Abstract
Background
The current literature regarding the transition from milks to solid foods across the first 2 years of life is limited despite the important influence of early dietary intake on children's growth and development. The present study describes dietary intake from birth to 2 years across four developmental relevant time‐points within an Australian birth cohort.
Methods
Dietary data from 466 infants was collected at four time‐points in the first 2 years of life via parent‐reported questionnaire, including a 45‐item food and beverage frequency questionnaire. Subsample analyses of children who were aged 1–3, 6–8, 12–14 and 18–20 months at the time of data collection were conducted.
Results
Infant formula remained consistently consumed by over 75% of children from the 6–8‐ to 18–20 months old age groups. Mean (SD) age of introduction to solid foods was 5.2 (1.3) months. Almost 20% and 10% of children were introduced before 16 and after 32 weeks, respectively. The highest consumption of core foods, recommended for a healthy diet, daily was seen in the 12–14 months old age group with lower proportions in the 18–20 months old age group coinciding with an increased proportion of children eating discretionary choice foods, not recommended for a healthy diet. Discretionary choice foods/beverages presented in children's diets as early as in the 6–8 months old age group. By 18–20 months, at least 20% of children were consuming savoury biscuits, sweet biscuits, muesli bars and luncheon meats at least twice a week.
Conclusions
The present study identified a number of findings outside the recommendations of the Australian Dietary and Infant Feeding Guidelines. Further work is warranted to explore these outcomes.
Keywords: child, core foods, diet, discretionary foods, infant feeding guidelines, introduction to solids
Introduction
During the first 2 years of life, children's diets change from solely milk based to a variety of solid foods. How diets transition during this period of life is poorly reported in current literature. It is well known that children's nutrition is essential for optimal growth and development 1 and, importantly, this is the time during which life‐long food preferences and eating patterns are established 2, 3, 4. Highlighting this is significant because evidence continues to grow between risk and protective child‐feeding habits in the development of lifestyle disease's, including obesity and dental decay 5, 6.
In Australia, two sets of dietary guidelines apply to children. The Australian Infant Feeding Guidelines (AIFG) (2012) 2 provide recommendations from birth to 24 months, with a focus on breast milk (BM) and infant formula (IF) feeding, as well as the transition onto a wider variety of food/beverage items. The Australian Dietary Guidelines (ADG) 7 provide more specific information about foods and beverages to include within a healthy diet from 2 years of age, including recommended serves and serving sizes. The AIFG do not specifically recommend serving sizes; rather, they advise on what types of foods and beverages should be introduced at different ages and also advise parents that the introduction of foods and beverages should be driven by the child's readiness and developmental stage. The over‐arching theme depicted by these guidelines is to enjoy a wide variety of core foods, foods/beverages recommended for a healthy diet, from the five main food groups; fruit, vegetables and legumes, meat and alternatives, cereals and dairy. With the aim to avoid the consumption of discretionary choice foods, food/beverages not necessary for inclusion in a healthy diet are those that contain large amounts of sugar, fat and salt, with little to no nutritional value 7.
To date, the majority of research in Australia and internationally has focused on diets of children older than 2 years, with little work before this age. Particularly lacking and of great interest is information on foods and beverages that children are introduced to as they are weaned from BM and IF. Limited research in Australia with children under 2 years has focussed primarily on the macro‐/micronutrient composition of the diet, specifically food amounts and contribution to total energy 8, 9 and/or a comparison of specific nutrients with Recommended Daily Intakes 9, 10, whereas other studies have identified specific diet profiles (e.g. healthy, unhealthy) 11, 12. These studies found that some dietary patterns in children under 2 years are not consistent with developing long‐term healthy food preferences and the high consumption of discretionary choice foods/beverages 10, 13, 14. Additional studies have explored the introduction of solid foods in children, finding the introduction to be earlier than the recommended age of 6 months, with averages of between 17 and 19 weeks 15, 16. The Australian 2010 National Infant Feeding Survey on children 0–24 months reported rates of breastfeeding, as well as the consumption of IF, other milks and solid foods; however, no evidence was presented on the types of foods consumed 17.
The VicGen study is a longitudinal birth cohort following children from birth to 6 years 18. Dietary data have been collected at four time‐points within the first 2 years of life, providing comprehensive dietary information about children's transition from solely milk to foods and other beverages. This research aims to provide a more detailed understanding of dietary consumption across the first 2 years of life, specifically describing:
Breast milk, infant formula and other milk consumption.
