Abstract
Introduction:
Despite the major improvements in surgical technique and perioperative care, radical cystectomy (RC) remains a major operative procedure with a significant morbidity and mortality. The present study analyzes the early complications of RC and urinary diversion using a standardized reporting system.
Materials and Methods:
Modified Clavien-Dindo classification was used to retrospectively assess the peri-operative course of 212 patients who had RC with urinary diversion between October 2003 and October 2014 at a single institution. The indications for surgery were muscle invasive urothelial carcinoma, high-grade nonmuscle invasive bladder cancer (BC), and Bacillus Calmette–Guerin-resistant nonmuscle invasive BCs. Data on age, sex, comorbidities, smoking history, American Society of Anaesthesiologists score, and peri-operative complications (up to 90 days) were captured. Statistical analysis was performed using SPSS 20.0 software (Chicago, USA).
Results:
The mean age was 56.15 ± 10.82. Orthotopic neobladder was created in 113 patients, ileal conduit in 88 patients, and cutaneous ureterostomy in 11 patients. A total of 292 complications were recorded in 136/212 patients. 242 complications (81.16%) occurred in the first 30 days, with the remaining 50 complications (18.83%) occurring thereafter. The rates for overall complication were 64.1%. The most common complications were hematologic (21.6%). Most of the complications were of Grade I and II (22.9% and 48.9%, respectively). Grade IIIa, IIIb, IVa, IVb, and V complications were observed in 10.2%, 8.9%, 3.4%, 2.7%, and 2.7% of the patients, respectively.
Conclusions:
RC and urinary diversion are associated with significant morbidity. This audit would help in setting a benchmark for further improvement in the outcome.
Key words: Bladder cancer, Clavien-Dindo classification, complication, cystectomy, urinary diversion
INTRODUCTION
The standard management for muscle invasive and high-risk nonmuscle invasive bladder cancer (BC) is radical cystectomy (RC) and urinary diversion.[1,2] Despite the significant improvements in surgical techniques and peri-operative care, RC remains a major operative procedure with significant morbidity and mortality varying between 30%–70% and 0.3%xyn5.7%, respectively.[3] Most earlier studies have categorized procedural morbidities into major and minor complications without considering the comorbidities and employing standardized reporting system of complications.[4,5] This makes it difficult to compare the data and may underestimate the morbidity. One of the major confounding factors is the type of diversion, which could adversely affect the rate of complications if not factored.[1] The Clavien classification system for surgical complications was originally developed in 1992[6] and modified by Dindo et al. in 2004.[7] This classification system has gained a wide acceptance in urology. Our patients are nutritionally challenged and present in advanced stage of disease. At present, there are insufficient data on standardized reporting of complications following RC.[8] The aim of this study is to present the audit of complications using a standardized reporting system of Clavien-Dindo.
MATERIALS AND METHODS
Data on RC performed between October 2003 and October 2014 were collected from the hospital information system and internal data management source of our institute. Of the 239 patients who underwent RC over this period, complete data could be retrieved for 212 patients, of whom orthotopic neobladder (ONB) was done in 113 patients, ileal conduit (IC) in 88, and cutaneous ureterostomy (CU) in 11 patients. The indications for surgery were muscle invasive urothelial carcinoma, high-grade nonmuscle invasive BC, and Bacillus Calmette-Guerin-resistant nonmuscle invasive BCs. Data on age, sex, comorbidities, smoking history, body mass index (BMI), American Society of Anaesthesiologists (ASA) score, and details of urinary diversion were recorded. Pre- and post-operative hematological investigations and serum chemistries were also recorded. Clinical and pathological stages were evaluated for all the patients according to the tumor node metastasis 2010 staging system.[9]
Polyethylene glycol solution was routinely administered a day before the surgery for bowel preparation. Deep vein thrombosis prophylaxis as elastic compressive stocking was used in all the patients, but low molecular weight heparin was administered in selected patients only. All RCs were done with open approach, and standard steps of surgery were followed. Lymphadenectomy was done up to the bifurcation of the aorta. Ileal ONB was made according to the Studer technique.[10,11,12] All uretero-intestinal and uretero-cutaneous anastomosis were stented regardless of the form of urinary diversion for at least 21 days.
