Abstract
Background and Objectives
Joint National Committee guidelines attempt to vary treatment recommendations for patients based on considerations of their comorbidities. The aim of the present study is to estimate the age-standardized prevalence of common comorbidities among Korean hypertension patients.
Subjects and Methods
We analyzed the Korea National Health and Nutrition Examination Survey from 2007 to 2013. Among the 58423 participants, 30092 adults, aged ≥30 yrs who completed a health examination and interview survey, were selected. The survey procedures were used to estimate weighted prevalence and odds ratios for 8 comorbidities, including obesity, diabetes mellitus, dyslipidemia, cardiovascular disease, chronic kidney disease, and thyroid disease.
Results
Most chronic conditions were more prevalent in adults with hypertension than in those without hypertension. Common comorbidities were obesity (60.1%), dyslipidemia (57.6%), and impaired fasting glucose (45.1%). Hypertensive patients with two or more comorbid diseases were 42.2% and those with three or more diseases were 17.7%. The age- and sex-specific prevalence of three or more comorbid diseases among male hypertension patients was significantly higher than those patients in the 30-59 (p<0.05) age group.
Conclusion
Comorbidity is highly prevalent in Korean patients with hypertension.
Keywords: Hypertension, Chronic disease, Epidemiology, Prevalence, Korea
Introduction
Comorbidity is a common and notable status concerning the increasing complexity of care associated with it. In developed countries, more than 50% of older adults have three or more chronic conditions1) and more than 20% of all patients were multimorbid.2) It has been suggested that managing multiple comorbidities requires more complex strategies to achieve effective care. However the prevalence estimates of multiple comorbidities differed significantly among studies.3),4)
The prevalence of comorbidity among people with hypertension is more common than those individuals with a normal BP. The comorbidity prevalence of hypertension has been estimated several times and estimates were inconsistent among publications from the government and those from academic societies.5) The marked differences of prevalence in several studies are due to the different reference population, the various study designs, inclusion of diseases categories, working definition of comorbidity, and representativeness of the data.
Among various routine data, information on several health statuses could be reflected better in health surveys than in medical records.6) Compared to other routine data, the KNHANES survey, which includes both a social and health status, could provide better representative prevalence estimates of diseases, including comorbidity with hypertension. The aim of the present study is to estimate the prevalence of comorbidity among Korean hypertension patients based on the KNHANES.
Subjects and Methods
This study analyzed the data from the KNHANES IV-VI (2007-2013). The KNHANES is a nationwide cross-sectional survey, conducted by the Korea Centers for Disease Control and Prevention (KCDC). The survey design, data collection, and detailed protocols in the KNHANES have been published.7) The survey chose a stratified and multistage clustered probability sampling method to select the representative households of Korean citizens who live in Korea. The KNHANES was initiated in 1998, was conducted tri-annually until 2006 and converted to an annual survey from 2007 to 2013. The survey was designed to provide the representative statistics on the health and nutrition status of the Korean population and was composed of 3 major parts: health interview, health examination, and nutrition. Trained medical staff and interviewers collected information about the age, gender, socioeconomic status, education, insurance type and lifestyle. The questionnaires included history of several chronic diseases by a physician diagnosis and current use of agents for those diseases. The response rate varied between 70.2% and 86.5% for KNHANES I-VI.7) Among total 55,386 participants, only those who performed the survey on comorbidities completely were included. The data from 30092 adults, aged ≥30 yrs was used to analyze the prevalence of comorbidities among patient with hypertension.
