Abstract
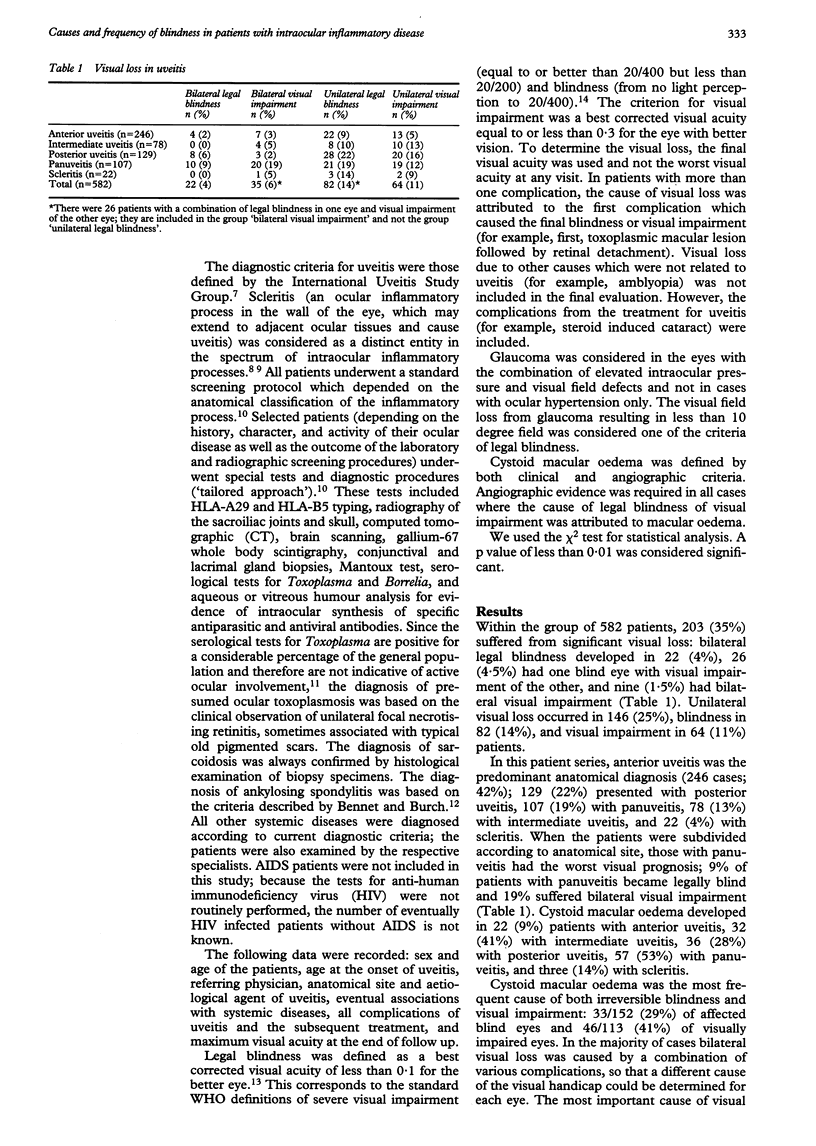
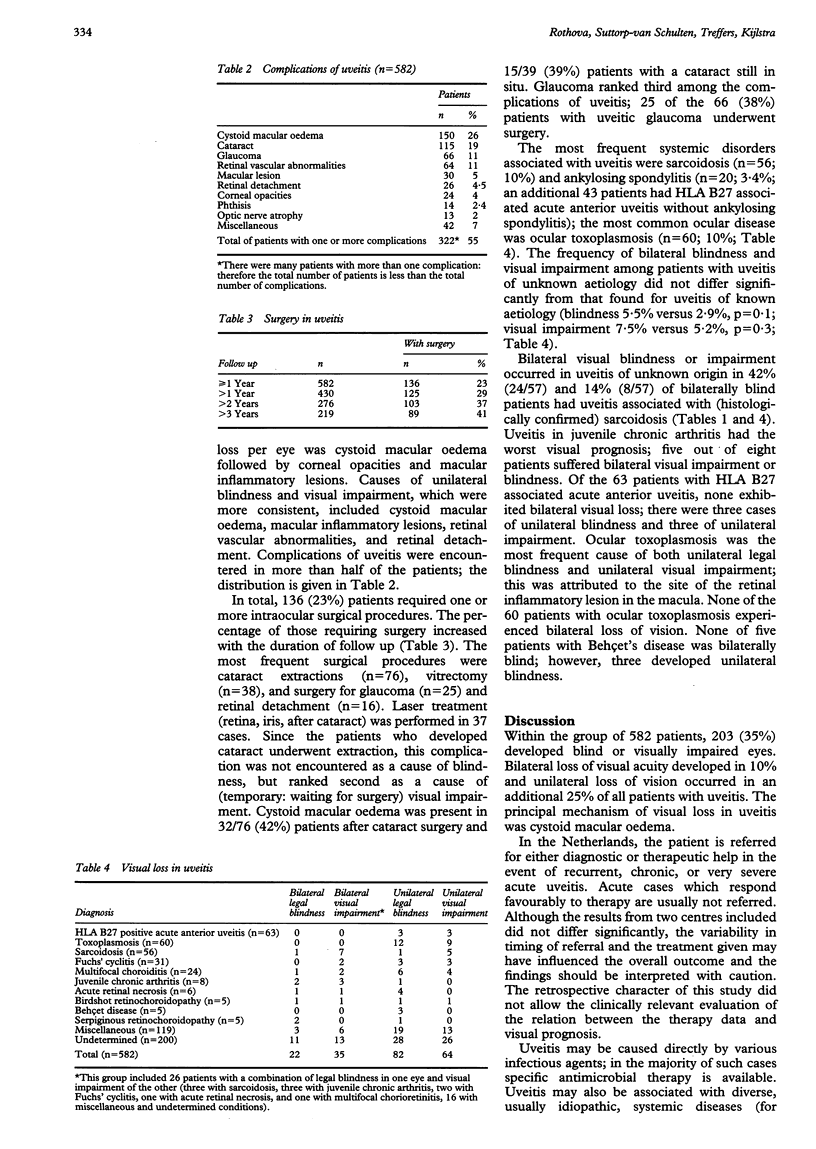
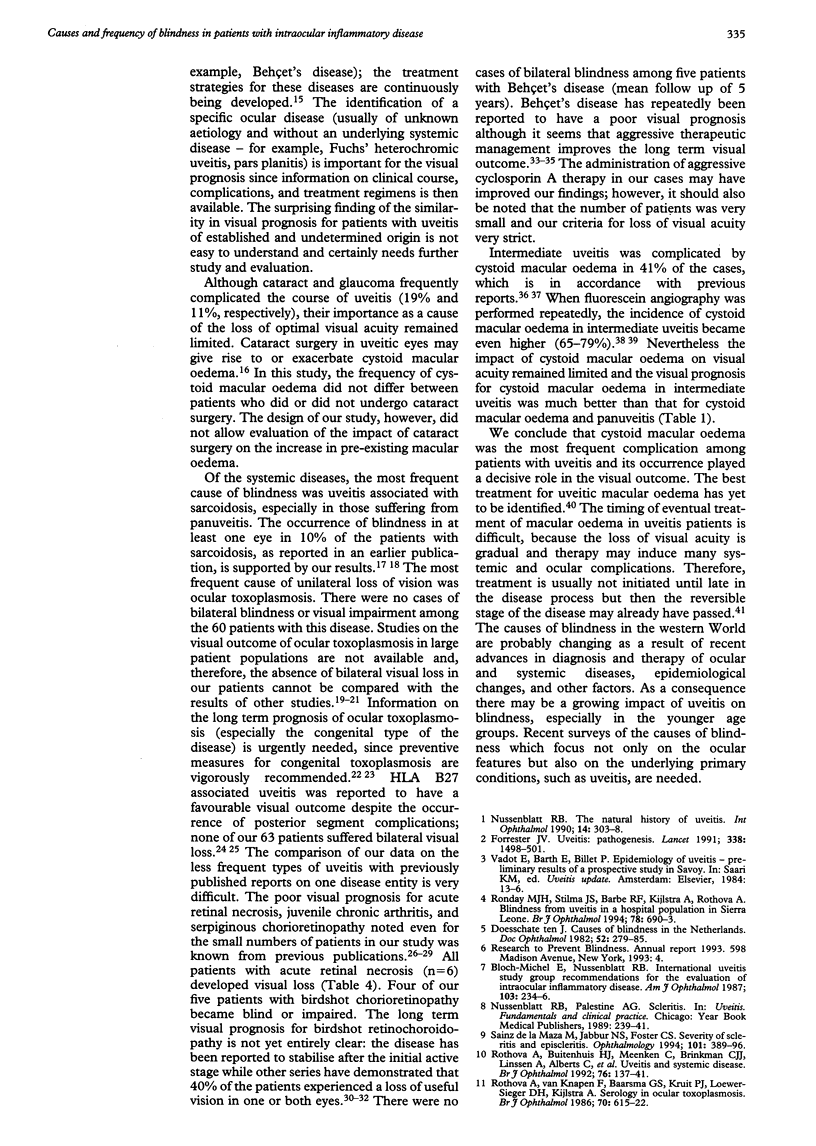
AIMS/BACKGROUND: Uveitis, an intraocular inflammatory disease, is a significant cause of visual impairment. It is not known how many patients with uveitis will retain visual acuity and how many develop visual impairment or even blindness. The aim of this study was to assess the frequency of blindness in patients with uveitis and, more specifically, to identify the clinical profile of patients at risk for visual loss. METHODS: A cross sectional and retrospective study of 582 patients with uveitis who visited the ophthalmology departments of two university hospitals in the Netherlands was performed. RESULTS: Within the group of 582 patients, 203 (35%) exhibited blindness or visual impairment; bilateral legal blindness developed in 22 (4%) patients, 26 (4.5%) had one blind eye with visual impairment of the other, and nine (1.5%) had bilateral visual impairment. Unilateral blindness developed in 82 (14%) patients, whereas 64 (11%) exhibited unilateral visual impairment. The most important cause of both blindness and visual impairment was cystoid macular oedema (29% and 41%, respectively). Complications of uveitis were encountered in more than half of the patients and 23% underwent one or more surgical procedures. When the patients were subdivided according to anatomical site, those with panuveitis had the worst visual prognosis. The systemic diseases associated with a poor visual prognosis were juvenile chronic arthritis and sarcoidosis. Ocular toxoplasmosis was the most frequent cause of unilateral visual loss. CONCLUSIONS: Cystoid macular oedema is the most frequent complication of uveitis and its occurrence plays a decisive role in the visual outcome of this disease.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bloch-Michel E., Nussenblatt R. B. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987 Feb 15;103(2):234–235. doi: 10.1016/s0002-9394(14)74235-7. [DOI] [PubMed] [Google Scholar]