Patients were followed up after surgery at 1 month, then 3 monthly for 2 years, and 6 monthly thereafter. All early complications within 90 days of surgery were recorded and classified into five grades according to the modified Clavien-Dindo classification system.[7]
Statistical analysis was performed using the SPSS 20.0 software (Chicago, USA). For continuous data, normality was tested using Kolmogorov-Smirnov test. One-way ANOVA was used to compare the means among independent groups when data were found normal. Fisher's exact test and Chi-square-test were used to test the difference in proportions, as appropriate, and P < 0.05 was considered statistically significant.
RESULTS
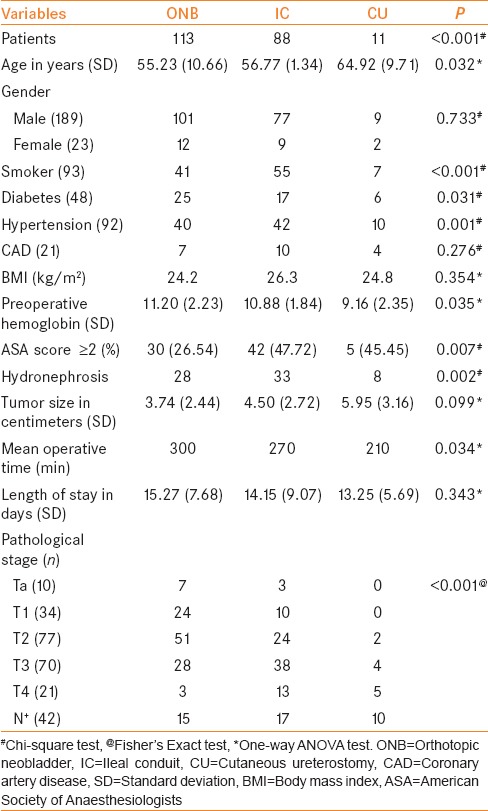
A total of 212 patients underwent RC and urinary diversion with a mean age of 56.15 ± 10.82 years. Majority of the patients were male (189/212). Diabetes mellitus, hypertension, and coronary artery disease were the major comorbidities in 48, 92, and 21 patients, respectively [Table 1]. The mean BMI was 25.1 kg/m2 (22.2–29.9) and the percentage of patients with an ASA ≥2 was 36.32%. ONB was done in 113 patients, IC in 88, and CU in 11 patients. Patients with CU presented with a higher rate of comorbidities as compared to that of IC and ONB. Median operating time was 300 min (150–418 min) and intraoperative blood loss was 700 ml (400-1100 ml). IC and ONB required a significantly (P < 0.05) longer operative time (270 and 300 min) as compared to CU (210 min). The overall length of hospital stay (LOS) was 14.76 ± 7.71 days (range: 7–35 days).
Table 1.
Patient demographics and characteristics according to the different types of urinary diversions
Mean tumor size was 4.297 ± 2.77 cm. Mean number of lymph nodes removed was 10.92 ± 8.13. Majority of the tumors were T2 stage (77/212). Overall, 42 patients (19.81%) had pathological N+ disease. Advanced disease (pT3–4) was more frequent in patients who received a CU (81.81%). Patients with ONB were more likely to have a lower tumor stage (T2 or less) (72.56%) as compared to IC and CU (42.04% and 18.18%, respectively). In six patients, nephroureterectomy (right side – 4, left side – 2) was done in addition to RC. Four patients had urinary diversion by CU while two patients had IC. In all the six patients, there was extension of bladder growth into the terminal ureter with proximal gross hydronephrosis and thinning of the renal parenchyma. The mean split function of the hydronephrotic kidneys was 9.6% ± 2.9%.
