Abstract
Proteomics has been widely used in the last few years to look for new biomarkers and decipher the mechanism of HIV–host interaction. Herein, we review the recent developments of HIV/AIDS proteomic research, including the samples used in HIV/AIDS related research, the technologies used for proteomic study, the diagnosis biomarkers of HIV-associated disease especially HIV-associated neurocognitive impairment, the mechanisms of HIV–host interaction, HIV-associated dementia, substance abuse, and so on. In the end of this review, we also give some prospects about the limitation and future improvement of HIV/AIDS proteomic research.
Key words: proteomics, HIV, biomarker, HIV–host interaction
Introduction
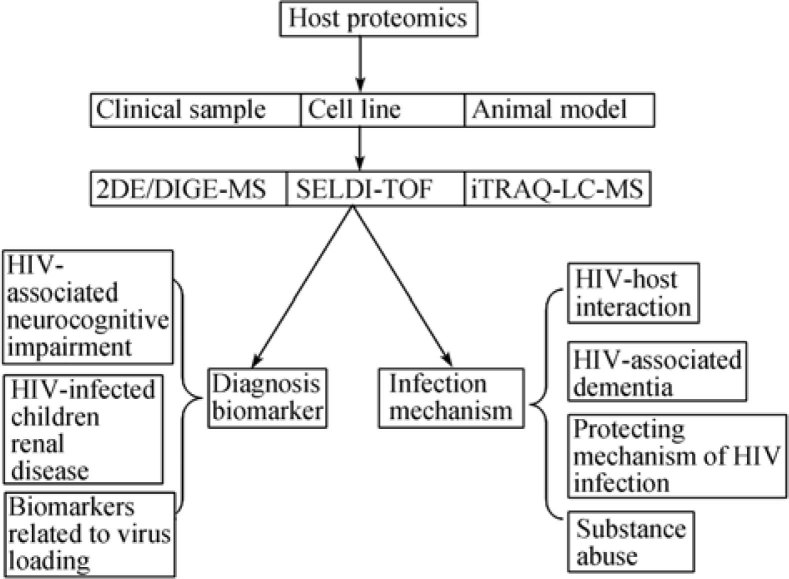
Human immunodeficiency virus (HIV) is recognized to be one of the most destructive pandemics in recorded history. Effective highly active antiretroviral therapy and the availability of genetic screening of patient virus data have led to sustained viral suppression and higher life expectancy in patients who have been infected with HIV. However, due to the complexity of HIV infection, virus mutation and drug resistance, the knowledge of HIV infection, HIV-associated disease, as well as the treatment of these diseases is very limited. Despite the massive amount of scientific data have been obtained via genomics, additional methodologies are needed to help understanding these diseases and to provide novel methods for diagnosis and treatment. Proteomics is one such methodology that is increasingly being used as a tool to study a variety of disease states. As reviewed by List et al. (1), proteomics has been widely used to study infection diseases, including for biomarkers of HIV-induced neurocognitive impairment through surface-enhanced laser desorption/ionization mass spectrometry (SELDI-MS), matrix-assisted laser desorption/ionization mass spectrometry (MALDI- MS) technologies, and protein arrays for immune response in HIV-infected patients. Proteomics has also been used to decipher the complex mechanisms in neurodegenerative diseases including HIV-associated neurodegenerative disorder, as reviewed by Noorbakhsh et al. (2). However, these two reviews 1, 2 only partly described the development in HIV/AIDS. Furthermore, there are some new developments in HIV research after these two reviews. So in this review, we systematically summarized the HIV-infected host proteomic research in HIV/AIDS, especially in the last two years (Figure 1).
Figure 1.
Illustration of the host proteome research in HIV infection.
Samples Used in HIV/AIDS Research
Clinical samples
In order to find biomarkers and understand the mechanism of HIV infection, many kinds of samples have been used for proteomic research, including sera/plasma from HIV-infected individuals with or without cognitive impairment (CI) 3, 4, cerebrospinal fluid (CSF) 5, 6, brain tissue (6), cell extraction (7), monocytes of HIV-infected women (8), lavage from sex worker (9), formalin fixed paraffin embedded oral HPV lesions from HIV-positive patients (10), and placental macrophages separated from HIV-infected patients (11).
HIV infection cell models
There are several cell models to imitate HIV infection, including human T-lymphocyte cell line PM1 stimulated with C33A-produced virus stocks of the HIV-1 LAI molecular clone (7), the T-cell line infected by a biological clone of HIV-1 (X4 strain) (12), the separated placental macrophages and blood borne monocyte-derived macrophages (MDMs) inoculated with 25 ng of HIV-1BaL per 2×105 cells (11), separated CD4 cells from healthy donors stimulated with autologous serum for 24 h in the presence of 400 pg/mL recombinant interleukin-2 (13), and HEK 293T cells transfected with pTat and flag NC gene of HIV (11).
