Abstract
Objective:
The aim of this study is to evaluate the etiological causes of pancytopenia in patients who were admitted to the hematology ward due to pancytopenia.
Materials and Methods:
All patients who were admitted to the hematology ward of Ministry of Health Istanbul Training and Research Hospital due to pancytopenia between 2013 and 2015 were retrospectively evaluated regarding etiological causes.
Results:
A total of 137 patients was evaluated. The etiological causes of pancytopenia were recorded as Vitamin B12 deficiency (n: 24; 17%), chronic liver disease (n: 21; 15%), malignancy (n: 19; 13%), myelodysplastic syndrome (n: 18; 13%), aplastic anemia (n: 11; 8%), rheumatic diseases (n: 7; 5%), and endocrine causes (n: 3; 2%).
Conclusion:
The etiological causes of pancytopenia vary depends on patients' age, gender, country, and other conditions. Vitamin B12 deficiency is the most common treatable cause of pancytopenia. Most of the etiological causes could be diagnosed with laboratory analysis and radiological imagings, without the need of a bone marrow examination.
Key words: Chronic liver disease, myelodysplastic syndrome, pancytopenia, Vitamin B12 deficiency
INTRODUCTION
Pancytopenia is defined as a reduction in the number of red cells, white cells, and platelets. It can manifest as a laboratory finding of many diseases. It can be treated with vitamin substitution in the case with vitamin deficiency, but diagnosis sometimes needs advanced techniques, such as bone marrow biopsy.[1] Etiological causes of pancytopenia often vary by geographical region, age, and gender. They include megaloblastic anemia, other nutritional anemia, aplastic anemia (AA), splenomegaly, sepsis, leukemia, lymphoma, multiple myeloma, myelodysplastic syndromes (MDSs), alcoholic diseases, HIV and hepatitis viruses, autoimmune diseases, endocrine diseases and bone marrow infiltrating diseases (such as Gaucher's disease).[2] During the diagnostic process, patients undergo laboratory tests and radiological imagings, and invasive procedures in case they are needed. The diagnosis can take a long time depending on the physician's experience and knowledge, as well as the cause of pancytopenia. Vitamin B12 deficiency commonly causes pancytopenia and mimics MDS.[3]
The aim of this study is to evaluate the etiological causes of pancytopenia in patients, who were admitted to the hematology ward due to pancytopenia.
MATERIALS AND METHODS
We retrospectively evaluated all the patients who were admitted to the hematology ward of Ministry of Health Istanbul Training and Research Hospital due to pancytopenia between 2013 and 2015. Pancytopenia was defined as a hemoglobin <9 g/dL; a total leukocyte count <4000/μL; or a platelet count <100,000/μL.[4] Patients were followed up as outpatients or inpatients depending on the clinical status of the patient. We retrospectively extracted and used the patients' medical record data, including anamnesis, physical examination, medical history, complete blood count, peripheral blood smear, biochemical and ELISA tests, blood vitamin levels, thyroid hormones, abdominal ultrasonography, autoimmune panels (antinuclear antibodies, anti-ds DNA), brucellosis tests, and bone marrow biopsy. We excluded patients who developed pancytopenia due to cancer chemotherapy and radiotherapy from this study. Chronic liver diseases have been diagnosed with laboratory tests, radiological imaginations (ultrasonography, magnetic resonance imaging, etc.), or biopsy. The Local Ethical Committee has approved the protocol for this study.
Statistical analysis
Continuous variables were described as mean ± standard deviation and range. Percentile values were described without decimals.
