Abstract
Background and Objectives
We estimated the prevalence of hypertension and hypertension subtypes in a large semi-urban city in Korea, using 24-hour ambulatory blood pressure monitoring (ABPM) in a randomly selected sample population.
Subjects and Methods
A random sample (aged 20-65 years) from a city with an adult population of approximately 600000 was selected by using a list-assisted random digit dialing method. The 24-hour ABPM and conventional blood pressure measurement (CBPM) of these individuals were obtained.
Results
Among the 496 participants, valid 24-hour ABPM and CBPM were obtained from 462 (93%) individuals. The estimated prevalence of hypertension in Goyang was 17.54% by CBPM and 32.70% by 24-hour ABPM (p<0.01). In the age stratified analysis, both CBPM and 24-hour ABPM showed increased prevalence of hypertension with age. The estimated prevalence of masked hypertension was 16.22% and that of white-coat hypertension was 1.08%. Men had a higher prevalence of masked hypertension than women (20.79% vs. 11.86%, p=0.0295). The estimated prevalence of masked hypertension was 17.5%, 20.58%, 24.34%, and 13.29% in the age categories of 30s, 40s, 50s, and 60s, respectively. The estimated prevalence of masked uncontrolled hypertension was 26.79% in patients with hypertension who were taking antihypertensive medications.
Conclusion
The estimated prevalence of hypertension by 24-hour ABPM was higher than that by CBPM, revealing high prevalence of masked hypertension. The high prevalence of masked hypertension supports the adoption of ABPM in the national population survey and clinical practice to improve public health and reduce health care costs.
Keywords: Masked hypertension, Ambulatory blood pressure monitoring, Prevalence
Introduction
Hypertension is an important risk factor for cardiovascular disease worldwide.1),2) Blood pressure (BP) lowering has been shown to be effective in reducing the risk of major cardiovascular events.2),3) The diagnosis of hypertension is traditionally made by conventional BP measurement (CBPM). The often-reported prevalence of hypertension in population surveys is based on multiple measurements of conventional BP using a mercury or automated sphygmomanometer.4),5)
Ambulatory BP monitoring (ABPM) has been shown to provide a stronger and better prediction of cardiovascular events than CBPM.6),7) ABPM has several advantages over CBPM, including the potential revelation of the subtype of hypertension (white-coat or masked hypertension),8) and enhanced cost-effectiveness compared to the CBPM.9) Patients with masked hypertension have shown higher incidence of cardiovascular events compared to normotensive individuals.10) Despite the increased use of ABPM in clinical practice and cohort studies, a population-based survey using ABPM to estimate the prevalence of hypertension and hypertension subtypes among Asian population has been rarely performed.11),12) Although the Ohasama11) and JingNing12) studies were performed on Asian populations, the study populations were selected from small towns within rural areas, and thus, they are not representative of a large, urban city.
We estimated the prevalence of hypertension and hypertension subtypes in a large semi-urban city in Korea, using 24-hour ABPM in a randomly selected sample based on the statistical weighting method.
Subjects and Methods
The original study was planned to estimate the sodium intake of the adult population of about 600000 in Goyang, a large semi-urban city and one of the largest cities in Korea. A random sample of adults in the city was selected by list-assisted random digit dialing (LARDD).13) The study design has been described in detail, elsewhere.14) In brief, a random sample of both listed and unlisted telephone households was selected by LARDD and adults aged between 20 and 65 years within the selected households were selected by a telephone interview. Of the 20000 sample telephone numbers, 10576 were working telephone numbers, and 1623 (8.1%) households were contacted and they were determined to be adult households. Of these households, 875 (4.4%) households agreed to take part in the study, and 496 (2.5%) participants visited the clinical trial center and participated in the planned study. The study protocol was reviewed and approved by Institutional Review Board of Dongguk University Ilsan Hospital. Every participant gave written informed consent.
