Abstract
Background and Objectives
Radiofrequency catheter ablation (RFCA) exposes patients to fixed angle radiation for extended periods of time. We investigated the incidence and characteristics of radiation-induced dermatitis (RID) associated with RFCA.
Subjects and Methods
We screened 1347 consecutive patients from 2000 to 2011 who underwent RFCA for any indication and reviewed patients with dermatologic issues at the 1-month follow-up. Skin lesions were classified into three groups: most likely RID, probable RID, and possible RID.
Results
Of the 1347 enrolled patients, 12 (0.89%) experienced dermatologic issues within 1 month after RFCA, including six patients (0.45%) clinically classified as 'most likely RID' and four patients (0.30%) with 'probable RID'. Ten patients, including most likely RID or probable RID patients, developed skin lesions on the right back and upper arm. Skin lesions did not improve without meticulous treatment, and three cases required surgical intervention. We compared the RID group to the remaining 1335 patients (normal group). The mean body mass indices (BMIs) of the RID and normal groups were 29.3 and 23.9 kg/m2, respectively (p<0.001). Radiation exposure times were longer in the RID group (180±31.0 vs. 47±49.9 minutes, p<0.001). We further analyzed 44 patients (6 RID cases and 38 normal patients) that had BMIs >26 kg/m2 and exposure times >115 minutes based on receiver operator characteristic curve analyses. Among the 35 patients without RID, 29 patients (82.9%) did not use biplane fluoroscopy.
Conclusions
Patients with high BMIs have a higher risk of developing severe RID with increasing fluoroscopy times using biplane fluoroscopy.
Keywords: Catheter ablation, Fluoroscopy, Radiation, Dermatitis, Body mass index
Introduction
Interventional cardiovascular procedures result in considerable radiation doses to patients due to prolonged fluoroscopy exposure times.1) However, it is believed that the radiological risk to patients is lower than that of radiofrequency catheter ablation (RFCA) for the treatment of arrhythmias. The RFCA procedure frequently requires more radiation exposure to patients than other interventional procedures in the cardiology field.2)
One of the severe but easily overlooked acute complications of radiation exposure is radiation-induced dermatitis (RID). Early skin changes in RID include erythema, blister formation, epidermal desquamation, and acute ulceration. Late or chronic skin changes consist of hypo- or hyperpigmentation, telangiectasia, cutaneous induration, recurrent erosions, severe ulceration, and scarring.3) These skin changes can resemble many other dermatologic conditions, which can delay the definitive diagnosis of RID.4) Furthermore, as skin lesions can develop over a period of days to weeks,5),6),7),8) the diagnosis may be missed without the clinician's awareness.
Because RFCA is usually performed with fixed angle radiation over a period of hours, RID can occur on predictable skin areas. However, the degree of radiation exposure in fluoroscopy patients during RFCA depends on the fluoroscopy machine and whether it is single plane or biplane. It is also influenced by patient age, sex, as well as individual patient susceptibilities. Furthermore, because RID is rare, its incidence, clinical, and pathologic features are not known well. Few reports have measured the radiation exposure to patients during RFCA (Table 1).5),6),7),8),9),10),11) In the present study, we analyzed RID incidence and characteristics for patients who underwent RFCA.
Table 1. Previous fluoroscopy studies of RFCA-induced radiation dermatitis.
