Abstract
Trauma, especially early life trauma, is a risk factor for the development of both posttraumatic stress disorder and psychosis. The goal of the present study was to determine specific associations between exposure to childhood abuse, PTSD symptoms, and current psychotic disorder. Subjects were recruited from a public, urban hospital (N = 328, >90% African American). Psychotic disorders were measured using the MINI International Neuropsychiatric Interview, PTSD was measured using the Clinician Administered PTSD Scale, child abuse was measured with the Childhood Trauma Questionnaire, and lifetime trauma exposure was measured with the Traumatic Events Inventory. Logistic regression analyses showed that both child abuse and current PTSD were statistically significant predictors of psychotic disorder beyond the effects of lifetime trauma load. When PTSD symptom clusters were examined, avoidance and numbing symptoms showed unique association with psychotic disorder independent of demographic variables and trauma exposure. Using bootstrapping techniques, we found a full indirect effect of PTSD on the association between child abuse and, suggesting a particularly important role of PTSD symptoms in relation to psychotic disorder in the presence of early life trauma. Because this is a cross-sectional study, continued research is needed to determine causality of such models. Identifying co-occurring psychosis and PTSD, particularly in populations with high levels of trauma exposure, is critical and will likely aid in more successful treatment interventions.
Keywords: Posttraumatic stress disorder, Trauma, Child abuse, Psychosis, Psychotic disorder
1. Introduction
Lifetime prevalence of non-affective psychotic disorders in the general population is approximately 1.5% (Kessler, Birnbaum, et al., 2005; Perälä et al., 2007). Research into the etiology of psychotic disorders has shown a complex interaction between genetic and environmental factors (Cannon & Clarke, 2005; Jablensky & Kalaydjieva, 2003). Trauma exposure, which is commonly reported in individuals with psychotic disorders, may be one environmental factor that plays a key role in psychotic etiology (Bendall, Jackson, Hulbert, & McGorry, 2008; Cutajar et al., 2010; Gaudiano & Zimmerman, 2010; Read, Os, Morrison, & Ross, 2005; Schäfer & Fisher, 2011).
Previous research suggests that exposure to childhood abuse in particular may be an important risk factor for the development of psychotic disorder. This is substantiated by two recent critical and meta-analytic reviews demonstrating clear associations between childhood trauma exposure and psychotic disorders (Morgan & Fisher, 2007; Varese et al., 2012). While evidence for this association continues to grow, only a limited number of prospective studies have been conducted (Arseneault et al., 2011; Bendall et al., 2008; Sideli, Mule, La Barbera, & Murray, 2012). However, at least one of these studies has shown that adolescents exposed to childhood abuse showed elevated rates of psychotic symptoms (Arseneault et al., 2011).
Many studies have also shown an association between PTSD and psychotic disorder. Although prevalence rates vary by sample, estimates suggest a significantly higher rate of PTSD in psychotic disorder patients (approximately 30%) versus that in the general population (7.8%) (Buckley, Miller, Lehrer, & Castle, 2009). Although there is growing evidence that PTSD is commonly found among individuals with psychotic disorder (Aakre, Brown, Benson, Drapalski, & Gearon, 2014; David, Kutcher, Jackson, & Mellman, 1999; Hamner, Frueh, Ulmer, & Arana, 1999; Sautter et al., 1999), much of it still goes unrecognized or undiagnosed, and the comorbidity between these disorders is not fully understood.
A number of models have been proposed to highlight the connection between trauma, PTSD, and psychotic disorder. In a model of the interrelation between trauma, PTSD, and severe mental illness (SMI), Mueser, Rosenberg, Goodman, and Trumbetta (2002) suggest that PTSD may mediate the relationship between trauma and symptom severity or impairment from SMI. In this model, PTSD and psychotic disorder are seen as distinct disorders that interact with one another creating compounded risk for increased psychotic and PTSD symptoms. Morrison, Frame, and Larkin (2003) propose a different integrative model of trauma and psychotic disorder. Within this model, PTSD and psychosis are seen as similar entities that are part of a broader spectrum of reactions to trauma. This fits with some initial evidence of a psychotic subtype of PTSD (Sautter et al., 2003; Shevlin, Armour, Murphy, Houston, & Adamson, 2011).
