Abstract
The female genital tract (FGT) mucosa is a critically important site for immune defense against microbes. Mucosal-associated invariant T (MAIT) cells are an innate-like T cell population that recognizes microbial riboflavin metabolite antigens in an MR1-dependent manner. The role of MAIT cells in the FGT mucosa is unknown. Here, we found that MAIT cells and MR1+ antigen-presenting cells were present in the upper and lower FGT, with distinct tissue localization of MAIT cells in endometrium versus cervix. MAIT cells from the FGT and blood displayed a distinct phenotype with expression of IL-18Rα, CD127, α4β7, PD-1, as well as the transcription factors PLZF, RORγt, Helios, Eomes and T-bet. Their expression levels of PLZF and Eomes were lower in the FGT compared to blood. When stimulated with Escherichia coli, MAIT cells from the FGT displayed a bias towards IL-17 and IL-22 expression, whereas blood MAIT cells produced primarily IFN-γ, TNF, and Granzyme B. Furthermore, both FGT- and blood-derived MAIT cells were polyfunctional and contributed to the T cell-mediated response to E. coli. Thus, MAIT cells in the genital mucosa have a distinct IL-17/IL-22 profile and may play an important role in immunological homeostasis and control of microbes at this site.
Introduction
The female genital tract (FGT) comprises different compartments with unique anatomical and immunological features, which all serve two main tasks: protection against invading pathogens and maintenance of a favorable environment for fertilization.1 The mucosa of the FGT provides an extraordinary barrier composed of an epithelium covered by mucus, and harbors numerous effector cells belonging to the innate and adaptive arms of the immune system.2 The mucosa of the uterus (endometrium) and the canal connecting the uterus and vagina (endocervix) are lined by a monolayer of columnar epithelial cells, and undergo major structural and functional changes during the menstrual cycle.2 The portion of the uterus facing the vaginal lumen (ectocervix) and the vagina display a thick squamous epithelium. Between the endocervix and ectocervix, where the epithelium transforms from single- to multi-layered, lays the transformation zone that is characterized by a remarkable abundance of immune cells compared to the rest of the FGT.2,3
Although the mechanisms regulating immune responses in the FGT are not fully understood, the combined defenses of the genital mucosa effectively shield the host from pathogenic microbes as demonstrated, for instance, by the low efficiency of vaginal HIV-1 transmission.4 To this purpose, immediate immune responses at the site of microbial infection are mediated by cellular and soluble innate factors, which constitute a first line of defense and play a major role in shaping local adaptive immune responses.1,5,6
Mucosal-associated invariant T (MAIT) cells are a recently described innate T cell population, which is abundant in mucosal tissues, blood, and liver.7-9 MAIT cells express a semi-invariant T cell receptor (TCR), including Vα7.2 coupled with restricted Jα segments (Jα33, Jα12, or Jα20), and limited Vβ repertoires.10,11 Human MAIT cells are defined by the surface expression of their semi-invariant TCR in combination with the high expression of the C- type lectin CD161 and the interleukin (IL)-18 receptor α-subunit (IL-18Rα).9,12 Mature MAIT cells display an effector memory phenotype and exhibit a distinct transcriptional profile, expressing promyelocytic leukemia zinc finger (PLZF) and retinoic acid-related orphan receptor γt (RORγt) transcription factors.8,9 MAIT cells also express classical effector T cell T-box transcription factors T-bet and Eomesodermin (Eomes) as well as Helios, a transcription factor involved in T cell activation and proliferation.13-15 Decreased expression of these transcription factors in chronic HIV-1 infection is associated with MAIT cell depletion in circulation and functional impairment of MAIT cells following bacterial stimulation.13 MAIT cells recognize microbial vitamin B2 metabolites presented via the evolutionarily conserved major histocompatibility complex (MHC) class I-related (MR) 1 molecule.7,12,16,17 Upon activation, these cells have the capacity to produce cytokines such as interferon (IFN)γ, tumor necrosis factor (TNF), IL-17, and IL-22, suggesting their involvement in both antimicrobial responses and preservation of mucosal barrier integrity.8,12,18 Furthermore, MAIT cells have been shown to be associated with protection against mycobacterial infections in both mice and humans.12,19,20
Despite the growing body of research on MAIT cells in humans, their presence in the FGT has to date not been investigated. In the current study, we characterized the localization and phenotype of MAIT cells in the mucosa from different compartments of the FGT in healthy women and compared them to circulating MAIT cells. Using an ex vivo model of bacterial stimulation with Escherichia coli (E. coli), we analyzed the functionality of MAIT cells by measuring the production of selected cytokines and effector proteins relevant to antimicrobial responses and mucosal homeostasis. We found that MAIT cells reside in the mucosa throughout the FGT, are biased towards IL-17 and IL-22 expression, and may thus contribute to anti-microbial immune defenses at this site. Our data point to MAIT cells as an active component of the early immune defenses of the FGT and serve as the basis for further investigation of their role in women's health and disease.
Results
Clinical data and CD4+ and CD8+ T cell counts in the study populations
Study participants (n=38, median age 49 years, range 35-62 years) were recruited at the St. Göran Hospital gynecological clinic where they were admitted to undergo hysterectomy due to benign conditions. Before surgery, a physician interviewed all patients and they were all found to have good general health. Individuals who were seropositive for Human papilloma virus (HPV), reported symptoms or clinical signs of sexually transmitted infections at the time of surgery or during three months prior to surgery, or were treated with corticosteroids or other systemic immunosuppressive therapy were excluded from the study.
Thirty-five women were premenopausal and three were postmenopausal. Neither age nor menstrual status affected the down-stream immunological comparisons performed between study participants (data not shown). Detailed characteristics of the women donating genital tissue are included in Supplementary Table 1. Peripheral blood samples were collected from healthy women (n=16) who were in the same age range as the women who underwent hysterectomy (median age 46 years, range 30-60 years). Individuals using immunosuppressive drugs were not eligible as blood donors. Frequencies of CD4+ and CD8+ T cells in the endometrium, cervix, and blood were determined by flow cytometry, and CD4+ and CD8+ T cells were defined as CD45+CD3+CD4+ cells and CD45+CD3+CD8+ cells, respectively. The CD4/CD8 ratio in the endometrium and cervix was 0.96 and 1.07, respectively, whereas it was 2.15 in blood. These results are in agreement with previous reports on distribution of CD4+ and CD8+ T cells in cervicovaginal mucosal tissue.21
MAIT cells and MR1+ antigen-presenting cells reside in the upper and lower FGT
In situ staining was used to determine the localization and distribution of MAIT cells in mucosal specimens from different portions of the FGT, including the endometrium, endocervix, transformation zone, and ectocervix. MAIT cells were defined by immunofluorescent double-staining for Vα7.2 in combination with IL-18Rα, which were co-expressed on all CD161highVα7.2+ T cells, a phenotype identifying MAIT cells, isolated from the cervix and endometrium as evaluated by flow cytometry (Supplementary Figure 1). MAIT cells were present throughout the FGT; however they displayed a diverse distribution within the analyzed compartments. Scattered MAIT cells were located in close proximity to and within the glandular epithelium in the lamina propria of the endometrium (Figure 1a). Endocervical MAIT cells were primarily localized adjacent to the simple columnar epithelium (Figure 1b), while in the transformation zone, MAIT cells were primarily found in the lamina propria (Figure 1c). Furthermore, ectocervical MAIT cells were located on both sides of the basal membrane, with the majority residing within clusters of IL-18Rα+ cells in the epithelium (Figure 1d). Moreover, in situ double staining of Vα7.2 and CD3, as well as of CD3 and CD8, in consecutive tissue sections confirmed that the Vα7.2+ cells within the FGT were T cells and localized in proximity to other T cells (Supplementary Figure 2). Additional double staining of Vα7.2 and CD8 showed that Vα7.2+ cells were also CD8+ (data not shown).