| Authors | Journal | Year | No | Age | Sex | BMI | Onset after exposure (weeks) | Location | Diagnosis | Procedure duration (minutes) | Fluoroscopy time (minutes) | Estimate absorbed radiation dose (Gy) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shope14) | RadioGraphics | 1996 | 3 | - | F | - | - | - | - | - | - | - |
| 25 | F | 12 | - | - | 325 | - | - | |||||
| 34 | F | - | 20 | - | - | 190 | - | - | ||||
| Rosenthal et al.11) | Pacing Clin Electrophysiol | 1997 | 1 | F | - | 12 | AVNRT | 65 | - | 15–20 | ||
| Nahass10 | J Am Acad Dermatol | 1997 | 2 | - | - | - | Several ~ 12 | Left upper back | SVTSVT | 190 | - | - |
| - | 190 | |||||||||||
| Vano et al.8) | Br J Radiol | 1998 | 1 | 12 17 7 50 |
F F F M |
- - - - |
12 4 16 4 |
Right arm Right axilla Right arm Right side |
AP (left posterior) AP (posterior) ATAP (postero septal) |
- 300 240 240 |
- - - 90–120 |
- - - - |
| Glazier and Dixon9) | Q J Med | 2012 | 1 | 45 | F | 42 | 7 wks | Right posterolateral chest wall | 720 | >90 | 12.7 |
RFCA: adiofrequency catheter ablation, No: number of patents, BMI: body mass index, AVNRT: atrioventricular nodal reentrant tachycardia, SVT: supraventricular tachycardia, AP: accessory pathway, AT: atrial tachycardia
Subjects and Methods
Study population
A total of 1347 consecutive patients who underwent RFCA procedures between 2000 to 2011 for any indication and were evaluated for dermatologic complications following RFCA were screened. Each of the 1347 patients routinely visited the arrhythmia clinic 1 month after RFCA and reported complications to the physicians. Patient characteristics and procedural data were analyzed.
RFCA procedure
RFCA procedures were performed at a single center by three independent expert electrophysiologists using the same fluoroscopy machine (Integris BH 5000 Bi-Plane system; Philips Medical Systems, Amsterdam, The Netherlands). The routine baseline settings of the biplane fluoroscopy angle were(right anterior oblique (RAO) of 30 degrees and left anterior oblique (LAO) of 60 degrees. Of the 1347 patients, a total of 894 patients had exact fluoroscopy time data available. The fluoroscopy frame rate setting was routinely set at 15 frames per second.
Radiation-induced dermatitis (RID)
Patients who complained of skin problems at the 1-month follow-up were retrospectively reviewed. An expert dermatologist re-diagnosed skin lesions based on clinical data including medical photos or medical descriptions. Lesions were classified into three groups: (1) most likely RID, (2) probable RID, and (3) possible RID. Patients in the 'most likely' RID or 'probable' RID groups comprised the RID group. Patients without any skin complications comprised the normal group.
Statistical analyses
Unless otherwise specified, all data are expressed as mean values±standard deviation. We used chi (χ2)-square tests to compare characteristics among patients, the Fisher's exact tests for categorical covariates, and the Student's t-tests for continuous covariates. For the risk factor (univariate/multivariate) analysis, we used binary logistic regression analysis. A receiver operator characteristic curve was used to determine the cutoff value of fluoroscopy time and body mass index (BMI) for RID. We selected the appropriate cutoff value which had high values for both sensitivity and specificity, using the Youden's index (sensitivity+specificity 1). Statistical analyses were performed using SPSS version 21 (IBM/SPSS Inc., Chicago, IL, USA). The category free net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were calculated with R v.3.02 (https://www.r-project.org/)) which is available as Free Software under the terms of the Free Software Foundation's GNU General Public License in source code form.
Results
Incidence of radiation-induced dermatitis
Of the 1347 patients who underwent RFCA, 12 patients who complained of skin problems within 1 month (0.89%). Nine patients had sufficient medical photos to review, and seven patients had skin biopsy data. Of these, six patients were classified as 'most likely' having RID, four patients having 'probable' RID, while one patient had possible dermatitis and another had a lesion that could not be re-evaluated due to the lack of sufficient medical data needed for re-diagnosis. Table 2 shows the characteristics of 10 RID patients.