It is unlikely that one model provides all the answers for these associations, considering the complexity of psychotic disorder and the many biological and environmental factors that interact in its development. However, it remains important to better understand how environmental factors, like early life trauma, and trauma-related psychiatric disorders may impact risk for the development of psychotic disorders. To our knowledge there have been no studies that investigated the unique contributions of childhood abuse and PTSD to adult psychotic disorder incidence. Thus, the goal of the present study was to investigate the associations between childhood abuse, PTSD, and psychotic disorder incidence in an urban, minority population. More specifically, we examined child abuse exposure and PTSD as predictors of current psychotic disorder diagnosis.
2. Method
2.1. Procedure
Participants were drawn from a study of risk factors for the development of PTSD in a low socioeconomic, urban minority population. Participants were recruited from waiting rooms in the gynecology and primary care medical clinics at a publically funded hospital and the emergency department waiting room of a pediatric, not-for-profit hospital, in Atlanta, Georgia. We did not narrow recruitment to specific criteria, but approached any individual in the waiting room. To be eligible for participation, subjects had to be at least 18 years old and able to give informed consent. After signing the informed consent approved by the Emory IRB, an interview was administered with questionnaires regarding trauma history and psychological variables. Trained research assistants administered this interview (approximately 45–75 min). Comprehensive assessments of psychological functioning were conducted in a separate associated study including fewer participants drawn from the pool of participants who completed the initial assessment (approximately 2 weeks post-assessment; see (Gillespie et al., 2009) for full details regarding study procedures).
2.2. Participants
The sample consisted of 328 individuals (see Table 1 for descriptive statistics).
Table 1.
Demographic and trauma-related descriptive details for sample.
| Female (%) | 85.4 |
| Age (mean (SD)) | 40.84 (12.04) |
| Race (%) | |
| African American | 96.0 |
| White | 1.8 |
| Hispanic/Latino | 0.3 |
| Mixed/Other | 1.8 |
| Household monthly income (%) | |
| $0–500 | 24.0 |
| $500–999 | 28.1 |
| $1000–1999 | 27.8 |
| $2000 or more | 27.8 |
| Lifetime trauma exposure (mean (SD)) | 21.30 (13.10) |
| Mod-to-severe child abuse, overall (%) | 42.8 |
| Physical abuse | 21.5 |
| Sexual abuse | 31.1 |
| Emotional abuse | 23.4 |
N = 328.
2.3. Measures
2.3.1. Childhood Trauma Questionnaire (CTQ)
The CTQ (Bernstein et al., 2003) is a 25-item, reliable and valid self-report instrument assessing sexual, physical, emotional abuse in childhood. Bernstein and Fink (1998) established scores for none, mild, moderate, and severe for each type of abuse. The data from the CTQ were used to create a categorical variable to account for presence/absence of moderate-to-severe reported exposure to emotional (score ≥ 13), physical (score ≥ 10), and sexual (score ≥ 8) abuse in childhood (0 = none/mild abuse; 1 = moderate/severe abuse scores for at least one type of abuse).
2.3.2. Traumatic Events Inventory (TEI)
The TEI is a 14-item screening instrument for lifetime history of traumatic events. It was administered to detail frequency and type of trauma(s) experienced; consistent with prior research (Gillespie et al., 2009; Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005), total level of trauma exposure was measured by a sum score refiecting the total frequency of different types of trauma (e.g., car accident, sexual assault) a participant had been exposed over the course of their life. For this study, the TEI was used to measure frequency of lifetime trauma exposure (excluding child abuse).
2.3.3. Clinician-Administered PTSD Scale (CAPS)
The CAPS is an interviewer-administered psychometrically validated diagnostic instrument measuring PTSD (Blake et al., 1990, 1995). The CAPS assesses current PTSD and yields a continuous measure of the severity of overall PTSD and of the three symptom clusters (intrusion, avoidance/numbing, and arousal). PTSD diagnosis based on DSM-IV-TR criteria was determined. Total severity scores based on frequency and intensity scores for the three PTSD symptom clusters were also calculated.
2.3.4. The MINI International Neuropsychiatric Interview (MINI)
The MINI (Lecrubier et al., 1997; Sheehan et al., 1997) is a well-validated structured interview developed to assess psychiatric disorders according to DSM-IV-TR diagnostic criteria. This measure was used to assess current and lifetime presence of psychotic disorders, alcohol and substance use disorders, and major depressive disorder. Psychotic disorders assessed included schizophrenia, substance-induced psychosis, psychosis due to GMC, and psychotic disorder NOS.