Mobile examination centers and trained medical staff such as nurses measured the anthropometric and biochemical information. The standard protocol was adapted when measuring for blood pressure (BP), blood sample collection and biochemical analysis. After of at least 5 minutes of rest and in sitting position, BP was measured on the right arm by a mercury sphygmomanometer. To increase accuracy, BP was measured three times and the mean of the second and third BP was calculated. All samples were venous blood gatherings in the morning after an 8 hr fast. Since 2005, for quality control, the protocol applied to all laboratory analyses and laboratory data was monitored to meet the standards with validity and reliability. Hypertension was defined as an average SBP ≥140 mmHg, DBP ≥90 mmHg or the presence of antihypertensive agents. Prehypertension was defined as an average SBP 120-139 mmHg or DBP 80-89 mmHg. Diabetes mellitus (DM) was defined as having a fasting plasma glucose ≥126 mg/dL, the current use of antidiabetic agents or the use of insulin prescribed by physician due to a previous diagnosis of diabetes. Impaired fasting glucose (IFG) was determined by the range; 100 mg/dL≤ fasting plasma glucose (FPG) <126 mg/dL. The diagnosis of hypercholesterolemia was defined as a total plasma cholesterol of ≥240 mg/dL after an 8 hour fast or current use of cholesterol-lowering agents. Hypertriglyceridemia was defined as triglyceride levels >200 mg/dL after a 12 hour fast. For the precise definition, KNHANES team released the triglyceride level of samples after a 12 hr fasting time and coded that of samples between 8 hr and 12 hr fast as a missing value. Hypo-HDL-cholesterolemia was regarded as HDL-C levels <40 mg/dL, and hyper-LDL-cholesterolemia was considered as LDL-C levels >160 mg/dL. Dyslipidemia was defined as hypercholesterolemia, hypertriglyceridemia, hypo-HDL-cholesterolemia, or hyper-LDL-cholesterolemia.8) Body mass index (BMI) was calculated as body mass divided by the square of height (kg/m2). Obesity was considered as a BMI of ≥25 kg/m2, according to the WHO Asia–Pacific region guidelines, redefined for the Asian population.9) Central, or abdominal, obesity was regarded as a waist circumference (WC) ≥90 cm for men and ≥85 cm for women. Obesity in logistic analysis was defined as obesity or central obesity. Stroke, myocardial infarction (MI), angina, chronic kidney disease (CKD), and thyroid disease were defined as being a previous diagnosis given by a physician. CVD was defined as the previous diagnosis of stroke, MI, or angina. Proteinuria was defined as a urine test strip ≥1+, azotemia as blood urea nitrogen (BUN) ≥18 mg/dL, and increased level of creatinine as serum creatinine (SCr) ≥1.6 mg/dL. Anemia was defined in accordance with WHO criteria:10) hemoglobin (Hb)<11.5 g/dL at 10-11 yr; Hb<12.0 g/dL at 12-14 yr; <13.0 g/dL in males ≥15 yr; Hb<12.0 g/dL among non-pregnant females ≥15 yr; and Hb<11.0 g/dL during pregnancy. Elevated liver enzyme was defined as aspartate aminotransferase >35 IU/L or alanine aminotransferase >40 IU/L. The number of comorbid diseases or multimorbidity was defined as the number of diseases among DM, obesity, dyslipidemia, CVD, CKD, thyroid disease, anemia, and liver function test abnormalities.
Survey procedures of the Statistical Analysis System program (SAS 9.3 Institute Inc., Cary, NC, USA) were used to perform the analysis of a complex sample data. The sampling weights were applied to all analyses in order for the results to represent the Korean population as a whole. Sampling weights were used to reflect a complex sample design, non-response rate, and post-stratification. A surveymeans procedure was used to find the prevalence of comorbidities related to hypertension, and a surveylogistic procedure was used concerning the association between comorbidities and hypertension. The results were presented with a weighted percentage and 95% confidence interval (CI)s. The results of association analysis were presented using odds ratio (OR) and 95% CI. Significance of the association between comorbidities and hypertension was tested through a surveylogistic regression analysis. Statistically significant differences between effect estimates across strata of a potential effect modifier (e.g., the difference between male and female) were determined by calculating 95% CIs.11) Differences with a two-sided p-value of <.05 were considered statistically significant.
