Abstract
Background:
Complications exclusive of new neurological deficits/injuries that follow extreme lateral interbody fusion (XLIF) and related lateral lumbar interbody techniques should be better recognized to determine the safety of these procedures. Unfortunately, a review of the XLIF literature did not accurately reflect the frequency of these “other complications” as few US surgeons publish such adverse events that may lead to medicolegal suits.
Methods:
Major complications occurring with XLIF included sympathectomy, major vascular injuries, bowel perforations, sterile seromas, and instrumentation failures.
Results:
The frequency of sympathectomy was 4% for XLIF vs. 15% for anterior lumbar interbody fusion (ALIF). There were three major vascular injuries for XLIF; one fatal intraoperative event, one life-threatening retroperitoneal hematoma, and one iatrogenic lumbar artery pseudoaneurysm that was successfully embolized. Two bowel perforations were reported, whereas a third was a “direct communication.” One patient developed a sterile recurrent seroma due to vancomycin powder utilized for an XLIF. One study cited malpositioning of an XLIF cage resulting in a lateral L3–L4 extrusion, whereas the second series looked at the 45% risk of cage-overhang when XLIF devices were placed in the anterior one-third of the vertebral body.
Conclusion:
Excluding new neurological deficits, XLIF techniques resulted in multiple other major complications. However, these small numbers likely reflect just the tip of the iceberg (e.g., 10%) and the remaining 90% may never be known as many US-based spine surgeons fail to publish such adverse events as they are discoverable in a court of law and may lead to medicolegal suits.
Keywords: Bowel perforation, extreme lateral interbody fusion, lateral cage extrusion, major vessel injury, non-neurological complications, persistent seroma, retroperitoneal hematoma, sympathectomy
INTRODUCTION
Excluding new neurological deficits, other major complications following extreme lateral interbody fusions (XLIF) and related lateral lumbar interbody techniques should be better recognized to determine the safety of these procedures. The initial list of complications included sympathectomy, major vascular injuries, bowel perforations, seromas, and instrumentation failures. Unfortunately, this list does not likely accurately reflect the real frequency of these “other complications” as few US-based surgeons publish their personal/series-based adverse events due to medicolegal exposure (e.g., “discoverable” in a court of law and potentially leading to a suit). Therefore, the list of major XLIF complications likely constitutes just the tip of the iceberg (e.g., 10%), while the remaining 90% is yet to be published, leaving us wonder just how “safe” XLIF are.
EXCLUDING NEW NEUROLOGICAL DEFICITS, COMPLICATIONS OF MINIMALLY INVASIVE EXTREME LATERAL INTERBODY FUSION AND RELATED TECHNIQUES
Risk of sympathectomy with anterior lumbar interbody fusion vs. extreme lateral interbody fusion
Hrabalek et al. in 2015 retrospectively analyzed the risk of sympathectomy (utilizing thermography) performing anterior lumbar interbody fusion (ALIF) vs. XLIF procedures between the T12–L5 levels [Table 1].[4] They found that ALIF correlated with a 15% rate of sympathectomy versus the 4% encountered with XLIF.