A total of 292 complications were recorded in 136/212 (64.1%) patients. 242 complications (81.1%) occurred in the first 30 days, with the remaining 50 complications (18.8%) occurring between 31 and 90 days postoperatively. The majority of complications (210/292, 71.9%) were classified as low-grade with 22.9% in Grade I and 48.9% in Grade II. High-grade (Clavien-Dindo Grade III-V) complications were seen in 82/292 (28%) patients. Grade IIIa, IIIb, IVa, IVb, and V complications were observed in 10.2%, 8.9%, 3.4%, 2.7% and 2.7% of the patients, respectively [Table 2]. Suffix I was used for intraoperative complication as rectal injury and ureteral injury in four patients. All these complications were categorized as Grade IIIb (I). The overall mortality rate within the first 90 days after surgery was 3.7% (8/212). High-grade complications were less in CU as compared to IC and ONB [Table 3]. When comparing all the three types of urinary diversion for complication rates, the result was statistically insignificant (P = 0.211), so was between ONB and IC (P = 0.294). The mean preoperative hemoglobin was 10.9 g/dL while the mean postoperative hemoglobin was 8.6 g/dL. The mean preoperative serum creatinine was 1.25 mg/dL and mean preoperative estimated glomerular filtration rate (eGFR) was 76 ml/min. Of the 212 patients, 32 (15.1%) had preoperative serum creatinine >1.5 mg/dL. Of them, 21/212 patients (9.9%) presented with gross hematuria and acute kidney injury. All these were managed with urgent bilateral percutaneous nephrostomies, following which there was postobstructive diuresis. Two patients required hemodialysis in acute setting. Among the patients with serum creatinine >1.5 mg/dL and eGFR <60 mL/min (established chronic kidney disease III; n = 13/212 or 6.1%), ten patients underwent IC and three patients underwent CU. The mean preoperative eGFR in these patients was 34.5 ml/min. The overall mean postoperative serum creatinine was 1.21 mg/dL. The mean preoperative albumin for the entire study group was 3.9 g/dL. Among the 136 out of 212 patients who developed complications, the mean preoperative albumin was 3.2 g/dL while for those without complications (n = 76), the mean albumin was 4.1 g/dL.
Table 2.
Complications of radical cystectomy classified according to the modified Clavien-Dindo system
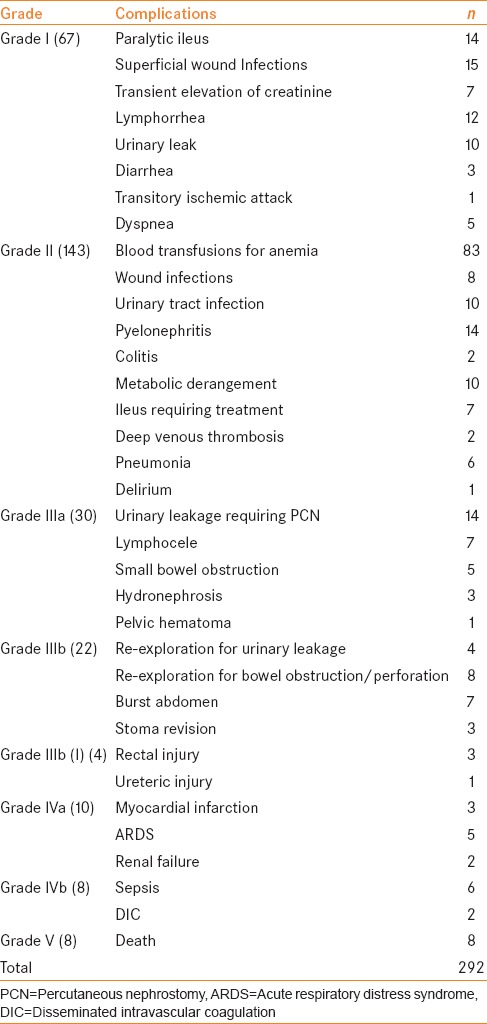
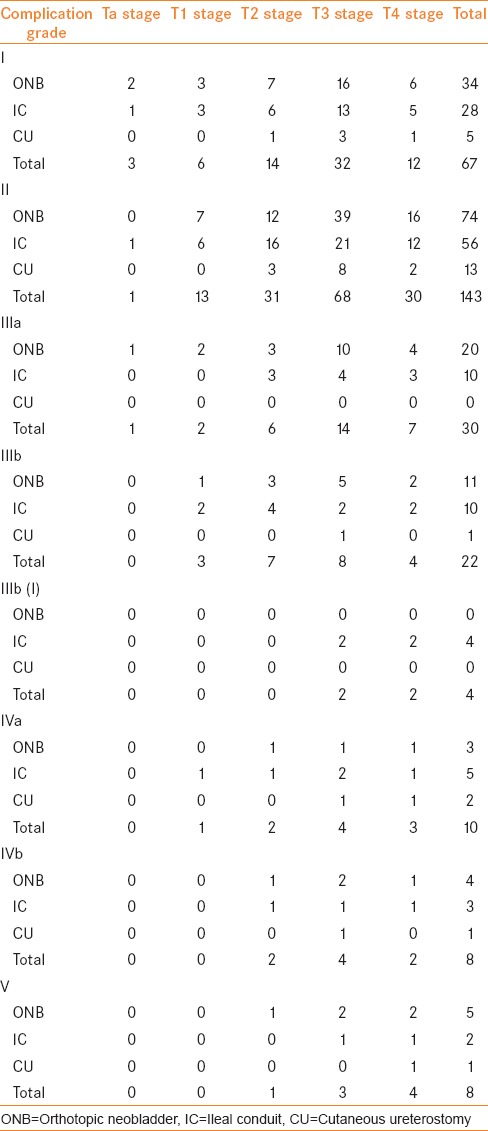
Table 3.
