Abstract
The present survey investigated the association between resilience, burnout and psychological distress among Chinese female nurses. A total of 366 female nurses were enrolled in our study. A series of self-reported questionnaires that dispose of the following constructs: psychological distress, burnout, and resilience were estimated. The hierarchical linear regression models were used to evaluate the mediating effect of resilience on the relationship between burnout and psychological distress. Results of the survey showed 85.5% nurses experienced psychological distress. Resilience was negatively related to psychological distress and burnout whereas burnout was positively associated with psychological distress. Mediation analysis revealed that resilience could partially mediate the relationship between the dimensions of emotional exhaustion, depersonalization, and psychological distress. This study highlights the mediator of resilience between burnout and psychological distress of female nurses. As such, interventions that attend to resilience training may be the focus for future clinical and research endeavors.
Keywords: Psychological distress, Resilience, Burnout, Female nurse
Introduction
There are sizeable studies concerning nursing occupational “burnout” in the current health-care context. Nurses are exposed to numerous stressful situations, for example, witnessing pain and death, misguided expectations, experiencing inadequate physical situations, complex interpersonal relationship, deficient knowledge and decisive autonomy1, 2, 3). Therefore, nurses are subject to occupational burnout. Burnout results from continuous job pressures that individuals cannot effectively manage or deal with and is composed of emotional exhaustion, depersonalization, and low personal accomplishment. In China, burnout risk may be even higher because comparatively low wages are combined with a shortage of nurses and a rapid growth of the aging population. Recent research focusing on the association between burnout and depression found that they were separate entities and showed a moderate association between them4, 5). Kirsi Ahola et al. found that 23% burnout sufferers among dentists who did not experience depressive symptoms at baseline reported depressive symptoms at the three-year follow-up6).
Psychological distress is a multi-factorial construct, which related to poor psychological function and quality of life7); it is also a predictor of higher rates of psychiatric morbidity and suicide8). There is also large variability in individual outcomes related to psychological distress because of transactional processes involving psychological risk and protective factors. Empirical evidence demonstrates that, burnout can result in psychological distress, which undoubtedly affects professional performance and quality of life as well as patient care9, 10). Therefore, more attention should be paid to the psychological distress and promote better mental health for nurses.
Despite the high risk of burnout, not every nurse develops severe distress or psychopathology. An explanation for this positive adaptation after facing adversity is the concept of resilience, regarded as a reintegration processing and a return to well function via the support of protective factors after exposing to a severe stressor11). In summary, resilience has been defined based on an individual’s capacity, the process he or she goes through, and the result12). The emerging field of positive psychology has made resilience (as a protective factor) a separate field of research. Studies of resilience among medical workers have also been widely reported and more research has certified resilience as a process that may alter depended on cultural, developmental and historical context of individuals across life13, 14, 15). Resilience was negatively associated with anxiety or depression, while positively associated with psychological well-being16). For example, a survey among Australian general practice registrars found that high resiliency individual would enjoy a high level of satisfaction and endurance for uncertainty which experienced in daily job. Meanwhile, high resiliency was positively related to low burnout17). Therefore, resilience can be considered as a key component in reducing the risk of psychological distress.
To the best of our knowledge, while the effects of burnout and resilience on psychological distress have been examined18, 19), the underlying psychological mechanisms are not well understood. To examine these mechanisms it is necessary to show how the two constructs (burnout and resilience) co-vary and ameliorate or intensify psychological problems. Existing evidence shows that burnout not only influences psychological distress directly but also has an indirect impact via several mediating variables such as psychological empowerment20) and psychological capital21). Taken together, current research suggests that there may be other potential mediators or underlying mechanism between burnout and psychological distress. Therefore, we hypothesized that resilience could mediate the association between burnout and psychological distress.
Although some studies have reported the mental health of medical workers, information about the Chinese female nurses were little. In order to gain a full understanding of them, we conducted this cross-sectional survey. We recorded the prevalence of psychological distress among Chinese female nurses and investigated whether resilience could mediate the relationship between burnout and psychological distress.