Results
Table 1 describes the demographic characteristics of subjects. Among a total of 30092 adults aged ≥30, the number of males (13358) were less than that of females (16734); the weighted percent for males was 51.2 (95% CI 50.7-51.7) and was larger than that for females; 48.8 (95% CI 48.3-49.3).
Table 1. Demographic characteristics of participants above 30 years old.
| Characteristics | Total (N=30092) | Male (n=13358) | Female (n=16734) | p | |||
|---|---|---|---|---|---|---|---|
| N | Percent (95% CI) | N | Percent (95% CI) | N | Percent (95% CI) | ||
| Age group (years) | <.001 | ||||||
| 30–39 | 6364 | 25.7 (24.8-26.6) | 2873 | 27.7 (26.6-28.9) | 3491 | 23.6 (22.6-24.5) | |
| 40–49 | 6482 | 27.4 (26.6-28.3) | 3018 | 28.9 (27.8-30.0) | 3464 | 25.9 (24.9-26.8) | |
| 50–59 | 6638 | 23.3 (22.6-24.0) | 2812 | 22.8 (21.8-23.7) | 3826 | 23.9 (23.1-24.7) | |
| 60–69 | 5923 | 13.6 (13.1–14.1) | 2633 | 12.7 (12.1–13.3) | 3290 | 14.7 (14.0–15.3) | |
| 70–79 | 4685 | 9.9 (9.5-10.4) | 2022 | 8.0 (7.5-8.4) | 2663 | 12.0 (11.4-12.6) | |
| Marital status | <.001 | ||||||
| Single | 1251 | 6.2 (5.8–6.6) | 0818 | 9.1 (8.3–9.8) | 0433 | 3.2 (2.8–3.5) | |
| Married | 24528 | 81.8 (81.1–82.5) | 11803 | 85.7 (84.8–86.5) | 12725 | 77.7 (76.8–78.5) | |
| Widowed, divorced, and separated | 4313 | 12.0 (11.5–12.5) | 0737 | 5.2 (4.8–5.7) | 3576 | 19.1 (18.3–19.9) | |
| Education level | <.001 | ||||||
| ≤ Elementary school | 5472 | 14.3 (13.6–14.9) | 1408 | 7.9 (7.3–8.5) | 4064 | 21.0 (20.1–21.9) | |
| Middle school | 5029 | 14.0 (13.5–14.6) | 1941 | 11.7 (11.0–12.4) | 3088 | 16.5 (15.8–17.2) | |
| High school | 7026 | 25.9 (25.1–26.7) | 3288 | 26.3 (25.2–27.3) | 3738 | 25.5 (24.6–26.4) | |
| ≥ College | 12565 | 45.8 (44.7–46.9) | 6721 | 54.1 (52.8–55.4) | 5844 | 37.0 (35.8–38.2) | |
| Household monthly income | <.001 | ||||||
| <25th | 6253 | 16.4 (15.7–17.2) | 2420 | 13.6 (12.8–14.3) | 3833 | 19.5 (18.5–20.4) | |
| 25–49th | 7622 | 25.9 (25.0–26.8) | 3375 | 25.3 (24.3–26.4) | 4247 | 26.5 (25.5–27.5) | |
| 50–75th | 7989 | 28.5 (27.7–29.4) | 3704 | 30.0 (29.0–31.0) | 4285 | 27.0 (26.1–27.9) | |
| ≥75th | 8228 | 29.1 (28.0–30.3) | 3859 | 31.1 (29.8–32.4) | 4369 | 27.1 (25.9–28.2) | |
| Type of health insurance | <.001 | ||||||
| Medical aid | 0925 | 2.8 (2.4–3.1) | 0303 | 2.1 (1.8–2.4) | 0622 | 3.5 (3.0–3.9) | |
| National Health Insurance | 29167 | 97.2 (96.9–97.6) | 13055 | 97.9 (97.6–98.2) | 16112 | 96.5 (96.1–97.0) | |
| Living area | 0.543 | ||||||
| Urban area | 22638 | 78.6 (76.4–80.9) | 10001 | 78.5 (76.2–80.8) | 12637 | 78.8 (76.5–81.0) | |
| Rural area | 7454 | 21.4 (19.1–23.6) | 3357 | 21.5 (19.2–23.8) | 4097 | 21.2 (19.0–23.5) | |
Hypertension patients had a higher proportion of comorbidity than adults with prehypertension in several diseases (Table 2). Prehypertension patients also tended to have a higher proportion of comorbidity than normal people without prehypertension. Obesity was 2.17 times (60.1%) more common among hypertension patients than among the normotensive group (27.7%). The prevalence of DM among people with hypertension (14.7%) was 2.37 times higher than in adults without hypertension (6.2%). In addition, hypertension patients had a 1.51 times higher prevalence of dyslipidemia (57.6%) than adult with normal BP (38.1%). CVD prevalence was 3.6% for hypertension patients, which was 2.00 times higher than the 1.8% for normotensive adults. Specifically, the prevalence of stroke was 3.40 times more common among adults with hypertension 1.7% than that among adults with normal BP 0.5%.