- Chester G. H., Blach R. K., Cleary P. E. Inflammation in the region of the vitreous base. Pars planitis. Trans Ophthalmol Soc U K. 1976 Apr;96(1):151–157. [PubMed] [Google Scholar]
- Cochereau-Massin I., Wechsler B., Le Hoang P., Le Thi Huong D. u., Girard B., Rousselie F., Godeau P. Pronostic oculaire de la maladie de Behçet. J Fr Ophtalmol. 1992;15(5):343–347. [PubMed] [Google Scholar]
- Diamond G. Ocular manifestations of genetic and developmental diseases. Curr Opin Ophthalmol. 1994 Dec;5(6):72–78. doi: 10.1097/00055735-199412000-00012. [DOI] [PubMed] [Google Scholar]
- Dick A. D. The treatment of chronic uveitic macular oedema. Br J Ophthalmol. 1994 Jan;78(1):1–2. doi: 10.1136/bjo.78.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester J. V. Uveitis: pathogenesis. Lancet. 1991 Dec 14;338(8781):1498–1501. doi: 10.1016/0140-6736(91)92309-p. [DOI] [PubMed] [Google Scholar]
- Foulon W., Naessens A., Derde M. P. Evaluation of the possibilities for preventing congenital toxoplasmosis. Am J Perinatol. 1994 Jan;11(1):57–62. doi: 10.1055/s-2007-994537. [DOI] [PubMed] [Google Scholar]
- Heiligenhaus A., Bornfeld N., Foerster M. H., Wessing A. Long-term results of pars plana vitrectomy in the management of complicated uveitis. Br J Ophthalmol. 1994 Jul;78(7):549–554. doi: 10.1136/bjo.78.7.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hikichi T., Trempe C. L. Role of the vitreous in the prognosis of peripheral uveitis. Am J Ophthalmol. 1993 Oct 15;116(4):401–405. doi: 10.1016/s0002-9394(14)71395-9. [DOI] [PubMed] [Google Scholar]
- Laatikainen L., Erkkilä H. A follow-up study on serpiginous choroiditis. Acta Ophthalmol (Copenh) 1981 Oct;59(5):707–718. doi: 10.1111/j.1755-3768.1981.tb08737.x. [DOI] [PubMed] [Google Scholar]
- Lightman S. Uveitis: management. Lancet. 1991 Dec 14;338(8781):1501–1504. doi: 10.1016/0140-6736(91)92310-x. [DOI] [PubMed] [Google Scholar]
- Mamo J. G. The rate of visual loss in Behçet's disease. Arch Ophthalmol. 1970 Oct;84(4):451–452. doi: 10.1001/archopht.1970.00990040453009. [DOI] [PubMed] [Google Scholar]
