Abstract
Objective
To investigate long‐term suicide risk in individuals with no, one or more mental disorders.
Method
In the Lundby Study, involving a total population of 3563 subjects, mental health and suicide risk were monitored over 54–64 years.
Results
The long‐term suicide risk in subjects with no, one, or more mental disorders was 0.3%, 3.4% and 6.2% respectively. For individuals with only depression, the risk was 6.0%, only alcohol use disorder 4.7%, and only psychosis 3.1%. However, when individuals had additional disorders, the suicide risks were 6.6%, 9.4% and 10.4% respectively. Each diagnosis per se was significantly related to increased risk of suicide. Men had a higher suicide risk in depression than women. Men who had alcohol use disorder in addition to depression showed a very high risk of suicide, 16.2%.
Conclusion
Long‐term suicide risk was increased for depression, alcohol use disorder, and psychosis per se. For the latter two the diagnosis alone there may be a lower risk than previously estimated when there is no additional diagnosis. In men, depression in addition to alcohol use disorder should be treated vigorously in the work to prevent suicide.
Keywords: suicide risk, long‐term course, depression, alcohol use disorder, psychosis
Significant outcomes.
In a long‐term perspective, among men with alcohol use disorder and depression there was a very high risk of suicide (16.2%).
For depression, alcohol use disorders, and psychosis per se, there was an increased risk of suicide in the long‐term course.
The very long‐term risk of suicide for alcohol use disorders and psychosis (but not depression) appeared to be smaller than previously estimated for one diagnosis, when additional diagnoses are excluded.
Limitations.
Limited sample of suicides, especially for women.
Change of diagnostic procedures over time, an inherent problem in all long‐term studies.
Recall periods were of considerable length, 10, 15 and 25 years.
Introduction
Mental disorders are associated with an increased risk of all‐cause mortality and suicide, as has recently been confirmed in a meta‐review 1. Suicide mortality, borderline personality disorder, depression, bipolar disorder, opioid use and schizophrenia, as well as anorexia nervosa and alcohol use disorder in women, were associated with substantially increased rates (more than ten times greater) compared with the general population. The authors have found no review on mortality in dual diagnoses.
In a meta‐analysis of follow‐up mortality studies, the lifetime suicide risk, was estimated to be 6% in affective disorders, 7% in alcohol dependence, and 4% in schizophrenia 2. Two other studies showed the overall suicide risk in general populations to be 2.4% in affective disorder and 3.5% in depressive disorder 3, 4. One study reported about 2.0% lifetime suicide risk in untreated alcoholics and 3.4% suicide risk in hospital admitted persons with alcoholism 5. Meta‐analyses have estimated that about 5% of all persons with schizophrenia will commit suicide during their lifetime 6, 7. Suicide risk in individuals with anxiety disorders has been studied in a clinical sample in a long‐term course and found to be 1.9% for anxiety neurosis 8. Another study following male conscripts for 13 years 9 showed suicide rates of 1.1% for neurotic disorders.
Apart from a high risk of suicide in specific mental disorders, comorbid disorders have been shown to increase the risk. A study by Nordentoft et al. 10 showed that, in all diagnostic groups, comorbidity with substance abuse disorder increased the cumulative incidence of suicide, except among men with schizophrenia. Comorbid affective disorder also increased the cumulative risk of suicide for all mental disorders according to that study.
Retrospective case–control studies have also shown that comorbidity of mental disorders is a risk factor for suicide. An important comorbidity associated with increased risk of suicide is depression/mood disorder combined with alcohol/substance use disorders 11, 12, 13, 14. A higher suicide risk has been reported in persons with schizophrenia who have depressive symptoms or depression 7, 15 and, in a meta‐analysis, previous depression in schizophrenia was estimated to increase the suicide risk 16. However, a study of hospitalized patients with psychosis and comorbid substance use disorder did not show an increased suicide risk 17.
Finally, psychological autopsies of suicide victims have shown mental disorders in around 90% of cases and additional comorbid diagnoses have been common 18, 19, 20, 21, 22, 23. In a review, only 0.1% of suicide victims in a psychiatric inpatient population and 3.2% of the general population had no established psychiatric diagnosis 24.
In the Lundby Study, we were able to follow a general population – including both persons with and without mental disorders – prospectively. Long‐term suicide risk for specific diagnoses in the Lundby population has previously been presented and was found to be 5.6% for depression 25, 6.3% for alcohol use disorders 26, 9% for psychosis 27 and 3.3% for anxiety disorders 28.
In summary, although additional disorders are frequently found among suicide victims, the impact of additional diagnoses on lifetime/long‐term risk (the proportion of a sample who eventually committed suicide) has, to the best of our knowledge, not been investigated.
Aims of the study
The aim of the present study was to estimate very long‐term suicide risk in no, one or more mental disorders (simultaneously or at different times) during the lifespan, gender considered.
Material and methods
The prospective epidemiological investigation called the Lundby Study was started in 1947 by Essen‐Möller and his collaborators with the idea of describing the mental health and personality traits in the general population in a geographically defined rural area near Lund, a city in the southern part of Sweden 29. The investigators studied all inhabitants, regardless of age. Field investigations were based on interviews by psychiatrists (a semi‐structured part and a free part), in which the subjects were asked about their life and health situation as well as other experiences. The descriptions and the diagnostic considerations were all carried out by psychiatrists.