Figure 1.
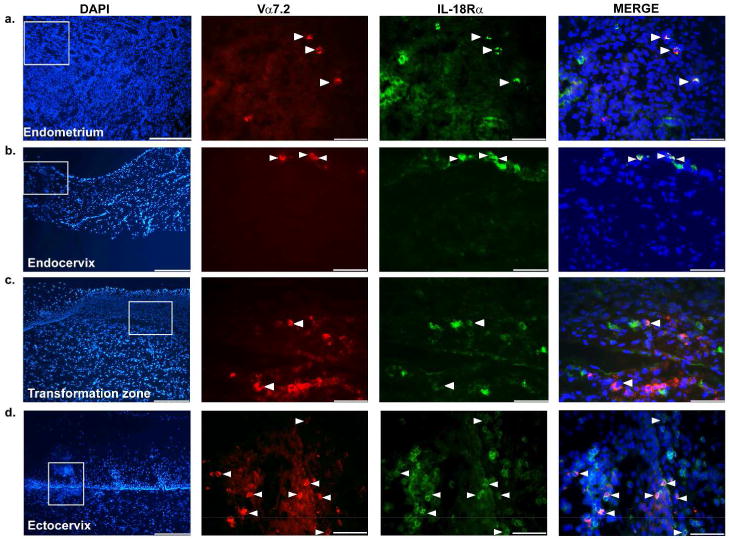
Localization and spatial distribution of MAIT cells in the FGT. Representative immunofluorescence images of (a) endometrial (n=6), (b) endocervical (n=2), (c) transformation zone (n=2), and (d) ectocervical (n=6) tissue sections stained for Vα7.2+ (red) and IL-18Rα+ (green) cells. To be noted, the 40× pictures of the ectocervix were rotated 90° right from the 10× overview picture. DAPI (blue) was used as a counterstain for visualization of cell nuclei. Double-positive (MAIT) cells are shown in yellow and are indicated by the white arrows. The images were collected with 10× and 40× objectives. The scale bars are 250 μm in the images in the first column and 60 μm in the images in the other three columns.
We next investigated if MR1+ antigen-presenting cells (APCs) were present within the same sites as MAIT cells. Thus, consecutive tissue sections of the endometrium and ectocervix were stained for MAIT cells and MR1+ APCs, which were defined by co-expression of MR1 and the APC marker HLA-DR. Similar to MAIT cells, MR1+HLA-DR+ cells were located within or in close proximity to the glandular epithelium of the endometrium and on both sides of the basal membrane in the ectocervix (Figure 2a). We also characterized the distribution of different APC subsets as well as their expression of MR1 in endometrial and ectocervical tissue samples. In line with previous observations,22,23 we found that Langerin+ cells were a minor population in endometrium, while they were more common in the ectocervix. CD11c+ dendritic cells were abundant in both compartments (data not shown). Furthermore, MR1 was expressed on CD11c+ cells in both the endometrium and ectocervix as well as on a few Langerin+ cells in the epithelial compartment of the ectocervix (Figure 2b).
Figure 2.
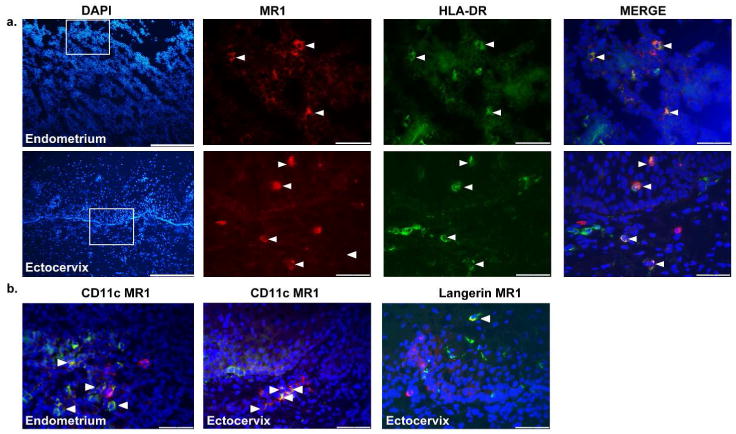
Localization and spatial distribution of MR1+ APCs in the endometrium and ectocervix. Representative immunofluorescence images of endometrial (n=2) and ectocervical (n=2) tissue sections stained for (a) MR1 (red) and HLA-DR (green); the scale bars are 250 μm in the images in the first column and 60 μm in the images in the other three columns. (b) Representative immunofluorescence images of endometrial and ectocervical tissue sections stained for MR1 (red) with CD11c (green) and MR1 (red) with Langerin (green); the scale bars are 60 μm. Double-positive cells are shown in yellow and are indicated by the white arrows. DAPI (blue) was used as a counterstain for visualization of cell nuclei. The images were collected with 10× and 40× objectives.
Comparable numbers and CD8/CD4 distribution of MAIT cells in FGT and blood
Next, flow cytometry was used to enumerate MAIT cells and assess their phenotype in endometrium, cervix, and blood samples. Due to the limited endocervix samples available, the endocervix and ectocervix were combined for this analysis and referred to as cervix. MAIT cells were identified as CD45+CD3+CD161hi Vα7.2+ cells (Figure 3a). MAIT cells isolated from the endometrium and cervix were quantified in comparable amounts (Figure 3b), and accounted for 1% and 1.8%, respectively, of the T cell population, defined as CD45+CD3+ cells. In blood, MAIT cells represented about 2.1% of T cells, thus accounting for a significantly higher proportion of cells compared to the endometrium (p=0.01), but not the cervix (Figure 3b). MAIT cells preferentially express CD8 with minor populations being CD4+ or double negative (CD4-CD8-). There were significant differences between these three sub-populations in the endometrium (p<0.0001), cervix (p=0.006) and blood (p<0.0001). Specifically, the percentage of CD8+ MAIT cells among T cells was significantly higher compared to both CD4+ MAIT cells and CD4-CD8- MAIT cells in all three compartments analyzed: in the endometrium, CD8+CD4-, CD8-CD4+, and CD8-CD4- MAIT cells were 69%, 12%, and 11% (p<0.0001); in the cervix 75%, 13%, and 12% (p=0.008); and in blood 84%, 2%, and 8% (p<0.0001), respectively. Furthermore, in blood, CD4+ MAIT cells were significantly lower compared to CD8-CD4- MAIT cells (2% vs. 8%, p=0.02) (Figure 3b). Additionally, similar frequencies of these three sub-populations of MAIT cells were observed between the different compartments, except for blood CD4+ MAIT cells, which were significantly lower compared to endometrial CD4+ MAIT cells (2% vs. 12%, p=0.01) (Figure 3b).