Methods
Ethical considerations
Before conducted this survey, the Ethics Committees Of Nursing School Of Shandong University approved the study design and written informed consent was acquired from each participant. During the whole study process, the privacy and anonymity of participants should be fully protected.
Participants
A cross-sectional study was carried out in two public hospitals in Shandong Province, China. A total of 391 female nurses were voluntary and anonymous to participate in the survey. The whole participants have obtained the National Qualified Certificate of Practice Nursing and were engaged in direct care department, such as medical or surgical wards, intensive care units, operating room, and in adult or pediatric wards. Considering the purpose of study, 10 male nurses were excluded and 15 female nurses were eliminated due to incomplete response questionnaires. The response rate was 93.6% and the final study sample consisted of 366 female nurses.
Measurement of psychological distress
The original Kessler-10 rating scale (K10) includes 10 items established by Kessler and Mroczek22) and widely used to assess individual’s psychological distress. The 10 items was rated on a 5-point Likert from 1 (hardly) to 5 (very much). The total score greater than 16 indicates psychological distress23). This scale was reliable and specific for screening serious mental illness. The cronbach’s α in this study was 0.92.
The maslach burnout inventory
The Maslach Burnout Inventory-General Scale was used to assess the individual burnout, which measures three dimensions: emotional exhaustion, depersonalization, and low personal accomplishment24). The Chinese version comprises 15 items, with five measuring emotional exhaustion, four measuring depersonalization, and six measuring personal accomplishment25). Participants were required to rate every item on 7-point Likert ranging from 0 (never) to 6 (every day)26). A combination of higher emotional exhaustion and depersonalization and lower personal accomplishment scores indicated a greater burnout. The cronbach’s α was 0.84, 0.867, 0.870 and 0.869 for the overall BMI-GS scale and the subscales in our research.
Measurement of resilience
The self-administered 10-item Connor-Davidson Resilience Scale (CD-RISC) was used to evaluate resilience27). The CD-RISC consisted of 10 items and each item was evaluated on a 5 point Likert type from 0(never) to 4(almost always). The total possible score is 40 with higher scores indicating higher levels of resilience. The CD-RISC-10 has a higher reliability and validation for Chinese version28). The cronbach’s α was 0.91 in present survey.
Participants socio-demographic characteristics
We also collected data concerning age, duration of employment, education level, and job type (Permanent nurse and Temporary nurse). The duration of employment was categorized as: <3 years, 3–5 years, 5–10 years, or >10 years.
Statistical analysis
Statistical analysis was performed using the SPSS19.0 statistical software. The descriptive analysis and frequency analysis were used to depict the sample characteristic. The independent-sample t tests and one-way analysis of variance (ANOVA) was used to evaluate the significances when appropriate between the outcome variables and the duration of employment, education, and job-type groups. In order to investigate the association among variables. Pearson’s correlation was performed among study variables. In order to examine the contribution of related factors of psychological distress and explore the potential mediating effect of resilience between burnout and psychological distress, multiple hierarchical regression analysis was applied. In the regression analysis, burnout dimensions and psychological distress were defined as the independent and dependent variable, while resilience defined as the mediator, and duration of employment as the control variable. The Baron and Kenny’s theory to used to establish mediation of resilience between burnout and psychological distress29, 30). The following four step regression approach was applied: (1) burnout is significantly related to psychological distress; (2) burnout is significantly related to resilience; (3) resilience is significantly related to psychological distress; and (4) the coefficients of burnout dimensions for psychological distress is reduced or made non-significant by adding resilience to the model. In order to eliminate the multicollinearity problem, the tolerance and variance test were performed before conducting the regression analysis, whereas the p<0.05 (two-tailed) was considered significant in statistical analysis.