- McAuley J., Boyer K. M., Patel D., Mets M., Swisher C., Roizen N., Wolters C., Stein L., Stein M., Schey W. Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial. Clin Infect Dis. 1994 Jan;18(1):38–72. doi: 10.1093/clinids/18.1.38. [DOI] [PubMed] [Google Scholar]
- McCabe R., Remington J. S. Toxoplasmosis: the time has come. N Engl J Med. 1988 Feb 4;318(5):313–315. doi: 10.1056/NEJM198802043180509. [DOI] [PubMed] [Google Scholar]
- Nussenblatt R. B. The natural history of uveitis. Int Ophthalmol. 1990 Oct;14(5-6):303–308. doi: 10.1007/BF00163549. [DOI] [PubMed] [Google Scholar]
- Priem H. A., Oosterhuis J. A. Birdshot chorioretinopathy: clinical characteristics and evolution. Br J Ophthalmol. 1988 Sep;72(9):646–659. doi: 10.1136/bjo.72.9.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruett R. C., Brockhurst J., Letts N. F. Fluorescein angiography of peripheral uveitis. Am J Ophthalmol. 1974 Apr;77(4):448–453. doi: 10.1016/0002-9394(74)90452-8. [DOI] [PubMed] [Google Scholar]
- Rodriguez A., Akova Y. A., Pedroza-Seres M., Foster C. S. Posterior segment ocular manifestations in patients with HLA-B27-associated uveitis. Ophthalmology. 1994 Jul;101(7):1267–1274. doi: 10.1016/s0161-6420(94)31179-1. [DOI] [PubMed] [Google Scholar]
- Ronday M. J., Stilma J. S., Barbe R. F., Kijlstra A., Rothova A. Blindness from uveitis in a hospital population in Sierra Leone. Br J Ophthalmol. 1994 Sep;78(9):690–693. doi: 10.1136/bjo.78.9.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothova A., Alberts C., Glasius E., Kijlstra A., Buitenhuis H. J., Breebaart A. C. Risk factors for ocular sarcoidosis. Doc Ophthalmol. 1989 Aug;72(3-4):287–296. doi: 10.1007/BF00153496. [DOI] [PubMed] [Google Scholar]