For cells that cannot be directly infected, some modifications are made. For example, Wang et al. 14, 15 separated neurons, microglia and astrocytes from embryonic 18-day-old fetuses of C57BL/6 mice. Then vesicular stomatitis virus pseudotyped HIV-1 strain YU2 (HIV-1/VSV) was used to circumvent the required viral/cellular receptors necessary to infect mouse cells.
Monkey models
Since HIV only infects primates, monkeys are the main animals for HIV research. Bonneh-Barkay et al. (6) obtained a simian immunodeficiency virus (SIV)-infection model to study proteins related to virus loading through pigtailed macaques Macaca nemestrina model. In this model, macaques were in age from 74 to 93 months, and were intravenously infected with SIVDeltaB670 viral swarm. The time of infection varied from 42 to 287 days (6). Pendyala et al. (5) used another monkey model in which Rhesus monkeys Macaca mulatta were infected with SIV.
Subcellular proteome
The proteins in whole cell or tissue are very complex. In order to decrease the complexness and discover more low abundant proteins, some researchers focus their studies on subcellular proteome, including plasma membrane 16, 17, secretome (18), exosome (19), mitochondria (20), and so on.
Proteomics Technologies
There are three general technology lines, including two-dimensional electrophoresis (2DE) or difference gel electrophoresis mass spectrometry (DIGE-MS) 7, 9, 17, surface-enhanced laser desorption/ionization time-of-flight mass spectrometry (SELDI-TOF-MS) 3, 6, and isobaric tag for relative and absolute quantitation (iTRAQ) labeling (10) followed by liquid chromatography (LC) separation and MS identification (5). Of these three kinds of technologies, DIGE-MS is used mostly, followed by SELDI-TOF-MS.
Biomarkers of HIV-associated Disease
HIV-associated neurocognitive impairment
HIV-1 penetrates the brain shortly after infection and remains there throughout entire disease. Approximately 50% of infected individuals develop some forms of CI ranging from an asymptomatic form diagnosed during formal testing to the most severe HIV-associated dementia (HAD) leading to death (21). In order to uncover biomarkers of HAD, proteomic approaches have been widely used. Wiederin et al. (3) analyzed the sera from HIV-infected individuals with or without CI through SELDI-TOF-MS analysis followed by weak cation exchange chromatography and one-dimensional electrophoresis, and discovered gelsolin and prealbumin as differentially expressed proteins. Laspiur et al. (22) used an integrated proteomic platform to assess cerebrospinal fluid protein profiles from 50 HIV-1 seropositive Hispanic women, and found that macrophage capping protein L-plastin and Cu/Zn superoxide dismutase (Cu/Zn SOD) were only detected in CSF with CI (22). Another research (8) showed a decreased Cu/Zn SOD activity in CSF with CI than with asymptomatics and normal cognition. Rozek et al. (23) reported that Vitamin D binding protein, clusterin, gelsolin, complement C3, procollagen C-endopeptidase enhancer 1, and cystatin C were up-regulated in HAD through 2D-DIGE analysis.
HIV-infected children renal disease
HIV-infected children usually develop renal disease, and have the risk of performing renal biopsies. To identify new diagnosis biomarkers, Soler-Garcia et al. (24) carried out urine proteomic analysis for HIV-infected children with renal disease. High urine levels of β2-microglobulin and retinol-binding protein suggested the presence of tubular injury. Elevated urine levels of iron and the iron-related proteins, transferrin, hemopexin, haptoglobin, lactoferrin, and neutrophil gelatinase-associated lipocalin were also found in children with HIV-nephropathy (HIVAN) and HIV-associated hemolytic uremic syndrome (HIV-HUS). These iron and iron-related proteins might be promising candidate urine biomarkers to identify HIV-infected children at risk of developing HIVAN and HIV-HUS. The release or accumulation of iron in the kidney of HIV-infected children may contribute to the rapid progression of their renal disease, and could become a new therapeutic target against HIVAN and HIV-HUS.
Biomarkers related to virus loading
Detection of virus loading is very expensive although it is the gold standard for the prognosis of AIDS. So it is very important to develop new biomarkers for replacing virus loading. Through proteomic analysis of postmortem CSF and brain tissue from the SIV primate model, Bonneh-Barkay et al. (6) found that Chitinase-3-like protein 1 (YKL-40) was tightly associated with lentiviral encephalitis and up-regulated with an increase in CSF viral load.