Table 2. The prevalence of comorbid diseases among participants.
| Type of comorbid diseases | Normal (n=13167) | Prehypertension (n=7100) | Hypertension (n=9825) | p | |||
|---|---|---|---|---|---|---|---|
| N | Percent (95% CI) | N | Percent (95% CI) | N | Percent (95% CI) | ||
| Obesity | 3513 | 27.7 (26.8–28.7) | 2931 | 43.0 (41.5–44.5) | 5369 | 60.1 (58.2–61.9) | <.001 |
| Diabetes mellitus | 694 | 6.2 (5.7–6.7) | 718 | 8.8 (8.0–9.6) | 2070 | 14.7 (13.7–15.8) | <.001 |
| Impaired fasting glucose | 2601 | 21.6 (20.7–22.5) | 2428 | 32.7 (31.2–34.1) | 4913 | 45.1 (43.3–47.0) | <.001 |
| Dyslipidemia | 3861 | 38.1 (36.9–39.2) | 2738 | 47.0 (45.3–48.6) | 4860 | 57.6 (55.4–59.7) | <.001 |
| Cardiovascular disease | 187 | 1.8 (1.5–2.1) | 187 | 1.9 (1.6–2.3) | 731 | 3.6 (3.2–4.0) | <.001 |
| Stroke | 60 | 0.5 (0.4–0.7) | 61 | 0.6 (0.4–0.8) | 327 | 1.7 (1.4–2.0) | <.001 |
| Myocardial infarction | 58 | 0.6 (0.4–0.8) | 44 | 0.5 (0.3–0.6) | 137 | 0.7 (0.5–0.9) | <.001 |
| Angina | 84 | 0.8 (0.6–1.0) | 86 | 0.9 (0.7–1.1) | 308 | 1.4 (1.2–1.6) | <.001 |
| Chronic kidney disease | 11 | 0.1 (0.02–0.2) | 8 | 0.1 (0.02–0.2) | 43 | 0.4 (0.1–0.6) | <.001 |
| Liver function test abnormality | 1264 | 10.4 (9.7–11.0) | 1201 | 18.9 (17.7–20.1) | 1690 | 26.3 (24.5–28.0) | <.001 |
| Thyroid disease | 288 | 2.0 (1.7–2.3) | 136 | 1.4 (1.1–1.7) | 195 | 1.5 (1.0–1.9) | 0.20 |
| Anemia | 1426 | 9.9 (9.3–10.5) | 467 | 5.6 (5.0–6.2) | 892 | 5.6 (5.0–6.2) | <.001 |
| Number of comorbid diseases | <.001 | ||||||
| 0 | 6780 | 50.4 (49.3–51.5) | 2958 | 43.9 (42.4–45.4) | 2922 | 35.2 (33.2–37.1) | <.001 |
| 1 | 3752 | 27.9 (27.0–28.9) | 1960 | 26.3 (25.0–27.6) | 2448 | 22.7 (21.1–24.3) | <.001 |
| 2 | 1956 | 16.0 (15.2–16.8) | 1472 | 19.9 (18.7–21.1) | 2588 | 24.5 (22.9–26.0) | <.001 |
| ≥3 | 679 | 5.6 (5.1–6.1) | 710 | 9.9 (9.0–10.8) | 1867 | 17.7 (16.3–19.2) | <.001 |
The number of comorbid diseases was defined by the number of diseases among diabetes mellitus, obesity, dyslipidemia (hypercholesterolemia, hypertriglyceridemia, hypo-HDL-cholesterolemia, or hyper-LDL-cholesterolemia), cardiovascular disease (stroke, myocardial infarction, or angina), CKD, thyroid disease, anemia, and liver function test abnormalities. HDL: high density lipoprotein, LDL: low density lipoprotein, CKD: chronic kidney disease
Among patients with 2 to 5 comorbid diseases and the more diseases an adult had, the prevalence was more common than for those adults with a normal BP (1.53, 2.89, 4.43, and 4.00 times higher prevalence, respectively). Patients with 3 or more comorbid diseases accounted for 17.7% (95% CI 16.3-19.2%) of hypertensive patients, which was 3.16 times more common than normotensive adults, 5.6% (95% CI 5.1-6.1%). Among subjects with prehypertension, the prevalence of adults with 2 or more comorbid diseases was 29.8%, and those with 3 or more diseases was 9.9%. Among hypertensive patients, prevalence was 42.2% and 17.7%, respectively.
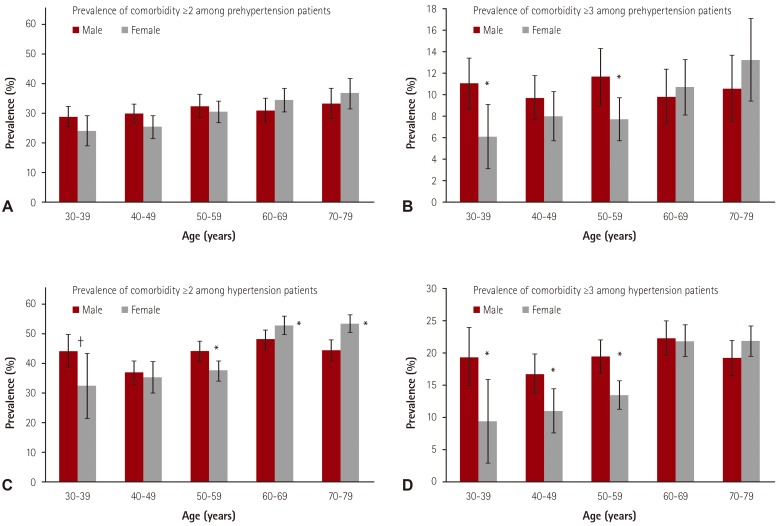
Male hypertensive patients had a higher prevalence of diseases including liver function test abnormalities, dyslipidemia, and impaired fasting glucose (Table 3). Meanwhile, hypo-HDL-cholesterolemia, hypercholesterolemia, thyroid disease, anemia and central obesity were more common among female hypertensive patients than among males (data not shown). The prevalence of 1 or 2 comorbid diseases among female patients was higher than that among male patients. However, hypertensive patients without disease or with at least 3 diseases were more common among males than females. Although most of the difference in the prevalence of multimorbidity between both sexes was non-significant, male hypertensive patients aged 30-39 (19.4±4.55%), 40-49 (16.8±3.05%) and 50-59 (19.5±2.65%) had a significantly elevated prevalence compared to females (9.4±6.5%, 11.0±3.45%, 13.5±2.20%), respectively (Fig. 1).