Table 1.
Non-neurological complications (COMP.) following minimally invasive surgery (MIS) extremelateral lumbar interbody fusion (XLIF)
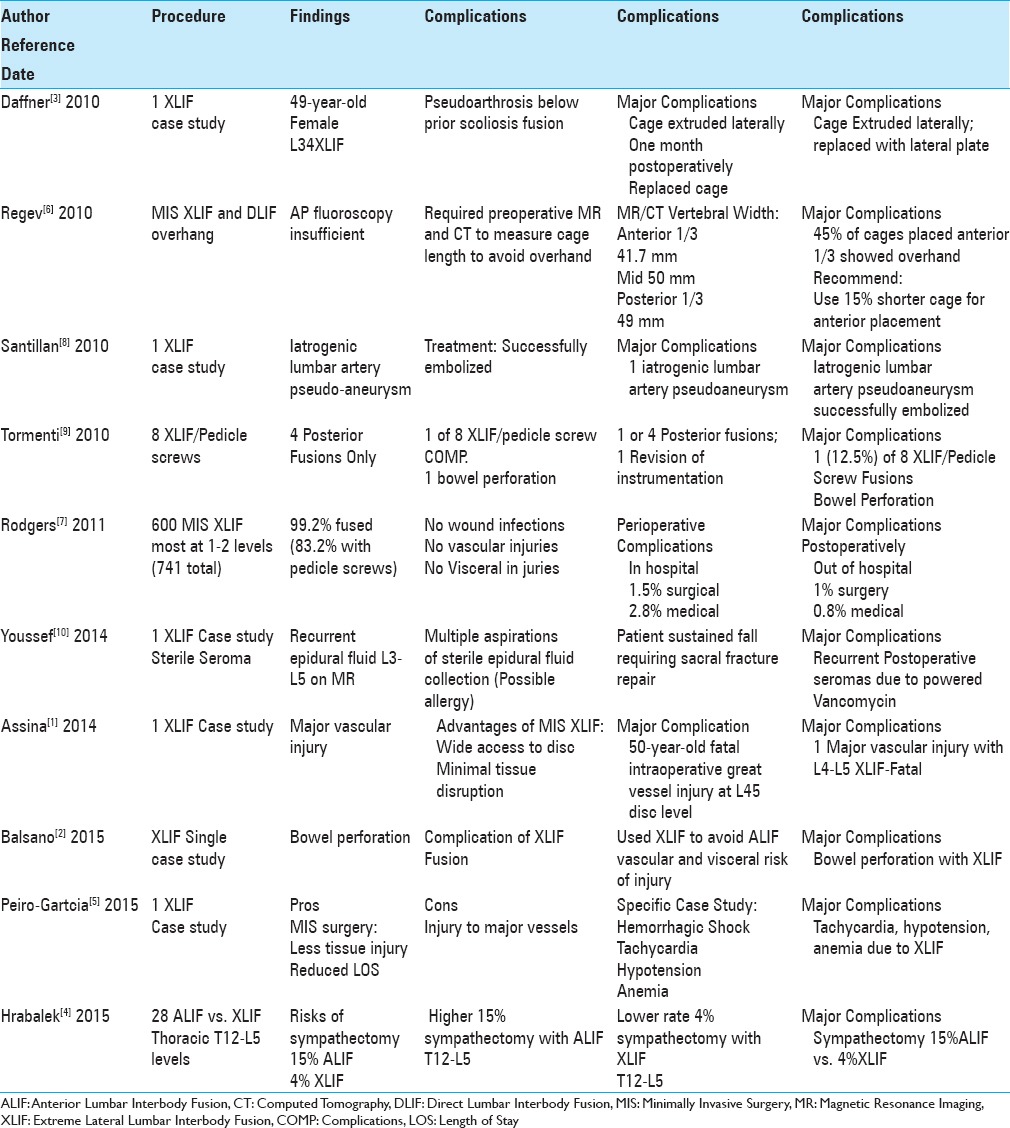
Three major vascular injuries attributed to extreme lateral interbody fusion
Three authors cited major vascular injuries attributed to XLIF. Santillan et al. in 2010 observed an iatrogenic lumbar artery pseudoaneurysm that followed a L4–L5 XLIF; it was successfully endovascularly embolized.[8] In 2014, Assina et al. noted the advantages of minimally invasive surgery (MIS) XLIF that included “wide access to the lumbar disc space” without using a separate access surgeon, and mininal tissue disruption [Table 1].[1] However, they reported a 50-year-old female who underwent an L4–L5 XLIF and sustained a fatal major intraoperative vascular injury. Subsequently, Peiro-Garcia et al. in 2015 cited the potential pros of a stand-alone XLIF approach to the lumbar spine (e.g., reduced intraoperative/postoperative bleeding/less tissue injury) along with its potential cons (e.g., trauma to segmental arteries and great vessels leading to retroperitoneal haematomas).[5] Their patient developed hemorrhagic shock (e.g., tachycardia, hypotension, and anemia) due to a retroperitoneal hematoma directly resulting from a major vessel injury occurring during an XLIF.
Rare bowel perforations attributed to extreme lateral interbody fusion
Two studies documented bowel perforations resulting from XLIF procedures, whereas a third case was a personal communication to the author.[2,9] Tormenti et al., in 2010, examined the complications of 8 XLIF/pedicles screw fusions utilized to treat adult scoliosis, and contrasted these results with 4 other patients undergoing posterior-only procedures/fusions.[9] Complications exclusive of new neurological deficits for the 8 patients included one bowel perforation requiring laparotomy/colon resection (later followed by a posterior procedure only), whereas 1 of the 4 patients undergoing posterior surgery required revision of instrumentation. In 2015, Balsano et al. wrote that XLIF procedures were developed to avoid/limit the morbidity of ALIF (e.g. especially major vessel/visceral injuries) [Table 1].[2] However, they presented a 70-year-old male who, following an L3–L4 and L4–L5 transpsoas XLIF fusion, sustained a bowel injury.
Through a personal communication, the author was also told of a patient who within 12 hours of XLIF surgery was draining feces.
Case of sterile seroma after multilevel extreme lateral interbody fusion due to vancomycin powder
Youssef et al. in 2014 cited a 59-year-old female who developed a recurrent sterile postoperative seroma following the application of 2 g of vancomycin powder to the XLIF wound; 1 g/bone graft/fusion and 1 g placed in the soft tissues [Table 1].[10] Six weeks later, due to a fall, the patient had a magnetic resonance (MRI) study that showed a surgical sacral fracture and a large epidural L3–L5 fluid collection; the fracture had to be repaired, and the seroma drained. Nevertheless, the fluid collection later required multiple additional aspirations. Notably, there was no clear explanation as to the etiology of this untoward event although one major differential diagnosis was an allergic response to the vancomycin.