Complications of radical cystectomy according to tumor stage and type of urinary diversion
Hematologic complications (83/292 or 28.4%) were the most common followed by infectious complications (54/292 or 18.4%), gastrointestinal (GI) complications (53/292 or 18.1%), genitourinary complications (45/292 or 15.4%), and pulmonary complications (22/292 or 7.5%). Anemia was the most common hematological complication. Minor wound infection represented 43.4% of the infectious complications. GI complications mostly consisted of ileus or small bowel obstruction (51%), with re-exploration required in 19.6% of the patients.
Forty patients required interventions under general or local anesthesia for the management of high-grade (≥III) complications. 14 patients underwent percutaneous nephrostomy for ureteroileal or vesicourethral anastomotic leak, whereas four patients had percutaneous drainage for lymphocele or pelvic collection. Re-exploration for intestinal obstruction, perforation, or urinary anastomotic leak was done in 12 and stoma revision was done in three patients. Seven patients needed repair for burst abdomen.
DISCUSSION
RC and urinary diversion are the standard of care treatments for muscle invasive or high-risk nonmuscle invasive BC.[1,2] RC and urinary diversion are associated with high rates of complications.[13] With time, surgical technique and perioperative management have improved, but open RC and urinary diversion have not seen a parallel improvement in the outcome in terms of peri-operative morbidity.[3]
There is a significant disparity in reporting the complications of this procedure, and no universally accepted grading system was available for a long time.[14] Martin et al. proposed a new methodology to improve the quality of reporting surgical complications to reduce the risk of variability, heterogeneity, and underestimation of morbidity.[15] Since then, various efforts have been made to standardize the reporting of surgical complications.[16,17,18] The spectrum of BC patients in India is different from the rest of the developed countries. Our patients present in advanced stage of the disease and are nutritional-challenged. There is no data published on the complications of RC in the standardized format.
Our overall complication rates were higher than the data reported in Western literature.[5,16,17,19,20] In the present series, majority of the complications were of low grade as rarely we see a patient having cystectomy with hemoglobin of more than 10 g%. High-grade complications have been reported as 21.8% and 20.72% in these series.[16,17] In the present study, 28% of our patients had high-grade complications (Grade III–V) [Table 2]. This difference may be due to the type of urinary diversion used. Neo bladder formation is technically more complex, challenging, and theoretically more likely to have procedure-related and infectious complications. In the present study, 53.30% patients had ONB as urinary diversion, which is greater than the series with lower percentage of high-grade complications (34.76% and 24.14%).[16,17]
Grade IIIa complications in the present study were comparable to De Nunzio et al.[17] (9.63%), but their Grade IIIb complications (4.71%) were lower than that reported in the present series. The reasons could be two-fold. First, we have reported intraoperative injuries to the surrounding structures in 4 cases and graded them as Grade IIIb with a suffix I (intraoperative). Out of these 4 patients, 3 had rectal injury and 1 had ureteric injury. This was not reported in any of the previous studies, although it was suggested to use suffix I for any intraoperative complication in the modification of Clavien-Dindo classification system.[21] Second, all repairs for fascial dehiscence were performed under anesthesia as compared to bedside wound management which resulted in the increase in the number of higher grade complications in our series. Thus, management strategy can influence the grading of complications too. In the present study, overall mortality rate was 3.77% (8/212), which was comparable to other studies. Four patients had pneumonia and acute respiratory distress syndrome with subsequent respiratory failure and two patients had small bowel obstruction and perforation with resulting sepsis (one of these had massive small bowel gangrene following internal herniation while the other had adhesive intestinal obstruction and perforation with late presentation). One patient had myocardial infarction in the postoperative period while another patient developed urinary leak and infected ascites with resulting sepsis.