Results
Demographic characteristics of the participants and prevalence of psychological distress
A summary of the descriptive statistics was demonstrated in Table 1. The sample consisted of 163 formal and 203 contract nurses. The average age of participants was 29.1 years (SD=6.8). For education, 58.2% of respondents had finished junior school (or lower schooling) and fewer than half had a bachelor degree or graduate degree. For duration of employment, 52.2% had been nurses for fewer than three years and 23.5% had been nurses for more than 10 years. Descriptive results for resilience, burnout, and psychological distress variables were depicted in Table 2. The overall score for burnout was 41.84 (SD=12.70). Among the three subscales, the highest score (23.5) was found for low personal accomplishment, the lowest score (6.60) was found for depersonalization. Mean scores for resilience and psychological distress were 26.03 and 22.53, respectively, indicating moderate levels of resilience and psychological distress.
Table 1. Socio-demographic characteristic data.
| Characteristic | Category | N | Percentage (%) |
|---|---|---|---|
| Age | 18–24 years | 98 | 26.8 |
| 25–30 years | 160 | 43.7 | |
| 31–35 years | 108 | 29.5 | |
| Education | Junior school or lower | 213 | 58.2 |
| level | Bachelor degree or higher | 153 | 41.8 |
| Duration of employment | <3 years | 191 | 52.2 |
| 3–5 years | 49 | 13.4 | |
| 5–10 years | 40 | 10.9 | |
| >10 years | 86 | 23.5 | |
| Job type | Permanent nurse | 163 | 44.5 |
| Temporary nurse | 203 | 55.5 |
Table 2. Mean and relationship between resilience, burnout and psychological distress.
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | ||
|---|---|---|---|---|---|---|---|
| 1Psychological distress | 22.53 (6.37) | 1 | |||||
| 2Resilience | 26.03 (6.49) | −0.388** | 1 | ||||
| Job burnout | 41.84 (12.70) | ||||||
| 3Emotional exhaustion | 11.76 (6.53) | 0.516** | −0.222** | 1 | |||
| 4Depersonalization | 6.60 (5.03) | 0.504** | −0.250** | 0.726** | 1 | ||
| 5Personal accomplishment | 23.48 (7.85) | 0.127* | −0.448** | 0.048 | 0.121* | 1 | |
*p<0.05 **p<0.01
Significant differences were found between burnout and age and duration of employment (p<0.001), type of job (p<0.05), except education (p>0.05). Overall, 85.5% of respondents had scores greater than 16 on the measure of psychological distress. However, the psychological distress scores differed significantly depending on job type, education, and duration of employment. The scores did not differ according to age.
Correlations among psychological distress, burnout and resilience
Pearson’s Correlations coefficients among the study variables were presented in Table 2. Emotional exhaustion, depersonalization, and low personal accomplishment of burnout dimensions and psychological distress were negatively associated with resilience. Psychological distress was positively associated with burnout dimensions. The inter-correlations among burnout dimensions were positively related. However, emotional exhaustion was not related to personal accomplishment.
Results of linear regression analysis showing associations between the study variables
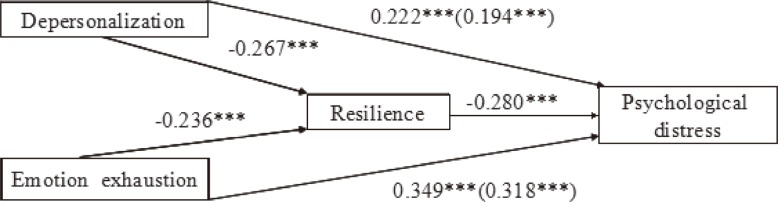
Table 3 presented the result of the multiple regression analysis for psychological distress. In Blocks 1–3, all independent variables including demographic characteristics, burnout, and resilience made a significant contribution to the variance in psychological distress. After adjusting for demographic characteristics in Block 1, Results of regression analysis revealed that the relationship between emotional exhaustion (β=0.349, p<0.001), depersonalization (β=0.222, p<0.001) and psychological distress were positive and significant, with explaining a 28.7% variation of psychological distress. When resilience was added in Block 3, resilience was negatively and significantly associated with psychological distress (β=−0.280, p<0.001), sharing an extra 5.8% variance of psychological distress. Together, burnout, resilience, and demographic characteristics explained 37.4% variance of psychological distress.