Figure 3.

Enumeration of the frequency of MAIT cells in the FGT and blood. (a) MAIT cell (CD161highVα7.2+) gating strategy and representative scatter plots. (b) Frequencies of MAIT cells out of T cells (CD45+CD3+) from the endometrium (n=19), cervix (n=14), and blood (n=16). (c) Frequencies of CD8 (CD4-CD8+), CD4 (CD4+CD8-), and DN (CD4-CD8-) MAIT cells out of total MAIT cells from the endometrium (n=10), cervix (n=5), and blood (n=10). The cervix samples consisted of pooled endocervical and ectocervical cells. Each dot represents a different patient; endometrium (circle), cervix (triangle), and blood (square). Horizontal lines represent median ± interquartile range. *P<0.05, **P<0.01, ***P<0.001.
Distinct transcription factor profiles of MAIT cells in the FGT and blood
We next characterized the expression of IL-18Rα, IL-7 receptor-α chain (CD127), the mucosal homing integrin α4β7, and PD-1, which are expressed on MAIT cells from blood, liver, and other mucosal tissues.8,18,24-26 MAIT cells from the endometrium, cervix, and blood displayed a universal expression of these markers, which was distinct from conventional CD8+ and CD4+ T cells (Supplementary Figure 1b).
We further characterized the transcription factor expression profile of endometrial, cervical, and blood MAIT cells. Similar expression levels of PLZF, RORγt, Helios, Eomes, and T-bet were observed between MAIT cells from the endometrium and cervix. However, endometrial MAIT cells and cervical MAIT cells, in comparison to those in blood, showed significantly lower expression levels of PZLF (median GMFI: 121 vs. 156; p=0.01) and Eomes (median GMFI: 776 vs. 1689; p=0.01), respectively (Figure 4a). Despite these differences, the overall expression pattern of the transcription factors in MAIT cells was similar between the three compartments and distinct from conventional T cells (Figure 4b) (Supplementary Figure 3).
Figure 4.

Expression of transcription factors in MAIT cells in the FGT and blood. Expression levels of PLZF, RORγt, Helios, Eomes, and T-bet transcription factors in MAIT cells (GMFI, geometric mean intensity fluorescence). (a) Scatter plots represent the expression levels of transcription factors in MAIT cells from the endometrium (n=7), cervix (n=4), and blood (n=6). Each symbol represents a different patient; endometrium (circle), cervix (triangle), and blood (square). Horizontal lines represent the median ± interquartile range, *P<0.05. (b) Representative histograms showing the expression levels of transcription factors in MAIT cells (red), CD4+ T cells (blue), and CD8+ T cells (green) from the endometrium (n=7), cervix (n=4), and blood (n=6).
MAIT cells in the FGT are biased towards IL-17 and IL-22 production upon E. coli stimulation
We next investigated the activation and cytokine production of MAIT cell from the FGT and blood in responses to bacteria encoding the riboflavin biosynthesis pathway. Endometrial and cervical samples were pooled in order to achieve a sufficient yield of cells needed for stimulation experiments, and these cells were referred to as FGT cells. Stimulation of cells from the FGT and blood with E. coli, or with phorbol 12-myristate 13-acetate (PMA), triggered production of IFN-γ, TNF, IL-17A (further referred to IL-17), IL-22, and GrzB in MAIT cells (Figure 5a). To increase the sensitivity of our bacterial stimulation assay, CD28 co-stimulation was included; however this did not alter the response profiles of MAIT cells (Supplementary Figure 4a). Additionally, stimulation with E. coli in the presence of MR1-blocking antibody resulted in a reduction of MAIT cell production of IFN-γ, TNF, and IL-17, indicating that the in vitro stimulation of MAIT cells occurred through bacterial antigen presentation on MR1 molecules. Notably, production of IL-22 and GrzB by MAIT cells was not altered by the MR1-blocking antibody (Supplementary Figure 4b).
Figure 5.

Cytokine and GrzB production profile by MAIT cells in the FGT and blood upon E. coli stimulation. (a) Representitive dot plot showing IFN-γ, TNF, IL-17, IL-22 and GrzB production by MAIT cells from FGT and blood samples that were either unstimulated (upper panel; n=8), stimulated with E.coli (middle panel; FGT n=10, blood n=6), or stimulated with PMA (lower panel; n=4). (b) Frequencies of cytokines and GrzB production by MAIT cells from the FGT (n=10) and blood (n=6). Each symbol represents a different patient; FGT (circle) and blood (square). Horizontal lines represent median ± interquartile range. *P<0.05, **P<0.01, ***P<0.001.
On average, E. coli stimulation induced IL-17 and IL-22 in a significantly higher fraction of MAIT cells from the FGT than in blood (9% vs. 1%; p=0.0005 and 2% vs. 0.2%; p=0.04, respectively). In contrast, the production of IFN-γ, TNF, and GrzB in response to E. coli was lower in FGT-derived MAIT cells compared to blood (IFN-γ 10% vs. 65%; p=0.004, TNF 11% vs. 38%; p=0.008, and GrzB 41% vs. 87%; p=0.003) (Figure 5b).
We next investigated if the preferential IL-17 and IL-22 production upon E. coli stimulation in the FGT was restricted to MAIT cells. We found that the total IL-17 and IL-22 production by CD45+ lymphocytes was two-fold and 20-fold higher in the FGT compared to blood while in contrast, CD45+ lymphocytes in the FGT produced lower levels of IFN-γ and TNF compared to blood (Supplementary figure 5a). We further assessed the production of these cytokines by CD3-CD45+ (non-T cells) and CD3+CD45+ (T cells) cells in the FGT and blood and, as expected, these cells had a different cytokine expression profile, depending on their anatomical origin (Supplementary Figure 5b). Furthermore, in line with previous findings showing that Th17 cells are a major subset in the FGT,27 we found that the frequencies of both IL-17 and IL-22 producing CD4+ T cells were significantly elevated in the FGT compared to blood (Supplementary Figure 5c). Collectively these data indicate that MAIT cells as well as other immune cells within the FGT are more prone to produce IL-17 and IL-22 after E. coli stimulation.