- Rothova A., Buitenhuis H. J., Meenken C., Brinkman C. J., Linssen A., Alberts C., Luyendijk L., Kijlstra A. Uveitis and systemic disease. Br J Ophthalmol. 1992 Mar;76(3):137–141. doi: 10.1136/bjo.76.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothova A., van Knapen F., Baarsma G. S., Kruit P. J., Loewer-Sieger D. H., Kijlstra A. Serology in ocular toxoplasmosis. Br J Ophthalmol. 1986 Aug;70(8):615–622. doi: 10.1136/bjo.70.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothova A., van Veenedaal W. G., Linssen A., Glasius E., Kijlstra A., de Jong P. T. Clinical features of acute anterior uveitis. Am J Ophthalmol. 1987 Feb 15;103(2):137–145. doi: 10.1016/s0002-9394(14)74218-7. [DOI] [PubMed] [Google Scholar]
- Ryan S. J., Maumenee A. E. Birdshot retinochoroidopathy. Am J Ophthalmol. 1980 Jan;89(1):31–45. doi: 10.1016/0002-9394(80)90226-3. [DOI] [PubMed] [Google Scholar]
- Sainz de la Maza M., Jabbur N. S., Foster C. S. Severity of scleritis and episcleritis. Ophthalmology. 1994 Feb;101(2):389–396. doi: 10.1016/s0161-6420(94)31325-x. [DOI] [PubMed] [Google Scholar]
- Weiss H., Annesley W. H., Jr, Shields J. A., Tomer T., Christopherson K. The clinical course of serpiginous choroidopathy. Am J Ophthalmol. 1979 Feb;87(2):133–142. doi: 10.1016/0002-9394(79)90131-4. [DOI] [PubMed] [Google Scholar]
- Wilson C. B., Remington J. S., Stagno S., Reynolds D. W. Development of adverse sequelae in children born with subclinical congenital Toxoplasma infection. Pediatrics. 1980 Nov;66(5):767–774. [PubMed] [Google Scholar]
- Wolf M. D., Lichter P. R., Ragsdale C. G. Prognostic factors in the uveitis of juvenile rheumatoid arthritis. Ophthalmology. 1987 Oct;94(10):1242–1248. doi: 10.1016/s0161-6420(87)80007-6. [DOI] [PubMed] [Google Scholar]
- de Boer J. H., Luyendijk L., Rothova A., Baarsma G. S., de Jong P. T., Bollemeijer J. G., Rademakers A. J., Van der Lelij A., Zaal M. J., Kijlstra A. Detection of intraocular antibody production to herpesviruses in acute retinal necrosis syndrome. Am J Ophthalmol. 1994 Feb 15;117(2):201–210. doi: 10.1016/s0002-9394(14)73077-6. [DOI] [PubMed] [Google Scholar]
- ten Doesschate J. Causes of blindness in The Netherlands. Doc Ophthalmol. 1982 Jan 29;52(3-4):279–285. doi: 10.1007/BF01675857. [DOI] [PubMed] [Google Scholar]