Table 3. The prevalence of comorbid diseases among participants, stratified by gender.
| Type of comorbid diseases | Normal (Male 4916, Female 8251) |
Prehypertension (Male 3785, Female 3315) |
Hypertension (Male 4657, Female 5168) |
p | |||
|---|---|---|---|---|---|---|---|
| N | Percent (95% CI) | N | Percent (95% CI) | N | Percent (95% CI) | ||
| Male | |||||||
| Obesity | 1471 | 29.8 (28.3–31.2) | 1576 | 43.4 (41.6–45.3) | 2445 | 59.9 (57.8–62.0) | <.001 |
| Diabetes mellitus | 379 | 8.2 (7.3–9.1) | 406 | 9.3 (8.3–10.4) | 988 | 15.4 (14.1–16.7) | <.001 |
| Impaired fasting glucose | 1280 | 26.5 (25.1–28.0) | 1433 | 35.7 (33.9–37.6) | 2519 | 48.1 (45.9–50.2) | <.001 |
| Dyslipidemia | 1768 | 47.3 (45.4–49.2) | 1487 | 50.0 (47.8–52.2) | 2235 | 60.2 (57.6–62.8) | <.001 |
| Cardiovascular disease | 113 | 2.4 (1.9–2.9) | 112 | 2.3 (1.8–2.8) | 356 | 4.0 (3.4–4.5) | <.001 |
| Chronic kidney disease | 4 | 0.1 (0.0–0.1) | 5 | 0.1 (0.0–0.3) | 17 | 0.4 (0.04–0.7) | <.01 |
| Liver function test abnormality | 865 | 17.4 (16.2–18.7) | 893 | 23.7 (22.1–25.4) | 1130 | 31.7 (29.6–33.9) | <.001 |
| Thyroid disease | 32 | 0.5 (0.3–0.7) | 24 | 0.5 (0.2–0.7) | 23 | 0.3 (0.1–0.5) | 0.49 |
| Anemia | 174 | 3.5 (2.9–4.1) | 127 | 2.7 (2.1–3.2) | 269 | 3.2 (2.6–3.8) | <.001 |
| Number of comorbid disease | |||||||
| 0 | 2447 | 50.0 (48.3–51.6) | 1616 | 44.3 (42.4–46.2) | 1560 | 37.1 (34.9–39.4) | <.001 |
| 1 | 1256 | 25.1 (23.7–26.5) | 991 | 25.3 (23.6–26.9) | 1050 | 20.4 (18.6–22.1) | <.001 |
| 2 | 863 | 18.0 (16.8–19.3) | 764 | 19.8 (18.3–21.3) | 1137 | 23.5 (21.7–25.3) | <.001 |
| ≥3 | 350 | 6.9 (6.1–7.7) | 414 | 10.6 (9.4–11.8) | 910 | 19.0 (17.3–20.8) | <.001 |
| Female | |||||||
| Obesity | 2042 | 26.5 (25.3–27.8) | 1355 | 39.4 (37.0–41.8) | 2924 | 55.5 (51.6–59.5) | <.001 |
| Diabetes mellitus | 315 | 4.6 (4.0–5.2) | 312 | 8.2 (7.0–9.5) | 1082 | 14.7 (12.3–17.1) | <.001 |
| Impaired fasting glucose | 1321 | 17.8 (16.7–18.9) | 995 | 28.5 (26.3–30.6) | 2394 | 41.3 (37.2–45.3) | <.001 |
| Dyslipidemia | 2093 | 31.9 (30.6–33.2) | 1251 | 40.6 (38–43.2) | 2625 | 50.3 (46.0–54.6) | <.001 |
| Cardiovascular disease | 74 | 1.3 (0.9–1.6) | 75 | 1.5 (1.1–1.9) | 375 | 3.6 (2.6–4.6) | <.001 |
| Chronic kidney disease | 7 | 0.1 (0.0–0.2) | 3 | 0.1 (0.0–0.1) | 26 | 0.3 (0.1–0.5) | <.001 |
| Liver function test abnormality | 399 | 4.8 (4.2–5.4) | 308 | 9.3 (7.8–10.8) | 560 | 11.2 (8.8–13.5) | <.001 |
| Thyroid disease | 256 | 3.1 (2.7–3.6) | 112 | 2.9 (2.1–3.6) | 172 | 4.4 (2.1–6.7) | 0.61 |
| Anemia | 1252 | 15 (14–15.9) | 340 | 12.1 (10.5–13.7) | 623 | 10.9 (8.8–13.1) | <.001 |
| Number of comorbid diseases | |||||||
| 0 | 4333 | 50.6 (49.3–52.0) | 1342 | 44.0 (41.5–46.5) | 1362 | 31.8 (28.1–35.5) | <.001 |
| 1 | 2496 | 30.2 (28.9–31.4) | 969 | 28.0 (25.8–30.2) | 1398 | 29.5 (25.6–33.4) | 0.02 |
| 2 | 1093 | 14.5 (13.6–15.5) | 708 | 19.8 (17.9–21.7) | 1451 | 25.3 (21.8–28.8) | <.001 |
| ≥3 | 329 | 4.7 (4.1–5.3) | 296 | 8.2 (6.9–9.5) | 957 | 13.4 (11.1–15.7) | <.001 |
The number of comorbid diseases was defined by the number of diseases among diabetes mellitus, obesity, dyslipidemia (hypercholesterolemia, hypertriglyceridemia, hypo-HDL-cholesterolemia, or hyper-LDL-cholesterolemia), cardiovascular disease (stroke, myocardial infarction, or angina), CKD, thyroid disease, anemia, and liver function test abnormalities. HDL: high density lipoprotein, LDL: low density lipoprotein, CKD: chronic kidney disease
Fig. 1. The prevalence of comorbidity ≥2 diseases (A, C) and ≥3 diseases (B, D) and 95% confidence intervals among people with hypertension by sex and age group. *p<0.05, †p<0.10.