MAIT cells in the FGT have a distinct polyfunctional profile upon E. coli stimulation
We further assessed the, E. coli induced, polyfunctional profile of MAIT cells from the FGT and blood, using the SPICE software. The majority of MAIT cells in the FGT were monofunctional cells (68.6%), with lower frequencies of bi- and trifunctional cells (17.5% and 13.3%, respectively). In contrast, circulating MAIT cells had similar proportions of mono- and bifunctional cells (43.5% and 38.9%, respectively), and a lower frequency of trifunctional cells (17.1%). For both sites, the frequency of tetra- and penta- functional MAIT cells were low, although the FGT appeared to have slightly higher proportions of these highly polyfunctional cells (2.4% vs. 0.5%, respectively) (Figure 6a). The polyfunctional profile of MAIT cells (i.e. cells exhibiting >1 function) from the FGT was different from that observed in blood. Specifically, the frequencies of GrzB+IL-17+MAIT cells were significantly elevated in the FGT compared to blood (p=0.01), while significantly lower frequencies of MAIT cells in the FGT comprised of bifunctional GrzB+IFNγ+ (p<0.0001) and GrzB+TNF+ (p=0.02) cells. Likewise, similar observations were noted for the trifunctional MAIT cells, with significantly higher proportion of GrzB+IFN-γ+IL-17+ and GrzB+IL-17+TNF+ cells in the FGT vs. blood (p= 0.05 and p=0.05 respectively), and significantly lower proportion of GrzB+IFNγ+TNF+ as well as GrzB+IL-22+TNF+ cells in the FGT vs. blood (p= 0.005 and p=0.004 respectively) (Figure 6b). Noteworthy, while monofunctional GrzB+ MAIT cells were present in both compartments, single-producing IL-17+ MAIT cells (p=0.0009) and co-producing IL-17+IL-22+ MAIT cells were more common in the FGT (Figure 6b).
Figure 6.

Polyfunctional characterization of MAIT cells from the FGT (n=10) and blood (n=6), using SPICE software. (a) Left and right pie charts representing the number of functions expressed by MAIT cells from the FGT and blood respectively (b) Bar and pie charts showing the distribution of GrzB, IFN-γ, IL-17, IL-22 and TNF combinations expressed by MAIT cells from the FGT (blue) and blood (red). Permutation test was performed between the bar charts. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
Discussion
This is the first study to show that MAIT cells, as well as MR1+ APCs, are present in the upper and lower FGT of healthy women. MAIT cells displayed a scattered distribution throughout the FGT, except for the ectocervix where the majority localized within clusters of IL-18Rα+ cells in the epithelium. As the upper FGT is considered to be a relatively “sterile” milieu compared to the lower FGT,1,2 the preferential localization of MAIT cells in the ectocervical epithelium may serve a functional purpose by sensing potential pathogenic microbes and the commensal microbiota populating the cervicovaginal environment. For instance, the Lactobacillus species, which belong to the commensal flora of the FGT, have stimulatory effects on murine MAIT cells.12,28,29 Since activation of MAIT cells is primarily MR1-dependent,7,12,16 we also investigated the presence of MR1+ APCs in the FGT. MR1 was expressed on dendritic cells that were localized at the same anatomical sites as MAIT cells within the FGT, thus indicating that MAIT cells and MR1+ APC have the potential to interact.
MAIT cells in the FGT and in blood displayed similar frequency and a shared phenotype with expression of IL-18Rα, CD127, PD-1, and α4β7, and comparable CD4/CD8 distribution. Furthermore, in both anatomical sites MAIT cells displayed a transcription factor profile with expression of PLZF, RORγt, Helios, Eomes, and T-bet, distinct from conventional CD4+ and CD8+ T cells. These observations indicate that MAIT cells residing in the genital mucosa display an effector memory-like phenotype and thus have the capacity to act as a first line of defense against invading microbial pathogens. Interestingly, PLZF and Eomes expression was lower in MAIT cells from the FGT as compared to blood, indicating that the transcriptional profile may differ to some extent between circulating and mucosal MAIT cells.
In order to investigate the potential role of MAIT cells in the mucosal defense against microbes, we characterized the cytokine profile of FGT- and blood-derived MAIT cells in response to E. coli stimulation. Mildly-fixed E. coli was used as an ex vivo model of bacterial stimulation. E. coli is not part of the normal commensal genital microflora in healthy women and is the most common gram-negative pathogen causing anaerobic vaginitis. The prevalence of diagnosed symptomatic anaerobic vaginitis varies from 5-10% in non-pregnant women.30 Here we showed that although E. coli-stimulated MAIT cells from both compartments were capable of producing GrzB, IFN-γ, TNF, IL-17, and IL-22, the FGT-derived MAIT cells were more prone to produce IL-17 and IL-22, whereas blood MAIT cells preferentially produced IFN-γ, TNF, and GrzB. The preferential IL-17 and IL-22 production in genital mucosa was not limited to MAIT cells since also other immune cells within the FGT produced these cytokines, highlighting that the FGT environment is more predisposed for production of these cytokines.
Our stimulation data was additionally validated by assessing E. coli-induced activation of MAIT cells in the presence of an MR1-blocking antibody, which significantly reduced the production of IFN-γ, TNF, and IL-17. Notably, we observed that expression levels of GrzB and IL-22 were not sensitive to MR1 blocking. This is in agreement with previous studies showing that GrzB production by MAIT cells is highly sensitive to the influence of a range of innate, inflammatory, and homeostatic cytokines, including IL-7, IL-12, IL-15 and IL-18 in an antigen-independent and MR1-independent manner.13,31-33 This may possibly also be applicable to MAIT cell IL-22 production, but it requires further investigation.
Deeper analyses of the E. coli induced cytokine profile of MAIT cells revealed that they displayed distinct polyfunctional profiles depending on their anatomical origin. FGT-derived MAIT cells displayed a mixed Th1/Th17 phenotype, with co-expression of Th1 effector molecules and IL-17, and to a lesser extent IL-22. In contrast, circulating MAIT cells predominantly co-expressed GrzB, IFNγ, and TNF. We also observed a relatively large GrzB single-producing MAIT cell population, which may possibly represent a subset of MAIT cells that produce cytokines other than those examined in this study. Our data thus reveal that FGT-derived MAIT cells respond to bacterial stimuli in a fashion that is unique to the FGT, supporting their importance as early immune mediators of immune responses upon infection of the FGT.
This difference in cytokine production and polyfunctionality is intriguing, considering that IL-17 and IL-22 play a pivotal role in mucosal immune responses.34,35 IL-17 is crucial for expression of antimicrobial peptides and antifungal defenses in skin and mucosal tissues, and IL-22 is also involved in regulation of the mucosal barrier integrity by promoting epithelial cell proliferation and epithelial tight junction protein expression in mucosal tissues.34-37 Additionally, IL-17 and IL-22 levels are increased in genital secretions of women with various genital infections, including trichomonas, chlamydia, and gonorrhea; however the source of these cytokines in the FGT remains unclear.38-40 MAIT cells are located close to the lumen of the FGT and can thus possibly serve as sentinels for incoming pathogens. It would hence be interesting to further investigate if Chlamydia and Neisseria gonorrhoeae could stimulate cytokine production by MAIT cells, in a similar manner as shown here for E. coli. Furthermore, IL-1β and IL-6 that are known to be important for IL-17 and IL-22 responses, are present in secretions from the upper and lower FGT and are significantly upregulated during genital infections locally, but not systemically.40-42 Due to limitations in sample availability, these cytokines were not measured here. However, IL-1β and IL-6 have been shown to be higher in genital secretions compared to blood in healthy premenopausal women.43 Thus, one may speculate that the preferential IL-17 and IL-22 production by MAIT cells in the FGT may be modulated by the local microflora and cytokine environment.
