Refer to the page 658-664
Heart failure (HF) is a complex clinical syndrome affecting more than 23 million people world-wide.1) The incidence of HF is associated with age, and it has remained stable in the past several decades. With the aging of society, the prevalence of HF is expected to rise, and indeed, in 1994 the prevalence of HF was 90 per 1000 beneficiaries and increased to 121 per 1000 beneficiaries in 2003 in the USA.2) There are more than 5.1 million HF patients in the USA and 875000 new patients are diagnosed with HF each year. Despite improved survival in the last 3 decades with introduction of new disease modifying drugs (beta blockers, renin-angiotensin-system inhibitors, mineralocorticoid receptor antagonists, ivabradine and angiotensin-receptor-neprylisin inhibitor), and devices (implantable cardioverter defibrillator, cardiac resynchronizing therapy, left ventricular assisting devices) HF is still associated with high mortality and morbidity, and enormous socio-economic burden. Knowing the exact prevalence of HF is important for developing healthcare policy for its management.
Until now, the prevalence of HF in Korea was unknown. In this edition of the Journal, Lim and colleagues reported the nationwide prevalence of HF in Korea for the first time, using data from the 2002-2013 National Sample Cohort based on the National Health Information Database.3) They reported that HF prevalence was 0.75% in 2002 and 1.53% in 2012. Interestingly, the projected HF prevalence is expected to be 1.89% and 3.35% in 2020 and 2040, respectively. By 2040, more than 1.7 million Koreans are expected to have HF.
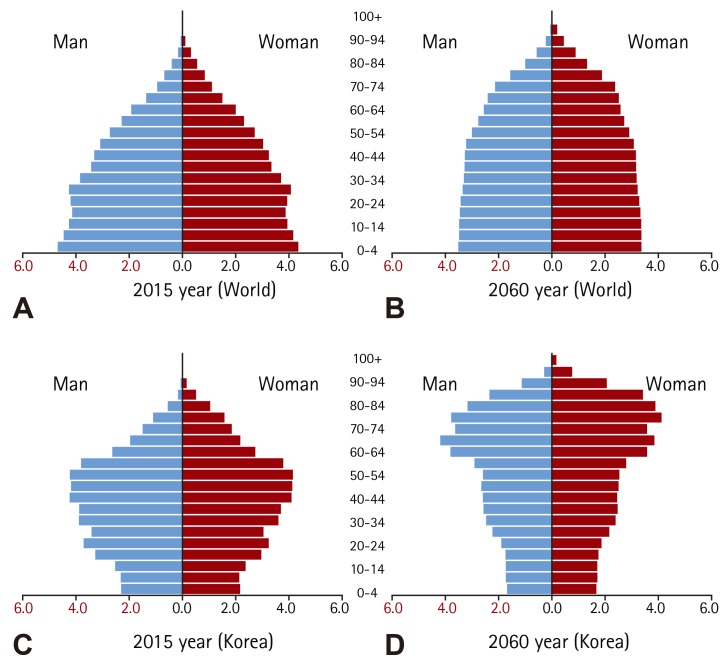
Korea is the most-rapidly aging society among the Organization for Economic Cooperation and Development countries; consequently, the prevalence of HF is expected to rise due to the change in population structure (Fig. 1). In addition, the westernization of lifestyle and an increasing prevalence of ischemic heart disease also contribute to the rise in HF prevalence. This is not a unique phenomenon confined to Korea, but an epidemic observed in other Asian countries and the world.
Fig. 1. Population structure in 2015 and the expected population structure in 2060 Korea. Population structure of the world in 2015 (A), and expected structure in 2060 (B), Population structure of Korea in 2015 (C), and expected population structure in 2060 (D). "Population status and prospect of Korea and World" Report by National Statistical Office of Korea July 2015.
It is challenging to obtain an accurate estimate of the prevalence of a disease by using a sample cohort, because the representativeness of the sample is not always accurate. Lim and colleagues used a 'one-million National Sample Cohort' based on the National Health Information Database. The National Sample Cohort was generated using a systematic sampling method, and included the most representative 2% of the whole population. The representativeness of this sample had been validated with the prevalence of hypertension, diabetes mellitus, and others. In our opinion, the National Sample Cohort enables the most accurate estimate of the nationwide prevalence of HF, which is the main strength of this study. In contrast, the estimation of HF prevalence based on data derived from a hospital, or a community may have limited value.4),5) It is noteworthy that the extrapolation of disease prevalence in the current population to another future population requires the assumption of a stable incidence of the disease over time. Whether this assumption remains true in HF is unknown.