2.4. Data analysis
The overall analytic approach was to examine the predictive utility of exposure to moderate-to-severe childhood abuse and current PTSD on psychotic disorder. Rates of psychiatric disorders based on the presence/absence of psychotic disorder were examined using Chi-square tests of independence and PTSD symptom severity by analysis of variance. Logistic regressions were utilized to examine the predictive value of childhood abuse and PTSD on psychotic disorder. Additional logistic regressions were run to examine the predictive effect of PTSD symptom clusters on psychotic disorder, beyond exposure to childhood trauma. Finally, mediation analysis was performed with INDIRECT (Preacher & Hayes, 2008) for SPSS, which allows for the examination of the indirect effects of a variable conditional on the effects of other variables in the model. Bootstrapping with 95% confidence intervals (CI) was utilized to determine significance of indirect effects.1 Age, sex, household monthly income, and frequency of lifetime trauma exposure were included as covariates in all analyses. All analyses were conducted with SPSS 22.0 software package.
3. Results
The rates of psychotic disorders were as follows: 5.8% (N = 19) met criteria for current psychotic disorder diagnosis and 8.8% (N = 29) met criteria for lifetime psychotic disorder diagnosis.2 Regarding types of diagnoses, 3.4% (N = 11) met current criteria for schizophrenia and 4.6% (N = 15) met lifetime criteria for schizophrenia; 1.5% (N = 5) met for lifetime substance-induced psychotic disorder; 2.4% (N = 8) met for current psychotic disorder NOS and 2.7% (N = 9) met for lifetime psychotic disorder NOS. There were higher rates of comorbid psychiatric conditions and outcomes for participants with current psychotic disorder than those that did not meet criteria for psychosis (see Table 2). Exposure to moderate-to-severe childhood abuse was also higher for participants with current psychotic disorder (72.7%) compared with participants without a current psychotic disorder (41.7%).
Table 2.
Psychiatric descriptive details for sample.
| Psychotic disorder |
||
|---|---|---|
| 0 | 1 | |
| % Rates of psychiatric disorders and outcomes | ||
| Current PTSD | 22.1 | 66.7*** |
| Lifetime PTSD | 48.8 | 88.9*** |
| Current Major Depression | 20.1 | 63.2*** |
| Lifetime Major Depression | 46.4 | 84.3*** |
| Current Alcohol/Substance Dependence (MINI) | 11.0 | 26.3** |
| Lifetime Alcohol/Substance Dependence (MINI) | 35.3 | 52.6 |
| Suicide attempt (lifetime) | 11.4 | 57.9*** |
| Mean (SD) for PTSD severity scores by cluster | ||
| Re-experiencing Symptom Severity (Cluster B) | 4.79 (7.07) | 10.82 (10.21)** |
| Avoidance/numbing Symptom Severity (Cluster C) | 8.41 (9.93) | 21.61 (15.27)*** |
| Hyperarousal Symptom Severity (Cluster D) | 9.52 (9.24) | 18.50 (12.55)*** |
N = 328
Note: Psychiatric disorders were assessed using the MINI. Differences in rates of psychiatric disorders between individuals with and without psychotic disorder were assessed using Chi-square tests of independence. Differences in PTSD symptom severity scores were assessed using analysis of variance. Significant differences are depicted with asterisks:
p < 0.05,
p < 0.01,
p < 0.001.
As shown in Table 3, logistic regression results showed that exposure to childhood abuse was significantly associated with the presence of psychotic disorder (95% CI = 1.18–10.67, p < 0.05), even when accounting for demographic variables and lifetime trauma load. However, when PTSD was included in the model, the association between childhood abuse and current psychotic disorder was no longer significant (95% CI = 0.55–6.33, p = 0.32), suggesting a potential mediation effect of PTSD on the association between exposure to child abuse and current psychotic disorder. PTSD diagnosis was significantly associated with current psychotic disorder independent of trauma (95% CI = 1.66–15.86, p < 0.01). Demographic variables and lifetime trauma were not significantly associated with current psychotic disorder.
Table 3.