RESULTS
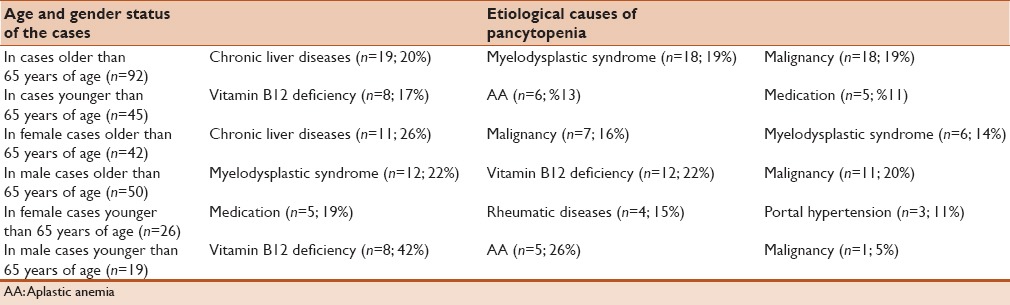
A total of 137 patients were included in this study and were evaluated retrospectively. Mean age was 63.52 ± 21.32 years (range: 17–95 years; 18s' 95 years for male; 17s' 84 years for female), and 69 patients (50%) were male. The numbers of patients who were younger than 65 years and older than 65 years were 45 (33%) and 92 (67%), respectively. Recorded signs and symptoms of patients at admission were anemia, paleness and fatigue (90%), splenomegaly (37%), hepatomegaly (28%), bleeding (24%), and leukopenia/neutropenia (12%), respectively. Etiological factors of pancytopenia were recorded as Vitamin B12 deficiency (n: 24; 17%); chronic liver disease (n: 21; 15%), malignancy (n: 19; 13%), MDS (n: 18; 13%), AA (n: 11; 8%), rheumatic diseases (n: 7; 5%), and endocrine causes (n: 3; 2%), respectively. Other rare causes included hemophagocytic syndrome (n: 1), storage disease (two sisters with Gaucher disease), and hypersplenism due to diffuse splenic involvement of sarcoidosis (n: 1). A case with pancytopenia that presented to our ward with splenomegaly was characterized by splenic hypodense multiple masses. It was thought to be lymphoma, but a histopathologic examination of the bone marrow biopsy was normal, and later splenectomy had been performed. Sarcoidosis was then diagnosed in that patient. The etiological causes of pancytopenia were categorized by age and gender in Table 1. Hemophagocytic cells were observed in the bone marrow biopsy of a case who later passed away within 2 weeks. Etiology, in that case, could not be determined.
Table 1.
The most common etiological causes of pancytopenia of cases by gender and age
DISCUSSION
Many diseases cause pancytopenia, and frequencies of those diseases vary by country, gender, and age. These causes tend not to be severe. For example, common cold viruses cause transient pancytopenia, but AA and MDS can have fatal consequences.[5] Vitamin B12 deficiency and infective causes are common in underdeveloped and developing countries, while malignant causes predominate in developed country. For example, a study of Kemal et al. had reported that malaria and hypersplenism were most the common causes in Yemen followed by megaloblastic anemia.[6] However, a study that evaluated the etiological causes in 195 cases with pancytopenia in South Africa revealed as causes of pancytopenia: bone marrow failure (67.7%), AA (11%), serious infections (9.7%), and hypersplenism (7.7%), respectively.[7] In another study that had evaluated the etiology of pancytopenia with 77 patients' bone marrow biopsies in India, megaloblastic anemia was reported to be the most common cause (68%), whereas AA (7.7%), MDS and hemophagocytic syndrome, respectively, were rare causes.[8] In a study, which had evaluated 166 pancytopenia cases from two centers for 6 years in India, the common causes were reported to be AA in 49 cases, megaloblastic anemia in 37 cases, leukemia and lymphoma in 30 cases, and hypersplenism in 19 cases, respectively. It emphasized that megaloblastic anemia should not be overlooked because it was a treatable cause of pancytopenia.[4]
Although our study did not include a large number of patients, it included pancytopenia cases living in Istanbul that had ethnocultural diversity. Etiological causes of pancytopenia vary by province in our country. For example, if this study had been conducted in Kelkit Valley in Turkey, especially in the spring and summer seasons, Crimean–Congo hemorrhagic Fever could have come across as the most important reason. In addition, we have categorized the cases as young- and older- middle-aged, because we aimed to reveal the importance of age that should be taken into consideration in the differential diagnosis of pancytopenia. In this study, the most common cause was chronic liver disease, followed by MDS in the cases who were older than 65 years of age, whereas Vitamin B12 deficiency was the most common cause in the young adults. Causes of pancytopenia were commonly benign in the young adults, whereas chronic diseases and malignant causes were observed at older ages. Hematological malignancies and chemotherapy-related pancytopenia were not evaluated in this study. It should be taken into consideration that immune hemolytic anemia and immune thrombocytopenia can develop in 10% of chronic lymphocytic leukemia (CLL) patients. Evans syndrome and pure red cell aplasia may be observed together as well.[9] Bone marrow biopsies can be examined as hypocellular or hypercellular in patients with pancytopenia. The hypocellular bone marrow is seen in AA, hypoplastic MDS, and paroxysmal nocturnal hemoglobinuria, whereas hypercellular view is seen in megaloblastic anemia, MDS, hypersplenism caused by portal hypertension, malaria, and visceral leishmaniasis.[10] It was reported that immune cytopenia had emerged before the diagnosis of CLL many years ago, and malignant B-CLL clone could cause antibody-producing immune cytopenia.[11] MDS is the deterioration of blood cell production in the bone marrow and often accompanies with other hematopoietic stem cell diseases. It is especially diagnosed in older men with pancytopenia.[12] MDS and cancers should be taken into consideration in older male cases with pancytopenia.