Timing and type of solid foods being introduced.
Type of core and discretionary choice foods and beverages being consumed by children and age they are introduced.
Where possible, how closely foods and beverages consumed reflect national dietary recommendations.
Materials and methods
Study design and data collection
The present study analyses data from the VicGen study, which began in 2008. VicGen has a longitudinal, multidisciplinary design aiming to investigate the factors involved in the development of early childhood caries. Four hundred and sixty‐six mother–child dyads were recruited several weeks after birth from Maternal and Child Health Centres in seven local government areas from a purposive mix of metropolitan, regional and rural areas in Victoria, Australia. Eight waves of data have been collected; baseline (approximately 6 weeks of age) and at 6, 12, 18, 36, 48, 60 and 72 months. Parent completed surveys were mailed in advance and collected by the research team at each wave. Ethical approval to conduct this study was received from the University of Melbourne Human Research Ethics Committee. Further information on the study design can be obtained from the protocol paper 18.
Outcome variables
Dietary information was collected via the self‐reported parent questionnaire. BM consumption was measured through a yes/no response: ‘Is this child currently receiving BM?’. Subsequent questions were answered as the number of times per day, week or month: ‘How old was this child when he/she was first given infant formula?’ and ‘How old was this child when he/she was first given any other milk, other than breast milk or infant formula?’.
Introduction to solid foods was measured using the questions: ‘Has this child started solid foods?’, with a yes/no response and ‘At what age was this child first given solid food regularly’, with response options of age in months, weeks or days.
Food and beverage consumption was collected using a food frequency questionnaire (FFQ), consisting of 33 food and 12 beverage items. Food consumption was measured by asking: ‘In a usual week, how often does the child have the following foods?’, with response options from never to 4+ times per day. Beverage consumption was measured by asking: ‘Does this child drink any of the following?’, with a yes/no response and requesting the times per day or week or month. This FFQ had been piloted for feasibility and acceptability, and examined for its reliability and validity 19.
Statistical analysis
The present study uses the first four waves of data from the VicGen study. Because diets of young children vary greatly and there was a wide age range of children at each wave, a subset of children from each wave were used for analysis (Fig. 1). Four age groups were selected (1–3, 6–8, 12–14 and 18–20 months), reflecting usual developmental progression and the AIFG recommended introduction of different foods and beverages. All children who fell within this specified age range at the time of data collection were included in the analysis. There were 141 children who fell into the corresponding age category at each data collection wave.
Figure 1.

Subsample selection from data collection wave.
According to the ADG, the FFQ measured 18 core foods, four core beverages, 15 discretionary foods and eight discretionary beverages 7. Two dietitians used their clinical judgement and the ADG and AIFG to create three consumption frequency categories to reflect what would be considered, low, moderate and high consumption. The three categories for core foods were: less than once per day; once per day; and more than once per day, whereas the discretionary food categories were less than twice per week; two or more times per week but less than once per day; and one or more times per day.
Simple descriptive statistics were produced for each food and beverage by age group. The top 10 core and discretionary choice foods, as well as the top five beverages, were selected by determining which were most consistently and highly consumed. All analyses were conducted in stata ic, version 13.1 (StataCorp, College Station, TX, USA).
Results
Participant characteristics
Table 1 shows the demographic characteristics of participants in each age group. Compared to younger groups, the older groups had slightly higher proportions of mothers with a tertiary education and who spoke English at home, as well as lower proportions of families who resided in a metropolitan area and had a healthcare card.
Table 1.