Participants visited the clinical trial center before 08:30 AM to receive instructions on the detailed study procedure and to provide their informed consent. Conventional BP in both arms in a sitting position was measured using a validated semiautomatic device (Watch BP Office, Microlife AG, Widnau, Switzerland) by a trained nurse. Conventional BP was measured three times at 1 min intervals after 5 min rest, and three systolic and diastolic BP values in each arm were averaged. Ambulatory BP was measured for 24 hour at a 30 min interval (Mobil-O-Graph, I.E.M. GmbH, Stolberg, Germany).15) For obtaining more than 70% of the expected measurements, 14 measurements during the day and 7 measurements at night were determined as a valid measurement.8) Fasting blood glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low density lipoprotein cholesterol, serum sodium and potassium levels were measured in sampled blood after at least 8 hours of overnight fasting.
Hypertension was defined according to the European Society of Hypertension/European Society of Cardiology guidelines for the management of arterial hypertension.16) Hypertension by conventional BP measurement was defined as recording of a systolic BP (SBP) ≥140 mmHg or a diastolic BP (DBP) ≥90 mmHg in one of the arms, or the current use of antihypertensive medication in patients with a previous diagnosis of hypertension. Hypertension by ABPM was defined as a 24-hour average SBP ≥130 mmHg or a 24-hour average DBP ≥80 mmHg, or the current use of antihypertensive medications. White-coat hypertension was defined as a conventional BP ≥140 and/or 90 mmHg and 24-hour ambulatory BP <130 and 80 mmHg in untreated individuals. Conversely, masked hypertension was defined as conventional BP <140 and 90 mmHg and 24-hour ABP ≥130 and/or 80 mmHg in untreated individuals. Masked, uncontrolled hypertension was defined as CBP <140 and 90 mmHg and 24-hour ABP ≥130 and/or 80 mmHg in treated individuals.
We compared the prevalence of hypertension in Goyang to that in Seoul (the largest city in Korea with a population of approximately 10 million), which was estimated in individuals aged 20 to 65 years through the Korea National Health and Nutrition Examination Survey (KNHNES) in 2011.
Statistical analyses were performed using the Statistical Analysis System (SAS) software package version 9.3 (SAS Institute, Cary, NC, USA). To estimate the population characteristics of interest, statistical weights were used to correct for imperfections in the sample that may lead to bias due to the selection of respondents with unequal probabilities, non-coverage of the target population, and non-response. To obtain the statistical weight, in the number of adults represented by each respondent in Goyang, we used the following different types of adjustments: random digit dialing initial weight, removal of non-residential phone numbers, household non-response adjustment, creation of person-level weight, person non-response adjustment, and post-stratification weighting based on the population size by age, sex, and region.
Results
Estimated prevalence of hypertension by ambulatory blood pressure monitoring