Table 2. Characteristics of 10 patients in the RID group.
| Patient | Age | Sex | Height | Body weight | BMI | Lesion location | Diagnosis | procedure time | Fluoroscopy time (min) | Lesion description | Biopsy result | Surgical treatment | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Most likely | 1 | 70 | F | 158.3 | 74.9 | 30.0 | Right arm, back | AVRT | 4 h 30 m | 180 | 3 cm-sized ulcerative lesion | 1) Mixed inflammatory cell infiltration in dermis, 2) hyperkeratosis and parakeratosis, 3) pustules in keratin layer, and 4) dense fibrosis in dermis and subcutaneous tissue | No |
| 2 | 52 | M | 167 | 88 | 31.7 | Right arm, back | AFL | 3 h 30 m | 116 | Bullae formation | Spongiotic dermatitis with 1) crust formation and 2) thick collagen laydown in dermis | Yes | |
| 3 | 30 | M | 170 | 78 | 26.9 | Right arm | AVRT | 3 h 55 m | Palm sized ulceration with oozing, dark colored patch, and erythematous patch | 1) Increased basal pigmentation, 2) some melanophages in upper dermis, and 3) increased dermal collagen | No | ||
| 4 | 41 | M | 185 | 92 | 26.9 | Right arm, back | AFL | 3 h 35 m | 138 | Red erythematous lesion (7.5 cm ´ 5 cm) | Dermal fibrosis with 1) ulceration and 2) focal dystrophic calcificatio | Yes | |
| 5 | 49 | M | 178.6 | 82.8 | 26.0 | Right arm, back | AFL | 6 h 15 m | 204 | Whitish patch | - | No | |
| 6 | 24 | M | 173.8 | 96.4 | 31.9 | Right arm, back | AVRT | 7 h 25 m | 182.8 | Erythema and follicular eruption with scales | - | No | |
| Probable | 7 | 47 | F | 151 | 69 | 30.2 | Right arm, back | AVRT | 4 h 20 m | Hyper-pigmented, well-demarcated patch with bullae lesion | Ulceration and fibrinoid necrosis of the injured tissue | No | |
| 8 | 22 | M | 175 | 93 | 30.2 | Right arm, back | AVRT | 4 h 0 m | Erythematous scaly patch, with crust and pus | - | No | ||
| 9 | 52 | F | 161 | 72 | 27.9 | Right arm, back | AVRT | 4 h 45 m | Ulcerative lesion | Ulcer with 1) markedly increased dermal collagen, 2) chronically active inflammation, and 3) dystrophic calcification | Yes | ||
| 10 | 49 | M | 169.8 | 89.8 | 31.2 | Right arm, back | AFL, PAF | 6 h 15 m | 187 | Deep ulcer | Ulceration and fibrinoid necrosis of the injured tissue | No |
RID: radiation-induced dermatitis, BMI: body mass index, AVRT: atrioventricular reentrant tachycardia; AFL: atrial flutter, PAF: paroxysmal atrial fibrillation
Cases of RID
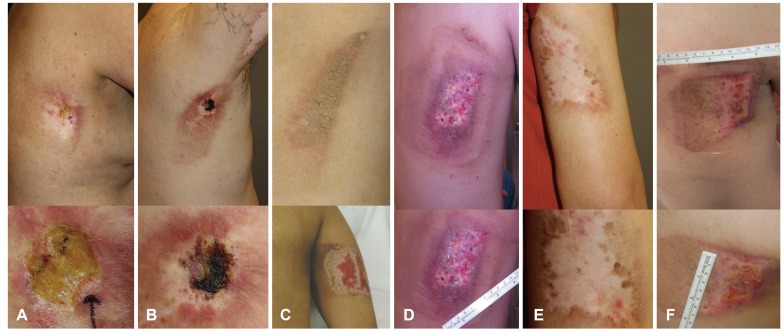
Fig. 1A-F shows medical photos of six patients that most like had RID. Detailed medical data are shown in Table 2 (patients 1-6). Of these patients, two patients required surgical repair for their skin problems. Detailed medical data of patients with probable RID are also listed in Table 2 (patients 7-10). Of these, one patient needed surgical repair for skin problems.
Fig. 1. Radiation induced dermatitis. Medical photos of six patients with dermatitis that is most likely RID. RID: radiation-induced dermatitis.