The difference in functional profile between MAIT cells in the FGT and blood may also be influenced by differences in the transcriptional profile of these cells. A recent study by Rahimpour et al. showed that murine MAIT cells displayed functional plasticity associated with RORγt and T-bet expression levels resulting in either preferential IL-17 or IFN-γ production.44 Our data showed that FGT-derived MAIT cells displayed lower Eomes and PLZF expression than MAIT cells from blood. However, since the transcription factor profile of MAIT cells was assessed in unstimulated samples, due to limited sample availability, it is difficult to ascertain the role in driving the preferential functional phenotypes of MAIT cells in the FGT.
A potential caveat in this study is that FGT and blood samples were not derived from the same donors. However, all study subjects were healthy women within the same age range and none used immunosuppressive drugs. Another limitation of working with tissue biopsies obtained from the human FGT is the limited sample availability. Additionally, while it would have been preferable to distinguish the response to E. coli between the upper and lower FGT, this was not feasible due to the relatively low numbers of MAIT cells retrieved. Furthermore, sex hormones affect the FGT and the immune cell distribution within the mucosa.2 Novak et al. reported higher numbers of MAIT cells in blood from women who were of reproductive age (15-50 years of age) compared to age-matched men, suggesting that sex hormones may influence the number of MAIT cells in blood.45 Although we did not observe any differences in the frequency of MAIT cells between pre- and postmenopausal women, the impact of sex hormones on MAIT cells should be further investigated.
In summary, this is the first study to show that MAIT cells, as well as MR1+ APCs, are localized near the luminal surface of the genital mucosa of healthy women. The combination of MAIT cell localization in the mucosa and their capacity to rapidly produce cytokines suggests that they may be an important component of the first line of defense against invading pathogens. In virtue of their polyfunctionality as well as preferential IL-17 and IL-22 production compared to their circulating counterparts, mucosal MAIT cells together with other innate immunity components and the local microflora, may also act as keepers of mucosal homeostasis and barrier integrity. The present study provides a foundation for future studies of mucosal MAIT cells in acute and chronic genital infections, which will ultimately lead to a better understanding of the mechanisms regulating immunity in the FGT.
Methods
Study population and sample collection
Uterine tissue samples were obtained from 38 Swedish women who underwent hysterectomy for nonmalignant and noninflammatory conditions such as heavy menstrual bleeding or benign myoma at the St. Göran Hospital in Stockholm, Sweden. HPV- infection was diagnosed with the PapilloCheck HPV genotyping test (Greiner Bio-One GmbH, Kremsmünster, Austria) by the accredited microbiological laboratory service at the Karolinska University Hospital in Stockholm, Sweden. Peripheral blood samples were collected from healthy Swedish women in the same age range as women who underwent a hysterectomy, and were recruited at the Blood Transfusion Clinic at the Karolinska University Hospital in Stockholm, Sweden. Written informed consent was obtained from all donors and ethical approval was obtained from the Regional Ethical Review Board of Stockholm.
Processing of uterus specimens and peripheral blood mononuclear cells
Samples of endometrium and cervical mucosa were collected by a pathologist immediately after the hysterectomy. The amount of tissue obtained varied depending on the overall dimension of the surgical specimens. At least 1 cm2 of mucosa (approximately 500 mg wet weight) was required for downstream applications. Samples were maintained in ice-cold RPMI 1640 supplemented with 50 μg/ml of gentamicin and 2.5 μg/ml of Fungizone (Gibco, Life Technologies Europe BV, Stockholm, Sweden), and processed within 24 hours of surgery. For each specimen, the mucosa was separated from any residual underlying stromal or muscular tissue and dissected into approximately 8 mm3 blocks using a scalpel and tweezers, as previously described.46 One or two tissue blocks were snap-frozen immediately after dissection and cryopreserved at -80°C for in situ staining. The remaining tissue blocks were digested with 0.1 mg/ml of DNase I (Roche, Basel, Switzerland) and 0.5 mg/ml of Collagenase II (Sigma-Aldrich, St. Louis, MO, USA) in a thermoshaker (Labnet International, Edison, NJ, USA) rocking at 1400 rpm for 30 min at 37°C. Digested tissue blocks were mechanically disrupted with a pestle. The obtained cell suspension was filtered through a 70-μm cell strainer (BD Biosciences, San Jose, CA, USA) and washed in phosphate-buffered saline (PBS) by centrifugation at 400×g for 5 min. For flow cytometry, mononuclear cells (MNCs) were isolated by density gradient centrifugation at 900× g for 20 min using Ficoll-Hypaque (Axis-Shield, Dundee, Scotland). Peripheral blood mononuclear cells (PBMC) were isolated by Ficoll-Hypaque density gradient centrifugation and either allowed to rest overnight in complete medium before use in the functional assay (see below) or cryopreserved in liquid nitrogen until required for the phenotypic analysis (see below).
In situ fluorescence staining
In situ staining was performed on 8-μm thick sections of the cryopreserved tissue samples. The tissue sections were fixed in 2% formaldehyde for 10 min and then washed with PBS. Immunofluorescent double-staining of Vα7.2 and IL-18Rα; Vα7.2 and CD3; Vα7.2 and CD8; CD3 and CD8 as well as of MR1 and HLA-DR, MR1 and CD1 1c; MR1 and Langerin were done sequentially. The following monoclonal primary antibodies were used: mouse anti-human Vα7.2 antibody (clone 3C10, BioLegend, San Diego, CA, USA); goat anti-human IL-18Ra antibody (AF840, R&D Systems, Minneapolis, MN, USA); rabbit anti-human CD3 antibody (clone SP7, Abcam, Cambridge, UK); Alexa 488 conjugated mouse anti-human CD8 antibody (clone RPA-T8, BD Biosciences); mouse anti-human MR1 antibody (clone 8F2.F9,47 a kind gift from Dr. Ted Hansen); biotinylated mouse anti-human HLA-DR antibody (clone L243, BD Biosciences) that was used in combination with streptavidin-conjugated Alexa Fluor 488 (Molecular Probes, Life Technologies); FITC conjugated mouse anti-human CD11c (clone B-ly6, BD Biosciences); and rat anti-human Langerin (clone 929F3.01, Dendritics, Lyon, France). The following secondary antibodies were used: Alexa Fluor 594 or 488-conjugated donkey anti-mouse IgG antibody; Alexa Fluor 488-conjugated donkey anti-goat IgG antibody; Alexa Fluor 488-conjugated donkey anti-rat IgG antibody; Alexa Fluor 594-conjugated donkey anti-rabbit IgG antibody (Molecular Probes, Life Technologies Europe BV, Stockholm, Sweden). The tissue sections were mounted with Vectashield containing DAPI (Vector Laboratories, Burlingame, CA, USA). Negative controls were included and consisted of incubations in the presence of secondary antibody alone. Images were acquired on a DMR-X microscope (Leica, Wetzlar, Germany) with a Retiga 2000R camera (QImaging, Surrey, Canada). Acquired images were processed using Image-Pro Premier 9.1 software (Media Cybernetics, Rockville, MD, USA).