Mechanism of HIV Infection
HIV–host interaction
HIV-1 interacts through multiple signaling pathways to reprogram the transcriptome and the proteome of host cells. HIV-1-induced stimulation of macrophages is a multi-step process that occurs directly in infected cells, as well as indirectly in bystander cells through paracrine signaling. Emerging genomic and proteomic techniques have elucidated a myriad of cellular genes involved in viral replication representing a collection of possible new drug targets. For example, in the study of Ringrose et al. (7), human T cells upon HIV-1 infection showed that 15% of 2,000 protein spots were differentially expressed at peak infection, in which 27 proteins were found to be significantly down-regulated and 66 were up-regulated at peak HIV infection. Early in infection, only a small group of proteins were changed. A clear and consistent program of metabolic rerouting of HIV causing host cell apoptosis through mitochondrial-dependent pathway was reported (20). The proteome of apoptotic T cells includes prominent fragments of cellular proteins generated by caspases. A high proportion of distinct T cell epitopes in these fragments is recognized by CD8+ T cells during HIV infection. The frequencies of effector CD8+ T cells that are specific for apoptosis-dependent epitopes correlate with the frequency of circulating apoptotic CD4+ T cells in HIV-1-infected individuals (25). Another research (17) showed that one functional consequence of virus-exposure to the monocyte was the facilitation of protein transformation from the cytosol to the plasma membrane. HIV-1-induced plasma membrane protein translocation was associated with cathepsin B- and caspase 9, 3-dependent apoptosis. Furthermore, Rasheed et al. (12) found that HIV replication alone could induce novel cellular enzymes and proteins that are significantly associated with biologically relevant processes involved in lipid synthesis, transport and metabolism. Proteomic research by Pathak et al. (26) also showed that HIV induces both a down-regulation of Interleukin-1 receptor-associated kinase 4 (IRAK-4) that impairs Toll-like receptor (TLR) signaling and an up-regulation of the antibiotic peptide dermcidin in monocytic cells. The decreased immune response resulted in HIV-infected individuals with an increased risk of invasive bacterial infections, even at early clinical stages with relatively normal CD4+ T-cell counts. In all, along each step of the viral life cycle, viral RNA and proteins encounter as many as 250 host cell factors that either facilitate or restrict viral infection (27). Dyer et al. (28) integrated human–pathogen protein–protein interactions (PPIs) for 190 pathogen strains from seven public databases. Nearly all of the 10,477 human–pathogen PPIs are for viral systems (98.3%), with the majority belonging to the human–HIV system (77.9%). They found that both viral and bacterial pathogens tend to interact with hubs (proteins with many interacting partners) and bottlenecks (proteins that are central to many paths in the network) in the human PPI network.
Apart from these researches considering the whole HIV interaction with host cells, there are also many studies thinking about the affection of function proteins in HIV to host, where the virus proteins also strongly influence levels of proteins involved in host proteins.
A quantitative proteomics analysis (29) using the plasma membrane fraction of HeLa cells expressing either wild-type Vpu or a Vpu mutant (S52N/S56N) that does not bind betaTrCP showed that one cellular protein, BST-2 (CD317), was consistently underrepresented in the membrane proteome of cells expressing wild-type Vpu compared to the proteome of cells expressing the Vpu mutant. BST-2 down-regulation occurred in a Vpu-dependent manner in the trans-Golgi network or in early endosomes, leading to lysosomal degradation of BST-2.
Moreover, proteomics was used to study the interaction between the Tat and nucleocapsid proteins 30, 31. Gautier et al. (31) has designed a proteomic strategy based on affinity chromatography coupled with MS. A total of 183 proteins were identified as Tat nuclear partners, 90% of which have not been previously characterized. These proteins are enriched for domains mediating protein, RNA and DNA interactions, as well as helicase and ATPase activities.
Proteomics was also used to study the interaction between HIV-1 viral protein R (Vpr) and host cells. For example, He et al. (32) infected C8166 cells with a recombinant adenovirus carrying both vpr and GFP genes (rAd-vpr), as well as the vector control virus (rAd-vector), and found apoptosis related protein changes, exhibiting the regulation of caspase-3 activity indicator proteins (vimentin and Rho GDP-dissociation inhibitor 2), mitochondrial protein (prohibitin) and other regulatory proteins. The up-regulation of anti-inflammatory redox protein, thioredoxin, was identified in the rAd-vpr infected group and the increase of caspase 3&7 activity in the rAd-vpr infected group was observed. Endogenous Vpr is able to kill HTLV-1 transformed C8166 cells, and may avoid the risks of inducing severe inflammatory responses through apoptosis-inducing and anti-inflammatory activities.
Another application of proteomics is to study the interaction between HIV-1 viral protein Vpx and host cells. Using biochemical and proteomic approaches, Srivastava et al. (33) found that Vpx protein of the pathogenic SIVmac 239 strain associates with a ternary protein complex comprising DDB1 and VprBP subunits of Cullin 4-based E3 ubiquitin ligase, and DDA1, which has been implicated in the regulation of E3 catalytic activity, and that Vpx participates in the Cullin 4 E3 complex comprising VprBP.
