Abstract
Ankle sprain is reported to be among the most common recurrent injuries. About 20% of acute ankle sprain patients develop chronic ankle instability. The failure of functional rehabilitation after acute ankle sprain leads to the development of chronic ankle instability. Differentiation between functional and anatomical ankle instability is very essential to guide the proper treatment. Stability testing by varus stress test and anterior drawer test should be carried out. Subtalar instability is an important pathology that is commonly by passed during the assessment of chronic ankle instability. Unlike acute ankle sprain, chronic ankle instability might require surgical intervention. The surgical and conservative management options can be very much developed by in-depth knowledge of the ankle anatomy, biomechanics, and pathology. Anatomical repair, augmentation by tendon, or both are the basic methods of surgical intervention. Arthroscopy is becoming more popular in the management of chronic ankle instability.
Key words: Etiology, ankle, chronic instability, diagnosis, surgical techniques
INTRODUCTION
Ankle sprains are very much common both in the sporting activities and the general community. Acute ankle sprains are treated mostly by conservative measures,[1] but many people might develop chronic ankle instability and pain.[2,3]
Although chronic ankle instability has a high repetitive prevalence, it is still not deeply understood. The impairments connected with chronic ankle instability can be highly, likely proprioceptive deficits and increased ligamentous laxity. Walking, jumping, occupational involvement, and sporting activities can be affected.[4]
EPIDEMIOLOGY
As the ankle is the most traumatized body part in sport injuries that account for 10–30% of all sport injuries,[5] many studies showed that 2–7 individuals are affected per 1000 in the general population each year.[6,7] Military service members were reported in epidemiology studies to have experienced greater ankle sprains than civilian population since 58/1000 person-years in the USA military service are affected.[8]
ETIOLOGY AND CLASSIFICATION
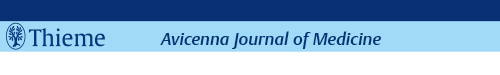
Since the anterior talofibular ligament (ATFL) is the weakest with the lowest ultimate load along with anatomical positions and insertions [Figure 1], it is most commonly injured in a lateral ankle sprain.[9] In comparison with the ATFL, the calcaneofibular ligament (CFL) is stronger and larger and runs obliquely. The posterior talofibular ligament is thick and strong which is rarely injured; it is a trapezoidal ligament and lies in a horizontal plane.[9]
Figure 1.
The lateral ligamentous components of the ankle joint
Chronic ankle instability can be functional instability or mechanical instability. Functional instability depends on the patient-generated reports or complaints that could be accompanied by clinical laxity while mechanical instability can be identified by physical examination.[10,11] When patients with chronic ankle instability fail to improve through a conservative management course and physical therapy, surgery is, in most cases, the only option for them.
PRESENTATION
Patients who fail to make a successful recovery through nonsurgical methods often complain of apprehension of ankle instability and are prone to experience chronic ankle instability.
Clinically, the history of patients with chronic ankle instability reveals past recurrent ankle sprains and severe inversion injury. They take special precautions against weight bearing, strenuous activities, and walking on rugged surfaces; wearing braces would just provide partial relief. Chronology, chronic ankle instability is when the injury is too obstinate to recover over the first 6 weeks and the ankle cannot retain its mechanical and functional performance.[12,13] Mechanical ankle instability is induced by ligament laxity; while functional ankle instability is caused by postural control deficits, neuromuscular deficits, muscle weakness, and proprioceptive deficits.[14] The chronic ankle instability selection criteria have recently been updated by the International Ankle Consortium,[15] and there may be seven subsets, including mechanical instability interaction, frequency of multiple sprains, and perceived instability.