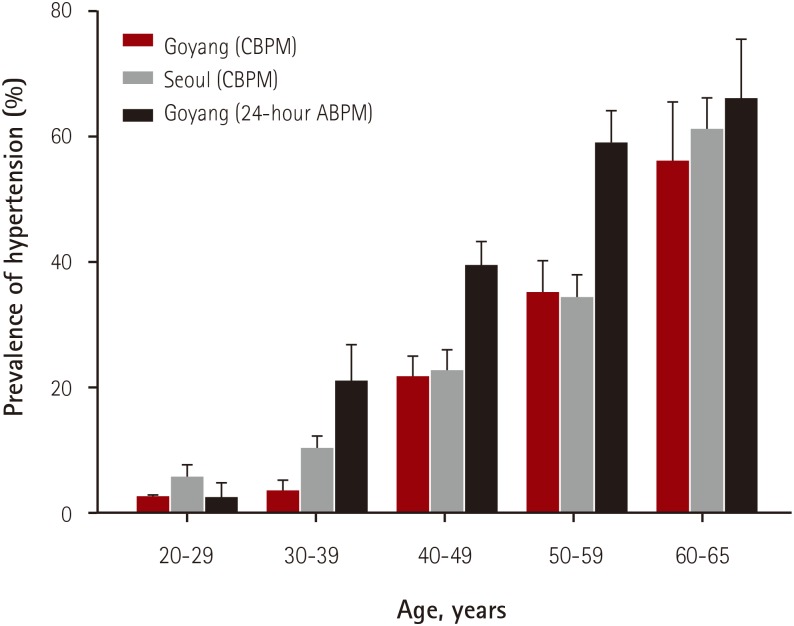
Among the 496 participants, 462 (93.1%) were included in the analysis after exclusion of 34 participants (withdrawal of informed consent of 8 participants, and samples of the 24-hour ABPM were inadequate in 26 participants). The characteristics of the study population are summarized in Tables 1 and 2. The mean age was 46.7±9.4 years (range: 20-65 years). The prevalence of hypertension in the study population was 23.38% by CBPM and 39.83% by 24-hour ABPM (Table 3). The estimated prevalence of hypertension in Goyang was 17.54% by CBPM and 32.70% by 24-hour ABPM (mean difference=15.16 %, 95% confidence interval [CI] 9.65 to 20.67, p<0.01). The estimated prevalence of hypertension in Seoul by CBPM was 21.24%, which was comparable to that in Goyang as recorded by CBPM (p=0.2338, 95% CI -4.96 to 4.34). Age stratified analysis revealed that both CBPM and 24-hour ABPM showed increased prevalence of hypertension with age (Fig. 1). The prevalence of hypertension estimated by 24-hour ABPM in age groups of 30s, 40s and 50s was higher compared to that estimated by CBPM (95% CI 6.78 to 28.22, 8.94 to 26.82, and 12.18 to 35.78, respectively). On the other hand, there was no difference between the prevalence of hypertension estimated by CBPM and 24-hour ABPM in the age group of 20s (95% CI -8.79 to 8.79) and 60s (95% CI -10.48 to 30.98). The estimated prevalence of hypertension by CBPM according to age categories was comparable between Goyang and Seoul.
Table 1. Characteristics of the study population (N=462).
| Variables | Values |
|---|---|
| Mean age (years) | 46.7±9.4 |
| SBP (mmHg) | |
| Right | 115.5±13.2 |
| Left | 117.0±13.7 |
| DBP (mmHg) | |
| Right | 74.1±10.2 |
| Left | 74.7±10.4 |
| 24-hour SBP (mmHg) | 115.9±11.1 |
| 24-hour DBP (mmHg) | 75.4±10.2 |
| Height (cm) | 162.1±8.4 |
| Weight (kg) | 62.9±12.0 |
| Body mass index (kg/m2) | 23.8±3.2 |
| Smoking (%) | 103 (22.3) |
| Drinking (%) | 137 (29.7) |
| Diabetes mellitus (%) | 28 (6.1) |
| Hypertension, treated (%) | 61 (13.2) |
| Fasting blood glucose (mm/dL) | 98.7±18.8 |
| Total cholesterol (mg/dL) | 196.4±34.6 |
| LDL-C (mg/dL) | 121.2±32.1 |
| Triglyceride (mg/dL) | 128.5±92.8 |
| HDL-C (mg/dL) | 57.4±15.8 |
Values are shown as means±standard deviation, or number and percent in parenthesis, as appropriate. SBP: systolic blood pressure, DBP: diastolic blood pressure, LDL-C: low density lipoprotein cholesterol, HDL-C: high density lipoprotein cholesterol
Table 2. Distribution of the study population and the sample from Goyang.
| Variables | Sample (n=462) | Goyang* | ||
|---|---|---|---|---|
| n | % | n | % | |
| Age | ||||
| 20–29 | 24 | 5.2 | 109287 | 18.7 |
| 30–39 | 67 | 14.5 | 149529 | 25.6 |
| 40–49 | 197 | 42.6 | 183461 | 31.3 |
| 50–59 | 131 | 28.4 | 108299 | 18.5 |
| 60–65 | 43 | 9.3 | 29653 | 5.9 |
| Gender | ||||
| Men | 166 | 35.9 | 284784 | 49.0 |
| Women | 296 | 64.1 | 295445 | 51.0 |
*Data from the 2010 Census of population and housing, Korea
Table 3. Prevalence of hypertension by conventional blood pressure measurement and ambulatory blood pressure measurement.