HIV-associated dementia (HAD)
Despite the availability of highly active antiretroviral therapy, HAD continues to affect approximately 10% of AIDS patients usually in the later stages of disease. HIV-1-associated neurocognitive disorder (HAND) is a complication marked by cognitive, behavioral, and motor dysfunction that develops during the later stages of AIDS. The pathological hallmarks of HAND are characterized by microglia cell activation, astrocytosis, decreased synaptic function, leukocyte infiltration, multinucleated giant cells and selective neuronal loss. Microglia/macrophages are the most commonly infected cells in the brain and serve as lifelong hosts for HIV. Microglial HIV infection and viral replication result in the secretion of neurotoxic pro-inflammatory cytokines, chemokines and viral proteins that strongly implicate microglia hyper-activation in the progression of HAND. So far, most research showed that the cardinal neuropathological features of HAD are represented by multinucleated giant cells, viral antigens and genomes in macrophages and microglia, diffuse myelin pallor, microglial nodules and synapto-dendritic pruning with neuronal loss (34). As reviewed by Noorbakhsh et al. (2), two main mechanisms have been considered in the neuropathogenesis of HAD: (1) HIV-encoded proteins, including gp120, Tat and Vpr, released by infected monocytoid cells exert direct neurotoxic effects 35, 36; (2) activated macrophages, microglia and astrocytes produce multiple host proinflammatory molecules and neurotoxins that contribute to neuronal dysfunction and death 35, 36.
HAD-descriptive analyses uncovered inflammation mechanism in patients
Comparison of the CSF proteome of HAD with non-demented HIV/AIDS patients shows altered levels of proteins related to cell signaling and the complement pathway related to inflammation in HAD patients 2, 22, 23, 37. For example, Toro-Nieves et al. (37) hypothesize that neurovirulent HIV-1 variants affect the mononuclear phagocytes proteome by inducing a signature of neurotoxic proteins and thus affect cognitive function. To test this hypothesis, they used HIV-1 separated from normal cognition (NC) and CI, and the laboratory adapted SF162 (a spinal fluid R5 isolate from a patient with HIV-1-associated dementia) to infect MDMs. As a result, 6 unique proteins in NC, 7 in SF162, and 20 in CI were identified. Three proteins were common to SF162 and CI strains. The MDM proteins linked to infection with CI strains were related to apoptosis, chemotaxis, inflammation and redox metabolism.
HAD was found to be involved in oxidative stress
Proteomic approaches have highlighted the involvement of oxidative-stress pathways in HIV-induced neurological injury. Proteins targeted by oxidative modification have been detected in neural cells exposed to HIV proteins. Proteomic analysis of HIV-infected microglia has shown altered levels of redox enzymes (14). Altered antioxidant activity in addition to altered vitamin-D-metabolism-related enzymes have been identified by proteomic analysis of CSF from HAD and non-demented HIV/AIDS patients 22, 23.
HIV altered brain microenvironment
Similar to other neuroinflammatory conditions, proteomic analysis of CSF from HIV-infected patients with CI has shown dysregulation of protease inhibitors (i.e., clusterin and cystatin C), enzymes involved in metabolism and also proteins involved in blood–brain-barrier function 23, 38. HIV-1-infected MDMs affect the human brain microvascular endothelial cell (HBMEC) proteome (38). These MDMs induced the up-regulation of over 200 HBMEC proteins, including metabolic, voltage-gated ion channels, heat shock, transport, cytoskeletal, regulatory, and calcium-binding proteins. HIV-1-infected MDMs affect the HBMEC proteome and, in this way, affect blood-brain-barrier dysfunction and the development of HIV-1 CNS disease (38).
Proteomics was used to discover how the communication of astrocytes with macrophages and microglia can influence disease (14). Using vesicular stomatitis virus pseudotyped HIV-infected murine microglia, Wang et al. (14) found 68 differentially expressed proteins involved in cell structure, regulation, etc., and demonstrated that astrocytes and microglial interaction probably accelerated cell death and increased the development of HAD through these proteins. At the same time, they found that infected astrocytes showed modest changes in protein elements as compared to uninfected cells through co-culture systems of HIV-infected mouse astrocytes and microglia (15). Similarly, another proteomic study (39) of isolated nerve endings from 19 human brain specimens showed that the concentrations of 31 candidate protein spots were potentially abnormal in HIV-infected decedents with HIV encephalitis and/or increased expression of immunoproteasome (IPS) subunits. Synapsin 1b and stathmin were inversely related to brain HIV-1 load; 14-3-3ζ and 14-4-4ε proteins were higher in subjects with HIV-1 loads. Perturbed synaptosome proteins were linked with IPS subunit composition, and 14-3-3ζ was histologically colocalized with IPS subunits in stained neocortical neurons.
Protecting mechanism of HIV infection
Mechanism of HIV resistance in sex workers
In HIV-resistant sex workers who are highly exposed to HIV infection yet remain uninfected, the identification of natural factors involved in protection against HIV-1 in the genital mucosa has caused great interest in the development of mucosal HIV-1 microbicides. The genital proteome of mucosal secretions from HIV-resistant women was examined by Iqbal et al. (40). Through SELDI-MS analysis of the mucosa from 315 HIV-resistant, HIV-uninfected and HIV-infected commercial sex workers, elevated elafin/trappin-2 in the female genital tract was found to be associated with protection against HIV acquisition. Another study (9) using quantitative proteomics technique of 2D-DIGE combined with MS showed that over 15 proteins were differentially expressed between HIV-1-resistant women and control groups, including the overexpressed serpin B family, and also cystatin A, a known anti-HIV-1 factor.
