Background:
Effective demand creation strategies are needed to increase uptake of medical male circumcision and reduce new HIV infections in eastern and southern Africa. Building on insights from behavioral economics, we assessed whether providing compensation for opportunity costs of time or lottery-based rewards can increase male circumcision uptake in Kenya.
Methods:
Uncircumcised men aged 21–39 years were randomized in 1:1:1 ratio to 2 intervention groups or a control group. One intervention group was offered compensation of US $12.50 conditional on circumcision uptake. Compensation was provided in the form of food vouchers. A second intervention group was offered the opportunity to participate in a lottery with high-value prizes on undergoing circumcision. The primary outcome was circumcision uptake within 3 months.
Results:
Among 903 participants enrolled, the group that received compensation of US $12.50 had the highest circumcision uptake (8.4%, 26/308), followed by the lottery-based rewards group (3.3%, 10/302), and the control group (1.3%, 4/299). Logistic regression analysis showed that compared with the control group, the fixed compensation group had significantly higher circumcision uptake [adjusted odds ratio 7.1; 95% CI: 2.4 to 20.8]. The lottery-based rewards group did not have significantly higher circumcision uptake than the control group (adjusted odds ratio 2.5; 95% CI: 0.8 to 8.1).
Conclusions:
Providing compensation was effective in increasing circumcision uptake among men over a short period. The results are consistent with studies showing that such interventions can modify health behaviors by addressing economic barriers and behavioral biases in decision making. Contrary to findings from studies of other health behaviors, lottery-based rewards did not significantly increase circumcision uptake.
Trial Registration:
Registry for International Development Impact Evaluations: RIDIE-STUDY-ID-530e60df56107.
Key Words: male circumcision, demand creation, economic interventions, lottery-based rewards, behavioral economics
INTRODUCTION
Male circumcision is considered a vital part of combination HIV-prevention programs in high prevalence regions of sub-Saharan Africa. After the results of 3 randomized controlled trials,1–3 a number of countries have been scaling-up voluntary medical male circumcision (VMMC) services. Models show that for these countries to achieve 80% circumcision prevalence among HIV-uninfected men between the ages of 15–49 years, a total of 20.2 million circumcisions will need to be performed by 2016.4 The benefits of such a rapid scale-up male circumcision include 3.4 million averted HIV infections and savings of US $16.5 billion in treatment costs.5 Despite significant support from donor organizations and partner countries, however, the number of VMMCs performed in many countries has been well below targets.4,6 Although circumcision uptake is high among adolescents in several countries, demand is low among adult men—a group that is essential to reach to maximize the population-level HIV-prevention benefits of VMMC. Even in Kenya, where high circumcision prevalence has been achieved with VMMC scale-up, circumcision uptake has been considerably lower among men aged >20 years than among younger men.7,8 There is thus a vital need for novel demand creation strategies.4,9
Previous studies have identified multiple barriers to VMMC uptake in eastern and southern Africa. These barriers include the fear of pain, concerns about the period of sexual abstinence after circumcision, female partner's resistance, and cultural factors.10–13 Another commonly reported barrier, particularly for working-age men, has been concern about lost wages on the day of the circumcision procedure and days after the procedure when early stages of wound healing may limit the ability to perform work, particularly in the informal employment sector.10,11 Because many of the costs associated with circumcision are largely immediate, whereas the benefits are in the future, low uptake could also result from men discounting the future significantly or making decisions largely on the basis of immediate costs and benefits (present-biased preferences).14,15 Economic interventions may help overcome some of these barriers to male circumcision. A recent study we conducted in Kenya found that compensation for lost wages significantly increased circumcision uptake among 25–49-year-old men.16 This is consistent with evidence that conditional cash transfers and the provision of in-kind compensation can promote health behaviors in low-income countries.17–20 Other studies conducted in high-income countries have used behavioral economics insights21,22 and found that lottery-based rewards can motivate changes in health behavior.23
We conducted a randomized trial in Kenya to compare 2 demand creation interventions for VMMC among men aged 21–39 years. One intervention provided men compensation conditional on VMMC uptake and another offered men the opportunity to receive lottery-based rewards conditional on VMMC uptake.
METHODS
Ethical Considerations
The study received approval from the Office of Human Research Ethics at the University of North Carolina at Chapel Hill and the Ethical Review Committee at the Kenya Medical Research Institute.
Study Setting
The study took place within greater Nyando district in the Nyanza region of western Kenya. Adult HIV prevalence in Kisumu County, which includes the study area, is estimated to be 18.7%.24 Primary occupations for men in the study area included farming, fishing, and other forms of skilled and casual labor. The study area was selected because circumcision prevalence among adult men remained well below the target of 80%.16 The study was implemented in partnership with Impact Research and Development Organization, the largest VMMC service delivery organization in Kenya and primary provider of VMMC services in the study area.
Study Design and Participants
Of 30 sublocations that were not adjacent to or part of those where our previous demand creation study took place,16 we randomly selected 7 sublocations for enrollment of study participants. Between April 28, 2014 and September 10, 2014, trained research assistants went to all households in the selected sublocations and sought to enroll men who met the following eligibility criteria: self-reported age between 21 and 39 years, self-reported to be uncircumcised, and no intention to leave study area in next 4 months. In households where multiple men met eligibility criteria, one person was randomly chosen for enrollment. After informed consent for the study, eligible participants were administered a questionnaire, provided with information about the risks and benefits of VMMC, and then randomized in a 1:1:1 ratio to 3 study groups. Randomization was performed using computer-generated scratch cards and balanced block randomization. Scratch cards were offered to participants sequentially and revealed the study group assignment to the participant and research assistant simultaneously. These scratch cards also contained participants' preprinted study identification number and served as referral cards for circumcision.