At the start, the sample consisted of 2550 persons. In a follow‐up carried out in 1957, 1013 new inhabitants who had either moved into the area or who had been born after 1947 entered the study. This makes two overlapping cohorts. A total of 3563 individuals were included in the Lundby Study (Fig. 1). Surviving subjects were asked to participate again in 1957, 1972 and 1997. The field investigators travelled to visit persons who had moved from the area or, if that was not possible, conducted the interview by telephone, so persons who had moved were also included in the study. The interviews were supplemented by information from key informants (e.g. the family members, clerics, district medical, teachers, foremen), and external sources such as hospital case notes, a register of social insurance data, as well as diagnoses from inpatient registers 30 and local outpatient registers clinics in the County Temperance Board and the Cause of Death Register. The kind of registers available varied in the different field investigations. In 1972, some new diagnostic schedules were introduced and, in 1997, supplementary self‐rating questionnaires were introduced 31.
Figure 1.
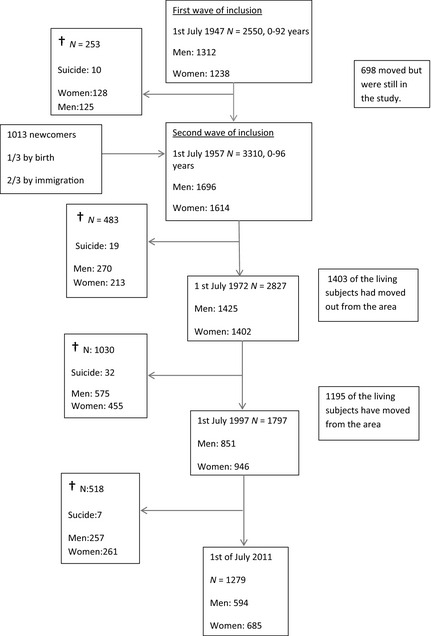
The Lundby population – inclusion, deaths and attrition during the follow‐up 1947–1997 . †Dead.
As shown in Fig. 1, the attrition rate increased with time but, on the whole, participation was very satisfactory. During the follow‐up period that ended in 1997, 1766 individuals died. For persons who had died since the latest field investigation, the researchers were able to find follow‐up information regarding the person's health and life events between the final interview and death; this information was obtained from key informants and various registers, and by studying death certificates, the Cause of Death Register [Epidemiological Centre, National Board of Health and Welfare 30], and autopsy reports. If no interview was possible at follow‐up, information from at least two of the other sources mentioned above was required for inclusion in the follow‐up. Where there was insufficient information for inclusion in the follow‐up, the subject was regarded as dropped out from the study. For the entire 50‐year period, the dropout rate was 5.6% (198/3563) when all sources of information were used. Between the field investigations in 1947 and 1972, the attrition rate was about 1%, and between 1972 and 1997, it was about 6%. In 1997, the dropout rate (refusal or insufficient information about the subject) was 8.7% among living subjects and 5.9% when both living and dead subjects were included. These figures are low according to common standards 32.
In the last field investigation, in 1997, the area had developed from rural to mainly suburban, but agriculture still took place. Most of the subjects lived in small villages with less than 10 000 inhabitants.
Diagnostics
In 1947 and 1957, there was no established diagnostic system suitable for a field study of a general population. Professor Essen‐Möller made his own ‘Lundby diagnostic system’, which was further developed in 1957 together with co‐investigator Hagnell. This system included most disorders in a main group called ‘Diagnosis I’ which was meant to represent acquired disorders with a perceptible onset and mostly termination. The main classes in this system were ‘organic brain disorders’, ‘psychoses’ and ‘neuroses’ 31. The main classes can be further divided into main categories such as ‘dementia’, ‘schizophrenia’, ‘depression’ and ‘anxiety’, and then to even more specific subcategories. This is a hierarchical system allowing only one diagnosis per episode; for example, dementia rules out psychosis. For the class ‘neuroses’, the researchers also devised subcategories for comorbid psychiatric symptoms, such as ‘depression + other psychiatric symptoms’. Habitual conditions rooted in personality, alcohol problems and psychosomatic complaints were also included in this group. In the Lundby classification, a subject could be given two ‘Diagnosis II’ or one ‘Diagnosis I’ and one ‘Diagnosis II’ in the same period of time.
In this study, the main Lundby categories are used. The diagnoses are organic brain disorder, psychosis, depression, anxiety disorder, alcohol use disorder (‘Diagnosis II’ as described above). The remaining ‘diagnoses I’ are put together in ‘other psychiatric disorders’. In the field investigation in 1997, diagnoses according to Lundby, DSM‐IV 33 and International Classification of Diseases (ICD)‐10 34 were assessed. This re‐evaluation included most first episodes of neurotic disorders 1947–1957, and all episodes were evaluated during the period 1972–1997.
In this study, the diagnoses will be mentioned in the hierarchal order of the Lundby system.
Degree of impairment
The functional impairments of the mental disorder episodes were estimated according to Leighton, who defined five levels: (i) minimal, (ii) mild, (iii) medium, (iv) severe and (v) very severe impairment 35. Medium impairment (number 3) or higher has previously been used as a criterion for mental illness or ‘caseness’ in subjects with a Lundby diagnosis 31, 36. This corresponds to a GAF score between 60 and 51 or less 33.
Organic brain disorder
‘Organic brain disorder’ represents disorders with clearly disturbed cognitive functions or a clear deterioration of personality or behaviour in which the aetiology is unquestionably organic. This is divided into the main category ‘dementia’ with its subcategories ‘vascular/multi‐infarct dementia’ and ‘senile dementia’ and the main category ‘organic syndrome’, which represents conditions not reaching the dementia threshold and other organic brain disorders due to, for example, medical conditions, injury or illegal drugs.