Participant characteristics in each cross‐sectional age group
| 1–3 months | 6–8 months | 12–14 months | 18–20 months | |
|---|---|---|---|---|
| n | 438 | 278 | 268 | 256 |
| Proportion of original sample, % | 94.0 | 59.7 | 57.5 | 54.9 |
| Child | ||||
| Birth weight (kg), mean (SD) | 3.4 (0.5) | 3.4 (0.6) | 3.5 (0.5) | 3.5 (0.5) |
| Birth length (cn), mean (SD) | 50.2 (2.3) | 50.4 (2.4) | 50.1 (2.3) | 50.3 (2.3) |
| Mother | ||||
| Age at baseline (years), mean (SD) | 30.1 (5.3) | 30.3 (5.3) | 30.7 (5.0) | 30.8 (5.0) |
| Born in Australia (%) | 64.8 | 69.8 | 72.4 | 71.9 |
| Speak English at home (%) | 73.5 | 80.6 | 81.0 | 80.9 |
| Post‐school education (%)a | ||||
| None | 21.2 | 19.4 | 16.0 | 15.2 |
| Certificate/apprenticeship/diploma/advanced diploma | 40.4 | 40.7 | 39.6 | 40.2 |
| Bachelor degree or higher | 37.7 | 39.9 | 44.4 | 44.1 |
| Family | ||||
| Possess healthcare cardb (%)a | 38.6 | 34.5 | 29.9 | 30.9 |
| Location (%)a | ||||
| Metropolitan | 65.8 | 64.4 | 60.8 | 59.8 |
| Regional | 11.2 | 13.3 | 14.9 | 15.2 |
| Rural | 23.1 | 22.3 | 24.3 | 25.0 |
Baseline measures.
Means tested card for low income earners entitling holder to concessions on certain services.
Breastfeeding, infant formula and other milk consumption
Figure 2 shows the proportion of children consuming BM, IF and other milk in each of the age groups. The proportion of children consuming BM became progressively lower as the age group increased; however, the proportion of children receiving IF was similar in the 1–3, 6–8 and 18–20 months old age groups. Very few children were receiving ‘other’ milk in the two younger groups, although this changed in the older two groups, with over 80% receiving ‘other’ milk.
Figure 2.
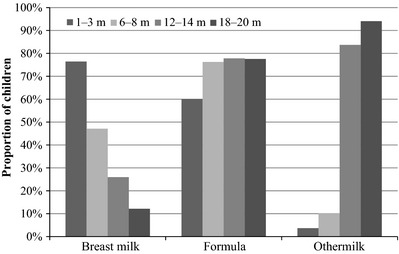
Consumption of breast milk, infant formula and other milk in four age groups of young children (n varies across time and item; 1–3 months, n = 436–438; 6–8 months, n = 276–278; 12–14 months, n = 264–266; 18–20 months, n = 252–254).
Introduction to solid foods
All children aged 12–14 months had commenced solid foods at a mean (SD) age of 5.2 (1.3) months. Almost 20% started solids before 16 weeks and almost 10% did not commence until at least 32 weeks. Figure 3 shows the age distribution in which children started consuming solid foods.
Figure 3.

Child age (weeks) when the consumption of solid foods commenced in the 12–14 months old age group (n = 265).
Core foods
The 10 most frequently consumed core foods in each age group are shown in Table 2. In the 6–8 months old age group, cereals, vegetables and fruit (fresh and stewed) were most frequently consumed. Approximately 70% of children in the 12–14 months old age group were consuming vegetables and just over 50% consuming fruit at least once a day. Slightly higher and lower proportions were seen for fruit and vegetables, respectively, in the 18–20 months old age group. The proportions of children consuming core foods at least once a day was highest in the 12–14 months old age group.
Table 2.
Proportion of children consuming the 10 most frequently reported core foods across each age groupa
| Food group | Food | 6–8 monthsb | 12–14 monthsc | 18–20 monthsd | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Less than once per day | Once per day | More than once per day | Less than once per day | Once per day | More than once per day | Less than once day | Once per day | More than once per day | ||
| Dairy | Cheese | 97.4 | 2.2 | 0.4 | 77.8 | 18.1 | 4.1 | 67.9 | 24.1 | 8.0 |
| Yoghurt | 87.9 | 11.0 | 1.1 | 65.0 | 28.5 | 6.5 | 66.0 | 30.4 | 3.6 | |
| Fruit | Banana | 91.5 | 8.2 | 0.4 | 72.8 | 25.3 | 1.9 | 80.8 | 18.4 | 0.8 |
| Fresh Fruit (not banana) | 73.2 | 23.1 | 3.7 | 48.1 | 31.4 | 20.5 | 44.2 | 29.1 | 26.7 | |
| Stewed fruit | 74.5 | 19.6 | 5.9 | 89.0 | 9.5 | 1.5 | 94.4 | 5.2 | 0.4 | |
| Cereals | Breakfast cereal | 43.7 | 47.4 | 9.0 | 31.3 | 66.4 | 2.3 | 45.8 | 52.6 | 1.6 |
| Bread | 94.1 | 4.4 | 1.5 | 57.1 | 33.1 | 9.8 | 55.9 | 34.0 | 10.1 | |
| Vegetables and legumes | Potato | 87.1 | 9.9 | 2.9 | 86.8 | 12.4 | 0.8 | 92.4 | 7.2 | 0.4 |
| Vegetables (not potato) | 49.1 | 36.1 | 14.9 | 31.7 | 47.2 | 21.1 | 34.9 | 43.0 | 22.1 | |
| Meat and alternatives | Meat/fishe | – | – | – | 67.3 | 24.8 | 7.9 | 58.7 | 32.5 | 8.7 |
Other measured core foods in the food frequency questionnaire not in the top 10 most frequently consumed were; eggs, nuts, noodles/pasta, rice/cous cous, baked beans, ready to eat baby food, soup, dried fruit.