Mechanism of placenta protecting the fetus
Mononuclear phagocytes (MP; monocytes, tissue macrophages and dendritic cells) are reservoirs, vehicles of dissemination, and targets for persistent HIV infection. However, not all MP population equally supports viral growth. Such differential replication is typified by the greater ability of placental acrophages (PM), as compared to blood borne MDM, to restrict viral replication (41). Luciano-Montalvo et al. (41) used a proteomics approach consisting of SELDI-TOF, tandem mass spectrometry and Western blots to identify differences between the uninfected and HIV-infected PM and MDM protein profiles linked to viral growth. The results demonstrate that the low molecular weight placental macrophage cytosolic proteins are differentially expressed in HIV-infected PM and MDM and identify a potential role for cystatin B in HIV replication. This work also serves to elucidate a mechanism by which the placenta protects the fetus from HIV transmission.
Mechanism of immune system responding to pathogens associated with substance abuse
Substance abuse has become a global health concern. Understanding how substance abuse modulates the immune system and how the immune system responds to pathogens associated with substance abuse, such as hepatitis C virus (HCV) and HIV-1, can be assessed by an integrated approach combining proteomic analyses and quantification of gene expression 42, 43. When monocyte-derived mature dendritic cells (DC) were treated with cocaine or methamphetamine, the protein expression of DC was significantly changed, including several functional classes of proteins such as those that modulate apoptosis, protein folding, protein kinase activity and metabolism as well as proteins that function as intracellular signal transduction molecules (42). The proteome of peripheral blood mononuclear cells isolated from HIV-1-positive donors that occurred after treatment with cocaine or methamphetamine also showed that both drugs differentially regulated the expression of several functional classes of proteins in monocytes and T cells (43).
Future Prospects
In the host proteome research reviewed herein, descriptive studies have pointed to biomarker discovery, infection mechanism, protecting mechanism of HIV infection, and immune system responding to pathogens associated with substance abuse. Although many progresses have been made in HIV/AIDS research through genomics, the advent of proteomics has been greatly broadening our view and accelerating our way in HIV/AIDS research fields. By jointly using genomics, proteomics and bioinformatics, there is a great potential to make considerable contribution to biomarker identification and to revolutionize both the development of new therapies and drug development process. However, the power of applying proteomics in understanding HIV/AIDS would be enhanced in the follows: (1) Human tissues available from autopsies chiefly reflect molecular changes related to the late stages of disease – a drawback to most descriptive studies on human tissues. More cells or animal models to imitate the HIV infection process are needed. So far, most researches use non-human primate animals 5, 6, 44 due to HIV infection characters. However, the primate animals are very expensive and difficult to obtain, therefore more animals that are easy to obtain and cheap to feed are needed. Luckily, mouse 45, 46 or rat 47, 48 models with trans-HIV genes have been developed and might be used to HIV infection research. It will be better to use these models for HIV–host interaction research and drug development. (2) Another issue facing descriptive analyses is the lack of “spatial” resolution. In whole-tissue extractions, the opportunity to examine an important level of biocomplexity (i.e., cell-specific expression of biomolecules) is lost. Therefore it is very important to develop more proteomic technologies for cell-specific proteomic studies. At present, different kinds of cells can be well separated through Flow Cytometer 49, 50. It will bring great progress to “spatial” resolution in proteomics if the cells separated by Flow Cytometer can be used in proteome study. Furthermore, 2D or 3D cell grow systems have been developed to study cell–cell interaction (51), and have great potential in proteomic research. In whole-cell extraction, the proteins with low abundance might be lost due to the overlap of high abundant proteins. In order to solve this question, subcellular proteomic technology, immuno-purification, fractionation and different protein separation technologies have been developed (52). (3) The dynamical protein changes were not considered in most of researches. Modeling the dynamical behavior of the networks using data derived from integrated analyses, coupled with descriptive studies with a temporal resolution, will be the best strategy to understand, predict and modify the disease course for HIV infection. To solve dynamical protein changes, many researchers have focused on multiple reaction monitoring (MRM) (53), which can simultaneously quantify nearly 500 ion-pairs with 50 copies/cell in several minutes. (4) The reports about protein post-translational modification (PTM) such as phospholation and glycosylation in HIV/AIDS were very limited. It is very inadequate for PTM studies since many functions of proteins are carried through PTM. So far only one glycoproteomic study reports HIV to uncover host proteins involved in virus (54). (5) Further research for discovering protein functions is very limited. Most of the studies only reported the differently expressed proteins. No data about the relationship between the different proteins and virus. (6) The application of proteomics in HIV/AIDS is very limited and neglected. During the past several years, proteomics has developed many new technologies such as iTRAQ/ICAT-LC-MS 55, 56, MRM (53), and Protein Chip or array technology (57). These new technologies have been widely used in cancer research 55, 57. Furthermore, genomics, proteomics and bioinformatics have been jointly used to deeply discover drug targets, biomarkers 58, 59, or evaluate vaccine and immune response 60, 61; however, so far only few studies were reported in HIV/AIDS (62).