Flow cytometry
Cell-surface staining was performed using directly-conjugated antibodies and cells were fixed in Cytofix/Cytoperm or in Transcription Factor Fixation/Permeabilization buffer (both from BD Biosciences) as appropriate. Intracellular staining was performed in Perm/Wash or Transcription Factor Perm/Wash buffer as appropriate (both from BD Biosciences). Samples were acquired on an LSRFortessa flow cytometer (BD Biosciences) equipped with 405, 488, 561, and 639 nm lasers. Single-stained polystyrene beads (BD Biosciences) were used for compensation purposes. Software-based compensation was performed using the compensation platform in FlowJo software version 9.6 (Tree Star, Ashland, OR, USA). Distribution of effector molecules expressed by MAIT cells was compared using SPICE software version 5.35.48 Antibodies used in the experiments are listed in Supplementary Table 2.
Functional assay
MAIT cell functions were determined in vitro using a formaldehyde-fixed E. coli stimulation (D21 strain, fixed in 1% formaldehyde for 5 min multiplicity of infection=5) in the presence of 1.25 μg/ml anti-CD28 mAb (clone L293, BD Biosciences) and, in selected experiments, 20 μg/ml anti-MR1 mAb (clone 26.5; Biolegend) or IgG2 isotype control (clone MOPC-173, BioLegend). PBMCs or FGT-derived MNCs were further cultured for 24 hours at 37°C and 5% CO2 in RPMI medium supplemented with 10% fetal calf serum and 50 μg/ml gentamicin (Gibco). Monensin (Golgi Stop, BD Biosciences) was added during the last 6 hours of the stimulation. Cells stimulated for 6 h with PMA/ionomycin (Leukocyte Activation Cocktail, BD Biosciences) and in the presence of monensin were included in parallel as positive controls.
Statistical analyses
Statistical significance between continuous variables was assessed using the Mann-Whitney U test for comparisons of independent samples and the Wilcoxon signed rank test for paired samples. Furthermore, multiple comparison analysis were performed with the use of the Kruskal-Wallis test followed by Dunn's post-hoc test for independent samples and the Friedman test followed by Dunn's post-hoc test for paired samples. Prism 5.00 for Windows (GraphPad Software, CA, USA) was used for statistical analysis and a p-value <0.05 was considered significant. Permutation tests were analyzed using the data analysis program SPICE version 5.35.48
Supplementary Material
Supplementary Figure 1. (a) Representative plot showing the co-expression of CD161 on CD45+IL-18Rα+Vα7.2+ and co-expression of IL-18Rα on CD45+CD3+CD161highVα7.2+ (MAIT) cells obtained from cervix. (b) Representative histograms of one of three replicate experiments showing the expression levels (GMFI, geometric mean intensity fluorescence) of IL-18Rα, CD127, α4β7, and PD-1 in MAIT cells (red), CD4+ T cells (blue), and CD8+ T cells (green) from the endometrium, cervix and blood.
Supplementary Figure 2. Localization and spatial distribution of Vα7.2+T cells and CD8+T cells in the FGT. Representative immunofluorescence images of (a) endometrial, (b) endocervical, (c) transformation zone, and (d) ectocervical tissue sections stained for CD3+ (red) and Vα7.2+ (green) cells in the first three columns and for CD3+ (red) and CD8+ (green) in the last column. Double-positive cells are shown in yellow, Va7.2+T cells are indicated by the white arrows. DAPI (blue) was used as a counterstain for visualization of cell nuclei. The images were collected with 40× and 20× objectives. The scale bars are 60 μm in the images in the first three columns and 200 μm in the images in the last column.
Supplementary Figure 3. Scatter plots represent the expression levels of PLZF, RORγt, Helios, Eomes, and T-bet transcription factors in MAIT cells (red), CD4+ T cells (blue), and CD8+ T cells (green) from the endometrium (n=7), cervix (n=4), and blood (n=6). Each symbol represents a different patient; endometrium (circle), cervix (triangle), and blood (square). Horizontal lines represent the median ± interquartile range. *p<0.05.
Supplementary Figure 4. Representative histogram and dot plots showing IFN-γ, TNF, IL-17, IL-22 and GrzB production by MAIT cells (a) from three donors, in unstimulated controls (black line) and upon stimulation with E.coli alone (blue line) and in the presence of α-CD28 (red line); (b) from FGT-derived cells of three donors, in unstimulated controls (upper panel) and upon stimulation with E. coli in the presence of the IgG2a isotype control (middle panel) or the MR1- blocking antibody (lower panel).
Supplementary Figure 5. Cytokine production by immune cells in the FGT (n=10) vs. blood (n=6). (a) Bar chart represents fold change in IL-17, IL-22, IFN-γ, and TNF production by CD45+ lymphocytes from FGT vs. blood. (b) Pie charts of compiled data showing percentage of median values of IL-17, IL-22, IFN-γ, and TNF production in the FGT and blood by CD3-CD45+ (red) and CD3+CD45+ (blue) cells as well as by MAIT, CD4+, CD8+, CD4-CD8- and other cells; the different shades of blue represent different T cell subsets. (c) Scatter plot represents IL-17 and IL-22 production by CD4+ T cells from the FGT and blood. Each symbol represents a different patient; FGT (circle) and blood (square). Horizontal lines represent median ± interquartile range. ***P<0.001.
Supplementary Table 1. Characteristics of the patients undergoing hysterectomy
Supplementary Table 2. Antibodies used in flow cytometry
Acknowledgments
We thank all study participants as well as Dr. Flam, Dr. Glaessgen, Dr. Kaldensjö and Dr. Bradley for their assistance in collecting cervical tissue samples. A.G. was supported by funds from the Karolinska Instititutet's faculty funds. E.L. was supported by funds from the Clas Groschinsky Memorial Funds, the Swedish Institute Swedish Physicians against AIDS Foundation, and the Swedish Society for Medicine. A.I. was supported by the Blanceflor Boncompagni Ludovisi, née Bildt Foundation. K.B. was supported by the Swedish Research Council. J.K.S. was supported by the Swedish Cancer Society, the Petrus and Augusta Hedlund Foundation, the Swedish Research Council, and the US National Institutes of Health grant R01DK108350. A.T. was supported by grants from the Clas Groschinsky Memorial Funds, and the Swedish Society of Medicine.
Footnotes
Disclosure: The authors declare no conflicts of interests.