Characteristics of the RID group
In 10 patients with RID, the skin lesions did not improve without medical or surgical treatment and were vulnerable to minor trauma. Because patients were exposed at a fixed angle, all patients in the RID group had lesions on the back of the right thorax and posteriolateral aspect of the right proximal arm. Seven cases improved with medical treatment alone, but three cases required surgical intervention.
In Table 3, we compare the 10 patients in the RID group with the 1335 normal group patients. The mean body weight and body mass indices (BMIs) of the RID and normal groups were 29.3 and 23.9, respectively (p<0.001). Body surface area (BSA) was also significantly higher in the RID group (p=0.006). Fluoroscopy times were significantly longer in the RID group. Age, sex, or past medical history did not affect the incidence of RID.
Table 3. RID patients vs. non-complicated patients.
| RID group (n=10) | Normal group (n=1335) | p | |
|---|---|---|---|
| Age (years) | 43.7±14.7 | 43.4±16.1 | 0.948 |
| Female | 3 (30%) | 585 (43.8%) | 0.527 |
| Height (cm) | 168.8±10.2 | 164.5±16.2 | 0.220 |
| Body weight (kg) | 83.5±9.7 | 65.7±12.2 | <0.001 |
| BSA* | 1.97±0.2 | 1.73±0.2 | 0.001 |
| BMI (kg/m2) | 29.3±2.2 | 23.9±3.5 | <0.001 |
| Repeated RFCA (>1) | 2 | 78 | 0.115 |
| 1 time | 8 | 1258 | 0.115 |
| 2 times | 0 | 65 | 0.609 |
| 3 times | 0 | 7 | 0.942 |
| 4 times | 2 | 4 | 0.001 |
| 6 times | 0 | 1 | 0.993 |
| Fluoroscopy time (min, n=894) | 180.0±31.0 (n=6) | 46.6±49.9 (n=888) | <0.001 |
| Estimated radiation exposure dose (n=894) | 6.8±7.3 | 25.1±4.6 | <0.001 |
| Hypertension | 2 (20%) | 96 (7.4%, n=1299) | 0.169 |
| Diabetes | 0 (0%) | 51 (3.9%, n=1299) | 0.999 |
| Previous myocardial infarction | 0 (0%) | 10 (0.8%, n=1299) | 0.999 |
| Previous cerebral infarction | 0 (0%) | 25 (1.9%, n=1299) | 0.999 |
| Hypothyroidism | 1 (10%) | 13 (1.0%, n=1299) | 0.102 |
RID: radiation-induced dermatitis, BSA: body surface area, BMI: body mass index, RFCA: radio-frequency catheter ablation. *BSA was calculated using the Mosteller formula : BSA (m2) = SQRT( [Height(cm) × Weight(kg) ]/ 3600)
Risk factors for RID
In univariate analyses, BMI (p<0.001), BSA (p=0.001), fluoroscopy time (p<0.001), and repeated RFCA (p=0.001) were significant risk factors for RID. Age, sex, indication for RFCA, or previous history did not correlate with RID. In multivariate analyses including BMI, BSA, fluoroscopy time, and repeated RFCA, BMI (p=0.016), fluoroscopy time (p=0.001), and repeated RFCA (p=0.006) were significant risk factors for RID. BSA was not correlated with RID (p=0.293). The detailed data is described in Table 4.
Table 4. Univariate and multivariate binary logistic regression analysis for risk factors of RID.