| The study population | Goyang | Seoul | ||||
|---|---|---|---|---|---|---|
| n | % | % (SE) | p* | % (SE) | p* | |
| CBPM | 108 | 23.38 | 17.54 (1.97) | 21.24 (1.46) | ||
| Men | 59 | 34.94 | 26.36 (3.80) | <0.0001 | 26.59 (2.38) | 0.0002 |
| Women | 50 | 16.89 | 10.80 (1.78) | 15.92 (1.67) | ||
| 24-hour ABPM | 184 | 39.83 | 32.70 (2.79) | |||
| Men | 93 | 56.02 | 44.25 (4.94) | <0.0001 | ||
| Women | 91 | 30.74 | 21.57 (2.74) | |||
*by Rao-Scott Chi-Square Test. SE: standard error, CBPM: conventional blood pressure measurement, ABPM: ambulatory blood pressure monitoring
Fig. 1. Estimated prevalence of hypertension according to age categories. Conventional blood pressure in Goyang residents was measured by the semi-automated oscillometric device. Conventional blood pressure in Seoul residents was measured by the auscultatory method with a mercury sphygmomanometer. Standard error was provided. CBPM: conventional blood pressure measurement, ABPM: ambulatory blood pressure monitoring.
Estimated prevalence of masked and white-coat hypertension
The prevalence of masked hypertension in the study population, when the diagnosis of hypertension was determined by 24-hour average BP, daytime BP and nighttime BP, was 17.97% (n=83), 13.85 % (n=64) and 26.41% (n=122), respectively.
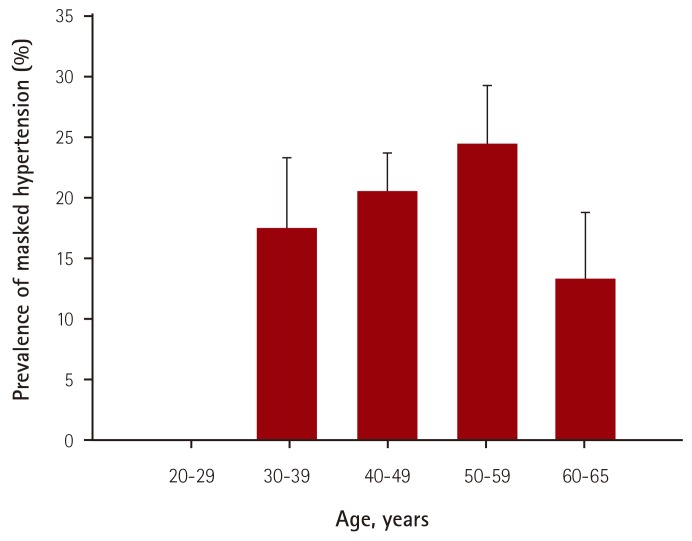
The estimated prevalence of masked hypertension by 24-hour ABPM was 16.22% and that of white-coat hypertension was 1.08% (Table 4). Men had a significantly higher prevalence of masked hypertension than women (20.79% vs. 11.86%, p=0.0295). There was no statistically significant difference in the estimated prevalence of masked hypertension among the age categories. The estimated prevalence of masked hypertension was 17.5%, 20.58%, and 24.34% in the age categories of the 30s, 40s, and 50s, respectively (Fig. 2). Meanwhile, the prevalence of masked hypertension in the 60s age group was 13.29%, which was lower than that in individuals in their 30s, 40s, and 50s, although this difference was statistically insignificant. The estimated prevalence of masked uncontrolled hypertension was 26.79% in patients with hypertension who were taking antihypertensive medications.