Psychosis
According to the Lundby Study, ‘psychotic disorder’ consists of ‘schizophrenia’ and ‘other psychosis’. When the Lundby diagnoses were re‐diagnosed according to DSM‐IV in 1997, the latter group included other non‐affective psychosis, psychotic disorder due to a general medical condition (including delirium/confusion), substance‐induced psychosis and manic conditions 37.
Depression
The Lundby diagnosis ‘depression’ has two subcategories: ‘depression proper’ and ‘depression +’, which means ‘with other psychiatric symptoms’, such as anxiety, obsessive or psychotic symptoms. Subjects with ‘depression with psychotic symptoms’ were included in the ‘depression’ group, following the DSM‐IV main classification of ‘mood disorders’ and the original Lundby classification of ‘depression +’. In the majority of cases, the depression group could be approximated to major depression in DSM‐IV if the medium and severe degree of impairment was used to select cases. However, subjects sometimes better fulfilled the criteria for other DSM‐IV diagnoses with depressive symptoms, such as dysthymia, depression NOS, bipolar depression, depression due to general medical condition or substance‐induced depression. (There were 12 cases of bipolar disorder in the Lundby Study.) In some cases, the DSM diagnosis corresponding to Lundby diagnosis was not included in the DSM‐IV mood disorders, for example adjustment disorder and somatoform disorder with depressive features.
Anxiety
‘Anxiety’ was subdivided into ‘anxiety proper’ and ‘anxiety + other psychiatric symptoms’ (in which anxiety should always be the predominant symptom). In the DSM‐IV evaluation, the main category ‘anxiety’ corresponded to disorders such as panic disorder, generalized anxiety disorder, phobias, anxiety NOS and some other disorders in which anxiety may be prominent such as obsessive compulsive disorder, somatoform disorder and adjustment disorder.
Other psychiatric disorders
The remaining group, which we call ‘other psychiatric disorders’ in this study, represents the Lundby diagnoses ‘Tiredness’ and ‘Mixed neurosis’. The group is heterogeneous and includes persons whose diagnoses according to DSM‐IV could be classified as ‘chronic fatigue syndrome’, ‘social phobia and somatoform/somatization disorder’, ‘adjustment disorders’, ‘phobias’, ‘sleep disorders’ and ‘anorexia nervosa’.
Alcohol use disorder
Alcohol problems in the Lundby Study were categorized as ‘alcoholism’ in the main group ‘Diagnosis II’ and are similar to the DSM‐IV criteria for alcohol abuse. ‘Alcohol dependence’ was defined by DSM‐IV criteria, with a maladaptive pattern of alcohol use, leading to clinically significant impairment or distress, as manifested by at least three of seven criteria occurring at any time during a 12‐month period. A subject was assessed as a case of the broader category ‘alcohol use disorder’, if he or she met the criteria for ‘alcohol problems’ or ‘alcohol dependence’, at any time between 1947 and 1997. In addition, an estimated duration of disorder of at least 1 year was needed. In this study, we have used the category ‘Alcohol use disorder’.
More detailed descriptions of the criteria of the Lundby diagnoses may be found in previously published articles 26, 38, 39, 40. In the field investigation in 1997, the diagnoses were evaluated and assessed into a diagnosis according to ICD‐10 and DSM‐IV. A re‐evaluation was made for all episodes in 1972, but only for most first‐incidence episodes from the earlier investigations and for cases of impairment grade 3. The procedure of validation against DSM‐IV has been discussed in a previous Lundby paper 31. There was good agreement between major ‘Lundby’ diagnoses, such as psychosis, depression and alcohol use disorders, and DSM‐IV 26, 27, 41, 42. The major analyses were based on the Lundby diagnoses. A validation of suicide risk in the present study was made according to DSM‐IV criteria.
Psychiatric long‐term morbidity and additional diagnoses in the Lundby sample
In the entire sample of 3563, 1528 subjects (42.9%) had one or more Lundby diagnoses during their lives, of whom 1156 (75.7%) had only one diagnosis until 1997. When a subject had more than one Lundby diagnosis during the observation period, this was defined as long‐term additional diagnoses. Additional diagnoses were most common in the psychosis group (51.1%) and quite rarely occurred in the group of organic brain disorders (27.4%). Presence of somatic diseases or personality disorders was not investigated in this study.
Of the 1823 men, 806 (44.2%) had at least one episode of mental disorder during the observation period, and 722 of the 1740 women (41.5%).
At the time of the latest check of the National Cause of Death Register (Epidemiological Centre, National Board of Health and Welfare) on 1 July 2011, 2284 of the 3563 persons had died (64%).
The characteristics of the sample by diagnosis and age are shown in Table 1.
Table 1.