The most common complications in the present study were hematologic (28.42%), followed by infectious complications (18.49%), GI complications (18.15%), genitourinary complications (15.41%), and pulmonary complications (7.5%). As in most of our patients, hemoglobin levels were around 9 or 10 g% at the beginning of the surgery, blood transfusion was needed in most of the patients, and that is the reason that hematologic complications were the most common. Ileus and small bowel obstruction (51%) were the most common GI complications requiring re-exploration in 19.60% of the patients. The likely reason could be inconsistency in the surgical prudence of floating population of residents as anastomosis was handsewn. Since the use of staplers, we observed a decreasing trend in GI complications.
On comparison of all the three types of diversion, we found that patients with ONB were younger than patients with IC or CU [Table 1]. Patients with CU had a higher incidence of comorbidities and hydronephrosis when compared to patients receiving ONB or IC. Most of these cases were operated as a palliative procedure to decrease the comorbidities of GI complications. Patients with ONB were more likely to experience genitourinary and infectious complications as compared to patients with IC. Similarly, Stimson et al.[22] also reported a higher rate of reflux pyelonephritis in ONB recipients.
There was no difference in blood transfusion rate in all the three types of urinary diversion. When compared for tumor stage, majority of the complications (135/292) occurred in T3 stage [Table 3]. This is partly because a significant proportion of the patients belonged to that stage (70/212). However, considering the average number of Clavien-Dindo complications per patient, the highest ratio was seen in T4 stage (3.04 complications per patient). Further, 26% (35/135) of the complications in T3 tumors and 34% (22/64) of the complications in T4 tumors were high grade, which also indicate a propensity for higher grade complications in T4 tumors.
In our study, the overall LOS was 14.76 ± 7.71 days. The LOS was significantly longer in patients with high-grade complications. On comparison of the different types of urinary diversions, CU had shorter LOS (13.25 ± 5.69) than ONB (15.27 ± 7.68) and IC (14.15 ± 9.07). This might be due to less GI morbidity and lack of multiple anastomosis. The relationship between hospital volume and RC outcome in terms of morbidity and mortality is well established.[23] We have performed 212 RC in 11 years with a mean of 19.27 RC per year. Some authors suggested fifty procedures per year as the desirable cystectomy rate, but the International Consultation on BC has proposed an annual rate of ten procedures per hospital as an adequate rate. Experience and volume help in standardizing each and every step of the procedure, which could help in minimizing Grade III and higher complications.
This study has a few limitations. Since this is a retrospective study, a risk of overlooking or missing the complications is likely to exist though we have tried to extract the entire patient information through hospital information system, patient files, and follow-up records. The present study was focused on the categorization of early complications of RC and we have not assessed any predictive factors for complications. Despite these shortcomings, an audit of complications would help counsel the patients and improve the outcome by paying more attention on surgical techniques to bring down the number of Grade III-V complications.