After adjustment for sex, age, marital status, education level, household income, smoking, alcohol drinking, exercise, type of insurance, and living area, the odds ratio was significantly elevated among hypertensive patients (Table 4). Hypertensive patients were more than 2 times as likely to have some comorbid diseases compared to adults without hypertension. ORs were for CKD; 3.94 (95% CI 1.71-9.07), obesity; 2.60 (95% CI 2.43-2.78), CVD; 2.11 (95% CI 1.78-2.50), DM; 2.22 (95% CI 2.02-2.45), liver function test abnormality; 1.82 (95% CI 1.65-2.01), comorbid diseases ≥3; 2.63 (95% CI 2.37-2.92) and comorbid diseases ≥2; 2.10 (95% CI 1.96-2.26). Hypertensive patients were also 1.74 times more likely to have dyslipidemia than those with a normal BP (95% CI 1.62-1.88). Anemia and thyroid disease were not significantly different compared with adults without hypertension.
Table 4. Adjusted odds ratios with 95% confidence interval for comorbidity conditions in women and men with hypertension.
| Type of comorbid diseases | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Chronic kidney disease | 3.94 (1.71–9.07) | <.001 | 3.86 (1.21–12.32) | 0.02 | 3.47 (1.05–11.48) | 0.04 |
| Obesity | 2.60 (2.43–2.78) | <.001 | 2.67 (2.43–2.94) | <.001 | 2.28 (2.07–2.51) | <.001 |
| Cardiovascular disease | 2.11 (1.78–2.50) | <.001 | 1.86 (1.48–2.35) | <.001 | 2.45 (1.88–3.18) | <.001 |
| Diabetes mellitus | 2.22 (2.02–2.45) | <.001 | 2.03 (1.78–2.30) | <.001 | 2.44 (2.11–2.82) | <.001 |
| Liver function test abnormality | 1.82 (1.65–2.01) | <.001 | 1.78 (1.58–2.01) | <.001 | 1.70 (1.42–2.04) | <.001 |
| Dyslipidemia | 1.74 (1.62–1.88) | <.001 | 1.70 (1.53–1.89) | <.001 | 1.68 (1.51–1.88) | <.001 |
| Anemia | 0.88 (0.79–0.99) | 0.03 | 1.03 (0.81–1.31) | 0.80 | 0.92 (0.81–1.05) | 0.22 |
| Thyroid disease | 0.89 (0.70–1.14) | 0.35 | 0.63 (0.33–1.19) | 0.16 | 0.95 (0.72–1.25) | 0.71 |
| Number of comorbid diseases ≥3 | 2.63 (2.37–2.92) | <.001 | 2.63 (2.29–3.01) | <.001 | 2.37 (2.03–2.76) | <.001 |
| Number of comorbid diseases ≥2 | 2.10 (1.96–2.26) | <.001 | 2.00 (1.82–2.21) | <.001 | 2.08 (1.87–2.30) | <.001 |
Adjusted for sex (only in total), age, marital status, education level, household income, smoking status, alcohol drinking, exercise, type of insurances, and living area. The number of comorbid diseases was defined by the number of diseases among diabetes mellitus, obesity, dyslipidemia (hypercholesterolemia, hypertriglyceridemia, hypo-HDL-cholesterolemia, or hyper-LDL-cholesterolemia), cardiovascular disease (stroke, myocardial infarction, or angina), CKD, thyroid disease, anemia, and liver function test abnormalities. HDL: high density lipoprotein, LDL: low density lipoprotein, CKD: chronic kidney disease
Discussion
The objective of the current study was to investigate the prevalence of comorbidity among Korean hypertensive patients based on the national representative survey. In this study, we compared the prevalence of comorbid diseases and multimorbidity in hypertensive patients among adults aged ≥30 years, using KNHANES 2007-2013.