Table 3. Resilience as a mediator of the relationship between burnout and psychological distress.
| Variable | psychological distress | |||
|---|---|---|---|---|
| Step 1 (β) | Step 2 (β) | Step 3 (β) | ||
| Block 1 | ||||
| Age | −0.080 | −0.092 | −0.098 | |
| Education level | −0.041 | −0.039 | −0.032 | |
| Job type | 0.070 | 0.033 | 0.025 | |
| Duration of employment | 0.277** | 0.153 | 0.129 | |
| Block 2 | ||||
| Emotional exhaustion | 0.349*** | 0.318*** | ||
| Depersonalization | 0.222*** | 0.194*** | ||
| Personal accomplishment | 0.084 | −0.040 | ||
| Block 3 | ||||
| Resilience | −0.280*** | |||
| R2 | 0.029 | 0.316 | 0.374 | |
| △R2 | 0.029 | 0.287 | 0.058 | |
**p<0.01 ***p<0.001
Resilience mediates the association between burnout and psychological distress
After adding resilience in the regression model, the β coefficients of emotional exhaustion and depersonalization were reduced (from 0.222 to 0.194, p<0.001; from 0.349 to 0.318, p<0.001), respectively, as shown in the final regression. Based on Baron and Kenny’s four step approach of mediation, we speculated that resilience could be a partial mediator between emotional exhaustion, depersonalization, and psychological distress. Sobel tests showed that there was a significant indirect effect between emotional exhaustion (Z=3.52, p<0.001), depersonalization (Z=3.82, p<0.001) and psychological distress, supporting the assertion that resilience is a partial mediator (Fig. 1).
Fig. 1.
Mediation model of resilience in the relationship between burnout and psychological distress
***p<0.001
Discussion
This study is one of the first to our knowledge that examines the potential mediator of resilience between burnout and psychological distress among Chinese female nurses. The 366 nurses reported high levels psychological distress, with 85.5% of sample scores being 16 or greater in this survey. Resilience was negatively related to psychological distress and burnout dimensions, whereas burnout dimensions were positively related to psychological distress. After controlling for socio-demographic characteristics, emotional exhaustion and depersonalization could positively predict psychological distress, while higher resilience was a negative predictor of psychological distress. Mediation analysis showed that resilience could partially mediate the relationship between emotional exhaustion, depersonalization and psychological distress. The current study expands upon the findings of the prior surveys4, 6) and explains why not everyone that suffers from the burnout syndrome develops psychological distress. Interestingly, it is important to note that this normative sample comes from various departments of the general hospital more than just psychiatric or intensive care units compared with previous surveys31, 32).
Nursing burnout has attracted increasing attention for two reasons: impact on individual health and potential impact on quality of patient care. Burnout and psychological distress were important and neglected health indicators among healthcare personnel33). Nursing burnout can occur during medical training (or even before) and the prevalence of burnout gradually increases during the first year when they began a medical profession as healthcare personnel34). Prior researches have found that nurses with higher burnout scores were at highly risking for developing psychological distress symptoms, for example, anxiety or depression35). Factors contributing to psychological distress of clinical nurses probably contain the rapid development of economy and aging population, a growing burden of chronic diseases, lacking of health resources, the medical reform and unreasonable expectations of administrators and patients36, 37). Further, all challenges nurses confronted are not just those mentioned above. Ding et al. thought burnout and psychological distress are likely emerging when the compensation or salaries these workers receive runs behind their demand or expenses38). We examined the links between burnout and psychological distress in present survey. Final results found that burnout dimensions were all positively associated with psychological distress, but hierarchical linear regression showed that psychological distress was only associated with two dimensions of burnout including emotional exhaustion, depersonalization. These results were congruent with previous research among Chinese primary health-care workers, reported that those who report emotional exhaustion and depersonalization experience more anxiety symptoms and thus greater psychological distress.