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.00 (0.96–1.04) | 0.951 | ||
| Sex | 1.82 (0.47–7.07) | 0.387 | ||
| BMI | 1.41 (1.21–1.63) | <0.001 | 1.47 (1.07–2.00) | 0.016 |
| BSA | 5.16 (1.88–14.16) | 0.001 | 2.70 (0.42–17.22) | 0.293 |
| Fluoroscopy time | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.01–1.04) | 0.001 |
| Repeated RFCA | 2.72 (1.53–4.86) | 0.001 | 3.41 (1.43–8.11) | 0.006 |
RID: radiation-induced dermatitis, OR: odd ratio, CI: confidence interval, BMI: body mass index, BSA: body surface area, RFCA: radio-frequency catheter ablation
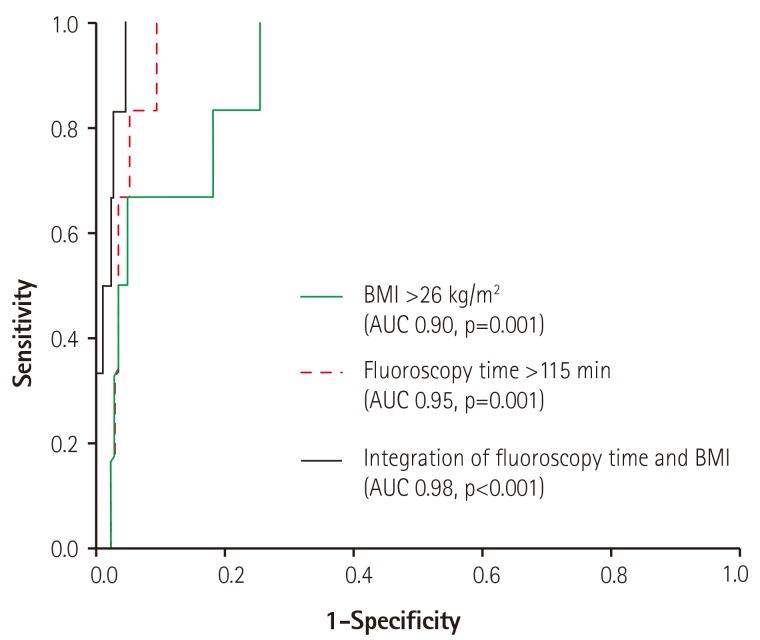
Based on the results of the ROA curve in Fig. 2, the BMI cutoff was 26 kg/m2 (area under curve [AUC] 0.903, p=0.001; sensitivity, 100%; specificity, 74%) and fluoroscopy time cutoff value was 115 min (AUC 0.953, p<0.001; sensitivity, 100%; specificity, 91%). The jointly obtained optimal cutoff values were 156 min and 27 kg/m2. The fluoroscopy time added on BMI did not show an additional prognostic power despite the greatest area under curve 0.980 (p<0.001), as measured by the category free NRI (p=0.39) and IDI (p=0.95).
Fig. 2. ROC curve results for predicting RID. The BMI cutoff was 26 kg/m2 and fluoroscopy time cutoff value was 115 min. ROC: receiver operator characteristic, RID: radiation-induced dermatitis, BMI: body mass index, AUC: area under curve.
Among 894 patients with exact fluoroscopy times, The mean estimated radiation doses of patients with or without RID were 25.1±4.6 vs. 6.8±7.3 Gy, respectively (p<0.001). Assuming that the radiation dose as obtained from the medical records is 0.147-0.375 Gy per minute, exposure time >115 minute can be calculated as total exposure dose of 17–43 Gy.
Subgroup analyses for patients with high BMIs and long fluoroscopy times
Among 894 patients with exact fluoroscopic time information, we further analyzed 41 patients with a BMI >26 kg/m2 and fluoroscopy times >115 minutes. There were 6 RID patients and 35 normal group patients. Of the 35 patients without complications, 29 cases (82.9%) underwent single-plane fluoroscopy because a 3-D mapping system was used. The remaining 6 patients without RID and 6 patients with RID were treated with biplane fluoroscopy.
Discussion
This is the first study with large-scale data to report the RID incidence following RFCA. The findings in this report highlight the importance of minimizing the radiation dose in individual patients to avoid catastrophic dermatologic complications. Physicians should pay special attention to patients with high BMIs (over 26 kg/m2) and when fluoroscopy times are longer than approximately 2 hours.
According to previous studies,12) acute, dose-dependent skin effects of beta-radiation are as follows: erythema from 6 Gy; moist desquamation from 18 Gy, ulceration with slow healing at 24 Gy, and ischemic dermal necrosis from 18 Gy. In daily practice, the thresholds vary by radiation source and each individual, and determining the exact dose given to a patient is not an easy task. Of 894 patients with exact fluoroscopy times, assuming that the radiation dose is 0.147-0.375 Gy per minute, the cutoff exposure time >115 minute from our result can be calculated as the total exposure dose of 17–43 Gy, which correlates with the previous known cutoff value of radiation-induced severe dermatitis.