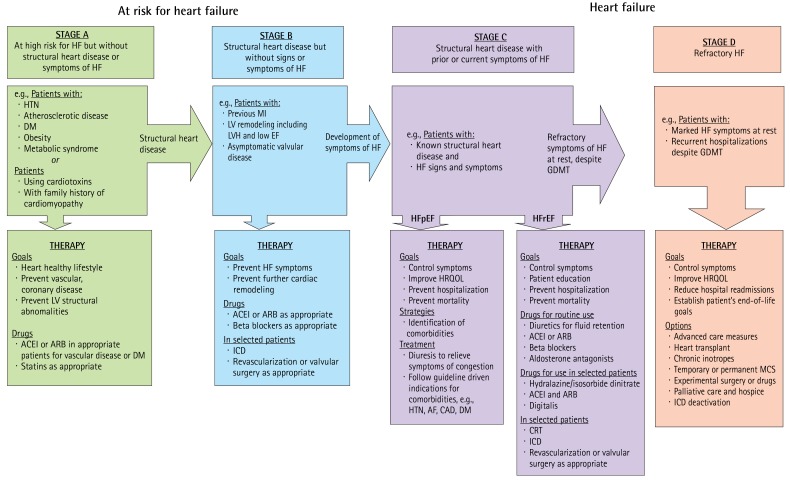
Currently the ACCF/AHA categorizes HF in 4 stages, i.e. stage A, B, C, and D (Fig. 2). This staging system recognizes the following: (i) both risk factors and structural cardiac abnormalities are considerably associated with HF: (ii) the stages are progressive and inviolate, i.e. once a patient moves to a higher stage of HF, regression to an earlier stage is not observed; and (iii) early and adequate therapeutic interventions are needed to stop the progression of HF stages, i.e. modifying risk factors (stage A), treating structural heart disease (stage B), and reducing morbidity and mortality (stages C and D).6)
Fig. 2. 2013 ACCF/AHA Guideline for the management of heart failure. HF: heart failure, ACEI: angiotensin-converting enzyme inhibitor, AF: atrial fibrillation, ARB: angiotensin-receptor blocker, CAD: coronary artery disease, CRT: cardiac resynchronization therapy, DM: diabetes mellitus, EF: ejection fraction, GDMT: guideline-directed medical therapy, HF: heart failure, HFpEF: heart failure with preserved ejection fraction, HFrEF: heart failure with reduced ejection fraction, HRQOL: health-related quality of life, HTN: hypertension, ICD: implantable cardioverter-defibrillator, LV: left ventricular, LVH: left ventricular hypertrophy, MCS: mechanical circulatory support, MI: myocardial infarction.
Stage A is classified as risk factor without objective structural heart disease. Lim and colleagues3) also showed that the prevalence of comorbidities associated with HF was high, such as history of ischemic heart disease, hypertension, and diabetes mellitus. Hypertension is the most important modifiable risk factor for HF with the highest prevalence, and requires strict control to prevent future HF and to stop the HF epidemic. The prevalence of ischemic heart disease and diabetes mellitus is also expected to increase among HF patients due to the accelerated adoption of Western lifestyles and sufficient treatment leading to improved survival.
High morbidity and mortality of HF is associated with enormous healthcare cost. More than 1 million people are hospitalized for heart failure, and the one-year readmission rate is greater than 25% in the USA. Consequently, total medical costs for HF in the USA are expected to increase from $20.9 billion in 2012 to $53.1 billion in 2030. Similar trends or even greater increases are expected in Korea, when considering the rapidly aging population structure in Korea.
Aging of the Korean population is inevitable. Only early intervention stopping the progression of HF stages is the key to preventing the HF epidemic.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Writing Group Members. Mozaffarian D, Benjamin EJ, et al. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 2.Curtis LH, Whellan DJ, Hammill BG, et al. Incidence and prevalence of heart failure in elderly persons, 1994-2003. Arch Intern Med. 2008;168:418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 3.Lee JH, Lim NK, Cho MC, Park HY. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016;46:658–664. doi: 10.4070/kcj.2016.46.5.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Larson MG, Leip EP, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 5.Okura Y, Ramadan MM, Ohno Y, et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008;72:489–491. doi: 10.1253/circj.72.489. [DOI] [PubMed] [Google Scholar]
- 6.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]