Consistent with previous research showing that resilience is a protective factor in depression39, 40), result of this survey certified that resilience was also the most important predictor of psychological distress (without considering burnout dimensions). By itself, resilience explained 14.8% of the variance in psychological distress. We also found that resilience was negatively related to psychological distress and we speculated that it could be an important factor for preventing psychological distress. Davydov et al. confirmed the protective and positive effect of resilience in the successful coping or adaptive growth to stress41). Inversely, lower resilience are associated with psychological disorders. Therefore, it is necessary to acknowledge that a training programme for resilience is important for clinical nurses.
Our study suggests that more strategies should be developed to promote better mental health among nurses; these strategies should include enhancement of resilience. We explored the mechanism between burnout and psychological distress with the ultimate goal of seeking an effective intervention for alleviating psychological distress. As expected, resilience could mediate the relationship between burnout and psychological distress. This survey is the first to find that resilience could mediate the relationship between burnout and psychological distress among nurses in China. That is to say, apart from the directly influence on psychological distress, resilience could also affect psychological distress as a mediator between burnout and psychological distress. Previous studies have found that resilience can emerge as the ability to take full advantage of personal positive resources despite stressful occupational circumstance42). Therefore, burnout may alter resilience and thus influence the level of psychological distress. It is possible to modify responses of individuals who have higher burnout through resilience training programs in the workplace. This may improve the health status of nurses. For example, Tomas Gomez-Gascon et al. found that organizational measures such as assistance in improving coping strategies or a 4-month transcendental meditation program play an important role in preventing burnout43, 44). In addition, Sood et al. reported a Stress Management and Resiliency Training Program significantly reduced levels of anxiety and stress while improving quality of life and mindfulness among radiology faculty45). We propose that administrators in different levels of human resources and healthcare organizations should pay attention to the development of such training programs.
There were several limitations to the present study. Due to the cross-sectional survey, a causal relationship between resilience, burnout, and psychological distress cannot be established. Future empirical longitudinal studies will be required to establish causality. Further, all data were collected by self-report questionnaires; thus, report bias cannot be avoided. In addition, all participants in our research were female. As society develops, the number of male nurses is growing rapidly and in future studies data from male nurses should be incorporated.
Conclusions and implications for nursing management
Chinese female nurses experienced a high prevalence of psychological distress. After adjusting for socio-demographic characteristics, psychological distress was positively associated with burnout dimensions and negatively associated with resilience. Additionally, resilience could partially mediate the relationship between psychological distress and dimensions of burnout. The combination of the training programs for resilience with organizational measures for alleviating burnout may be helpful for preventing psychological distress among Chinese female nurses.
Acknowledgments
The study was supported by grants from the Shandong Province Natural Science Foundation (ZR2015HM064) and the Innovation Foundation for Young Talent Team of Shandong University (IFYT15010).