Gender distribution, suicide, age at onset and suicide by diagnoses
| Gender M/F | Suicide Total M/F | Age at onset years (SD) All cases | Age at onset means (SD) Suicide cases | Age at suicide years (SD) | |
|---|---|---|---|---|---|
|
Total population N = 3563 |
1823/1740 |
68 51/17 |
|||
|
No diagnosis N = 2035 |
1017/1018 |
6 4/2 |
69.5 (±16.5) |
||
|
Organic brain disorder N = 423 |
225/198 |
5 5/0 |
74.6 (±13.9) |
40.0 (±16.2) |
57.2 (±12.4) |
|
Psychosis N = 131 |
72/59 |
9 7/2 |
51.9 (±20.6) |
42.7 (±19.9) |
55.4 (±17.8) |
|
Depression N = 508 |
196/312 |
32 25/7 |
48.9 (±17.2) |
47.4 (±18.3) |
57.9 (±18.2) |
|
Anxiety N = 300 |
112/188 |
10 5/5 |
40.4 (±16.3) |
32.4 (±14.3) |
57.2 (±12.2) |
|
Other psychiatric disorders N = 192 |
72/120 |
6 3/3 |
37.9 (±18.7) |
34.2 (±20.0) |
62.5 ±13.8) |
|
Alcohol use disorders N = 427 |
390/37 |
29 28/1 |
34.7 (±14.8) |
33.3 (±14.6) |
58.4 (±15.7) |
|
Two or more diagnoses – First: Second: N = 372 |
157/215 |
23 21/2 |
39.6 (±19.4) 52.7 (±19.8) |
32.9 (±15.1) 45.2 (±17.3) |
59.3 (±14.6) |
|
Three or more diagnoses – First Second: Third: N = 70 |
32/38 |
4 3/1 |
34.3 (±14.1) 48.6 (±18.3) 55.6 (±19.6) |
24.0 (±6.8) 36.8 (±14.5) 41.3 (±16.5) |
58.8 (±11.2) |
In some cases, onset of the mental disorder was unknown: organic 4, depression 1, alcohol use disorders 79 cases, other psychiatric disorder 64 cases.
Criteria for suicide
By 1 July 2011, a total of 68 suicide cases had occurred, including 19 undetermined deaths.
Suicide was defined by the ICD codes, from revisions 6 to 10 34, 43, 44, 45, 46. As a new category, self‐inflicted death by undetermined intent, E980–989, was introduced in 1968, uncertain suicides according to this definition were also noted after 1968. It has often been assumed that most injuries and poisonings of undetermined intent are cases where the harm was self‐inflicted but where was insufficient evidence to prove that the deceased deliberately intended to take their own life 47, 48.
Information about suicide cases was retrieved from the Cause of Death Register. Until 1994, classification codes E950–E959 for obvious suicide, and E980–989 for undetermined death in ICD 8 and ICD‐9 were used. From 1994 until 2011, ICD 10 was used and the categories X60–X84 for obvious suicides and Y10–Y34 for event of undetermined intent were used.
The time of suicide shown by each of the follow‐ups is presented in Fig. 1.
Statistics
Comparison calculations of category variables were made with Pearson chi‐square test or Fisher′s exact test in a cross‐tabulation for estimating which variables were suitable for entering in multivariate analyses.
As we wanted to examine whether a mental disorder increased the suicide risk, and the influence of additional diagnoses of mental disorders over time, the Lundby diagnosis groups ‘organic brain disorder’, ‘psychosis’, depression’, ‘anxiety’, ′other psychiatric disorders’ and ‘alcohol use disorder’ were entered in a logistic regression analyses with a backward stepwise elimination of non‐significant results. In one of the procedures, the existence of only ‘1 diagnosis’ or ‘≥2 diagnoses’ during the observation period was included as variables. Interactions between variables, that is gender in combination with specific diagnosis, were also used in some of the analyses.
Results were considered as statistically significant for P‐values below 0.05.
The pasw Statistics 18 and version ibm spss statistics 21 (Armonk, New York, USA) software were used for the statistical calculations.
Ethical approval
The Research Ethics Committee of the Medical Faculty at University of Lund approved the 1997 follow‐up of the Lundby Study, and the participants provided written consent.
Results
Age, diagnoses and suicide
Gender distribution, suicide, age at onset and suicide in relation to diagnoses are presented in Table 1. The mean age at suicide was highest for persons without a mental disorder (69 years) and ‘other psychiatric disorders’, while for other diagnostic groups suicide occurred between 55 and 60. Those who had one or more additional disorders also died on average in their late fifties, so no earlier than those who had only one diagnosis. There was, on average, more than a decade between the debut of first and second diagnosis.
Lundby diagnoses, additional diagnoses and long‐term suicide risk
Suicide risk in all patients with different diagnoses and divided into one diagnosis and additional diagnoses in the Lundby population is presented in Table 2.
Table 2.
Suicide risk in all patients with different diagnoses and divided into one diagnosis and additional diagnoses in the Lundby population until of 1 July 2011
| All persons with the diagnosis, % | 1 diagnosis, % | ≥2 diagnoses, % | |
|---|---|---|---|
| Organic brain disorder | 5/423, 1.2 | 2/307, 0.7 | 3/116, 2.6 |
| Psychosis | 9/131, 6.9 | 2/64, 3.1 | 7/67, 10.4 |
| Depression | 32/508, 6.3 | 17/281, 6.0 | 15/227, 6.6 |
| Anxiety | 10/300, 3.3 | 4/158, 2.5 | 6/142, 4.2 |
| Other psychiatric disorders | 6/192, 3.1 | 3/110, 2.7 | 3/82, 3.7 |
| Alcohol use disorder | 29/427, 6.8 | 11/236, 4.7 | 18/191, 9.4 |
| No diagnosis | 6/2035, 0.3 |
Any diagnoses
Sixty‐eight persons of 3563 (1.9%) took their own lives during the follow‐up period 1947–2011. Fifty‐one of these (75%) were male and 17(25%) female.