Vitamin B12 deficiency was recorded as the most frequent cause of pancytopenia in the young adults. It is commonly diagnosed as MDS. Because nuclear maturation abnormalities, dysplasia and megaloblastic changes in all three series are observed in the evaluation of bone marrow smears. It can be distinguished with elevated blood lactic dehydrogenase and recovery of pancytopenia in 1s' 2 weeks after Vitamin B12 substitution.[3]
Chronic liver diseases (infectious, noninfectious, compensated, and noncompensated cirrhosis) were common causes in all patients and female patients older than 50 years, whereas solid tumors and MDS were more common in male cases older than 50 years. As a complication of chronic liver disease, portal hypertension diseases lead pancytopenia by hypersplenism.[13] Acute and chronic viral hepatitis B and C, brucellosis, and HIV infections cause pancytopenia as well. Suppression of bone marrow, hypersplenism due to splenomegaly and antiviral drugs are related to pancytopenia in cases with chronic liver disease.[14]
Medications and rheumatic diseases were common causes in female cases younger than 65 years old in our study population. Drugs, which are used in the treatment of rheumatic diseases cause pancytopenia as a side effect or as primary illness.[15] In fact, drugs and acute respiratory tract infections caused by viruses (influenza virus, parainfluenza virus, adenovirus, etc.) are very common in cases who are admitted to internal diseases and infectious diseases wards with pancytopenia, but those cases generally recover within a short time.[15,16] Those causes were not recorded among our cases. Hematologic causes have stood out in the etiology of pancytopenia among our cases, as cases who were admitted to hematology ward had been evaluated.
Gaucher disease and sarcoidosis are rarely observed in the etiology of pancytopenia. Pancytopenia develops due to bone marrow infiltration and/or splenomegaly related to those diseases. We have diagnosed a rare clinical form of sarcoidosis in one patient that caused cytopenia being related to splenomegaly and hypersplenism.[17] A rare cause of pancytopenia is macrophage activation syndrome (MAS) or hemophagocytic syndrome that commonly results in death.[18,19] MAS is generally secondary to infection or malignancy. Hemophagocytic cells were observed in the bone marrow biopsy of our case who had died within 2 weeks. Etiology could not be determined.
Up to the time of completion of this study, there was no study that had evaluated the etiological causes of pancytopenia in Turkey. Almost all patients with pancytopenia had been presented as case reports. Brucellosis, Vitamin B12 deficiency, malaria, and hematological causes have been reported as the etiological causes of pancytopenia as well.[20,21,22,23]
CONCLUSION
Patient's age, gender, anamnesis, physical examination, history, laboratory test results, and radiological findings provide important hints in the diagnosis of pancytopenia. Etiological causes of pancytopenia and their rates may differ in each study from same and different countries. However, most of the etiological causes of pancytopenia were associated with nonhematological diseases and were diagnosed with laboratory tests without the need of a bone marrow examination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Khattak MB, Ismail M, Marwat ZI, Khan F. Frequency and characterisation of pancytopenia in megaloblastic anaemia. J Ayub Med Coll Abbottabad. 2012;24:53–5. [PubMed] [Google Scholar]
- 2.Rangaswamy M, Prabhu, Nandini NM, Manjunath GV. Bone marrow examination in pancytopenia. J Indian Med Assoc. 2012;110:560–2, 566. [PubMed] [Google Scholar]
- 3.Kim M, Lee SE, Park J, Lim J, Cho BS, Kim YJ, et al. Vitamin B(12)-responsive pancytopenia mimicking myelodysplastic syndrome. Acta Haematol. 2011;125:198–201. doi: 10.1159/000322941. [DOI] [PubMed] [Google Scholar]
- 4.Kumar R, Kalra SP, Kumar H, Anand AC, Madan H. Pancytopenia – A six year study. J Assoc Physicians India. 2001;49:1078–81. [PubMed] [Google Scholar]