The association between current psychotic disorder, moderate-to-severe childhood abuse, and PTSD using a logistic regression model.
| β | SE | Wald | p | exp(B) | |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | 0.01 | 0.02 | 0.44 | 0.51 | 1.01 |
| Sex | 1.26 | 1.05 | 1.43 | 0.24 | 3.52 |
| Income | 0.04 | 0.19 | 0.04 | 0.84 | 1.04 |
| Lifetime trauma load | 0.01 | 0.02 | 0.03 | 0.86 | 1.00 |
| Step 2 | |||||
| Child abuse | 1.26 | 0.56 | 5.04 | 0.02* | 3.52 |
| Step 3 | |||||
| Child abuse | 0.61 | 0.62 | 0.95 | 0.3 | 1.84 |
| Current PTSD | 1.63 | 0.57 | 7.97 | 0.00** | 5.09 |
N = 328; age, sex, household income level, and lifetime trauma load remained in the model but were not significant at any step.
p < 0.05.
p < 0.01.
When PTSD symptom clusters were entered individually in logistic regression models (see Table 4), all three symptom clusters were significantly associated with current psychotic disorder independent of trauma. As shown with model 2, when the three symptom clusters were included in the logistic model together, only Cluster C remained significantly associated with current psychotic disorder (p < 0.05). In all models, child abuse was no longer significantly associated with current psychotic disorder when PTSD symptoms were added into the model in the final step.
Table 4.
The associations between current psychotic disorder and PTSD symptom clusters using logistic regression models.
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| B | OR (95% CI) | B | OR (95% CI) | |
| Criterion B PTSD Symptoms | 0.07* | 1.01–1.14 | −0.03 | 0.90–1.05 |
| Criterion C PTSD Symptoms | 0.09*** | 1.04–1.14 | 0.09* | 1.02–1.17 |
| Criterion D PTSD Symptoms | 0.08** | 1.03–1.14 | 0.03 | 0.95–1.12 |
N = 328.
Model 1: Final step adjusting for sex, age, household income level, lifetime trauma load, and child abuse with each PTSD symptom cluster entered separately into a model.
Model 2: Final step adjusting for sex, age, household income level, lifetime trauma load, and child abuse with all three symptom clusters included in the model together.
p < 0.05.
p < 0.01.
p < 0.001.
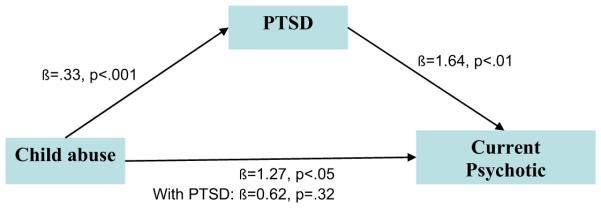
We used bootstrapping techniques to formally test for the indirect effect of PTSD diagnosis on the association between childhood abuse and current psychotic disorder. As expected based on logistic regression findings, there was a significant full indirect effect of PTSD (95% CI = 0.12–1.16, p < 0.01; see Fig. 1).
Fig. 1.
The full indirect effect of current PTSD on the relation between childhood abuse and current psychotic disorder. Sex, age, household income level, and lifetime trauma load were controlled.
4. Discussion
The relationship between trauma and psychotic disorder remains understudied despite growing evidence to suggest that traumatic experiences, particularly in early life, may increase risk for psychotic disorders. Using data obtained from a highly traumatized, primarily African American, urban population, this study provides further evidence of the strong connection between exposure to childhood abuse and the development of psychotic disorders in adulthood. We found that reported exposure to moderate-to-severe child abuse was predictive of current psychotic disorder diagnosis, even after controlling for demographic variables and frequency of exposure to lifetime trauma. More specifically, individuals with significant child abuse exposure were 3.5 times as likely to be diagnosed with a psychotic disorder at the time of assessment than those with no or low levels of exposure to child abuse.