n = 268–272.
n = 263–266.
n varies = 247–251.
Data were not collected for meat/fish in the 6–8 months old age group.
Discretionary choice foods
The 10 most frequently consumed discretionary choice foods in each age group are shown in Table 3. Custard and savoury biscuits were the most frequently consumed items within the 6–8 and 12–14 months old age groups. In the 18–20 months old age group, savoury and sweet biscuits had the largest proportion of children consuming them at least twice a week and over 30% consumed savoury biscuits at least once a day. Larger proportions of children in this group consumed muesli bars, chocolates/lollies and hot chips at least twice a week, compared to the earlier age groups.
Table 3.
Proportion of children consuming the 10 most frequently reported discretionary choice foods across each age groupa
| 6–8 monthsb | 12–14 monthsc | 18–20 monthsd | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Less than twice per week | Two or more times per week, less than once per day | One or more times per day | Less than twice per week | Two or more times per week, less than once per day | One or more times per day | Less than twice per week | Two or more times per week, less than once per day | One or more times per day | |
| Jame | 97.1 | 1.9 | 1.1 | 91.3 | 7.9 | 0.8 | 83.9 | 13.3 | 2.8 |
| Muesli bars | 98.5 | 0.7 | 0.7 | 87.6 | 10.9 | 1.5 | 79.4 | 15.7 | 4.8 |
| Savoury biscuits | 73.7 | 14.1 | 12.2 | 17.9 | 39.9 | 42.2 | 17.6 | 50.8 | 31.6 |
| Ice‐cream | 99.3 | 0.7 | 0.0 | 994.0 | 5.7 | 0.4 | 87.2 | 12.1 | 0.8 |
| Custard | 78.7 | 17.3 | 4.0 | 75.6 | 19.2 | 5.3 | 87.2 | 11.2 | 1.6 |
| Sweet biscuits | 95.6 | 2.2 | 2.2 | 79.6 | 17.7 | 2.6 | 65.1 | 27.3 | 7.6 |
| Chocolate/lollies | 99.6 | 0.4 | 0.0 | 97.4 | 2.3 | 0.4 | 81.1 | 16.5 | 2.4 |
| Hot chips (e.g. French fries) | 98.2 | 1.8 | 0.0 | 91.7 | 7.5 | 0.8 | 82.0 | 18.0 | 0. |
| Peanut butter/nutellaf | 100 | 0.0 | 0.0 | 93.2 | 6.4 | 0.4 | 84.9 | 13.2 | 2.0 |
| Luncheon meatsg | 99.3 | 0.7 | 0.0 | 82.3 | 15.0 | 2.6 | 66.9 | 28.6 | 4.4 |
Other measured discretionary foods in the food frequency group not in the top 10 most frequently consumed were; pudding, jelly, donuts, cakes/muffins, potato chips/crisps.
n = 270–272.
n = 263–266.
n = 248–251.
A spread usually made with preserved fruit and sugar.
Chocolate and hazelnut spread.
Also known as delicatessen meats/cold cuts (e.g. salami, ham, strasburg).