Patients receiving RFCA are typically exposed to fixed angle radiation for an extended period of time. Although fluoroscopy-induced skin injuries are rare,13) physicians on occasion overlook this preventable but severe skin complication. In the present study, RID ranged in severity from erythema to tissue necrosis requiring skin graft surgery.14) Radiation can penetrate the human body but is rapidly attenuated by the tissues. Therefore, the maximum radiation dose accumulates in the skin at the point of entrance.15) In our patients, the sites of injury were the right arm and back, which is very distinct in RID following fixed angle RFCA. As described, we routinely use fixed angle fluoroscopy with a RAO of 30 degrees and LAO of 60 degrees. The radiation generator with LAO of 60 degrees is usually very close to the right arm of a patient, which is a common site of RID, particularly for patients with a high BMI (Fig. 3A and B). Therefore, we recommend adjusting the radiation projection angle (e.g., adjust LAO angle from 60 degrees to 30 degrees) to prevent RID in patients with high BMIs and long procedure times (Fig. 3C). Fluoroscopy angles generally used during cardiac electrophysiological studies are LAO 60 and RAO 30. Frequent alternative angles that are used are LAO 30 and RAO 30. Our suggestion of LAO 30 is not arbitrary but based on general practice.
Fig. 3. Recommended radiation projection angle to prevent RID. Distance between the radiation generator and a patient with a low BMI (A) or high BMI (B). The recommended projection angle for patients with a high BMI and long procedural times (C). RID: radiation-induced dermatitis, BMI: body mass index, LAO: left anterior oblique, RAO: right anterior oblique.
X-ray penetration through thicker body masses usually requires higher radiation doses. In obese patients with high BMIs, radiation doses can be several times higher compared to patients with lower BMIs. In general, current fluoroscopic equipment automatically adjusts the radiation dose to achieve a certain level of resolution on the image intensifier, and the operator may not be aware of how much radiation the patient is receiving during the procedure. This can result in RID, which is most often reported in obese patients.6),7),16)
In the present study, we found that RID is highly predictable in obese patients with long procedure times. The ROC curve showed that the AUC of both BMI and fluoroscopy time were greater than 0.90. Although integration of these two factors did not improve the predictive power, the AUC of the integration curve was the greatest. The reduced image quality in overweight patients may increase the technical difficulty of the procedure, potentially prolonging procedure times and, thus, requiring greater radiation input. Accordingly, in planning RFCA, operators should take into account the patient's BMI and be prepared to adjust their approach accordingly. Therefore, misdiagnoses and delayed diagnoses of RID could be avoided.
One limitation of this retrospective study is the lack of exact fluoroscopy times and/or radiation doses for 453 patients (33.7%). As there were only 10 RIDs among 1347 patients, weak statistical power is an additional limitation to this study. We cannot determine that the cutoff value presented is an absolute number, as values can be alteredoin future studies. Based on these findings, The authors proposg that with increasing BMI and fluoroscopy time, greater concern should be given to the increased likelihood of ra diation dermatitis.