CONCLUSIONS
Early complications of RC and urinary diversion based on Clavien-Dindo classification are a significant health problem affecting the overall outcome of this procedure. Although most of the complications were categorized as low grade, the 28% of the high-grade complications pose a significant challenge to improve the technique and peri-operative management. This audit would help in setting a benchmark for improving the outcome of RC and urinary diversion in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hautmann RE, Abol-Enein H, Hafez K, Haro I, Mansson W, Mills RD. Urinary diversion. Urology. 2007;69(1 Suppl):17–49. doi: 10.1016/j.urology.2006.05.058. [DOI] [PubMed] [Google Scholar]
- 2.Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: Long-term results in 1,054 patients. J Clin Oncol. 2001;19:666–75. doi: 10.1200/JCO.2001.19.3.666. [DOI] [PubMed] [Google Scholar]
- 3.Liedberg F. Early complications and morbidity of radical cystectomy. Eur Urol Suppl. 2010 Apr 30;9(1):25–30. [Google Scholar]
- 4.Chang SS, Cookson MS, Baumgartner RG, Wells N, Smith JA., Jr Analysis of early complications after radical cystectomy: Results of a collaborative care pathway. J Urol. 2002;167:2012–6. [PubMed] [Google Scholar]
- 5.Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, Savage C, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol. 2009;55:164–74. doi: 10.1016/j.eururo.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- 7.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng CK, Kauffman EC, Lee MM, Otto BJ, Portnoff A, Ehrlich JR, et al. A comparison of postoperative complications in open versus robotic cystectomy. Eur Urol. 2010;57:274–81. doi: 10.1016/j.eururo.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010. [Google Scholar]
- 10.De Nunzio C, Cicione A, Leonardo F, Rondoni M, Franco G, Cantiani A, et al. Extraperitoneal radical cystectomy and ureterocutaneostomy in octogenarians. Int Urol Nephrol. 2011;43:663–7. doi: 10.1007/s11255-010-9876-7. [DOI] [PubMed] [Google Scholar]
- 11.Glenn JF, Alyea EP. Ureterocutaneous anastomosis. I. Experimental use of a surgical splint to prevent stricture. Trans Southeast Sect Am Urol Assoc. 1960;1959:36–9. [PubMed] [Google Scholar]
- 12.Dahl DM, McDougal WS. Use of intestinal segments in urinary diversion. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell Walsh Urology. 9th ed. Philadelphia: WB Saunders Co; 2006. pp. 2534–78. Sec. 15, Ch. 6. [Google Scholar]
- 13.Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH, Holm HV, et al. ICUD-EAU international consultation on bladder cancer 2012: Urinary diversion. Eur Urol. 2013;63:67–80. doi: 10.1016/j.eururo.2012.08.050. [DOI] [PubMed] [Google Scholar]
- 14.Donat SM, Siegrist T, Cronin A, Savage C, Milowsky MI, Herr HW. Radical cystectomy in octogenarians – Does morbidity outweigh the potential survival benefits? J Urol. 2010;183:2171–7. doi: 10.1016/j.juro.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–13. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roghmann F, Trinh QD, Braun K, von Bodman C, Brock M, Noldus J, et al. Standardized assessment of complications in a contemporary series of European patients undergoing radical cystectomy. Int J Urol. 2014;21:143–9. doi: 10.1111/iju.12232. [DOI] [PubMed] [Google Scholar]
- 17.De Nunzio C, Cindolo L, Leonardo C, Antonelli A, Ceruti C, Franco G, et al. Analysis of radical cystectomy and urinary diversion complications with the Clavien classification system in an Italian real life cohort. Eur J Surg Oncol. 2013;39:792–8. doi: 10.1016/j.ejso.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Yuh BE, Nazmy M, Ruel NH, Jankowski JT, Menchaca AR, Torrey RR, et al. Standardized analysis of frequency and severity of complications after robot-assisted radical cystectomy. Eur Urol. 2012;62:806–13. doi: 10.1016/j.eururo.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Novara G, De Marco V, Aragona M, Boscolo-Berto R, Cavalleri S, Artibani W, et al. Complications and mortality after radical cystectomy for bladder transitional cell cancer. J Urol. 2009;182:914–21. doi: 10.1016/j.juro.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 20.Schiavina R, Borghesi M, Guidi M, Vagnoni V, Zukerman Z, Pultrone C, et al. Perioperative complications and mortality after radical cystectomy when using a standardized reporting methodology. Clin Genitourin Cancer. 2013;11:189–97. doi: 10.1016/j.clgc.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Myatt A, Palit V, Burgess N, Biyani CS, Joyce AD. The Uro-Clavien-Dindo system – Will the limitations of the Clavien-Dindo system for grading complications of urological surgery allow modification of the classification to encourage national adoption within the UK? British J Med Surg Urol. 2012;5:54–60. [Google Scholar]
- 22.Stimson CJ, Chang SS, Barocas DA, Humphrey JE, Patel SG, Clark PE, et al. Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. J Urol. 2010;184:1296–300. doi: 10.1016/j.juro.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Hautmann RE, de Petriconi RC, Volkmer BG. Lessons learned from 1,000 neobladders: The 90-day complication rate. J Urol. 2010;184:990–4. doi: 10.1016/j.juro.2010.05.037. [DOI] [PubMed] [Google Scholar]