Beverages
Table 4 shows the consumption patterns of the five most commonly reported beverages across each age group. Water was the most commonly consumed beverage in each age group. Very few children in the 6–8 months old age group were drinking full fat cow's milk regularly; consumption was more common in the older age groups, with 65.5% of children in the 12–14 months old age group and 76.8% in 18–20 months old age group consuming it at least once a day. Juice was the most commonly consumed discretionary choice beverage across all age groups, with soft drink and cordial becoming predominant with increasing age group.
Table 4.
Proportion of children consuming the five most frequently reported beverages across each age group
| Core Beverages | 6–8 monthsa | 12–14 monthsb | 18–20 monthsc | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Less than once per day | once per day | More than once per day | Less than once per day | once per day | More than once per day | Less than once per day | once per day | More than once per day | |
| Water | 30.5 | 15.6 | 53.9 | 3.2 | 5.1 | 91.7 | 2.1 | 4.1 | 93.8 |
| Full fat milk | 98.6 | 0.7 | 0.7 | 34.5 | 16.3 | 49.2 | 23.2 | 12.8 | 64.0 |
| Discretionary choice beverages | Less than twice per week | Two or more times per week, less than once per day | One or more times per day | Less than twice per week | Two or more times per week, less than once per day | One or more times per day | Less than twice per week | Two or more times per week, less than once per day | One or more times per day |
|---|---|---|---|---|---|---|---|---|---|
| Juice | 92.0 | 2.6 | 5.5 | 77.7 | 11.5 | 10.8 | 57.5 | 18.5 | 24.0 |
| Cordiald | 99.3 | 0.4 | 0.4 | 93.2 | 2.3 | 4.5 | 88.5 | 6.0 | 5.6 |
| Soft drink | 100 | 0.0 | 0.0 | 97.4 | 2.6 | 0.0 | 95.3 | 4.3 | 0.4 |
n = 269–276.
n = 253–266.
n = 242–255.
A concentrated, noncarbonated syrup usually mixed with water before drinking.
Discussion
The present study has examined Australian children's dietary consumption patterns from birth to 20 months of age, investigating BM, IF and milk consumption, the introduction of solid foods and when core and discretionary choice foods present in children's diets. To our knowledge, this is the first study to report data regarding food and beverage consumption within the first 2 years of children's lives from within a cohort of children across a range of time‐points.
Breast milk, infant formula and other milks
BM consumption was consistent with other Australian findings 17, 20, with over 75% of children in the 1–3 months old age group receiving BM, and a decreasing proportion at each older time‐point. Use of IF and nonhuman milks within the first 2 years of life has only been reported by one cross‐sectional study in Australia with children aged 12–16 months. They found that 32% and 78% of children consumed IF and cow's milk, respectively, with younger age being associated with higher IF intake and older age with cow's milk consumption 9. The National Feeding survey reported whether children received nonhuman milk or IF, however, was not specific to which drink was received. Therefore, these data provide the first evidence concerning what fluids children under 2 years are drinking other than BM and highlight that a large proportion consumed IF in the first 20 months of life. Particularly interesting was the proportion of children at 18–20 months consuming IF. The AIFG recommend IF as a substitute for breast milk (when mothers cannot or choose to cease breastfeeding) until 12 months; subsequently, it is to the mothers discretion regarding whether to continue using formulas or, alternatively, whether cow's milk can be introduced as the main drink. Further research is required to explore the determinants for mothers continuing to use formulas past 12 months and the how this effects overall dietary quality and variety. The proportion of children who consumed other milks was exponentially larger at 12–14 months than at the earlier time‐points. The AIFG recommend that, after 12 months, cow's milk may be given as the main drink; however, it should not be given to children under 12 months because it is associated with increased incidence of iron deficiency and has a high renal solute as a result of higher electrolyte and protein levels 2. Despite these recommendations, 10% of children at 6–8 months in our sample were drinking other milks such as cow's milk.
Introduction to solid foods
By 6 months, BM and IF no longer provide sufficient nutrition 2 and children require solid foods. Children's average age of introduction to solid foods was 5.2 months of age (22.5 weeks), which is older than in previously reported Australian studies. The Perth Infant Feeding study reported an average of 17.5 weeks (4 months) 15 and a western Melbourne study reported 4.3 months (18.6 weeks) 16. Almost 20% of children began solids earlier than recommended at 16 weeks (3.7 months) and, in contrast, almost 10% of children did not commence until 32 weeks (7.4 months) or later. Although the average age of introduction was close to recommendations, the outliers are at risk. Early introduction can result in less time on the breast, a decline in maternal milk production and, in some cases, under‐nutrition and a higher risk of allergy development. By contrast, a late introduction can falter growth as a result of insufficient nutrition, particularly iron and zinc, as iron stores deplete around 6 months 2, 5.