Table 4. Estimated prevalence of masked and white coat hypertension.
| Study population, % (n) | Goyang, % (SE) | |
|---|---|---|
| Masked hypertension | 17.97 (83) | 16.22 (2.16) |
| Men* | 23.49 (39) | 20.79 (3.79) |
| Women* | 14.86 (44) | 11.86 (2.17) |
| White coat hypertension | 1.73 (8) | 1.08 (0.43) |
*Prevalence of masked hypertension in men or women of the study population and sample from Goyang. SE: standard error
Fig. 2. The estimated prevalence of masked hypertension according to age categories. Standard error was provided.
Among the hypertensive patients, the estimated rate of treatment (percentage of patients taking antihypertensive medications) was 27.35% by 24-hour ABPM, and 50.99% by CBPM. Among the hypertensive patients, 19.89% of patients were estimated by CBPM and 44.72% of patients were estimated by 24-hour ABPM as having uncontrolled hypertension despite taking antihypertensive medications.
Discussion
Our study is the first study to estimate the prevalence of hypertension by ABPM in a population-based survey in Korea, and to report the prevalence of masked hypertension in the general population in Korea. The prevalence of hypertension in most nationwide surveys is estimated by CBPM and not by ABPM. White-coat and masked hypertension are the representative disadvantages of CBPM. Thus, the reported prevalence of hypertension by CBPM may not reflect the true prevalence of hypertension. Although several cohorts have performed ABPM,17) most nationwide surveys have not adopted ABPM to estimate the prevalence of hypertension until most recently. Furthermore, none of the previous studies in the Asian population have performed ABPM in a large urban city through a population-based survey.
The higher prevalence of hypertension by ABPM compared to that by CBPM in our study demonstrates the importance of ABPM because CBPM under-estimates the true prevalence of hypertension by misdiagnosis of masked hypertension as normotension. Moreover, ABPM is considered to be a feasible method for estimating the prevalence of hypertension through a population-based survey. The studied subjects were recruited as a random sample from a large city population using the probability-based selection method, allowing estimation of hypertension prevalence in the city population with the least bias. In addition, eligibility rate of 93% for ABPM suggests that ABPM is a feasible method of surveying the population for the prevalence of hypertension.
The estimated prevalence of hypertension by ABPM in our study was 32.7%, which is comparable to that in the Ohasama study (31.8%).11) However, the estimated prevalence of hypertension in our study could have been higher than that in the Ohasama study11) if individuals aged more than 65 years had been included. The greater prevalence of hypertension in our study compared to that in the Ohasama study11) is likely to be due to the difference in the studied area although there may be some other factors. Goyang is a semi-urbanized area and Ohasama is a rural area. The prevalence of hypertension in urban populations has been reported to be higher than that in the rural population in China.18)
Our study showed the usefulness of ABPM in the population survey by establishing the diagnosis of masked and white-coat hypertension. The high prevalence of masked hypertension contributed to the under-estimation of hypertension by CBPM. The prevalence of masked hypertension was comparable to that in the previous study, which was performed in a similar age group (16% vs. 15%, respectively).19) The high prevalence of masked hypertension is problematic for public health. Undiagnosed hypertension at a relatively young age can contribute to the increased development of cardiovascular disease by delaying access to adequate treatment. Furthermore, under-estimation of the prevalence of true hypertension may have a negative influence on the public health policy by decreasing the interest and priority. The prevalence of white-coat hypertension in our study was lower than that reported in the Ohasama study.11) However, it was comparable to that in the study by Trudel et al.19) (1.5% vs. 1.8% respectively). The reported prevalence of white-coat hypertension is 10-53%.20) White-coat hypertension is more prevalent in the elderly.21),22) The low prevalence of white-coat hypertension in our study may be explained by the age range of the study population (20-65 years). In the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO), daytime BP was higher than the conventional BP until the age of 50 years, and in contrast, it was similar in the 50-60 year age group, suggesting a high prevalence of masked hypertension and low prevalence of white-coat hypertension before the age of 60 years.17)