References
- 1.Pappas NA, Alamanos Y, Dimoliatis IDK (2005) Self-rated health, work characteristics and health related behaviours among nurses in Greece: a cross sectional study. BMC Nurs 4, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garrosa E, Rainho C, Moreno-Jiménez B, Monteiro MJ (2010) The relationship between job stressors, hardy personality, coping resources and burnout in a sample of nurses: a correlational study at two time points. Int J Nurs Stud 47, 205–15. [DOI] [PubMed] [Google Scholar]
- 3.Bakker AB, Demerouti E, Schaufeli WB (2005) The crossover of Burnout and work engagement among working couples. Hum Relat 58, 661–89. [Google Scholar]
- 4.Iacovides A, Fountoulakis KN, Kaprinis S, Kaprinis G (2003) The relationship between job stress, burnout and clinical depression [J] J Affect Disord 75, 209–21. [DOI] [PubMed] [Google Scholar]
- 5.Bakir B, Oze rM, Ozcan C T, Cetin M, Fedai T (2010) The association between burnout, and depressive symptoms in a Turkish military nurse sample. Bulletin of Clinical Psychopharmacology 20, 160–3. [Google Scholar]
- 6.Ahola K, Hakanen J (2007) Job strain, burnout, and depressive symptoms: a prospective study among dentists [J] J Affect Disord 104, 103–10. [DOI] [PubMed] [Google Scholar]
- 7.Shih M, Simon PA (2008) Health-related quality of life among adults with serious psychological distress and chronic medical conditions. Qual Life Res 17, 521–8. [DOI] [PubMed] [Google Scholar]
- 8.Egede LE, Dismuke CE (2012) Serious psychological distress and diabetes: a review of the literature. Curr Psychiatry Rep 14, 15–22. [DOI] [PubMed] [Google Scholar]
- 9.Romani M, Ashkar K (2014) Burnout among physicians. Feb 17;9:23556. doi:10.3402/ljm.v9.23556. eCollection 2014. [DOI] [PMC free article] [PubMed]
- 10.Bargellini A, Barbieri A, Rovesti S, Vivoli R, Roncaglia R, Borella P (2000) Relation between immune variables and burnout in a sample of physicians. Occup Environ Med 57, 453–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richardson GE. (2002) The metatheory of resilience and resiliency. J Clin Psychol 58, 307–21. [DOI] [PubMed] [Google Scholar]
- 12.Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R (2014) Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol 5, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cicchetti D. (2010) Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry 9, 145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Masten AS. (2001) Ordinary magic. Resilience processes in development. Am Psychol 56, 227–38. [DOI] [PubMed] [Google Scholar]
- 15.Egeland B, Carlson E, Sroufe LA (1993) Resilience as process. Dev Psychopathol 5, 517–28. [Google Scholar]
- 16.Benetti C, Kambouropoulos N (2006) Affect-regulated indirect effects of trait anxiety and trait resilience on self-esteem. Pers Individ Dif 41, 341–52. [Google Scholar]
- 17.Jackson D, Firtko A, Edenborough M (2007) Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. J ournal of Advance Nursing, 60 (1):1–9. [DOI] [PubMed]
- 18.Quinn-Lee L, Olson-McBride L, Unterberger A (2014) Burnout and death anxiety in hospice social workers [J] J Soc Work End Life Palliat Care 10, 219–39. [DOI] [PubMed] [Google Scholar]
- 19.Xiao Y, Wang J, Chen S, Wu Z, Cai J, Weng Z, Li C, Zhang X (2014) Psychological distress, burnout level and job satisfaction in emergency medicine: A cross-sectional study of physicians in China. Emerg Med Australas 26, 538–42. [DOI] [PubMed] [Google Scholar]
- 20.Muldoon J, Matthews RA, Foley C (2012) Mediated effects of physical risk factors, leader-member exchange and empowerment in predicting perceived injury risk. Stress Health 28, 149–62. [DOI] [PubMed] [Google Scholar]
- 21.Roche M, Haar JM, Luthans F (2014) The role of mindfulness and psychological capital on the well-being of leaders. J Occup Health Psychol 19, 476–89. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60, 184–9. [DOI] [PubMed] [Google Scholar]
- 23.Andrews G, Slade T (2001) Interpreting scores on the Kessler Psychological Distress Scale (K10) [J] Aust N Z J Public Health 25, 494–7. [DOI] [PubMed] [Google Scholar]