The physical examination of the chronic ankle instability should include inspecting the lower extremity to check if there is any hindfoot varus misalignment – the heels posture is slightly turned inside. The physical examination should also include assessing ligamentous laxity and midfoot cavus, which is a foot-high arch condition.[16] Peroneal muscle strength and hindfoot motion should be assessed. The proprioception in patients with chronic ankle instability is commonly abnormal; hence, the Romberg's maneuver should be carried out.[17] It helps in assessing normal ankles as well. Assessing the motion range at the midtarsal and subtalar joints and the ankle is significant. To assess subluxation, weakness, or tenderness, the tendoachilles ligamentous complex should also be assessed. Table 1 summarizes author approach to patients with a history of chronic ankle instability.
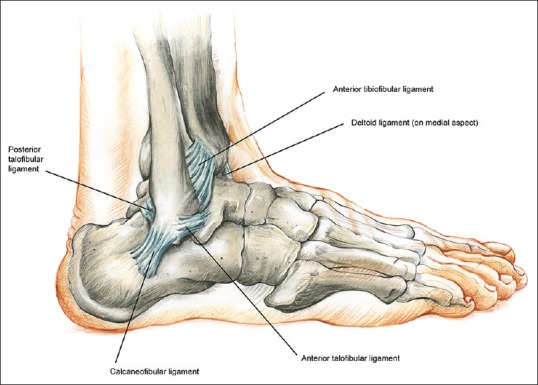
Table 1.
The authors' views regarding patients with lateral ankle laxity
Associated lesions
Chronic ankle instability is often associated with lesions that evolve from contributory factors. They do not necessarily occur with chronic ankle instability, and if any, not all these lesions occur together. Associated lesions that may accompany chronic ankle instability are chronic regional pain syndrome, neuropraxia, sinus tarsi syndrome, tendon disorders such as peroneal tendinopathy, dislocation or subluxation, impingement syndromes, fractures such as anterior calcaneal process, fibula and lateral talar process, loose bodies, and osteochondral lesion of talar dome or distal tibia. The following lesions frequently present with chronic ankle instability:
Sinus tarsi syndrome is common among basketball and volleyball players, dancers, and overweight people. It is also common among patients with flatfoot and hyperpronation deformities. It consists of pain and tenderness of the sinus tarsi; that is, the lateral side of the hindfoot. It may occur following a single or series of ankle sprains.[18] It is diagnosed by exclusion although magnetic resonance imaging could show evidence of the inflammation. Sinus tarsi syndrome is treated by primary repair of the sinus tarsi ligaments, augmentation by tendon, or both
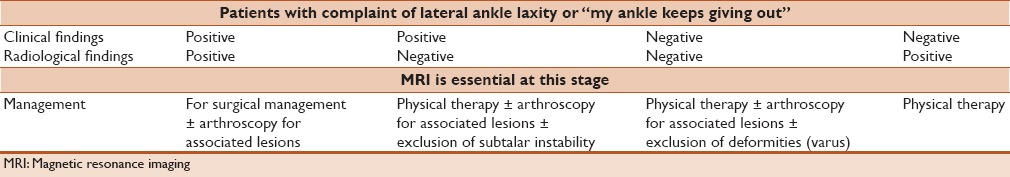
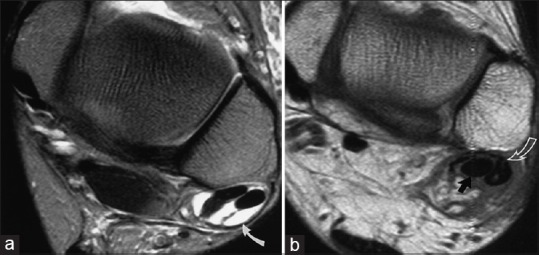
Osteochondral defects (OCD) are injuries to the talus [Figure 2]. They may include cartilage layers blistering and in-the-bone cyst-like lesions or even bone layers and cartilage fracture. OCD may occur as a result of one traumatic injury or recurrent trauma. OCD display swelling, ankle joint instability, and long pain. The exact mechanism of both pain and instability is not fully understood. Treatment is ideally operative depending on the nature, size, and location of the lesions[19]
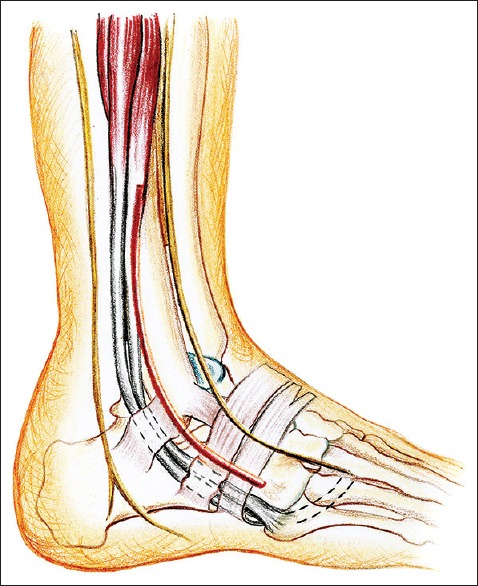
Peroneal tendinopathy [Figure 3] is chronic inflammation of the peroneal tendon resulting in weakness of the active ankle stabilizers. This happens when a person performs a repetitive activity that annoys the tendon over a long period. In addition, poor and rapid training and poor shoe-wear may cause peroneal tendinosis. People who have a hindfoot varus posture are more likely to experience peroneal tendinosis. Most cases of peroneal tendinosis are treated conservatively although surgical debridement and stimulation of healing either open or tendoscopically are gaining popularity[20]