In the present study, the diagnosis of hypertension by ABPM was based on 24-hour BP instead of daytime BP. The sensitivity was 83.7% and the specificity was 97.5% when the diagnosis of hypertension was based on the daytime BP and 24-hour BP was used as a reference method (data not shown in the results). The sensitivity and specificity was increased to 100% and 97.6%, respectively when the diagnosis of hypertension was based on the combination of 24-hour BP and daytime average BP (data not shown in the results). The 24-hour BP and nighttime average BP is stronger than daytime BP in the prediction of cardiovascular mortality.23) Moreover, daytime BP does not reflect nighttime hypertension, leading to under-diagnosis of hypertension. The prevalence of masked hypertension in the study population was higher when the diagnosis of hypertension was determined by average nighttime BP than by daytime BP. Unlike the existing hypothesis which suggests that an elevation of blood pressure related to physical activity can explain the high prevalence of masked hypertension in individuals aged <60 years,17) nighttime hypertension, not daytime hypertension was considered as a major contributing factor to the high prevalence of masked hypertension in our study. Thus, we used the 24-hour BP as a reference method instead of daytime BP. Nonetheless, the adoption of ABPM in the national health survey and system may improve public health. Moreover, the promotion of ABPM utilization in clinical practice, together with informed public health policy may help eventually lower health-care costs.24),25)
One issue that should be discussed is the method of CBPM. The English and Canadian surveys have also used automatic oscillometric devices in CBPM, but not the US survey.5) Likewise, the present study used an automatic oscillometric device in CBPM. Blood pressure obtained by the oscillometric method may be lower than that obtained by the auscultatory method, yielding lower prevalence of hypertension.26) Although the prevalence of hypertension as measured by the automated oscillometric device may be different from that measured by the auscultatory method, the hypertension prevalence in Goyang obtained by CBPM was compared to that in Seoul using the KNHNES data obtained in 2011, because the prevalence of hypertension in Goyang city was not available in KNHNES. Goyang is located close to Seoul, sharing similarities in the social and economic landscape. KNHNES used the auscultatory method with a mercury sphygmomanometer in CBPM. Even though we considered a 4% lower detection of hypertension by the oscillometric method compared to that by the auscultatory method in a recent study in Korea,26) a 4% difference was within the 95% confidence interval. Thus, the prevalence of hypertension in the two cities seemed to be similar. The use of automated oscillometric device is increasing in various studies including the general population survey because of the biohazard of mercury and inaccuracy of aneroid sphygmomanometer. Although it was not planned to estimate the prevalence of hypertension by the automated oscillometric device in this study, we have provided important data for the future research and survey.
There are several limitations that should be mentioned. In our study, individuals older than 65 years were not included. Thus, the prevalence of masked and white-coat hypertension in individuals of that age could not be determined. In addition, the feasibility and usefulness of the ABPM in the population survey could not be determined. However, considering the age range in the Ohasama study11) (20-79 years), ABPM may be feasible in the elderly. The sample size was comparatively small. However, we used a random sample that was selected by using the LARDD method and statistical post-stratification weighting to correct for imperfections in the sample that may lead to bias due to the selection of respondents with unequal probabilities, non-coverage of the target population, and non-response.
The other limitation that should be mentioned is that none of the individuals with masked hypertension were in the 20 to 29 years age group. The reason for this may be the low participation rate among individuals in this age range. The estimated prevalence of masked hypertension may be higher than 16.22%, considering more than 10% prevalence of masked hypertension in this age group in IDACO.17)
In conclusion, the estimated prevalence of hypertension by 24-hour ABPM was higher than that by CBPM, revealing high prevalence of masked hypertension. The high prevalence of masked hypertension supports the adoption of ABPM in the national population survey and clinical practice to improve public health and reduce health care costs.