We did not find a significant association between lifetime trauma exposure (excluding child abuse) and psychosis in this sample, suggesting that the strong relationship found between trauma exposure and psychosis does in fact depend on when the trauma occurs and the nature of the trauma, rather than how many discrete times an individual is traumatized. The presence of childhood abuse, especially at a significant level, may be indicative of a particularly toxic home environment where trauma occurs on a continuous basis, rather than via a single discrete traumatic event, and it is in this kind of environment where risk for the development of psychopathology is particularly strong (Herman, 1992; Mullen et al., 1996). This is in part because exposure to trauma and abuse during childhood when development is still underway can have a profound negative impact on normative neurobiological development and the stress response system, thus producing broad neurobiological vulnerabilities that may serve as pathways to later development of negative psychiatric outcomes (Anda et al., 2006; Watts-English, Fortson, Gibler, Hooper, & De Bellis, 2006). One system consistently shown to be altered by child abuse is the hypothalamic-pituitary-adrenal (HPA) axis, a main component of the body’s stress response. Individuals exposed to child abuse show hyperreactivity of the HPA system (Heim et al., 2000). Alterations in the HPA axis thus results in alterations to many neurobiological components such as neurotransmitter functioning in the body (e.g., dopamine), physiological reactivity via the autonomic nervous system, and structural and functional neural changes, all of which may then increase vulnerability to the development of psychosis (Read, Perry, Moskowitz, & Connolly, 2001).
Importantly, current PTSD was also strongly related to current psychosis in this sample. Individuals with current PTSD were five times as likely to be diagnosed with a current psychotic disorder than those without current PTSD, independent of trauma exposure. Our results also demonstrated that current PTSD may have an indirect effect on the association between childhood abuse and psychosis, suggesting that the presence of PTSD in individuals exposed to significant child abuse, and not only the experience of abuse itself, may increase risk for the emergence of psychosis in adulthood. Our finding fits with research that suggests both PTSD and psychosis may be on a spectrum of trauma-related psychopathology (Morrison et al., 2003), and HPA axis dysfunction and the resulting neurobiological changes associated with that dysfunction may be a critical common factor (Heim et al., 2000). Some researchers posit that positive psychotic symptoms, like hallucinations and delusions, may in fact be trauma intrusions or interpretations of intrusions that then cause distress (Morrison, 2001). In fact, there is some evidence that child abuse is particularly related to the presence of positive symptoms, as opposed to negative symptoms (Ross, Anderson, & Clark, 1994). “Psychosis” as a construct is heterogeneous and the presentation of psychotic disorders may therefore differ based on environmental experiences, like child abuse. Thus, our findings provide further evidence that trauma and PTSD may be particularly important factors that contribute to one subtype within the broader category of “psychosis”.
When examining symptom severity based on the DSM-IV-TR clusters of PTSD, we found that all three symptom clusters were related to current psychotic disorder independently. However, avoidance/numbing symptoms showed a particularly strong association with psychotic disorder beyond the effects of the other symptom clusters. It is unclear why this might be the case. One might imagine that re-experiencing symptoms would be more strongly related to the positive symptoms of psychotic disorder, since these PTSD symptoms (e.g., flashbacks, intrusive memories) can often present as psychotic-like hallucinations. These results suggest that other PTSD symptoms are also relevant. There is likely overlap between some of the symptoms of PTSD and negative symptoms of psychotic disorder (e.g., emotional numbing, social withdrawal, and anhedonia in PTSD). This could explain at least part of this association found. More research is needed to better understand how avoidance/numbing symptoms may contribute to or interact with psychotic symptoms. It is important to note that this was cross-sectional data and we did not have information on when the onset of psychotic symptoms occurred in relation to PTSD symptoms. While there is evidence to support this type of model, there is also evidence to show that individuals with psychosis are more likely to be traumatized later on, and can go on to develop PTSD following these traumas or even develop PTSD in relation to the onset of psychosis (Mueser & Rosenberg, 2003; Mueser et al., 2002; Williams-Keeler, Milliken, & Jones, 1994). Therefore, prospective studies are necessary to fully determine how PTSD may fit into the pathway through which psychotic symptoms emerge.
Our results also showed significant comorbidity between current psychotic disorder and other Axis I disorders, including major depression and substance use disorders, as well as suicide attempts. This is consistent with research showing high comorbidity between psychotic disorders and other psychopathology (Kessler, Chiu, Demler, & Walters, 2005; McMillan, Enns, Cox, & Sareen, 2009). However, the rates of psychosis and comorbid psychiatric diagnosis in our samples are substantially higher than national averages (Gillespie et al., 2009; Schwartz et al., 2005). Considering that this is not a treatment-seeking population, these rates are both alarming and concerning and increased awareness about the increased psychiatric risk for low-income individuals living in urban environments is critical.