Overall dietary consumption
The consumption frequency of core foods within the five main food groups highlighted discrepancies between the guidelines and what children aged between 6 and 20 months were consuming. Within each food group, a number of children were not consuming core foods at least once a day, with the highest consumption of core foods at least once a day occurring within the 12–14 months old age group. Only fresh fruit, bread, cheese and meat/fish were consumed more highly within the 18–20 months old age group. This coincides with the 18–20 months old age group having a higher proportion consuming discretionary choice foods at least twice a week. This may indicate the displacement of core foods with discretionary choice alternatives. Core foods are essential for providing key nutrients and a nutritionally adequate diet is protective against childhood morbidity and mortality, in addition to being protective for immunity, and helping with the proper growth of muscles and bones for adulthood, as well as the prevention of obesity and malnutrition. Dairy intake from cheese and yoghurt was low, with only one‐third eating these at least once a day within the 12–14 and 18–20 months old age groups and, although milk consumption was high, dairy intake was most likely inadequate. Dairy provides an essential source of calcium, phosphorus, protein and potassium, which are necessary for proper bone and tissue development; therefore, an inadequate intake can be detrimental towards this growth. Just over one‐third of children consumed meat or fish and only a minority ate meat alternatives at least once a day within the 12–14 and 18–20 months old age groups. An inadequate meat/fish intake is particularly concerning after 6 months because meat/fish comprises a rich source of iron, zinc, protein, omega 3 and vitamin B12 and, as a result of iron stores being depleted, they need to be replaced through food. Iron‐rich foods are the first foods that should be introduced, which shows a discrepancy in how the guidelines are being followed at this time of weaning. Both inadequate intakes of dairy and meat and alternatives are important to emphasise because they contain rich sources of essential nutrients that children require in this rapid time of growth and development.
The cereals, fruit and vegetable food groups were most frequently consumed with over half of the children in the 12–14 and 18–20 months old age groups consuming cereal, bread, vegetables and fresh fruit at least once a day. Vegetables and fresh fruit particularly had the highest proportions of children eating these greater than once a day. Potato and banana were measured separately and, even when combined with vegetables and fresh fruit, respectively, and not necessarily mutually exclusively, this highlights that one‐third of children in the 18–20 months old age group are still not consuming core foods from within the fruit and vegetable food groups at least once a day. 2. The evidence of the health benefits of consuming fruit, cereals and vegetable and legumes is well documented for being protective against the development of chronic conditions, including obesity, type 2 diabetes and cardiovascular conditions; therefore, not including these within the daily diet is detrimental to overall child growth and development.
The displacement of core with discretionary choice alternatives as seen in the 18–20 months old age group is important to highlight because nutritionally adequate diets can be achieved without discretionary choice foods/beverages in that they contribute minimal essential nutrients. These presented in the diets of some children as early as in the 6–8 months old age group and the proportion of children and consumption frequency increased within each age group. In particular, dietary intakes in the 18–20 months old age group were almost 20% for muesli bars, chocolate/lollies and hot chips, almost 30% for sweet biscuits and luncheon meats, and almost 80% for dry biscuits, all individually at least twice a week. Cordial and soft drink consumption was quite low, with 11.5% and 4.7%, respectively, consuming each; however, the proportion drinking juice increased at each time point, from just over 5% having at least once a day within the 6–8 months old age group to 24% in the 18–20 months old age group. Preceding Australian studies found similar results, in that young children aged between 12 and 36 months are consuming higher than recommended amounts of discretionary choice food and beverages 1, 9, 12, 13; however, these findings have only looked at one time‐point, with none exploring consumption from birth up to 20 months. Twenty‐five percent of Australian children are classed as overweight or obese 21 and almost half of children aged 5–6 years have a history of dental decay 22. Strong evidence exists supporting connections between the consumption of discretionary choice foods/beverages and the development of dental caries and obesity 6, 23; therefore, the dietary patterns that we observe within these children may be predictive of future disease development.