Subtalar instability is an incidence whose etiology is still not known. It seems to be underdiagnosed. It can have the symptoms of the chronic ankle instability. Clinically, the patients with subtalar instability have increased inward rotation. It is treated by a tendon transfer or tenodesis procedure such as Chrisman–Snook or alternatively by an anatomic ligament reconstruction.[21]
Figure 2.
(a) Sagittal and (b) coronal views of magnetic resonance imaging showing osteochondral defects of the talus
Figure 3.
Peroneal tendinopathy. (a) Peroneal tenosynovitis. (b) Longitudinal tear of the peroneal brevis tendon
MANAGEMENT
Conservative approach
Before conducting any surgical procedure, nonsurgical management is highly recommended for patients with chronic ankle instability at least over the first 2-month period. During the rehabilitation stage, physiotherapy and orthotics should be initiated. Neuromuscular and proprioceptive training should be provided.[22]
When bracing and taping methods fail to provide support for chronically unstable ankles persistently fail to recover, surgery is to be considered.
Surgical approach
Surgical management is advised when chronic ankle instability is persistent and other options are of no use. Operative procedures of chronically unstable ankles fall into: Anatomic repair, nonanatomic reconstruction, and anatomic reconstruction. Figure 4 shows the standard surgical approach.[23]
Figure 4.
Standard surgical approach
Anatomic repairs revealed good and excellent results at 85% of patents.[24] However, patients who had poor tissue, long-standing ankle instability, cavovarus foot deformity, and ligamentous laxity failed to realize success even though local tissues or free tendon allograft.[25] Therefore, the nonanatomic and anatomic procedures of reconstructive tenodesis should be considered.
The injured ligaments are repaired by applying tendon grafts or local tissues by anatomic reconstruction procedures. Broström procedure is the most common among the other approaches. The midsubstance repair of the ATFL and CFL was conducted by the Broström procedure [Figure 5].[26] Patients with chronic ankle instability and intra-articular symptoms had good results when they underwent the modified Broström procedures and ankle arthroscopy.[27]
Figure 5.
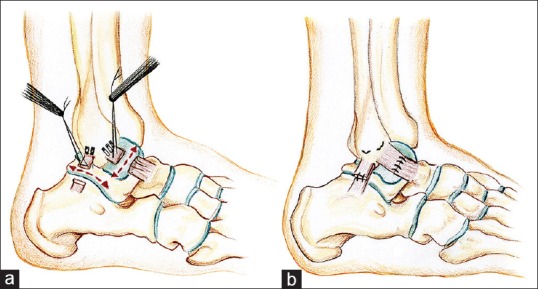
Primary repair. (a) Identification and suturing of the torn ligament. (b) End-to-end repair on tension
The Broström procedure repairs damaged lateral ligaments, ankle stability, the ATFL, in particular. Around 85–90% of the patients who underwent the Broström procedure gained ankle stability.[24] It takes about 3–6 months for the patient to recover. Gould modified the Broström procedure as the repair was strengthened by the inferior extensor retinaculum, and the subtalar joint became more stabilized.[28] When attenuation is noted at the ATFL and CFL, anatomic reconstruction is recommended to be performed.