References
- 1.Quayle AJ. The innate and early immune response to pathogen challenge in the female genital tract and the pivotal role of epithelial cells. J Reprod Immunol. 2002;57:61–79. doi: 10.1016/s0165-0378(02)00019-0. [DOI] [PubMed] [Google Scholar]
- 2.Wira CR, Rodriguez-Garcia M, Patel MV. The role of sex hormones in immune protection of the female reproductive tract. Nature reviews Immunology. 2015 doi: 10.1038/nri3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pudney J, Quayle AJ, Anderson DJ. Immunological microenvironments in the human vagina and cervix: mediators of cellular immunity are concentrated in the cervical transformation zone. Biology of reproduction. 2005;73:1253–1263. doi: 10.1095/biolreprod.105.043133. [DOI] [PubMed] [Google Scholar]
- 4.Boily MC, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis. 2009;9:118–129. doi: 10.1016/S1473-3099(09)70021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burgener A, et al. A systems biology examination of the human female genital tract shows compartmentalization of immune factor expression. J Virol. 2013;87:5141–5150. doi: 10.1128/JVI.03347-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valore EV, Park CH, Igreti SL, Ganz T. Antimicrobial components of vaginal fluid. Am J Obstet Gynecol. 2002;187:561–568. doi: 10.1067/mob.2002.125280. [DOI] [PubMed] [Google Scholar]
- 7.Treiner E, et al. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422:164–169. doi: 10.1038/nature01433. [DOI] [PubMed] [Google Scholar]
- 8.Dusseaux M, et al. Human MAIT cells are xenobiotic-resistant, tissue-targeted, CD161hi IL-17-secreting T cells. Blood. 2011;117:1250–1259. doi: 10.1182/blood-2010-08-303339. [DOI] [PubMed] [Google Scholar]
- 9.Martin E, et al. Stepwise development of MAIT cells in mouse and human. PLoS Biol. 2009;7:e54. doi: 10.1371/journal.pbio.1000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reantragoon R, et al. Antigen-loaded MR1 tetramers define T cell receptor heterogeneity in mucosal-associated invariant T cells. The Journal of experimental medicine. 2013;210:2305–2320. doi: 10.1084/jem.20130958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lepore M, et al. Parallel T-cell cloning and deep sequencing of human MAIT cells reveal stable oligoclonal TCRbeta repertoire. Nature communications. 2014;5:3866. doi: 10.1038/ncomms4866. [DOI] [PubMed] [Google Scholar]
- 12.Le Bourhis L, et al. Antimicrobial activity of mucosal-associated invariant T cells. Nature immunology. 2010;11:701–708. doi: 10.1038/ni.1890. [DOI] [PubMed] [Google Scholar]
- 13.Leeansyah E, et al. Arming of MAIT Cell Cytolytic Antimicrobial Activity Is Induced by IL-7 and Defective in HIV-1 Infection. PLoS pathogens. 2015;11:e1005072. doi: 10.1371/journal.ppat.1005072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaech SM, Cui W. Transcriptional control of effector and memory CD8+ T cell differentiation. Nature reviews Immunology. 2012;12:749–761. doi: 10.1038/nri3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akimova T, Beier UH, Wang L, Levine MH, Hancock WW. Helios expression is a marker of T cell activation and proliferation. PloS one. 2011;6:e24226. doi: 10.1371/journal.pone.0024226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kjer-Nielsen L, et al. MR1 presents microbial vitamin B metabolites to MAIT cells. Nature. 2012;491:717–723. doi: 10.1038/nature11605. [DOI] [PubMed] [Google Scholar]
- 17.Corbett AJ, et al. T-cell activation by transitory neo-antigens derived from distinct microbial pathways. Nature. 2014;509:361–365. doi: 10.1038/nature13160. [DOI] [PubMed] [Google Scholar]
- 18.Leeansyah E, Loh L, Nixon DF, Sandberg JK. Acquisition of innate-like microbial reactivity in mucosal tissues during human fetal MAIT-cell development. Nature communications. 2014;5:3143. doi: 10.1038/ncomms4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakala IG, et al. Functional Heterogeneity and Antimycobacterial Effects of Mouse Mucosal-Associated Invariant T Cells Specific for Riboflavin Metabolites. Journal of immunology. 2015;195:587–601. doi: 10.4049/jimmunol.1402545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gold MC, et al. Human mucosal associated invariant T cells detect bacterially infected cells. PLoS Biol. 2010;8:e1000407. doi: 10.1371/journal.pbio.1000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saba E, et al. HIV-1 sexual transmission: early events of HIV-1 infection of human cervico-vaginal tissue in an optimized ex vivo model. Mucosal immunology. 2010;3:280–290. doi: 10.1038/mi.2010.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaldensjo T, et al. Detection of intraepithelial and stromal Langerin and CCR5 positive cells in the human endometrium: potential targets for HIV infection. PloS one. 2011;6:e21344. doi: 10.1371/journal.pone.0021344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirbod T, et al. Abundant and superficial expression of C-type lectin receptors in ectocervix of women at risk of HIV infection. Journal of acquired immune deficiency syndromes (1999) 2009;51:239–247. doi: 10.1097/QAI.0b013e3181a74f89. [DOI] [PubMed] [Google Scholar]
- 24.Carolan E, et al. Altered distribution and increased IL-17 production by mucosal-associated invariant T cells in adult and childhood obesity. Journal of immunology. 2015;194:5775–5780. doi: 10.4049/jimmunol.1402945. [DOI] [PubMed] [Google Scholar]
- 25.Hiejima E, et al. Reduced Numbers and Proapoptotic Features of Mucosal-associated Invariant T Cells as a Characteristic Finding in Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1529–1540. doi: 10.1097/MIB.0000000000000397. [DOI] [PubMed] [Google Scholar]
- 26.Tang XZ, et al. IL-7 licenses activation of human liver intrasinusoidal mucosal-associated invariant T cells. Journal of immunology. 2013;190:3142–3152. doi: 10.4049/jimmunol.1203218. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez-Garcia M, Barr FD, Crist SG, Fahey JV, Wira CR. Phenotype and susceptibility to HIV infection of CD4+ Th17 cells in the human female reproductive tract. Mucosal immunology. 2014;7:1375–1385. doi: 10.1038/mi.2014.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vasquez A, Jakobsson T, Ahrne S, Forsum U, Molin G. Vaginal Lactobacillus Flora of Healthy Swedish Women. Journal of Clinical Microbiology. 2002;40:2746–2749. doi: 10.1128/JCM.40.8.2746-2749.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ravel J, et al. Vaginal microbiome of reproductive-age women. Proceedings of the National Academy of Sciences of the United States of America. 2011;108 Suppl 1:4680–4687. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tansarli GS, Kostaras EK, Athanasiou S, Falagas ME. Prevalence and treatment of aerobic vaginitis among non-pregnant women: evaluation of the evidence for an underestimated clinical entity. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 2013;32:977–984. doi: 10.1007/s10096-013-1846-4. [DOI] [PubMed] [Google Scholar]