Eating habits and behaviours are developed at a young age and, between 6 and 24 months, children are learning about foods taste, smell, feel and look. They do not choose which foods are available to them; this is the role of parents and caregivers. Previous studies and our findings support the notion of a gap in parental knowledge and/or highlight poor food‐related behaviours of parents towards their children's dietary intake. Offering nutritionally balanced and varied diets in the early years has been shown to influence the adoption of future healthy eating patterns and good health. Hence, capturing this information is important for tailoring dietary interventions targeted at parents and their young children.
Limitations and strengths of the present study
Parent‐reported dietary frequency intakes were used and we recognise that these measures may attract bias or socially desirable responses; however, reliability data indicate that this is unlikely in our sample. Our dietary data are measured as the frequency of consumption; thus, the absence of metric measurements prevents an assessment of the exact nutritional composition. Although we have a population mix, the overall study examines the relationship between diet and oral health outcomes; therefore, recruitment targeted a representation of children at greater risk of caries, and thus a lower socio‐economic risk. Accordingly, for generalisability to other population groups, a comparison of sample data will be required. Meat/fish data were not collected at the 6‐month time‐point because the FFQ targeted sugar intake; however, to capture better the overall diet quality, such data were included from 12 months onwards. Although the food and beverage frequency scales are comprehensive, they do not measure an entire diet of food and drink (specifically, no sources of fats and oils), nor are they able to indicate the way in which foods have been prepared or cooked. Additionally, data collection occurred before the change in the ADG and AIFG in 2013 and 2012, respectively. Prior to this, one reference document existed: the Dietary Guidelines for Children and Adolescents in Australia released in 200324. Minimal differences exist between these guidelines, with the exception of the 2003 guidelines recommending a delayed introduction of cheese, yoghurt, ice‐cream, fish, wheat cereal and peanuts until 12 months if there is a family history of allergy, compared to new evidence suggesting that a delayed exposure may increase the probability of an allergy.
The strengths of the present study are that data were captured from as soon as feasible after birth up to age 2 years, over four waves, and within the same cohort of children. The questions specifically addressed the age of introduction to solid foods, IF and other milks. Food and beverage frequency data were obtained with respect to times per week rather than capturing just a single or few days’ worth of food, as had been conducted in previous Australian studies. Another advantage is that food and beverage data were collected from the second wave onwards, therefore allowing us to determine the exact types of food and beverages that were introduced and how these changed over subsequent waves.
Conflict of interests, source of funding and authorship.
The authors declare that they have no conflicts of interest.
The VicGen birth cohort was funded by a National Health and Medical Research Council Project Grant, with contributions from The Financial Markets Foundations for Children, Dental Health Services Victoria and the Victorian Government Department of Early Childhood and Education.
EA and E‐O'C were responsible for study conception and design, acquisition of data, analysis and interpretation, drafting and critical revision of the manuscript. LC was responsible for data management, statistical analysis, conception and design, analysis and interpretation, drafting and critical revision of the manuscript. All authors critically reviewed the manuscript and approved the final version submitted for publication.
Acknowledgments
We thank the families involved with the VicGen cohort, as well as the Maternal Child Health Nurses for assisting with the recruitment. We also acknowledge the contribution of all staff involved in the VicGen birth cohort.