In nonanatomic reconstruction, the lateral ankle ligaments were reconstructed by the tensor fasciae latae [Figure 6]. Chronic lateral ankle instability can be reconstructed by applying also a nonanatomic tenodesis, which is stabilizing the end of the tendon to a bone.[16] Watson-Jones [Figure 7] carried out a procedure to limit rotation and interior subluxation: They used peroneus brevis and routed the tendon through anterior-to-posterior (distal-to-proximal) style passing through the fibula to be secured to the talar neck.[29] About 88% of patients revealed good-to-excellent results in Watson-Jones reconstruction procedure after 13-year follow-up.[30] In the Chrisman-Snook reconstruction procedure, the peroneus brevis tendon is the first split and then driven into the fibula and then into the calcaneus.[31] This procedure supports anatomic reconstruction, but some patients were reported to experience nonphysiological kinematics and subtalar stiffness [Figure 7].
Figure 6.
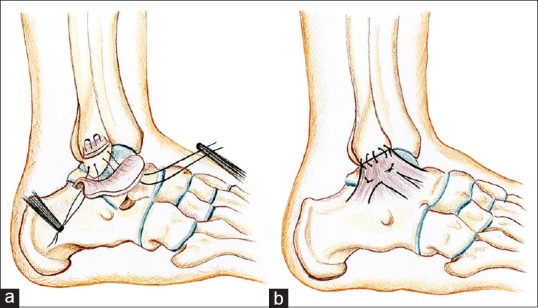
Ahlgren technique. (a) Augmentation by nearby fascia. (b) Interosseous suture
Figure 7.
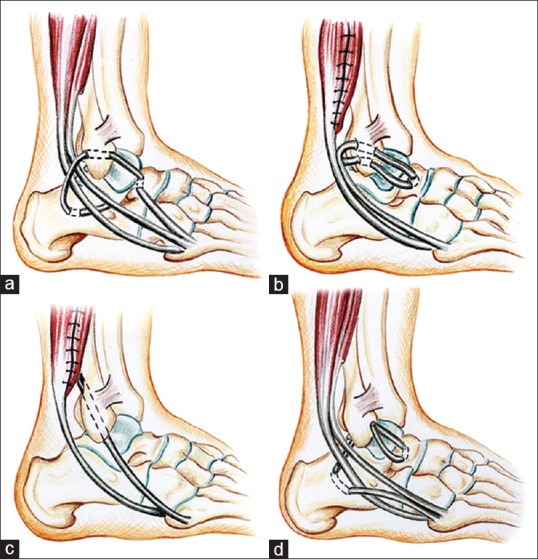
Augmentation by peroneal brevis flap. (a) Watson-Jones. (b) Evans. (c) Chrisman-Snook. (d) Colville
Arthroscopic role
Because intra-articular conditions such as impingement, painful ossicles, talus osteochondral lesions, osteophytes, and chondromalacia can accompany chronic ankle instability and can be factored in dysfunction and pain, arthroscopy is recommended somehow.
To help the reconstruction of autogenous plantaris tendon of the CFL and ATFL, a 3-portal arthroscopic approach is recommended to be employed.[32] For chronic ankle instability with no ligamentous repair, arthroscopic thermal capsular shrinkage is also recommended.[33] In our opinion, Broström-Gould procedure is recommended as an anatomic repair and can be preceded by arthroscopy to look for and treat associated lesions.
Complications
The most common problems associated with postoperative management can be wound complications, which can happen at about 4% of nonanatomic tenodesis and about 1.6% after anatomic repair.[34] Other prognoses include stiffness, recurrent instability, and nerve problems.