Several study limitations are worth noting. As highlighted above, given the cross-sectional nature of this study and use of retrospective reports, we cannot make assertions about causality or time of onset for child abuse, PTSD symptoms and psychotic symptoms. We also focused on self-report measures of child abuse. This may have affected the accuracy of our classification of individuals into abuse groups and may have either overestimated or underestimated the amount of child abuse that occurred, as multiple studies have previously shown that self-reports of abuse can both overestimate (e.g., Offer, Kaiz, Howard, & Bennett, 2000) and underestimate abuse that occurred (e.g., Berger, Knutson, Mehm, & Perkins, 1988; Kemper, Carlin, & Buntain-Ricklefs, 1994). However, the measure that was used to assess child abuse (CTQ) uses very specific language to help make classification more accurate (e.g., “People in my family called me things like stupid, lazy or ugly” to assess emotional abuse and “I got hit so hard by someone in my family that I had to see a doctor or go to the hospital” to assess physical abuse). Additionally, although these self-report data may have a biased estimation of abuse exposure, there is still a strong, significant association with psychosis and thus appears to be capturing an important relationship between child abuse exposure and psychosis. Finally, generalizability may be limited based on the convenience sampling strategy used and specificity of the population examined in this study. Since recruitment occurred by approaching individuals in waiting rooms, the sample does not reflect a representative sample of urban Atlanta and results could have been influenced by the type of individuals willing to participate or biases by interviewers in the type of individuals approached. Our sample was also largely low income, majority female, and primarily (>90%) African American. Concerns about the specificity of this sample are balanced by the public health importance of studying psychiatric risk in an under-researched and under-served population with high rates of trauma exposure and post-traumatic psychopathology. The resources for psychiatric care are limited for individuals in this population. Research focusing on psychiatric risk brings attention to the need for increased resources.
Our findings provide further evidence of the detrimental effects of exposure to childhood abuse on psychiatric outcomes in adulthood, including both PTSD and psychotic disorder. The rates of psychotic disorder in this population highlight the association between early life trauma and psychosis and shed light on the high levels of comorbidity between psychotic disorder and other trauma-related psychopathology. These results suggest that PTSD may help to explain the relationship between early life trauma and the development of psychosis, although continued research is still needed. The findings suggest that, like PTSD, psychotic symptoms may represent post-traumatic sequelae, a notion that warrants further examination in longitudinal studies. Regardless, it will be critical moving forward to determine if treating PTSD could also bring relief of psychotic symptoms to these individuals. There is some initial evidence that treating subthreshold psychotic symptoms can reduce the likelihood of symptom progression in individuals at risk for the development of psychotic disorders (McGorry et al., 2002). Other research has also shown that individuals with comorbid PTSD and psychosis can still benefit from evidence-based trauma treatment (de Bont, van Minnen, & de Jongh, 2013; van den Berg et al., 2015). Overall, understanding how co-occurring psychotic disorder and PTSD might affect treatment is important and identifying comorbidity, particularly in populations with high levels of trauma exposure, could aid in more successful treatment interventions.
Acknowledgments
We would like to thank Allen W. Graham, Rebecca Roffman, Angelo Brown, and the entire Grady Trauma Project staff and volunteers for all their assistance in the collection and management of the data used for this study.
Funding
This work was primarily supported by the National Institute of Mental Health (MH071537 for Ressler; MH102890 for Powers) and the National Institute of Child Health and Human Development (HD071982 for Bradley). Support also included Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01 RR00039).
Footnotes
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government.
Bootstrapping is a preferred method for interpreting mediation analyses because it does not assume that sampling distributions of the indirect effects are normally distributed.
If participant did not endorse active current psychotic symptoms, then the participant was diagnosed with lifetime but not current psychotic disorder.
Conflict of interest
There are no conflicts of interest to disclose.