Amezdroz, E. , Carpenter, L. , O'Callaghan, E. , Johnson, S. , Waters, E. (2015) Transition from milks to the introduction of solid foods across the first 2 years of life: findings from an Australian birth cohort study. J Hum Nutr Diet. 28, 375–383 doi:10.1111/jhn.12313
References
- 1. Conn JA, Davies MJ, Walker RB et al., (2009) Food and nutrient intakes of 9‐month‐old infants in Adelaide, Australia. Public Health Nut 12, 2448–2456. [DOI] [PubMed] [Google Scholar]
- 2. National Health and Medical Research Council (2012) Infant Feeding Guidelines Australia. Canberra, ACT: National Health and Medical Research Council. [Google Scholar]
- 3. Schwartz C, Scholtens PA, Lalanne A et al., (2011) Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite 57, 796–807. [DOI] [PubMed] [Google Scholar]
- 4. Birch LL & Doub AE (2014) Learning to eat: birth to age 2 y. Am J Clin Nutr 99, 723S–728S. [DOI] [PubMed] [Google Scholar]
- 5. Wu TC & Chen PH (2009) Health consequences of nutrition in childhood and early infancy. Pediatr Neonatal 50, 135–142. [DOI] [PubMed] [Google Scholar]
- 6. Palmer CA, Kent R Jr, Loo CY et al., (2010) Diet and caries‐associated bacteria in severe early childhood caries. J Dent Res 89, 1224–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Health and Medical Research Council (2013) Australian Dietary Guidelines. Canberra, ACT: National Health and Medical Research Council. [Google Scholar]
- 8. Byrne R, Magarey A & Daniels L (2014) Food and beverage intake in Australian children aged 12‐16 months participating in the NOURISH and SAIDI studies. Aust N Z J Public Health 38, 326–331. [DOI] [PubMed] [Google Scholar]
- 9. Webb K, Rutishauser I & Knezevic N (2008) Foods, nutrients and portions consumed by a sample of Australian children aged 16‐24 months. Nutr Diet 65, 56–65. [Google Scholar]
- 10. Webb KL, Lahti‐Koski M, Rutishauser I et al (2005) Consumption of ‘extra’ foods (energy‐dense, nutrient poor) among children aged 16‐24 months from western Sydney Australia. Public Health Nutr 9, 1035–1044. [DOI] [PubMed] [Google Scholar]
- 11. Golley RK, Smithers LG, Mittinty MN et al (2012) An index measuring adherence to complementary feeding guidelines has convergent validity as a measure of infant diet quality. J Nutr 142, 901–908. [DOI] [PubMed] [Google Scholar]
- 12. Bell LK, Golley RK, Daniels L et al (2013) Dietary patterns of Australian children aged 14 and 24 months, and associations with socio‐demographic factors and adiposity. Eur J Clin Nutr 67, 638–645. [DOI] [PubMed] [Google Scholar]
- 13. Chan L, Magarey AM & Daniels LA (2011) Maternal feeding practices and feeding behaviors of Australian children aged 12‐36 months. Matern Child Health J 15, 1363–1371. [DOI] [PubMed] [Google Scholar]
- 14. Lioret S, McNaughton SA, Spence AC et al (2013) Tracking of dietary intakes in early childhood: the Melbourne InFANT Program. Eur J Clin Nutr 67, 275–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Scott JA, Binns CW, Graham KI et al (2009) Predictors of the early introduction of solid foods in infants: results of a cohort study. BMC Pediatr 9, 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Graham VA, Gibbons K, Marraffa C et al (1998) Filling the gap: weaning practices of children aged 0‐2 years in western metropolitan Melbourne. J Paediatr Child Health 34, 513–517. [DOI] [PubMed] [Google Scholar]
- 17. Australian Institute of Health and Welfare (2011) Australian National Infant Feeding Survey Indicator Results. Canberra, ACT: Australian Institute of Health and Welfare. [Google Scholar]
- 18. de Silva‐Sanigorski AM, Calache H, Gussy M et al (2010) The VicGeneration study – a birth cohort to examine the environmental, behavioural and biological predictors of early childhood caries: background, aims and methods. BMC public health 10, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carpenter L, Boak R. & Porter J. et al eds. Reliability and validity of a food frequency questionnaire with six month to six year old children Nutrition Society of Australia Annual Scientific Meeting 2014 Hobart, Tasmania, Australia.
- 20. Baxter J. (2008) Breastfeeding, Employment and Leave. Canberra, ACT: Family Matter: Australian Institute of Family Studies. Canberra, Australia. [Google Scholar]
- 21. Australian Bureau of Statistics (2009) National Health Survey Summary of Results 2007–2008. Canberra, ACT: Australian Bureau of Statistics. Canberra, Australia. [Google Scholar]
- 22. Department of Education and Early Childhood Development (2010) The State of Victoria's Children. Melbourne, Vic.: Department of Education and Early Childhood Development, Melbourne, Australia. [Google Scholar]
- 23. Ambrosini GL (2014) Childhood dietary patterns and later obesity: a review of the evidence. Proc Nutr Soc 73, 137–146. [DOI] [PubMed] [Google Scholar]
- 24. National Health and Medical Research Council (2003) Australian Dietary Guidelines for Children and Adolescents in Australia. Canberra, ACT: National Health and Medical Research Council. [Google Scholar]