Mostly, wound problems require special care, but nerve problems can be a postoperative sensation of paresthesia, which disappears by time or neuromata, which is recommended to be excised operatively. Nerve-related problems account for 9.7% for nonanatomic tenodesis, 3.8% for anatomic repair, and 1.9 for anatomic tenodesis.[34] Long-standing instability and ligamentous laxity in addition to a cavovarus foot are among the risk factors for failure after the operation.[34] After anatomic and nonanatomic reconstructions, stiffness is common but can be tolerated. The loss of tibiotalar and subtalar impingement and motion can be caused by overtightening when performing nonanatomic tenodesis reconstruction.[34] To treat subjective failure, physiotherapy is highly recommended. Late recurrent instability may be caused by minor chronic injuries while early recurrent instability may be caused by acute injury.[34]
CONCLUSION
Acute ankle sprains are generally treated conservatively while chronic ankle instabilities usually require surgery. Chronic ankle instability has associated lesions depending on the nature of the instability; addressing these associated lesions is very critical to the outcome. Treatment methods are either conservative or surgical. In the rehabilitation stage, physiotherapy and orthotics should be initiated. Surgically, the injured ligaments are repaired by applying tendon grafts or local tissues. Among the surgical methods is the Broström procedure that primarily repairs the damaged ligaments. Augmenting the primary repair by tendon transfer protects the repair and adds to the stability. Arthroscopy is ready to lend a hand to diagnose and treat the ankle instability.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to duly express their heartfelt appreciation and gratitude to Ms. Jana Elias, Cambridge School of Art (BA [Hons] Illustration, 3rd year) Cambridge, UK, for providing this manuscript with its artwork.
REFERENCES
- 1.Al-Mohrej OA, Al-Kenani NS. Acute ankle sprain: Conservative or surgical approach? EFORT Open Rev. 2016;1:28–38. doi: 10.1302/2058-5241.1.000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bridgman SA, Clement D, Downing A, Walley G, Phair I, Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20:508–10. doi: 10.1136/emj.20.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324–31.e6. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Snyder AR, Parsons JT, Valovich McLeod TC, Curtis Bay R, Michener LA, Sauers EL. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part I: Disablement models. J Athl Train. 2008;43:428–36. doi: 10.4085/1062-6050-43.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hølmer P, Søndergaard L, Konradsen L, Nielsen PT, Jørgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15:72–4. doi: 10.1177/107110079401500204. [DOI] [PubMed] [Google Scholar]
- 6.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279–84. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 7.Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984;183:160–8. [PubMed] [Google Scholar]
- 8.Waterman BR, Belmont PJ, Jr, Cameron KL, Deberardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38:797–803. doi: 10.1177/0363546509350757. [DOI] [PubMed] [Google Scholar]
- 9.Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, et al. Anatomy of the ankle ligaments: A pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557–69. doi: 10.1007/s00167-010-1100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ajis A, Maffulli N. Conservative management of chronic ankle instability. Foot Ankle Clin. 2006;11:531–7. doi: 10.1016/j.fcl.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez-Merchan EC. Chronic ankle instability: Diagnosis and treatment. Arch Orthop Trauma Surg. 2012;132:211–9. doi: 10.1007/s00402-011-1421-3. [DOI] [PubMed] [Google Scholar]
- 12.Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16:608–15. doi: 10.5435/00124635-200810000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: A critical review. Foot Ankle Spec. 2014;7:298–326. doi: 10.1177/1938640014539813. [DOI] [PubMed] [Google Scholar]