Conclusion
RID is a critically severe but predictable complication following RFCA. Patients with a high BMI had a higher risk of developing RID with increased exposure times or repeated RFCA using biplane fluoroscopy. Preventive measures, such as adjusting the projection angle, reducing the radiation dose, positioning the radiation generator farther from patients' skin, and careful observation of skin complications during follow-up, should be implemented in these patients.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Weiss EM, Thabit O. Clinical considerations for allied professionals: radiation safety and protection in the electrophysiology lab. Heart Rhythm. 2007;4:1583–1587. doi: 10.1016/j.hrthm.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Heidbuchel H, Wittkampf FH, Vano E, et al. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014;16:946–964. doi: 10.1093/europace/eut409. [DOI] [PubMed] [Google Scholar]
- 3.Koenig TR, Mettler FA, Wagner LK. Skin injuries from fluoroscopically guided procedures: part 2, review of 73 cases and recommendations for minimizing dose delivered to patient. AJR Am J Roentgenol. 2001;177:13–20. doi: 10.2214/ajr.177.1.1770013. [DOI] [PubMed] [Google Scholar]
- 4.Koenig TR, Wolff D, Mettler FA, Wagner LK. Skin injuries from fluoroscopically guided procedures: part 1, characteristics of radiation injury. AJR Am J Roentgenol. 2001;177:3–11. doi: 10.2214/ajr.177.1.1770003. [DOI] [PubMed] [Google Scholar]
- 5.Park TH, Eichling JO, Schechtman KB, Bromberg BI, Smith JM, Lindsay BD. Risk of radiation induced skin injuries from arrhythmia ablation procedures. Pacing Clin Electrophysiol. 1996;19:1363–1369. doi: 10.1111/j.1540-8159.1996.tb04216.x. [DOI] [PubMed] [Google Scholar]
- 6.Rosenthal LS, Mahesh M, Beck TJ, et al. Predictors of fluoroscopy time and estimated radiation exposure during radiofrequency catheter ablation procedures. Am J Cardiol. 1998;82:451–458. doi: 10.1016/s0002-9149(98)00356-7. [DOI] [PubMed] [Google Scholar]
- 7.Lindsay BD, Eichling JO, Ambos HD, Cain ME. Radiation exposure to patients and medical personnel during radiofrequency catheter ablation for supraventricular tachycardia. Am J Cardiol. 1992;70:218–223. doi: 10.1016/0002-9149(92)91278-c. [DOI] [PubMed] [Google Scholar]
- 8.Vañó E, Arranz L, Sastre JM, et al. Dosimetric and radiation protection considerations based on some cases of patient skin injuries in interventional cardiology. Br J Radiol. 1998;71:510–516. doi: 10.1259/bjr.71.845.9691896. [DOI] [PubMed] [Google Scholar]
- 9.Glazier JJ, Dixon SR. Skin injury following prolonged fluoroscopy: early and late appearances. QJM. 2012;105:571–573. doi: 10.1093/qjmed/hcr089. [DOI] [PubMed] [Google Scholar]
- 10.Nahass GT. Acute radiodermatitis after radiofrequency catheter ablation. J Am Acad Dermatol. 1997;36:881–884. doi: 10.1016/s0190-9622(97)70047-1. [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal LS, Beck TJ, Williams J, et al. Acute radiation dermatitis following radiofrequency catheter ablation of atrioventricular nodal reentrant tachycardia. Pacing Clin Electrophysiol. 1997;20:1834–1839. doi: 10.1111/j.1540-8159.1997.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 12.Vlietstra RE, Wagner LK, Koenig T, Mettler F. Radiation burns as a severe complication of fluoroscopically guided cardiological interventions. J Interv Cardiol. 2004;17:131–142. doi: 10.1111/j.1540-8183.2004.09885.x. [DOI] [PubMed] [Google Scholar]
- 13.Wagner L. Radiation injury is a potentially serious complication to fluoroscopically-guided complex interventions. Biomed Imaging Interv J. 2007;3:e22. doi: 10.2349/biij.3.2.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shope TB. Radiation-induced skin injuries from fluoroscopy. Radiographics. 1996;16:1195–1199. doi: 10.1148/radiographics.16.5.8888398. [DOI] [PubMed] [Google Scholar]
- 15.Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. J Vasc Interv Radiol. 1994;5:71–84. doi: 10.1016/s1051-0443(94)71456-1. [DOI] [PubMed] [Google Scholar]
- 16.Mettler FA, Jr, Koenig TR, Wagner LK, Kelsey CA. Radiation injuries after fluoroscopic procedures. Semin Ultrasound CT MR. 2002;23:428–442. doi: 10.1016/s0887-2171(02)90014-4. [DOI] [PubMed] [Google Scholar]