Summarily, proteomics is a very useful tool for HIV/AIDS research, but needs to be improved in several aspects such as spatial, dynamic, low abundant protein information.
Acknowledgements
This work was supported by grants from Shanghai Natural Science Foundation (09ZR1426300) and Research Foundation for Young Scholars of Shanghai Medical College, Fudan University (2008).
Contributor Information
Lijun Zhang, Email: zhanglijun1221@163.com.
Honghao Zhou, Email: hhzhou@public.cs.hn.cn.
References
- 1.List E.O. The use of proteomics to study infectious diseases. Infect. Disord. Drug Targets. 2008;8:31–45. doi: 10.2174/187152608784139640. [DOI] [PubMed] [Google Scholar]
- 2.Noorbakhsh F. Deciphering complex mechanisms in neurodegenerative diseases: the advent of systems biology. Trends Neurosci. 2009;32:88–100. doi: 10.1016/j.tins.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Wiederin J. Biomarkers of HIV-1 associated dementia: proteomic investigation of sera. Proteome Sci. 2009;7:8. doi: 10.1186/1477-5956-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim S.S. Different isoforms of apolipoprotein AI present heterologous post-translational expression in HIV infected patients. J. Proteome Res. 2007;6:180–184. doi: 10.1021/pr060323f. [DOI] [PubMed] [Google Scholar]
- 5.Pendyala G. Cerebrospinal fluid proteomics reveals potential pathogenic changes in the brains of SIV-infected monkeys. J. Proteome Res. 2009;8:2253–2260. doi: 10.1021/pr800854t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonneh-Barkay D. YKL-40, a marker of simian immunodeficiency virus encephalitis, modulates the biological activity of basic fibroblast growth factor. Am. J. Pathol. 2008;173:130–143. doi: 10.2353/ajpath.2008.080045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ringrose J.H. Proteomic studies reveal coordinated changes in T-cell expression patterns upon infection with human immunodeficiency virus type 1. J. Virol. 2008;82:4320–4330. doi: 10.1128/JVI.01819-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Velazquez I. Antioxidant enzyme dysfunction in monocytes and CSF of Hispanic women with HIV-associated cognitive impairment. J. Neuroimmunol. 2009;206:106–111. doi: 10.1016/j.jneuroim.2008.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burgener A. Identification of differentially expressed proteins in the cervical mucosa of HIV-1-resistant sex workers. J. Proteome Res. 2008;7:4446–4454. doi: 10.1021/pr800406r. [DOI] [PubMed] [Google Scholar]
- 10.Jain M.R. Quantitative proteomic analysis of formalin fixed paraffin embedded oral HPV lesions from HIV patients. Open Proteomics J. 2008;1:40–45. doi: 10.2174/1875039700801010040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia K. Characterization of the placental macrophage secretome: implications for antiviral activity. Placenta. 2009;30:149–155. doi: 10.1016/j.placenta.2008.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasheed S. HIV replication enhances production of free fatty acids, low density lipoproteins and many key proteins involved in lipid metabolism: a proteomics study. PLoS One. 2008;3:e3003. doi: 10.1371/journal.pone.0003003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan E.Y. Dynamic host energetics and cytoskeletal proteomes in human immunodeficiency virus type 1-infected human primary CD4 cells: analysis by multiplexed label-free mass spectrometry. J. Virol. 2009;83:9283–9295. doi: 10.1128/JVI.00814-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T. Proteomic modeling for HIV-1 infected microglia-astrocyte crosstalk. PLoS One. 2008;3:e2507. doi: 10.1371/journal.pone.0002507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang T. HIV-1-infected astrocytes and the microglial proteome. J. Neuroimmune Pharmacol. 2008;3:173–186. doi: 10.1007/s11481-008-9110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasheed S. Proteomic characterization of HIV-modulated membrane receptors, kinases and signaling proteins involved in novel angiogenic pathways. J. Transl. Med. 2009;7:75. doi: 10.1186/1479-5876-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kadiu I. HIV-1 transforms the monocyte plasma membrane proteome. Cell Immunol. 2009;258:44–58. doi: 10.1016/j.cellimm.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kadiu I. Cytoskeletal protein transformation in HIV-1-infected macrophage giant cells. J. Immunol. 2007;178:6404–6415. doi: 10.4049/jimmunol.178.10.6404. [DOI] [PubMed] [Google Scholar]
- 19.Simpson R.J. Proteomic profiling of exosomes: current perspectives. Proteomics. 2008;8:4083–4099. doi: 10.1002/pmic.200800109. [DOI] [PubMed] [Google Scholar]