Acknowledgments
This research was supported by a grant (11162KFDA162) from the Korea Food and Drug Administration in 2011.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Lawes CM, Vander Hoorn S, Rodgers A International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Turnbull F Blood Pressure Lowering Treatment Trialists' C. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 4.Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014;174:64–72. doi: 10.1016/j.ijcard.2014.03.163. [DOI] [PubMed] [Google Scholar]
- 5.Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3:e003423. doi: 10.1136/bmjopen-2013-003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–161. doi: 10.1161/01.HYP.0000170138.56903.7a. [DOI] [PubMed] [Google Scholar]
- 7.Conen D, Bamberg F. Noninvasive 24-h ambulatory blood pressure and cardiovascular disease: a systematic review and meta-analysis. J Hypertens. 2008;26:1290–1299. doi: 10.1097/HJH.0b013e3282f97854. [DOI] [PubMed] [Google Scholar]
- 8.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Lovibond K, Jowett S, Barton P, et al. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet. 2011;378:1219–1230. doi: 10.1016/S0140-6736(11)61184-7. [DOI] [PubMed] [Google Scholar]
- 10.Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941–948. doi: 10.1038/ajh.2010.112. [DOI] [PubMed] [Google Scholar]
- 11.Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of "masked" hypertension and "white-coat" hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–515. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Wang JG, Gao P, et al. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit. 2005;10:125–134. doi: 10.1097/00126097-200506000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Kim SW, Lee SK, Hong SJ, Park SH. List-assisted RDD sampling in Korea: testing the feasibility of national survey under within-household selection. Int J Pub Opin Res. 2012;24:79–92. [Google Scholar]
- 14.Rhee MY, Shin SJ, Park SH, Kim SW. Sodium intake of a city population in Korea estimated by 24-h urine collection method. Eur J Clin Nutr. 2013;67:875–880. doi: 10.1038/ejcn.2013.87. [DOI] [PubMed] [Google Scholar]
- 15.Wei W, Tölle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–228. doi: 10.1097/MBP.0b013e328338892f. [DOI] [PubMed] [Google Scholar]
- 16.Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2007;25:1105–1187. doi: 10.1097/HJH.0b013e3281fc975a. [DOI] [PubMed] [Google Scholar]
- 17.Conen D, Aeschbacher S, Thijs L, et al. Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension. 2014;64:1073–1079. doi: 10.1161/HYPERTENSIONAHA.114.03957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang L, Song J, Ma Z, Zhang L, Jing C, Chen D. Prevalence and characteristics of hypertension in mainland Chinese adults over decades: a systematic review. J Hum Hypertens. 2014;28:649–656. doi: 10.1038/jhh.2014.5. [DOI] [PubMed] [Google Scholar]
- 19.Trudel X, Brisson C, Larocque B, Milot A. Masked hypertension: different blood pressure measurement methodology and risk factors in a working population. J Hypertens. 2009;27:1560–1567. doi: 10.1097/HJH.0b013e32832cb036. [DOI] [PubMed] [Google Scholar]
- 20.Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res. 2015;38:1–7. doi: 10.1038/hr.2014.149. [DOI] [PubMed] [Google Scholar]
- 21.Dolan E, Stanton A, Atkins N, et al. Determinants of white-coat hypertension. Blood Press Monit. 2004;9:307–309. doi: 10.1097/00126097-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Franklin SS, Thijs L, Hansen TW, O'Brien E, Staessen JA. White-coat hypertension: new insights from recent studies. Hypertension. 2013;62:982–987. doi: 10.1161/HYPERTENSIONAHA.113.01275. [DOI] [PubMed] [Google Scholar]
- 23.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–1783. doi: 10.1161/01.CIR.0000160923.04524.5B. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Health and Clinical Excellence. Hypertension in adults: diagnosis and management [Internet] London, UK: National Institute for Health and Clinical Excellence; 2011. Aug, [cited 2011 August]. Available from: http://www.nice.org.uk/guidance/CG127. [Google Scholar]
- 25.Krakoff LR. Cost-effectiveness of ambulatory blood pressure: a reanalysis. Hypertension. 2006;47:29–34. doi: 10.1161/01.HYP.0000197195.84725.66. [DOI] [PubMed] [Google Scholar]
- 26.Lim YH, Choi SY, Oh KW, et al. Comparison between an automated device and a manual mercury sphygmomanometer in an epidemiological survey of hypertension prevalence. Am J Hypertens. 2014;27:537–545. doi: 10.1093/ajh/hpt100. [DOI] [PubMed] [Google Scholar]