Some of the subjects with no psychiatric diagnosis before 1997 took their own lives – six of 2035, indicating a long‐term suicide risk of 0.3% in individuals with no mental disorder (Table 2). Two of them were women and 4 were men (0.4% in men and 0.2% in women). Suicide risk in persons with any kind of mental disorder (one or more) according to Lundby diagnoses was 4.1% (62 of 1528 subjects). In the entire study population, 3.4% (39/1156) of persons with one Lundby diagnosis had taken their lives, whereas 6.2% of individuals with at least two diagnoses (23/372) had taken their lives. Suicide risk was higher for individuals with one psychiatric diagnosis than those with no diagnosis (OR: 11.76, 95% CI: 4.96–27.88, P < 0.0005). If a person had two or more diagnoses, the risk was even higher (OR: 21.00, 95% CI: 8.48–52.04, P < 0.0005). The groups with more than two diagnoses were too small for calculations.
Specific diagnoses
Long‐term suicide risk in different diagnoses and the influence of any kind of additional mental disorder is presented in Table 2. In individuals with only depression, the risk was 6.0%; with only alcohol use disorder, 4.7%; and with only psychosis, 3.1%, but with long‐term additional disorders, the suicide risk rose to 6.6%, 9.4% and 10.4% respectively. We found that among the Lundby main diagnoses, depression had the strongest association with suicide and increased the risk almost six times compared with the remaining cohort during the observation period (OR: 5.93, 95% CI: 3.57–9.86, P < 0.001). Alcohol use disorder and psychosis also appeared to be significant risk factors, increasing the risk about three times (OR: 3.19, 95% CI: 1.83–5.55, P < 0.001 and OR: 2.89, 95% CI: 1.32–6.34, P < 0.008).
Specific Lundby diagnoses and association with suicide by gender
In a next step, we analysed suicide risk for individual diagnoses by gender. Only diagnoses significantly included in the first analysis were used.
We used a logistic regression analysis where the variables psychosis, depression, alcohol use disorder and also gender were entered (backward stepwise elimination). This is presented in Table 3. Persons with no diagnosis were used as a reference. Psychosis in men and women showed an increased risk of suicide (OR: 2.98). Depression in women also showed an increased risk (OR: 2.56), but depression in men showed a higher risk (OR: 8.44). Alcohol use disorders in men showed a lower but increased risk (OR: 3.81).
Table 3.
Psychiatric diagnosis and gender as a risk factor for future suicide
| Risk factor | Odds ratio (OR) | 95% CI | P‐value |
|---|---|---|---|
| No diagnosis | 1 | ||
| Psychosis in both men and women | 2.98 | 1.35–6.57 | 0.007 |
| Depression in women | 2.56 | 1.11–5.93 | 0.028 |
| Depression in men | 8.44 | 4.78–14.91 | 0.0001 |
| Alcohol use disorder in men | 3.81 | 2.17–6.69 | 0.0001 |
The variables, psychosis in men and women, depression in women, depression in men, alcohol use disorder in women, alcohol use disorder in men entered a logistic regression analysis (backward stepwise elimination), with suicide as the dependent variable. Variables with at least 10% significance persisted in the last step.
Depression in men showed an increased risk compared with depression in women (OR: 3.29, CI: 1.30–8.34, P = 0.012).
Specific Lundby diagnoses and additional disorders, and association with suicide by gender
The relations between alcohol use disorders and depression per se, and in combination, in men are presented in Table 4. Alcohol use disorder only showed OR 7.14, while depression only showed an OR of 17.83. Men who had both diagnoses had a very high risk, 16% (OR: 25.11). Persons with psychosis and additional disorders had a high risk of suicide, but there were too few cases for statistical significance. As there was only one suicide among the 28 female alcoholics, no further analysis was made for the female group.
Table 4.
The Lundby diagnoses their interaction terms ‘by gender’ as risk factors for future suicide in the alcohol use disorder group. Logistic regression analyses (backward stepwise elimination)
| OR | 95% CI for EXP(B) | P‐value | |
|---|---|---|---|
| Alcohol but no depression in men | 7.14 | 3.64–14.03 | 0.0001 |
| Depression but no alcohol in men | 17.83 | 8.71–36.52 | 0.0001 |
| Both alcohol and depression in men | 25.11 | 11.32–55.73 | 0.0001 |
Suicide risk in diagnoses according to Lundby vs. DSM‐IV – a validation
Suicide risk in Lundby and DSM‐IV diagnoses for the main categories was estimated as a validation. There were similar risks for suicide among those with Lundby diagnoses and DSM‐IV diagnoses (Table 5).
Table 5.
Suicide risk in mental disorders from a long‐term perspective – Lundby diagnoses and DSM‐IV
| Suicide risk | ||
|---|---|---|
| Lundby, % | DSM‐IV, % | |
| Organic brain disorder | 5/423, 1.2 | 2/226, 0.9 |
| Psychosis | 9/131, 6.9 | 9/131, 6.9 |
| Depression | 32/508, 6.3 | 31/448a, 6.9 |
| Anxiety | 10/300, 3.3 | 5/207b, 2.4 |
| Other psychiatric disorders | 6/192, 3.1 | 1/79, 1.3 |
| Alcohol use disorder | 29/427, 6.8 | 29/427, 6.8 |
| No diagnosis | 6/2035, 0.3 | 15/2292, 0.7 |
Excluded DSM‐IV diagnoses: adjustment disorder with depressed mood (55 persons), adjustment disorder with mixed anxiety and depressed mood (1 person), adjustment disorder UNS (1 person), undifferentiated somatoform disorder (1 person), social phobia (1 person), personality change because of medical condition (1 person).
Excluded DSM‐IV diagnoses: Undifferentiated Somatoform disorder (14 persons), somatoform disorder hypochondriasis (2 persons), adjustment disorder (25 persons).