- 20.Peraire J. HIV-1-infected long-term non-progressors have milder mitochondrial impairment and lower mitochondrially-driven apoptosis in peripheral blood mononuclear cells than typical progressors. Curr. HIV Res. 2007;5:467–473. doi: 10.2174/157016207781662452. [DOI] [PubMed] [Google Scholar]
- 21.Ances B.M., Ellis R.J. Dementia and neurocognitive disorders due to HIV-1 infection. Semin. Neurol. 2007;27:86–92. doi: 10.1055/s-2006-956759. [DOI] [PubMed] [Google Scholar]
- 22.Laspiur J.P. CSF proteomic fingerprints for HIV-associated cognitive impairment. J. Neuroimmunol. 2007;192:157–170. doi: 10.1016/j.jneuroim.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rozek W. Cerebrospinal fluid proteomic profiling of HIV-1-infected patients with cognitive impairment. J. Proteome Res. 2007;6:4189–4199. doi: 10.1021/pr070220c. [DOI] [PubMed] [Google Scholar]
- 24.Soler-Garcia A.A. Iron-related proteins: candidate urine biomarkers in childhood HIV-associated renal diseases. Clin. J. Am. Soc. Nephrol. 2009;4:763–771. doi: 10.2215/CJN.0200608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rawson P.M. Cross-presentation of caspase-cleaved apoptotic self antigens in HIV infection. Nat. Med. 2007;13:1431–1439. doi: 10.1038/nm1679. [DOI] [PubMed] [Google Scholar]
- 26.Pathak S. HIV induces both a down-regulation of IRAK-4 that impairs TLR signalling and an up-regulation of the antibiotic peptide dermcidin in monocytic cells. Scand. J. Immunol. 2009;70:264–276. doi: 10.1111/j.1365-3083.2009.02299.x. [DOI] [PubMed] [Google Scholar]
- 27.Brass A.L. Identification of host proteins required for HIV infection through a functional genomic screen. Science. 2008;319:921–926. doi: 10.1126/science.1152725. [DOI] [PubMed] [Google Scholar]
- 28.Dyer M.D. The landscape of human proteins interacting with viruses and other pathogens. PLoS Pathog. 2008;4:e32. doi: 10.1371/journal.ppat.0040032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Douglas J.L. Vpu directs the degradation of the human immunodeficiency virus restriction factor BST-2/Tetherin via a {beta}TrCP-dependent mechanism. J. Virol. 2009;83:7931–7947. doi: 10.1128/JVI.00242-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee M.J., Park J.H. Pathway analysis in HEK 293T cells overexpressing HIV-1 tat and nucleocapsid. J. Microbiol. Biotechnol. 2009;19:1103–1108. doi: 10.4014/jmb.0903.3005. [DOI] [PubMed] [Google Scholar]
- 31.Gautier V.W. In vitro nuclear interactome of the HIV-1 Tat protein. Retrovirology. 2009;6:47. doi: 10.1186/1742-4690-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He F. Endogenous HIV-1 Vpr-mediated apoptosis and proteome alteration of human T-cell leukemia virus-1 transformed C8166 cells. Apoptosis. 2009;14:1212–1226. doi: 10.1007/s10495-009-0380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Srivastava S. Lentiviral Vpx accessory factor targets VprBP/DCAF1 substrate adaptor for cullin 4 E3 ubiquitin ligase to enable macrophage infection. PLoS Pathog. 2008;4:e1000059. doi: 10.1371/journal.ppat.1000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzalez-Scarano F., Martin-Garcia J. The neuropathogenesis of AIDS. Nat. Rev. Immunol. 2005;5:69–81. doi: 10.1038/nri1527. [DOI] [PubMed] [Google Scholar]
- 35.Power C. Retroviral diseases of the nervous system: pathogenic host response or viral gene-mediated neurovirulence? Trends Neurosci. 2001;24:162–169. doi: 10.1016/s0166-2236(00)01737-9. [DOI] [PubMed] [Google Scholar]
- 36.Kaul M., Lipton S.A. Mechanisms of neuronal injury and death in HIV-1 associated dementia. Curr. HIV Res. 2006;4:307–318. doi: 10.2174/157016206777709384. [DOI] [PubMed] [Google Scholar]
- 37.Toro-Nieves D.M. Proteomic analyses of monocyte-derived macrophages infected with human immunodeficiency virus type 1 primary isolates from Hispanic women with and without cognitive impairment. J. Neurovirol. 2009;15:36–50. doi: 10.1080/13550280802385505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ricardo-Dukelow M. HIV-1 infected monocyte-derived macrophages affect the human brain microvascular endothelial cell proteome: new insights into blood-brain barrier dysfunction for HIV-1-associated dementia. J. Neuroimmunol. 2007;185:37–46. doi: 10.1016/j.jneuroim.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gelman B.B., Nguyen T.P. Synaptic proteins linked to HIV-1 Infection and immunoproteasome Induction: proteomic analysis of human synaptosomes. J. Neuroimmune Pharmacol. 2010;5:92–102. doi: 10.1007/s11481-009-9168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Iqbal S.M. Elevated elafin/trappin-2 in the female genital tract is associated with protection against HIV acquisition. AIDS. 2009;23:1669–1677. doi: 10.1097/QAD.0b013e32832ea643. [DOI] [PubMed] [Google Scholar]