Although several studies to estimate the prevalence of comorbidity among hypertension patients have been undertaken, the estimates have not yet been fully established and are still controversial between publications from the government and academic society. The prevalence estimates of multiple comorbidities also differ significantly among studies3),4) and the definition of it is still the subject of controversy. Even in Korea, the estimates of multimorbidity among hypertensive patients were different depending on the source of the data. The marked differences in several studies are due to the various study designs, inclusion of diseases, working definition of multimorbidity, and representativeness of the data.
Among the study population, the prevalence of hypertension (27.4 for total, 30.6% for male and 23.5% for female) was relatively lower than the result (56.0% for total) of the research by the Working Group of the Italian Society of Hypertension12) or the findings (52.4% for male and 37.8% for female) in the Progetto CUORE cohort study by the Italian Ministry of Health.13) The prevalence of acute myocardial infarction, stroke, and angina pectoris were similar to that in the Progetto CUORE cohort study (0.9, 1.2, and 1.1% for male and 0.3, 0.8, and 1.1% for female.
In agreement with similar studies,14),15),16) common comorbidities of hypertensive patients were dyslipidemia, obesity, and impaired fasting glucose. Seven of the eight chronic conditions were more prevalent in hypertensive patients than in adults without hypertension. Among hypertension patients aged ≥30 years, 64.8% suffer from 1 or more comorbidities, 42.2% from 2 or more diseases, and 17.7% had 3 or more comorbidities. Comorbidity was more common among adults with hypertension than among those without high BP. Male hypertensive patients with 3 or more diseases were more common than female patients. The results of the present study correspond well with those found in earlier studies that stated comorbidity proportions of several diseases tended to be the highest among hypertensive patients, following prehypertension and normal people without prehypertension.17) The results of the present study correspond well with those found in the earlier systematic review which reported that multimorbidity influence more than half of the elderly population.4) These results expanded upon previous multimorbidity studies of adults, elucidating the high prevalence of multimorbidity in adults with hypertension.
Stratified by age and sex, male hypertensive patients aged 30-59 had a significantly higher prevalence of multimorbidity ≥3 than female patients. This finding is similar to another study that stated the age and sex-specific prevalence of multimorbidity, more than 2 comorbidities, showed a marked difference among young hypertensive patients; the gap declined until age 70 and only between ages 70-79 did the prevalence among females exceed that among males.18) These findings might be attributed to the disparities in the diagnosis and treatment, which has been discussed in other studies.19),20) In terms of the prevalence of multimorbidity≥2, female patients aged 60-79 had significantly higher estimates than male patients. Several studies have shown a higher prevalence of multimorbidity, more than 1 comorbid disease, among females compared to males. This could possibly be due to a longer life expectancy and the biological and social status related with a declining health status of females.21),22)
In an association analysis, the results of the present study are similar to the previous report.23) After adjustment for age, sex, marital status, socioeconomic status, insurance, and living area, hypertension had a positive association with the risk of multiple comorbidities. Stratified by sex among hypertensive patients, the risk for comorbidity was different without statistical significance. Only the risk for obesity was statistically significantly higher among males than among females.
The current study has several limitations. First, the study population could be different from general hypertensive patients. The KNHANES cannot include institutionalized patients and the result could underestimate severe diseases and the prevalence of CKD. That is, KNHANES represents the non-institutionalized general population among Korean citizens. In addition, the target population of this study did not include all hypertensive patients with chronic diseases but only those with 8 diseases, which are known to be hypertensive related diseases. The prevalence of hypertension in this study is different from that of Korea health statistics due to the difference of the study population.24) However, if we used the same inclusion criteria for the target population, the prevalence estimates would be the same. Second, the working definition of some diseases could be different from the diagnosis criteria. Several comorbidities were defined by just 1 laboratory test result and the prevalence might be overestimated due to a possible false positive. Other diseases defined by the current prevalence could be underestimated due to the response rate of questionnaires, varying between 70.2% and 86.5% for KNHANES I-VI.7) Third, the present study was a cross-sectional analysis and could not investigate the factors affecting the prevalence for comorbidities among adults with hypertensive. Fourth, the laboratory and some of the methods for measuring blood concentrations were changed, so glucose and cholesterol level could influence the results of related diseases such as DM or dyslipidemia. However, KCDC attempted to control the quality with a parallel test of the laboratory analysis, to maintain the blood analysis stability, and to suggest the transformation equation.
Although there are several limitations, the present study estimated the prevalence and risk of comorbidity among hypertensive patients based on a continuous survey with nationally representative samples of Korean citizens through health interviews, physical examinations and nutrition surveys (KNHANES). KCDC and related academic societies have managed external quality control programs for all steps (including survey administration, data collection, laboratory analysis and data processing) as well as internal quality assurance and control procedures. The present study could provide national representative descriptive statistics for the care of hypertensive patients with complex comorbid conditions.