Discussion
Main findings
The very long‐term suicide risk in subjects with no, one or more mental disorders was 0.3%, 3.4% and 6.2% respectively. Suicide risk in depression was 6.3%, alcohol use disorder 6.8% and psychosis 6.9%. For individuals with only depression, the risk was 6.0%, only alcohol use disorder 4.7% and only psychosis 3.1%. However, when individuals had additional disorders, the suicide risks were 6.6%, 9.4% and 10.4% respectively. Each diagnosis per se was significantly related to increased risk of suicide, most so for depression but also for alcohol use disorders and psychosis. No significantly increased risk was found for organic disorders, anxiety or ‘other psychiatric diagnoses’. Depression was related to an increased risk in women, but the risk was higher for men. Men had a high risk for suicide when they had an alcohol use disorder, a higher risk when they had a depression and a very high risk when they had both disorders, 16.2% (OR: 25.11).
In the Lundby population, the long‐term prevalence of any mental disorder was 42.9%. The high figure is probably due to the very long follow‐up that also included organic brain disorder and dementia. This is similar to observed lifetime prevalence of 46.6% in an American population 49.
It appeared that different diagnoses could occur at different ages and there may be a long time from the occurrence of diagnosis to suicide (more than 10 years after a third diagnosis for instance). Thus, additional diagnoses are not only found prior to suicide, but may be a long‐standing problem.
Our first finding was that the long term in individuals with no mental disorder was 0.3%. To the best of our knowledge, no previous longitudinal study has reported a long‐term risk of suicide over such a long period, approaching lifetime, of risk, among people without mental disorders. An estimate of suicide risk up to the age of 51 was made by Nordentoft et al. 10, and showed 0.72% for men and 0.26% for women compared with 0.39% and 0.20% in the present study. The present study gives further evidence to a very small suicide risk among mentally healthy people. The rates in the former study appeared somewhat higher, considering the shorter time of follow‐up. This may be because the Lundby population was investigated by a trained psychiatrist, and mental disorders were more often and more accurately detected.
Secondly, the figures we found for each diagnosis, when additional diagnoses were not excluded, were fairly similar to a previous meta‐analysis 2, 6.3% for Lundby depression vs. 6% for affective disorders, 6.8% for Lundby alcohol use disorder vs. 7% for alcohol dependence and 6.9% for Lundby psychosis vs. 4% for psychosis/schizophrenia. It should be noted that the study by Inskip et al. gave a computerized estimate of lifetime mortality by suicide, while the present study is a long‐term study where not the entire population had died. However, as the study is a very long‐term follow‐up (54–64 years), we may conclude that we are approaching the lifetime risk. There is also a possibility that there would be more diagnostic cases in a new follow‐up, when the youngest individuals reach middle age and therefore higher rates of mental disorders and suicides. However, an even longer follow‐up would not necessarily show a higher risk.
Thirdly, depressed men showed an increased risk of suicide compared with depressed women. Male gender is known to be a risk factor for suicide 50, which was also found for depression in the present study. Alcohol use disorders alone in men showed an increased risk of suicide, which is in agreement with a previous study by Flensborg‐Madsen 51.
Fourthly, suicide risk was increased for men who had depression with additional alcohol use disorder. Comorbidity of alcohol use disorder and depression has been found to be associated with suicide in previous studies 11, 12, 13, 14, 23, which is in agreement with the present finding.
A large Danish study involving a (total) national cohort monitored for 15–36 years after inclusion of the study 10 showed a cumulative incidence of suicide risk in unipolar affective disorder combined with alcohol use disorder of 6.74% in men. (There was a higher risk for men with bipolar disorder in that study, but there were very few with that diagnosis in the present study.) This seems lower than the 16.2% found in the present study with a longer follow‐up. Consequently, the risk may be very high, when persons are followed up to old age. An additional or synergistic effect of alcohol use disorder and comorbid depression has been suggested 52.
An important clinical implication of the present study is that both alcohol use disorders and depression should be detected and vigorously treated to prevent suicide, especially in men, not only in concurrent or overlapping episodes, but also in separate episodes in a very long‐term perspective.
Strengths and limitations
The major strength of the present study is the very long follow‐up period, 54–64 years, which enables an estimate of suicide risk over a near lifetime span. The major limitation is the sample size with a limited number of suicides.
The Lundby Study, started in 1947, was a prospective longitudinal study on a geographically defined population in southern Sweden. Studying a community sample with a low dropout rate, as in the Lundby Study, minimizes selection bias. Hospitalized samples, for instance, may over‐represent people who had made a suicide attempt, and non‐suicidal cases of a certain diagnosis are not studied. However, lifetime suicide risk could not be investigated, as all included persons had not died, but the long‐term follow‐up did enable an approximate estimate of the lifetime suicide risk.
As suicide is less common in women, men and women could not always be compared, so the suicide risk was sometimes estimated for men only. The recall periods of 10, 15 and 25 years were of considerable length, possibly introducing bias and resulting in some episodes of mental disorders being forgotten. However, one of the strengths is the use of multiple sources to collect information in addition to the interviews, that is key informants, registers and case files, which reduced the risk of recall, observation and measurement bias. One weakness is that when family members are asked, they may be subjective in their responses.
The hierarchical diagnostic system in the Lundby Study excludes co‐occurring, less severe diagnoses at the time of evaluation. Analogous to this, episodes of combined psychiatric conditions only are registered as one diagnosis, which has precedence in this hierarchical system, but a person could have a new episode of another disorder. Alcohol use disorder is a Lundby ‘Diagnosis II’ that could be set at the time of the same episode as ‘Diagnosis I’, that is all the other diagnoses included in this study. In other words, ordinary comorbidity probably existed with alcohol use disorder.