- 41.Luciano-Montalvo C. Proteomic analyses associate cystatin B with restricted HIV-1 replication in placental macrophages. Placenta. 2008;29:1016–1023. doi: 10.1016/j.placenta.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reynolds J.L. Proteomic analyses of the effects of drugs of abuse on monocyte-derived mature dendritic cells. Immunol. Invest. 2009;38:526–550. doi: 10.1080/08820130902874110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reynolds J.L. Modulation of the proteome of peripheral blood mononuclear cells from HIV-1-infected patients by drugs of abuse. J. Clin. Immunol. 2009;29:646–656. doi: 10.1007/s10875-009-9309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haase A.T. Targeting early infection to prevent HIV-1 mucosal transmission. Nature. 2010;464:217–223. doi: 10.1038/nature08757. [DOI] [PubMed] [Google Scholar]
- 45.Grandy S.A. Reduction of ventricular sodium current in a mouse model of HIV. J. Cardiovasc. Electrophysiol. 2010 doi: 10.1111/j.1540-8167.2009.01713.x. In press. [DOI] [PubMed] [Google Scholar]
- 46.Denton P.W. Systemic administration of antiretrovirals prior to exposure prevents rectal and intravenous HIV-1 transmission in humanized BLT mice. PLoS One. 2010;5:e8829. doi: 10.1371/journal.pone.0008829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hag A.M. Regional gene expression of LOX-1, VCAM-1, and ICAM-1 in aorta of HIV-1 transgenic rats. PLoS One. 2009;4:e8170. doi: 10.1371/journal.pone.0008170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peng J. The HIV-1 transgenic rat as a model for HIV-1 infected individuals on HAART. J. Neuroimmunol. 2010;218:94–101. doi: 10.1016/j.jneuroim.2009.09.014. [DOI] [PubMed] [Google Scholar]
- 49.Collins C.E. A rapid and reliable method of counting neurons and other cells in brain tissue: a comparison of flow cytometry and manual counting methods. Front. Neuroanat. 2010;4:5. doi: 10.3389/neuro.05.005.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ibrahim S.F., van de Engh G. Flow cytometry and cell sorting. Adv. Biochem. Eng. Biotechnol. 2007;106:19–39. doi: 10.1007/10_2007_073. [DOI] [PubMed] [Google Scholar]
- 51.Kunz F. A novel modular device for 3-D bone cell culture and non-destructive cell analysis. Acta Biomater. 2010 doi: 10.1016/j.actbio.2010.03.015. In press. [DOI] [PubMed] [Google Scholar]
- 52.Helbig A.O. Exploring the membrane proteome—challenges and analytical strategies. J. Proteomics. 2010;73:868–878. doi: 10.1016/j.jprot.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 53.Picotti P. Full dynamic range proteome analysis of S. cerevisiae by targeted proteomics. Cell. 2009;138:795–806. doi: 10.1016/j.cell.2009.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Graham D.R. Two-dimensional gel-based approaches for the assessment of N-Linked and O-GlcNAc glycosylation in human and simian immunodeficiency viruses. Proteomics. 2008;8:4919–4930. doi: 10.1002/pmic.200800608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Latterich M. Proteomics: new technologies and clinical applications. Eur. J. Cancer. 2008;44:2737–2741. doi: 10.1016/j.ejca.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 56.Zamo A., Cecconi D. Proteomic analysis of lymphoid and haematopoietic neoplasms: there’s more than biomarker discovery. J. Proteomics. 2010;73:508–520. doi: 10.1016/j.jprot.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 57.Sun S. Oncoproteomics of hepatocellular carcinoma: from cancer markers’ discovery to functional pathways. Liver Int. 2007;27:1021–1038. doi: 10.1111/j.1478-3231.2007.01533.x. [DOI] [PubMed] [Google Scholar]
- 58.Psyrri A. Strategies to promote translational research within the European Organisation for Research and Treatment of Cancer (EORTC) Head and Neck Cancer Group: a report from the Translational Research Subcommittee. Ann. Oncol. 2010 doi: 10.1093/annonc/mdq060. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cho W.C. Proteomics technologies and challenges. Genomics Proteomics Bioinformatics. 2007;5:77–85. doi: 10.1016/S1672-0229(07)60018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thomas C., Moridani M. Interindividual variations in the efficacy and toxicity of vaccines. Toxicology. 2009 doi: 10.1016/j.tox.2009.10.008. In press. [DOI] [PubMed] [Google Scholar]
- 61.Regnstrom K.J. Pharmacogenomics in the preclinical development of vaccines: evaluation of efficacy and systemic toxicity in the mouse using array technology. Methods Mol. Biol. 2008;448:447–467. doi: 10.1007/978-1-59745-205-2_16. [DOI] [PubMed] [Google Scholar]
- 62.Lucchese A. Sequence uniqueness as a molecular signature of HIV-1-derived B-cell epitopes. Int. J. Immunopathol. Pharmacol. 2009;22:639–646. doi: 10.1177/039463200902200309. [DOI] [PubMed] [Google Scholar]