Malpositioning of extreme lateral interbody fusion cages: Migration and overhang
Malpositioning and overhang are two technical surgical complications that must be considered when performing XLIF interbody cage procedures.[3,6] Daffner and Wang in 2010 presented a 49-year-old female who underwent a L3–L4 XLIF cage placement to address a pseudarthrosis resulting from a fusion attempted caudad to an old scoliosis arthrodesis.[3] When the cage extruded laterally 1 month postoperatively, it was removed/replaced though a mini-open lateral approach and supplemented with a lateral plate (e.g., to additionally address the “significant coronal deformity/lateral listhesis” due to the scoliosis). Furthermore, in 2010, Regev et al. noted that MIS XLIF or MIS direct lateral interbody fusion (DLIF) cage overhang (beyond the disc space) could occur if the cage length was solely estimated/based on anteroposterior fluoroscopy.[6] Using both MR and CT studies, they determined that 45% of cages were placed centrally (vertebral width was widest at 50 ± 4 mm), 34% were placed in the anterior one-third of the disc (vertebral body width was narrowest 41.7 ± 6 mm), whereas 7% were placed in the posterior one-third of the disc space (width 49 ± 1 mm). For those placed in the anterior one-third of the disc space, 45% demonstrated overhang that could potentially compromise the contralateral neural foramen in addition to other structures. They, therefore, recommended that surgeons consider shortening cages by 15% if they plan anterior placement.
Medical vs. surgical complications of extreme lateral interbody fusion
Rodgers et al. in 2011 evaluated intraoperative/postoperative complications of 600 predominantly 1–2 level MIS XLIF (741 levels) that included a 99.2% instrumentation rate (83.2% pedicle screws).[7] Perioperative complications (up to 6 postoperative weeks) occurred in 6.2% of patients; in the hospital, these included 9 (1.5%) surgical and 17 (2.8%) medical events; out of the hospital 6 (1.0%) were surgery-related, whereas 5 (0.8%) consisted of medical events. They reported no wound infections, vascular injuries, or intraoperative visceral injuries, but 11 (1.8%) patients required additional surgery. Notably, this study demonstrated that MIS XLIF are not without their medical risks as 3.6% of patients had significant medical complications within 6 postoperative weeks. Furthermore, the surgical reported risks of just 2.3% within this short 6-week postoperative interval probability missed some of the 6-week postoperative complications (note: the series involved 600 cases and data analysis may not always be performed by experts), along with the even more critical 3, 6, and 12-month postoperative adverse events.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
REFERENCES
- 1.Assina R, Majmundar NJ, Herschman Y, Heary RF. First report of major vascular injury due to lateral transpsoas approach leading to fatality. J Neurosurg Spine. 2014;21:794–8. doi: 10.3171/2014.7.SPINE131146. [DOI] [PubMed] [Google Scholar]
- 2.Balsano M, Carlucci S, Ose M, Boriani L. A case report of a rare complication of bowel perforation in extreme lateral interbody fusion. Eur Spine J. 2015;24(Suppl 3):S405–8. doi: 10.1007/s00586-015-3881-6. [DOI] [PubMed] [Google Scholar]
- 3.Daffner SD, Wang JC. Migrated XLIF cage: Case report and discussion of surgical technique. Orthopedics. 2010;33:518. doi: 10.3928/01477447-20100526-21. [DOI] [PubMed] [Google Scholar]
- 4.Hrabalek L, Sternbersky J, Adamus M. Risk of sympathectomy after anterior and lateral lumbar interbody fusion procedures. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159:318–26. doi: 10.5507/bp.2013.083. [DOI] [PubMed] [Google Scholar]
- 5.Peiró-García A, Domínguez-Esteban I, Alía-Benítez J. Retroperitoneal hematoma after using the extreme lateral interbody fusion (XLIF) approach: Presentation of a case and a review of the literature. Rev Esp Cir Ortop Traumatol. 2015 doi: 10.1016/j.recot.2014.12.006. pii: S1888-4415(15)00019-3. [DOI] [PubMed] [Google Scholar]
- 6.Regev GJ, Haloman S, Chen L, Dhawan M, Lee YP, Garfin SR, et al. Incidence and prevention of intervertebral cage overhang with minimally invasive lateral approach fusions. Spine. 2010;35:1406–11. doi: 10.1097/BRS.0b013e3181c20fb5. [DOI] [PubMed] [Google Scholar]
- 7.Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: An analysis of 600 cases. Spine. 2011;36:26–32. doi: 10.1097/BRS.0b013e3181e1040a. [DOI] [PubMed] [Google Scholar]
- 8.Santillan A, Patsalides A, Gobin YP. Endovascular embolization of iatrogenic lumbar artery pseudoaneurysm following extreme lateral interbody fusion (XLIF) Vasc Endovascular Surg. 2010;44:601–3. doi: 10.1177/1538574410374655. [DOI] [PubMed] [Google Scholar]
- 9.Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AS. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus. 2010;28:E7. doi: 10.3171/2010.1.FOCUS09263. [DOI] [PubMed] [Google Scholar]
- 10.Youssef JA, Orndorff DG, Scott MA, Ebner RE, Knewitz AP. Sterile Seroma Resulting from Multilevel XLIF Procedure as Possible Adverse Effect of Prophylactic Vancomycin Powder: A Case Report. Evid Based Spine Care J. 2014;5:127–33. doi: 10.1055/s-0034-1386754. [DOI] [PMC free article] [PubMed] [Google Scholar]