References
- Aakre JM, Brown CH, Benson KM, Drapalski A, Gearon JS. Trauma exposure and PTSD in women with schizophrenia and coexisting substance use disorders: Comparisons to women with severe depression and substance use disorders. Psychiatry Research. 2014 doi: 10.1016/j.psychres.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. American Journal of Psychiatry. 2011;168(1):65–72. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: A systematic, critical review of the evidence. Schizophrenia Bulletin. 2008;34(3):568–579. doi: 10.1093/schbul/sbm121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger AM, Knutson JF, Mehm JG, Perkins KA. The self-report of punitive childhood experiences of young adults and adolescents. Child Abuse & Neglect. 1988;12(2):251–262. doi: 10.1016/0145-2134(88)90033-6. [DOI] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Manual for the childhood trauma questionnaire. The Psychological Corporation; New York: 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer G, Charney D, et al. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. 1990 [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophrenia Bulletin. 2009;35(2):383–402. doi: 10.1093/schbul/sbn135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon M, Clarke MC. Risk for schizophrenia-broadening the concepts, pushing back the boundaries. Schizophrenia Research. 2005;79(1):5–13. doi: 10.1016/j.schres.2005.05.027. [DOI] [PubMed] [Google Scholar]
- Cutajar MC, Mullen PE, Ogloff JR, Thomas SD, Wells DL, Spataro J. Schizophrenia and other psychotic disorders in a cohort of sexually abused children. Archives of General Psychiatry. 2010;67(11):1114–1119. doi: 10.1001/archgenpsychiatry.2010.147. [DOI] [PubMed] [Google Scholar]
- David D, Kutcher GS, Jackson EI, Mellman TA. Psychotic symptoms in combat-related posttraumatic stress disorder. Journal of Clinical Psychiatry. 1999 doi: 10.4088/jcp.v60n0106. [DOI] [PubMed] [Google Scholar]
- de Bont PA, van Minnen A, de Jongh A. Treating PTSD in patients with psychosis: A within-group controlled feasibility study examining the efficacy and safety of evidence-based PE and EMDR protocols. Behavior Therapy. 2013;44(4):717–730. doi: 10.1016/j.beth.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Gaudiano BA, Zimmerman M. Evaluation of evidence for the psychotic subtyping of post-traumatic stress disorder. British Journal of Psychiatry. 2010;197(4):326–327. doi: 10.1192/bjp.bp.110.078824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, et al. Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry. 2009;31:505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner MB, Frueh BC, Ulmer HG, Arana GW. Psychotic features and illness severity in combat veterans with chronic posttraumatic stress disorder. Biological Psychiatry. 1999;45(7):846–852. doi: 10.1016/s0006-3223(98)00301-1. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. Journal of the American Medical Association. 2000;284(5):592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Herman JL. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress. 1992;5(3):377–391. [Google Scholar]
- Jablensky AV, Kalaydjieva LV. Genetic epidemiology of schizophrenia: Phenotypes, risk factors, and reproductive behavior. American Journal of Psychiatry. 2003;160(3):425–429. doi: 10.1176/appi.ajp.160.3.425. [DOI] [PubMed] [Google Scholar]
- Kemper KJ, Carlin AS, Buntain-Ricklefs J. Screening for maternal experiences of physical abuse during childhood. Clinical Pediatrics. 1994;33(6):333–339. doi: 10.1177/000992289403300604. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Demler O, Falloon IR, Gagnon E, Guyer M, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R) Biological Psychiatry. 2005;58(8):668–676. doi: 10.1016/j.biopsych.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. [Google Scholar]
- McGorry PD, Yung AR, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Archives of General Psychiatry. 2002;59(10):921–928. doi: 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]
- McMillan KA, Enns MW, Cox BJ, Sareen J. Comorbidity of Axis I and II mental disorders with schizophrenia and psychotic disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Canadian Journal of Psychiatry. 2009;54(7):477–486. doi: 10.1177/070674370905400709. [DOI] [PubMed] [Google Scholar]
- Morgan C, Fisher H. Environment and schizophrenia: Environmental factors in schizophrenia: Childhood trauma—a critical review. Schizophrenia Bulletin. 2007;33(1):3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison AP. The interpretation of intrusions in psychosis: An integrative cognitive approach to hallucinations and delusions. Behavioural and Cognitive Psychotherapy. 2001;29(3):257–276. [Google Scholar]