Finally, the Lundby Study deals with a rural population originally studied in the 1940s and 1950s and followed up to 1997; this is not representative of a modern urban population with immigration and drug addiction for instance.
Declaration of interests
The authors declare that they have no conflict of interests.
Acknowledgements
We thank the Lundby population for taking part of the study. The study was supported by the Swedish Council for Planning and Coordination, The Swedish Council for Social Research, The Swedish Research Council, The Swedish Medical Research Council, The Medical Faculty, Lund University, The Principal Government of Scania, The Söderström‐Königska Foundation, The Bror Gadelius Foundation, The Sjöbring Foundation and The OM Persson Foundation. Anna Lindgren, Mathematical Statistics, Centre of Mathematical Sciences, Lund University, provided statistical advice and Anders Odensten gave data support. Leslie Walke revised the language. Mats Berglund gave valuable comments during the revision procedure.
Holmstrand C, Bogren M, Mattisson C, Brådvik L. Long‐term suicide risk in no, one or more mental disorders: the Lundby Study 1947–1997.
References
- 1. Chesney E, Goodwin GM, Fazel S. Risks of all‐cause and suicide mortality in mental disorders: a meta‐review. World Psychiatry 2014;13:153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry 1998;172:35–37. [DOI] [PubMed] [Google Scholar]
- 3. Boardman AP, Healy D. Modelling suicide risk in affective disorders. Eur Psychiatry 2001;16:400–405. [DOI] [PubMed] [Google Scholar]
- 4. Blair‐West GW, Mellsop GW, Eyeson‐Annan ML. Down‐rating lifetime suicide risk in major depression. Acta Psychiatr Scand 1997;95:259–263. [DOI] [PubMed] [Google Scholar]
- 5. Murphy GE, Wetzel RD. The lifetime risk of suicide in alcoholism. Arch Gen Psychiatry 1990;47:383–392. [DOI] [PubMed] [Google Scholar]
- 6. Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 2005;62:247–253. [DOI] [PubMed] [Google Scholar]
- 7. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol 2010;24(4 Suppl):81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Allgulander C, Lavori PW. Excess mortality among 3302 patients with ‘pure’ anxiety neurosis. Arch Gen Psychiatry 1991;48:599–602. [DOI] [PubMed] [Google Scholar]
- 9. Allebeck P, Allgulander C, Fisher LD. Predictors of completed suicide in a cohort of 50,465 young men: role of personality and deviant behaviour. BMJ 1988;297:176–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry 2011;68:1058–1064. [DOI] [PubMed] [Google Scholar]
- 11. Cheng AT. Mental illness and suicide. A case‐control study in east Taiwan. Arch Gen Psychiatry 1995;52:594–603. [DOI] [PubMed] [Google Scholar]
- 12. Dumais A, Lesage AD, Alda M et al. Risk factors for suicide completion in major depression: a case‐control study of impulsive and aggressive behaviors in men. Am J Psychiatry 2005;162:2116–2124. [DOI] [PubMed] [Google Scholar]
- 13. Conner KR, Beautrais AL, Conwell Y. Risk factors for suicide and medically serious suicide attempts among alcoholics: analyses of Canterbury Suicide Project data. J Stud Alcohol 2003;64:551–554. [DOI] [PubMed] [Google Scholar]
- 14. Murphy GE, Wetzel RD, Robins E, McEvoy L. Multiple risk factors predict suicide in alcoholism. Arch Gen Psychiatry 1992;49:459–463. [DOI] [PubMed] [Google Scholar]
- 15. de Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long‐term follow‐up study. Schizophr Res 2001;47:127–134. [DOI] [PubMed] [Google Scholar]
- 16. Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry 2005;187:9–20. [DOI] [PubMed] [Google Scholar]
- 17. Reutfors J, Brandt L, Jonsson EG, Ekbom A, Sparen P, Osby U. RISk factors for suicide in schizophrenia: findings from a Swedish population‐based case‐control study. Schizophr Res 2009;108:231–237. [DOI] [PubMed] [Google Scholar]
- 18. Arsenault‐Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta‐analysis. BMC Psychiatry 2004;4:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Barraclough B, Bunch J, Nelson B, Sainsbury P. A hundred cases of suicide: clinical aspects. Br J Psychiatry 1974;125:355–373. [DOI] [PubMed] [Google Scholar]
- 20. Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395–405. [DOI] [PubMed] [Google Scholar]
- 21. Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. Br J Psychiatry 1997;170:447–452. [DOI] [PubMed] [Google Scholar]
- 22. Henriksson MM, Aro HM, Marttunen MJ et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 1993;150:935–940. [DOI] [PubMed] [Google Scholar]
- 23. Isometsa ET. Psychological autopsy studies–a review. Eur Psychiatry 2001;16:379–385. [DOI] [PubMed] [Google Scholar]
- 24. Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry 2002;1:181–185. [PMC free article] [PubMed] [Google Scholar]
- 25. Brådvik L, Mattisson C, Bogren M, Nettelbladt P. Long‐term suicide risk of depression in the Lundby cohort 1947–1997 – severity and gender. Acta Psychiatr Scand 2008;117:185–191. [DOI] [PubMed] [Google Scholar]
- 26. Mattisson C, Bogren M, Ojehagen A, Nordstrom G, Horstmann V. Mortality in alcohol use disorder in the Lundby Community Cohort–a 50 year follow‐up. Drug Alcohol Depend 2011;118:141–147. [DOI] [PubMed] [Google Scholar]