- 14.Coughlin MJ, Schenck RC, Jr, Grebing BR, Treme G. Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft. Foot Ankle Int. 2004;25:231–41. doi: 10.1177/107110070402500407. [DOI] [PubMed] [Google Scholar]
- 15.Gribble PA, Delahunt E, Bleakley CM, Caulfield B, Docherty CL, Fong DT, et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J Athl Train. 2014;49:121–7. doi: 10.4085/1062-6050-49.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69:17–26. [PubMed] [Google Scholar]
- 17.Nitz AJ, Dobner JJ, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med. 1985;13:177–82. doi: 10.1177/036354658501300306. [DOI] [PubMed] [Google Scholar]
- 18.Helgeson K. Examination and intervention for sinus tarsi syndrome. N Am J Sports Phys Ther. 2009;4:29–37. [PMC free article] [PubMed] [Google Scholar]
- 19.Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, Hennessy M, et al. Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int. 2015;36:1045–9. doi: 10.1177/1071100715585525. [DOI] [PubMed] [Google Scholar]
- 20.Heckman DS, Gluck GS, Parekh SG. Tendon disorders of the foot and ankle, part 1: Peroneal tendon disorders. Am J Sports Med. 2009;37:614–25. doi: 10.1177/0363546508331206. [DOI] [PubMed] [Google Scholar]
- 21.Aynardi M, Pedowitz DI, Raikin SM. Subtalar instability. Foot Ankle Clin. 2015;20:243–52. doi: 10.1016/j.fcl.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 22.McCriskin BJ, Cameron KL, Orr JD, Waterman BR. Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop. 2015;6:161–71. doi: 10.5312/wjo.v6.i2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Besse JL. Instabilités latérales chroniques de cheville. In: Leemrijse T, editor. Pathologie du Pied et de la Cheville. France: Elsevier Masson; 2009. pp. 454–66. [Google Scholar]
- 24.Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34:975–8. doi: 10.1177/0363546505282616. [DOI] [PubMed] [Google Scholar]
- 25.Nakata K, Shino K, Horibe S, Natsu-Ume T, Mae T, Ochi T. Reconstruction of the lateral ligaments of the ankle using solvent-dried and gamma-irradiated allogeneic fascia lata. J Bone Joint Surg Br. 2000;82:579–82. doi: 10.1302/0301-620x.82b4.10368. [DOI] [PubMed] [Google Scholar]
- 26.Hua Y, Chen S, Li Y, Chen J, Li H. Combination of modified Broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy. 2010;26:524–8. doi: 10.1016/j.arthro.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Lee KT, Park YU, Kim JS, Kim JB, Kim KC, Kang SK. Long-term results after modified Brostrom procedure without calcaneofibular ligament reconstruction. Foot Ankle Int. 2011;32:153–7. doi: 10.3113/FAI.2011.0153. [DOI] [PubMed] [Google Scholar]
- 28.Buerer Y, Winkler M, Burn A, Chopra S, Crevoisier X. Evaluation of a modified Broström-Gould procedure for treatment of chronic lateral ankle instability: A retrospective study with critical analysis of outcome scoring. Foot Ankle Surg. 2013;19:36–41. doi: 10.1016/j.fas.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Watson-Jones R. Recurrent forward dislocation of the ankle joint. J Bone Jt Surg Br. 1952;34:519. [Google Scholar]
- 30.Sugimoto K, Takakura Y, Akiyama K, Kamei S, Kitada C, Kumai T. Long-term results of Watson-Jones tenodesis of the ankle. Clinical and radiographic findings after ten to eighteen years of follow-up. J Bone Joint Surg Am. 1998;80:1587–96. doi: 10.2106/00004623-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Chrisman OD, Snook GA. Reconstruction of lateral ligament tears of the ankle. An experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969;51:904–12. [PubMed] [Google Scholar]
- 32.Lui TH. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:554.e1–5. doi: 10.1016/j.arthro.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 33.Maiotti M, Massoni C, Tarantino U. The use of arthroscopic thermal shrinkage to treat chronic lateral ankle instability in young athletes. Arthroscopy. 2005;21:751–7. doi: 10.1016/j.arthro.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 34.Sammarco VJ. Complications of lateral ankle ligament reconstruction. Clin Orthop Relat Res. 2001;391:123–32. doi: 10.1097/00003086-200110000-00013. [DOI] [PubMed] [Google Scholar]