The KNHANES was from a quality controlled and standardized survey with a nation-wide representative sample of Korea. We specified the national prevalence estimate of comorbidity among hypertensive patients. In summary, comorbid diseases were common in Korean hypertensive patients and increased with age in both sexes. About 44% of patients with hypertension had at least two comorbidities and 17% had at least three comorbidities. Physicians should have special considerations during the evaluation of patients with comorbidity and hypertension to provide better comprehensive care.
Acknowledgments
This work was supported by the Korean Health Technology R&D Project, Ministry of Health and Welfare (HI13C0715), Republic of Korea.
The authors wish to thank Yumi Cho, Division of Health and Nutrition Survey, Korea Centers for Disease Control and Prevention, Republic of Korea, for her helpful comments on statistical analysis.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60:E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 3.Fortin M, Stewart M, Poitras M-E, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10:142–151. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Sung YN, Jang SM, Lim DH, Shin SY, Song HJ, Lee SH. Prescribing patterns of antihypertensive drugs by outpatients with hypertension in 2007. Korean J Clin Pharm. 2009;19:167–179. [Google Scholar]
- 6.Violán C, Foguet-Boreu Q, Hermosilla-Pérez E, et al. Comparison of the information provided by electronic health records data and a population health survey to estimate prevalence of selected health conditions and multimorbidity. BMC Public Health. 2013;13:251. doi: 10.1186/1471-2458-13-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014;174:64–72. doi: 10.1016/j.ijcard.2014.03.163. [DOI] [PubMed] [Google Scholar]
- 8.Lewis SA, Weiss ST, Platts-Mills TA, Burge H, Gold DR. The role of indoor allergen sensitization and exposure in causing morbidity in women with asthma. Am J Respir Crit Care Med. 2002;165:961–966. doi: 10.1164/ajrccm.165.7.2103044. [DOI] [PubMed] [Google Scholar]
- 9.Bassett J International Diabetes Institute; World Health Organization Regional Office for the Western Pacific; International Association for the Study of Obesity; International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Melbourne: Health Communications Australia; 2000. [Google Scholar]
- 10.Benoist Bd, McLean E, Cogswell IEaM. Worldwide prevalence of anaemia 1993-2005 of WHO: Global Database of anaemia. Geneva: World Health Organization; 2008. [Google Scholar]
- 11.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tocci G, Muiesan ML, Parati G, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during world hypertension day in Italy. J Clin Hypertens (Greenwich) 2016;18:551–556. doi: 10.1111/jch.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giampaoli S, Palmieri L, Donfrancesco C, Lo Noce C, Pilotto L, Vanuzzo D. Cardiovascular health in Italy. Ten-year surveillance of cardiovascular diseases and risk factors: Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey 1998-2012. Eur J Prev Cardiol. 2015;22(2 Suppl):9–37. doi: 10.1177/2047487315589011. [DOI] [PubMed] [Google Scholar]
- 14.Steinman MA, Lee SJ, Boscardin WJ, et al. Patterns of multimorbidity in elderly veterans. J Am Geriatr Soc. 2012;60:1872–1880. doi: 10.1111/j.1532-5415.2012.04158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in US adults, 1999-2006. NCHS Data Brief. 2010;(36):1–8. [PubMed] [Google Scholar]
- 16.Davila EP, Hlaing WM. Co-Morbidities of Emergency Department Patients Admitted with Essential Hypertension in Florida. Ann Epidemiol. 17:726–727. [Google Scholar]
- 17.Strandberg AY, Strandberg TE, Stenholm S, Salomaa VV, Pitkälä KH, Tilvis RS. Low midlife blood pressure, survival, comorbidity, and health-related quality of life in old age: the Helsinki Businessmen Study. J Hypertens. 2014;32:1797–1804. doi: 10.1097/HJH.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 18.Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14:75. doi: 10.1186/1471-2318-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perelman J, Mateus C, Fernandes A. Gender equity in treatment for cardiac heart disease in Portugal. Soc Sci Med. 2010;71:25–29. doi: 10.1016/j.socscimed.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 20.Bowling A, Bond M, McKee D, et al. Equity in access to exercise tolerance testing, coronary angiography, and coronary artery bypass grafting by age, sex and clinical indications. Heart. 2001;85:680–686. doi: 10.1136/heart.85.6.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García-Olmos L, Salvador CH, Alberquilla Á, et al. Comorbidity patterns in patients with chronic diseases in general practice. PLoS One. 2012;7:e32141. doi: 10.1371/journal.pone.0032141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Violán C, Foguet-Boreu Q, Roso-Llorach A, et al. Burden of multimorbidity, socioeconomic status and use of health services across stages of life in urban areas: a cross-sectional study. BMC Public Health. 2014;14:530. doi: 10.1186/1471-2458-14-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jung YH, Ko SJ, Kim EJ. A study on the effective chronic disease management: Policy directions for chronic diseases management. Seoul: Korea Institute for Health and Social Affairs Press; 2013. [Google Scholar]
- 24.Ministry of Health and Welfare; Korea Centers for Disease Control and Prevention. Korea health statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1) Cheongju: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]