- 24.Maslach C, Jackson SE (1981) The measurement of experiences burnout. J Occup Behav 2, 99–103. [Google Scholar]
- 25.Li CP, Shi K (2003) The influence of distributive justice and procedural justice on job burnout [J] Acta Psychol Sin 35, 677–84. [Google Scholar]
- 26.Wang Y, Liu L, Wang J, Wang L (2012) Work-family conflict and burnout among Chinese doctors: the mediating role of psychological capital [J] J Occup Health 54, 232–40. [DOI] [PubMed] [Google Scholar]
- 27.Campbell-Sills L, Stein MB (2007) Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress 20, 1019–28. [DOI] [PubMed] [Google Scholar]
- 28.Wang L, Shi Z, Zhang Y, Zhang Z (2010) Psychometric properties of the 10-item Connor-Davidson Resilience Scale in Chinese earthquake victims [J] Psychiatry Clin Neurosci 64, 499–504. [DOI] [PubMed] [Google Scholar]
- 29.Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51, 1173–82. [DOI] [PubMed] [Google Scholar]
- 30.Sobel ME. (1982) Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol 13, 290–312. [Google Scholar]
- 31.Gito M, Ihara H, Ogata H (2013) The relationship of resilience, hardiness, depression and burnout among Japanese psychiatric hospital nurses. J Nurs Educ Pract 3, 12. [Google Scholar]
- 32.Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, Moss M (2014) Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care 23, e97–105. [DOI] [PubMed] [Google Scholar]
- 33.Wallace JE, Lemaire JB, Ghali WA (2009) Physician wellness: a missing quality indicator. Lancet 374, 1714–21. [DOI] [PubMed] [Google Scholar]
- 34.Willcock SM, Daly MG, Tennant CC, Allard BJ (2004) Burnout and psychiatric morbidity in new medical graduates. Med J Aust 181, 357–60. [DOI] [PubMed] [Google Scholar]
- 35.Fiabane E, Giorgi I, Sguazzin C, Argentero P (2013) Work engagement and occupational stress in nurses and other healthcare workers: the role of organisational and personal factors. J Clin Nurs 22, 2614–24. [DOI] [PubMed] [Google Scholar]
- 36.Chen Z. (2009) Launch of the health-care reform plan in China. Lancet 373, 1322–4. [DOI] [PubMed] [Google Scholar]
- 37.Xu K, Zhang K, Wang D, Zhou L (2014) Trend in distribution of primary health care professionals in Jiangsu province of eastern China [J] Int J Equity Health 13, 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ding YW, Qu J, Yu XS, Wang S (2014) The Mediating Effects of Burnout on the Relationship between Anxiety Symptoms and Occupational Stress among Community Health-care Workers in China: A Cross-Sectional Study. PLoS One 9, 107–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wooten NR. (2012) Deployment cycle stressors and post-traumatic stress symptoms in Army National Guard women: the mediating effect of resilience. Soc Work Health Care 51, 828–49. [DOI] [PubMed] [Google Scholar]
- 40.Wu MS, Yan X, Zhou C, Chen Y, Li J, Zhu Z, Shen X, Han B (2011) General belief in a just world and resilience: Evidence from a collectivistic culture. Eur J Pers 25, 431–42. [Google Scholar]
- 41.Davydov DM, Stewart R, Ritchie K, Chaudieu I (2010) Resilience and mental health, 30(5), 479–95. doi:10.1016/j.cpr.2010.03.003. Epub 2010 Mar 25. [DOI] [PubMed]
- 42.Zwack J, Schweitzer J (2013) If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med 88, 382–9. [DOI] [PubMed] [Google Scholar]
- 43.Gómez-Gascón T, Martín-Fernández J, Gálvez-Herrer M, Tapias-Merino E, Beamud-Lagos M, Mingote-Adán JC, Grupo EDESPROAP-Madrid (2013) Effectiveness of an intervention for prevention and treatment of burnout in primary health care professionals. BMC Fam Pract 14, 173–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elder C, Nidich S, Moriarty F, Nidich R (2014) Effect of transcendental meditation on employee stress, depression, and burnout: a randomized controlled study [J] Perm J 18, 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sood A, Sharma V, Schroeder DR, Gorman B (2014) Stress Management and Resiliency Training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore (NY) 10, 358–63. [DOI] [PubMed] [Google Scholar]