- 5.Santra G, Das BK. A cross-sectional study of the clinical profile and aetiological spectrum of pancytopenia in a tertiary care centre. Singapore Med J. 2010;51:806–12. [PubMed] [Google Scholar]
- 6.Hamid GA, Shukry SA. Patterns of pancytopenia in Yemen. Turk J Hematol. 2008;25:71–4. [PubMed] [Google Scholar]
- 7.Retief FP, Heyns AD. Pancytopenia and aplastic anemia: A retrospective study. S Afr Med J. 1976;50:1318–22. [PubMed] [Google Scholar]
- 8.Tilak V, Jain R. Pancytopenia – A clinico-hematologic analysis of 77 cases. Indian J Pathol Microbiol. 1999;42:399–404. [PubMed] [Google Scholar]
- 9.Hauswirth AW, Skrabs C, Schützinger C, Gaiger A, Lechner K, Jäger U. Autoimmune hemolytic anemias, Evans' syndromes, and pure red cell aplasia in non-Hodgkin lymphomas. Leuk Lymphoma. 2007;48:1139–49. doi: 10.1080/10428190701385173. [DOI] [PubMed] [Google Scholar]
- 10.Jha A, Sayami G, Adhikari RC, Panta AD, Jha R. Bone marrow examination in cases of pancytopenia. JNMA J Nepal Med Assoc. 2008;47:12–7. [PubMed] [Google Scholar]
- 11.Zent CS, Kay NE. Autoimmune complications in chronic lymphocytic leukaemia (CLL) Best Pract Res Clin Haematol. 2010;23:47–59. doi: 10.1016/j.beha.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrett AJ, Sloand E. Autoimmune mechanisms in the pathophysiology of myelodysplastic syndromes and their clinical relevance. Haematologica. 2009;94:449–51. doi: 10.3324/haematol.2009.006080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarin SK, Kumar A. Noncirrhotic portal hypertension. Clin Liver Dis. 2006;10:627–51, x. doi: 10.1016/j.cld.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 14.Klco JM, Geng B, Brunt EM, Hassan A, Nguyen TD, Kreisel FH, et al. Bone marrow biopsy in patients with hepatitis C virus infection: Spectrum of findings and diagnostic utility. Am J Hematol. 2010;85:106–10. doi: 10.1002/ajh.21600. [DOI] [PubMed] [Google Scholar]
- 15.Choi YS, Suh JP, Song KH, Lee JB, Lee DS, Lee IT, et al. A case of Crohn's disease with improvement after azathioprine-induced pancytopenia. Case Rep Gastroenterol. 2011;5:344–9. doi: 10.1159/000329707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuen KY, Chan PK, Peiris M, Tsang DN, Que TL, Shortridge KF, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998;351:467–71. doi: 10.1016/s0140-6736(98)01182-9. [DOI] [PubMed] [Google Scholar]
- 17.Ebert EC, Kierson M, Hagspiel KD. Gastrointestinal and hepatic manifestations of sarcoidosis. Am J Gastroenterol. 2008;103:3184–92. doi: 10.1111/j.1572-0241.2008.02202.x. [DOI] [PubMed] [Google Scholar]
- 18.Goldschmidt N, Gural A, Kornberg A, Spectre G, Shopen A, Paltiel O. Prolonged fever of unknown origin and hemophagocytosis evolving into acute lymphoblastic leukemia. Am J Hematol. 2004;76:364–7. doi: 10.1002/ajh.20123. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe H, Hirase N, Goda H, Nishikawa H, Ikuyama S. Oral low-dose tacrolimus therapy for refractory hemophagocytic syndrome associated with systemic lupus erythematosus. Mod Rheumatol. 2012;22:284–9. doi: 10.1007/s10165-011-0491-y. [DOI] [PubMed] [Google Scholar]
- 20.Eser B, Altuntas F, Soyuer I, Er O, Canoz O, Coskun HS, et al. Acute lymphoblastic leukemia associated with brucellosis in two patients with fever and pancytopenia. Yonsei Med J. 2006;47:741–4. doi: 10.3349/ymj.2006.47.5.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yokuþ O, Gedik H. A case with pancytopenia and autoimmune hemolytic anemia due to Vitamin B12 deficiency. J Blood Disord Transfus. 2015;S5:002. [Google Scholar]
- 22.Sari I, Altuntas F, Hacioglu S, Kocyigit I, Sevinc A, Sacar S, et al. A multicenter retrospective study defining the clinical and hematological manifestations of brucellosis and pancytopenia in a large series: Hematological malignancies, the unusual cause of pancytopenia in patients with brucellosis. Am J Hematol. 2008;83:334–9. doi: 10.1002/ajh.21098. [DOI] [PubMed] [Google Scholar]
- 23.Mert A, Ozaras R, Tabak F, Bilir M, Ozturk R, Aktuglu Y. Malaria in Turkey: A review of 33 cases. Eur J Epidemiol. 2003;18:579–82. doi: 10.1023/a:1024648902848. [DOI] [PubMed] [Google Scholar]