- Morrison AP, Frame L, Larkin W. Relationships between trauma and psychosis: A review and integration. British Journal of Clinical Psychology. 2003;42(4):331–353. doi: 10.1348/014466503322528892. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD. Treating the trauma of first episode psychosis: A PTSD perspective. Journal of Mental Health. 2003;12(2):103–108. doi: 10.1080/096382300210000583371. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Goodman LA, Trumbetta SL. Trauma, PTSD, and the course of severe mental illness: An interactive model. Schizophrenia Research. 2002;53(1):123–143. doi: 10.1016/s0920-9964(01)00173-6. [DOI] [PubMed] [Google Scholar]
- Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The long-term impact of the physical, emotional, and sexual abuse of children: A community study. Child abuse & neglect. 1996;20(1):7–21. doi: 10.1016/0145-2134(95)00112-3. [DOI] [PubMed] [Google Scholar]
- Offer D, Kaiz M, Howard KI, Bennett ES. The altering of reported experiences. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(6):735–742. doi: 10.1097/00004583-200006000-00012. [DOI] [PubMed] [Google Scholar]
- Perälä J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsä E, Pirkola S, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Archives of General Psychiatry. 2007;64(1):19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Read J, Os JV, Morrison A, Ross CA. Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica. 2005;112(5):330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- Read J, Perry BD, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: A traumagenic neurodevelopmental model. Psychiatry. 2001;64(4):319–345. doi: 10.1521/psyc.64.4.319.18602. [DOI] [PubMed] [Google Scholar]
- Ross CA, Anderson G, Clark P. Childhood abuse and the positive symptoms of schizophrenia. Psychiatric Services. 1994;45(5):489–491. [PubMed] [Google Scholar]
- Sautter FJ, Bissette G, Wiley J, Manguno-Mire G, Schoenbachler B, Myers L, et al. Corticotropin-releasing factor in posttraumatic stress disorder (PTSD) with secondary psychotic symptoms, nonpsychotic PTSD, and healthy control subjects. Biological Psychiatry. 2003;54(12):1382–1388. doi: 10.1016/s0006-3223(03)00571-7. [DOI] [PubMed] [Google Scholar]
- Sautter FJ, Brailey K, Uddo MM, Hamilton MF, Beard MG, Borges AH. PTSD and comorbid psychotic disorder: Comparison with veterans diagnosed with PTSD or psychotic disorder. Journal of Traumatic Stress. 1999;12(1):73–88. doi: 10.1023/A:1024794232175. [DOI] [PubMed] [Google Scholar]
- Schäfer I, Fisher HL. Childhood trauma and posttraumatic stress disorder in patients with psychosis: Clinical challenges and emerging treatments. Current Opinion in Psychiatry. 2011;24(6):514–518. doi: 10.1097/YCO.0b013e32834b56c8. [DOI] [PubMed] [Google Scholar]
- Schwartz A, Bradley B, Sexton M, Sherry A, Ressler K. Posttraumatic stress disorder among African Americans in an Innery City Mental Health Clinic. Psychiatric Services. 2005;56:212–216. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Sheehan D, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12(5):232–241. [Google Scholar]
- Shevlin M, Armour C, Murphy J, Houston JE, Adamson G. Evidence for a psychotic posttraumatic stress disorder subtype based on the National Comorbidity Survey. Social Psychiatry and Psychiatric Epidemiology. 2011;46(11):1069–1078. doi: 10.1007/s00127-010-0281-4. [DOI] [PubMed] [Google Scholar]
- Sideli L, Mule A, La Barbera D, Murray RM. Do child abuse and maltreatment increase risk of schizophrenia? Psychiatry Investigation. 2012;9(2):87–99. doi: 10.4306/pi.2012.9.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg DP, de Bont PA, van der Vleugel BM, de Roos C, de Jongh A, Van Minnen A, et al. Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder a randomized clinical trial. JAMA Psychiatry. 2015;72:259–267. doi: 10.1001/jamapsychiatry.2014.2637. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin. 2012;38(4):661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts-English T, Fortson BL, Gibler N, Hooper SR, De Bellis MD. The psychobiology of maltreatment in childhood. Journal of Social Issues. 2006;62(4):717–736. [Google Scholar]
- Williams-Keeler L, Milliken H, Jones B. Psychosis as precipitating trauma for PTSD: A treatment strategy. American Journal of Orthopsychiatry. 1994;64(3):493. doi: 10.1037/h0079543. [DOI] [PubMed] [Google Scholar]