexual orientation and health: Comparisons in the Women’s Health Initiative sample. Archives of Family Medicine. 2000;9(9):843–853. doi: 10.1001/archfami.9.9.843. [DOI] [PubMed] [Google Scholar]
- Wallace SP, Cochran SD, Durazo EM, Ford CL. The health of aging lesbian, gay and bisexual adults in California. Los Angeles, CA: UCLA Center for Health Policy Research; 2011. [PMC free article] [PubMed] [Google Scholar]
- Wolford CC, McConoughey SJ, Jalgaonkar SP, Leon M, Merchant AS, Dominick JL, … Hai T. Transcription factor ATF3 links host adaptive response to breast cancer metastasis. Journal of Clinical Investigation. 2013;123(7):2893–2906. doi: 10.1172/JCI64410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolkowitz OM, Reus VI, Mellon SH. Of sound mind and body: Depression, disease, and accelerated aging. Dialogues in Clinical Neuroscience. 2011;13(1):25–39. doi: 10.31887/DCNS.2011.13.1/owolkowitz. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Social determinants of health: The solid facts. 2003 Retrieved from http://www.euro.who.int/en/what-we-publish/abstracts/social-determinants-of-health.-the-solid-facts.
- World Health Organization. Depression Mental Health. 2012 Retrieved from http://www.who.int/mediacentre/factsheets/fs369/en/
- Yang Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. Journal of Health & Social Behavior. 2007;48(1):16–32. doi: 10.1177/002214650704800102. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. The Gerontologist. 1986;26(3):260–266. doi: 10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Zarit JM. Mental disorders in older adults: Fundamentals of assessment and treatment. 2. New York, NY: The Guilford Press; 2007. [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, … Lima VD. Validating a shortened depression scale (10 Item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999. Diathesis-stress models; pp. 3–23. [Google Scholar]