- 27. Bogren M, Mattisson C, Isberg PE, Munk‐Jorgensen P, Nettelbladt P. Incidence of psychotic disorders in the 50 year follow up of the Lundby population. Aust N Z J Psychiatry 2010;44:31–39. [DOI] [PubMed] [Google Scholar]
- 28. Anderberg J, Bogren M, Mattisson C, Brådvik L. Long‐term suicide risk in anxiety – the Lundby study 1947–2011. Arch Suicide Res 2015; (In press). [DOI] [PubMed] [Google Scholar]
- 29. Essen‐Möller E. Individual traits and morbidity in a Swedish rural population. Copenhagen: Munksgaard, 1956:160 pp. [PubMed] [Google Scholar]
- 30. NATIONAL BOARD OF HEALTH AND WELFARE . Patient register. Stockholm: National Board of Health and Welfare; 2004. [Google Scholar]
- 31. Nettelbladt P, Bogren M, Mattisson C et al. Does it make sense to do repeated surveys? – the Lundby Study, 1947–1997. Acta Psychiatr Scand 2005;111:444–452. [DOI] [PubMed] [Google Scholar]
- 32. Rothman KJ, Greenland S, Lash TL. Modern epidemiology, 3rd edn Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2008:x, 758 pp. [Google Scholar]
- 33. Frances A, American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM‐IV: prepared by the Task Force on DSM‐IV, 4th edn Washington, DC: American Psychiatric Assoc, 1994:xxvii, 886 pp. [Google Scholar]
- 34. World Health Organization . ICD‐10: international statistical classification of diseases and related health problems, 10th revision edn Geneva: World Health Organization, 1992. [Google Scholar]
- 35. Leighton DC, Harding JS, Macklin DB, Hughes CC, Leighton AH. Psychiatric findings of the Stirling Country Study. Am J Psychiatry 1963;119:1021–1026. [DOI] [PubMed] [Google Scholar]
- 36. Bogren M, Mattisson C, Horstmann V, Bhugra D, Munk‐Jorgensen P, Nettelbladt P. Lundby revisited: first incidence of mental disorders 1947–1997. Aust N Z J Psychiatry 2007;41:178–186. [DOI] [PubMed] [Google Scholar]
- 37. Bogren M, Mattisson C, Isberg PE, Nettelbladt P. How common are psychotic and bipolar disorders? A 50‐year follow‐up of the Lundby population. Nord J Psychiatry 2009;63:336–346. [DOI] [PubMed] [Google Scholar]
- 38. Grasbeck A, Hagnell O, Otterbeck L, Rorsman B. Anxiety in the Lundby Study: re‐evaluation according to DSM‐III‐R, incidence and risk. Neuropsychobiology 1993;27:1–8. [DOI] [PubMed] [Google Scholar]
- 39. Hagnell O. A prospective study of the incidence of mental disorder. A study based on 24,000 person years of the incidence of mental disorders in a Swedish population together with an evaluation of the aetiological significance of medical, social, and personality factors. The Lundby project.] [Akademisk avhandling]. Lund:Svenska bokförlaget, 1966. [Google Scholar]
- 40. Mattisson C, Bogren M, Nettelbladt P, Munk‐Jorgensen P, Bhugra D. First incidence depression in the Lundby Study: a comparison of the two time periods 1947–1972 and 1972–1997. J Affect Disord 2005;87:151–160. [DOI] [PubMed] [Google Scholar]
- 41. Mattisson C, Bogren M, Bradvik L, Horstmann V. Mortality of subjects with mood disorders in the Lundby community cohort: a follow‐up over 50 years. J Affect Disord 2015;178:98–106. [DOI] [PubMed] [Google Scholar]
- 42. Mattisson C, Bogren M, Horstmann V, Tambs K, Munk‐Jorgensen P, Nettelbladt P. Risk factors for depressive disorders in the Lundby cohort–a 50 year prospective clinical follow‐up. J Affect Disord 2009;113:203–215. [DOI] [PubMed] [Google Scholar]
- 43. World Health Organization . ICD‐7: international statistical classification of diseases and related health problems, 7th revision edn Paris: World Health Organization, 1955. [Google Scholar]
- 44. World Health Organization . ICD‐9: international statistic classification of diseases and related health problems, 9th revision edn Geneva: World Health Organization, 1987. [Google Scholar]
- 45. World Health Organization . ICD‐6: international statistical classification of diseases and related health problems, 6th revision edn Paris: World Health Organization, 1949. [Google Scholar]
- 46. World Health Organization . ICD‐8: international statistical classification of diseases and related health problems, 8th revision edn Geneva: World Health Organisation, 1968. [Google Scholar]
- 47. Hawton K, Bergen H, Simkin S et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ 2013;346:f403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Linsley KR, Schapira K, Kelly TP. Open verdict v. suicide – importance to research. Br J Psychiatry 2001;178:465–468. [DOI] [PubMed] [Google Scholar]
- 49. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593–602. [DOI] [PubMed] [Google Scholar]
- 50. Canetto SS, Sakinofsky I. The gender paradox in suicide. Suicide Life Threat Behav 1998;28:1–23. [PubMed] [Google Scholar]
- 51. Flensborg‐Madsen T, Knop J, Mortensen EL, Becker U, Sher L, Gronbaek M. Alcohol use disorders increase the risk of completed suicide – irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Res 2009;167:123–130. [DOI] [PubMed] [Google Scholar]
- 52. Cornelius JR, Salloum IM, Mezzich J et al. Disproportionate suicidality in patients with comorbid major depression and alcoholism. Am J Psychiatry 1995;152:358–364. [DOI] [PubMed] [Google Scholar]