- 31.Ussher JE, et al. CD161++ CD8+ T cells, including the MAIT cell subset, are specifically activated by IL-12+IL-18 in a TCR-independent manner. European journal of immunology. 2014;44:195–203. doi: 10.1002/eji.201343509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kurioka A, et al. MAIT cells are licensed through granzyme exchange to kill bacterially sensitized targets. Mucosal immunology. 2015;8:429–440. doi: 10.1038/mi.2014.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sattler A, Dang-Heine C, Reinke P, Babel N. IL-15 dependent induction of IL-18 secretion as a feedback mechanism controlling human MAIT-cell effector functions. European journal of immunology. 2015;45:2286–2298. doi: 10.1002/eji.201445313. [DOI] [PubMed] [Google Scholar]
- 34.Sonnenberg GF, Fouser LA, Artis D. Border patrol: regulation of immunity, inflammation and tissue homeostasis at barrier surfaces by IL-22. Nature immunology. 2011;12:383–390. doi: 10.1038/ni.2025. [DOI] [PubMed] [Google Scholar]
- 35.Weaver CT, Elson CO, Fouser LA, Kolls JK. The Th17 pathway and inflammatory diseases of the intestines, lungs, and skin. Annual review of pathology. 2013;8:477–512. doi: 10.1146/annurev-pathol-011110-130318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Puel A, et al. Inborn errors of human IL-17 immunity underlie chronic mucocutaneous candidiasis. Current opinion in allergy and clinical immunology. 2012;12:616–622. doi: 10.1097/ACI.0b013e328358cc0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim CJ, et al. A role for mucosal IL-22 production and Th22 cells in HIV-associated mucosal immunopathogenesis. Mucosal immunology. 2012;5:670–680. doi: 10.1038/mi.2012.72. [DOI] [PubMed] [Google Scholar]
- 38.Makinde HM, et al. IL-22 levels are associated with Trichomonas vaginalis infection in the lower genital tract. American journal of reproductive immunology. 2013;70:38–44. doi: 10.1111/aji.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jha R, et al. Spontaneous secretion of interleukin-17 and -22 by human cervical cells in Chlamydia trachomatis infection. Microbes and infection / Institut Pasteur. 2011;13:167–178. doi: 10.1016/j.micinf.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 40.Masson L, et al. Defining genital tract cytokine signatures of sexually transmitted infections and bacterial vaginosis in women at high risk of HIV infection: a cross-sectional study. Sexually transmitted infections. 2014;90:580–587. doi: 10.1136/sextrans-2014-051601. [DOI] [PubMed] [Google Scholar]
- 41.Zielinski CE, et al. Pathogen-induced human TH17 cells produce IFN-gamma or IL-10 and are regulated by IL-1beta. Nature. 2012;484:514–518. doi: 10.1038/nature10957. [DOI] [PubMed] [Google Scholar]
- 42.Boomsma CM, et al. Cytokine profiling in endometrial secretions: a non-invasive window on endometrial receptivity. Reprod Biomed Online. 2009;18:85–94. doi: 10.1016/s1472-6483(10)60429-4. [DOI] [PubMed] [Google Scholar]
- 43.Al-Harthi L, et al. The impact of the ovulatory cycle on cytokine production: evaluation of systemic, cervicovaginal, and salivary compartments. J Interferon Cytokine Res. 2000;20:719–724. doi: 10.1089/10799900050116426. [DOI] [PubMed] [Google Scholar]
- 44.Rahimpour A, et al. Identification of phenotypically and functionally heterogeneous mouse mucosal-associated invariant T cells using MR1 tetramers. The Journal of experimental medicine. 2015;212:1095–1108. doi: 10.1084/jem.20142110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Novak J, Dobrovolny J, Novakova L, Kozak T. The decrease in number and change in phenotype of mucosal-associated invariant T cells in the elderly and differences in men and women of reproductive age. Scandinavian journal of immunology. 2014;80:271–275. doi: 10.1111/sji.12193. [DOI] [PubMed] [Google Scholar]
- 46.Introini A, Vanpouille C, Grivel JC, Margolis L. An Model of HIV-1 Infection in Human Lymphoid Tissue and Cervico-vaginal Tissue. Bio Protoc. 2014;4 doi: 10.21769/bioprotoc.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chua WJ, et al. Endogenous MHC-related protein 1 is transiently expressed on the plasma membrane in a conformation that activates mucosal-associated invariant T cells. Journal of immunology. 2011;186:4744–4750. doi: 10.4049/jimmunol.1003254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roederer M, Nozzi JL, Nason MC. SPICE: exploration and analysis of post-cytometric complex multivariate datasets. Cytometry Part A : the journal of the International Society for Analytical Cytology. 2011;79:167–174. doi: 10.1002/cyto.a.21015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. (a) Representative plot showing the co-expression of CD161 on CD45+IL-18Rα+Vα7.2+ and co-expression of IL-18Rα on CD45+CD3+CD161highVα7.2+ (MAIT) cells obtained from cervix. (b) Representative histograms of one of three replicate experiments showing the expression levels (GMFI, geometric mean intensity fluorescence) of IL-18Rα, CD127, α4β7, and PD-1 in MAIT cells (red), CD4+ T cells (blue), and CD8+ T cells (green) from the endometrium, cervix and blood.
Supplementary Figure 2. Localization and spatial distribution of Vα7.2+T cells and CD8+T cells in the FGT. Representative immunofluorescence images of (a) endometrial, (b) endocervical, (c) transformation zone, and (d) ectocervical tissue sections stained for CD3+ (red) and Vα7.2+ (green) cells in the first three columns and for CD3+ (red) and CD8+ (green) in the last column. Double-positive cells are shown in yellow, Va7.2+T cells are indicated by the white arrows. DAPI (blue) was used as a counterstain for visualization of cell nuclei. The images were collected with 40× and 20× objectives. The scale bars are 60 μm in the images in the first three columns and 200 μm in the images in the last column.
Supplementary Figure 3. Scatter plots represent the expression levels of PLZF, RORγt, Helios, Eomes, and T-bet transcription factors in MAIT cells (red), CD4+ T cells (blue), and CD8+ T cells (green) from the endometrium (n=7), cervix (n=4), and blood (n=6). Each symbol represents a different patient; endometrium (circle), cervix (triangle), and blood (square). Horizontal lines represent the median ± interquartile range. *p<0.05.
Supplementary Figure 4. Representative histogram and dot plots showing IFN-γ, TNF, IL-17, IL-22 and GrzB production by MAIT cells (a) from three donors, in unstimulated controls (black line) and upon stimulation with E.coli alone (blue line) and in the presence of α-CD28 (red line); (b) from FGT-derived cells of three donors, in unstimulated controls (upper panel) and upon stimulation with E. coli in the presence of the IgG2a isotype control (middle panel) or the MR1- blocking antibody (lower panel).
Supplementary Figure 5. Cytokine production by immune cells in the FGT (n=10) vs. blood (n=6). (a) Bar chart represents fold change in IL-17, IL-22, IFN-γ, and TNF production by CD45+ lymphocytes from FGT vs. blood. (b) Pie charts of compiled data showing percentage of median values of IL-17, IL-22, IFN-γ, and TNF production in the FGT and blood by CD3-CD45+ (red) and CD3+CD45+ (blue) cells as well as by MAIT, CD4+, CD8+, CD4-CD8- and other cells; the different shades of blue represent different T cell subsets. (c) Scatter plot represents IL-17 and IL-22 production by CD4+ T cells from the FGT and blood. Each symbol represents a different patient; FGT (circle) and blood (square). Horizontal lines represent median ± interquartile range. ***P<0.001.
Supplementary Table 1. Characteristics of the patients undergoing hysterectomy
Supplementary Table 2. Antibodies used in flow cytometry