Interventions
All participants received information about 4 Impact Research and Development Organization clinics in the study area where VMMC services were available free-of-charge. Participants in the control group were offered compensation of Kenya Shillings (KES) 50 (US $0.60) if they came for circumcision at one of the clinics within 3 months. Participants randomized to the 2 intervention groups were either offered fixed compensation or lottery-based rewards.
Fixed Compensation Group
Participants were informed they would receive a fixed amount of economic compensation (in the form of a food voucher worth KES 1000, or US $12.50) if they underwent circumcision at one of the VMMC clinics within 3 months. This amount approximated 2–3 days of wages for most men. The amount selected was in the range of the amount proven effective in the previous study we conducted.16 The vouchers listed 4 shops in the study area where food items could be redeemed.
Lottery-Based Rewards Group
Participants were informed they would be given the opportunity to participate in a lottery if they underwent male circumcision at one of the VMMC clinics within 3 months. This lottery was designed to have an identical expected value as the fixed compensation amount of US $12.50 and participants were informed about the prizes and probabilities of winning them. Participants were told that “1 in 20” (5%) would win a bicycle or a smartphone (value of KES 9500, or US $120), “2 in 20” (10%) would win a standard mobile phone or pair of shoes (value KES 3600 or USD $45), and that the remaining 17 in 20 (or 85%) would receive compensation in the form a food voucher worth KES 200 (US $2.50).
Compensation offers were valid for 3 months because we sought to rapidly assess the efficacy of the interventions. At 1 and 2 months after enrollment, participants received brief mobile phone–based text messages reminding them of the time remaining to go for circumcision to receive compensation as part of the study.
VMMC Uptake Data Collection
VMMC uptake was monitored at study clinics until December 10, 2014. All participants who underwent male circumcision at the study clinics were asked to present the scratch cards issued to them at enrollment to clinic-based research assistants. These research assistants also verified the circumcision procedure was performed by consulting with clinic surgeons. They then provided participants the compensation corresponding to their study group. Participants in the lottery-based rewards group received a lottery card that instantly revealed the prize, which was then given to them by research assistants.
Statistical Analyses
The main outcome analyzed was VMMC uptake within 3 months of enrollment. VMMC uptake in each intervention group was compared with the control group using logistic regression, and a Wald test was performed to compare effect sizes for the fixed compensation and lottery-based rewards groups. We also estimated models that adjusted for participants' age, educational attainment, marital status, and wealth.
In addition, we compared the effect of lottery-based rewards relative to fixed compensation among participant subgroups with different demographic characteristics, income, and self-reported sexual behavior. We were particularly interested in determining whether participants who self-reported higher risk sexual behavior were more likely to uptake VMMC when offered lottery-based rewards, with rationale that risk-seeking men would find the lottery-based rewards more appealing. These analyses included significance testing of the subgroup-intervention interaction term in logistic regression models. All statistical tests analyses were performed using Stata version 13.1.
The planned sample size for the trial was 900, with 300 participants in each study group. Power calculations indicated that with 300 participants in each study group and 2% VMMC uptake in the control group, there would be 90% power to detect a difference in uptake as small as 7% and 80% power to detect a difference in uptake as small as 6%.
RESULTS
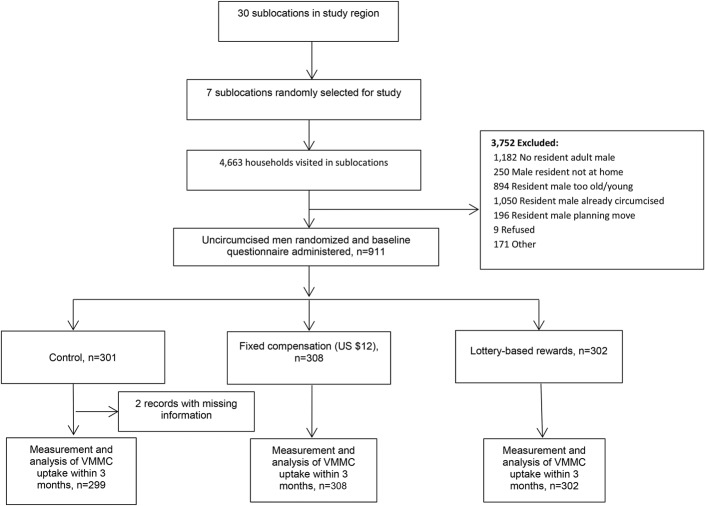
Figure 1 describes the participant recruitment and randomization. A total of 4663 households were enumerated and 3752 (80.5%) of them were excluded for various reasons: no resident adult male (1182, 31.5%), resident adult male reported already being circumcised (1050, 28.0%), did not meet self-reported age criteria (894, 23.8%), planned to move within 4 months (196, 5.2%), not at home (250, 6.7%), or refused to participate (9, 0.2%). Enrollment and randomization occurred in 911 households.
FIGURE 1.
Study flowchart.
Baseline Data
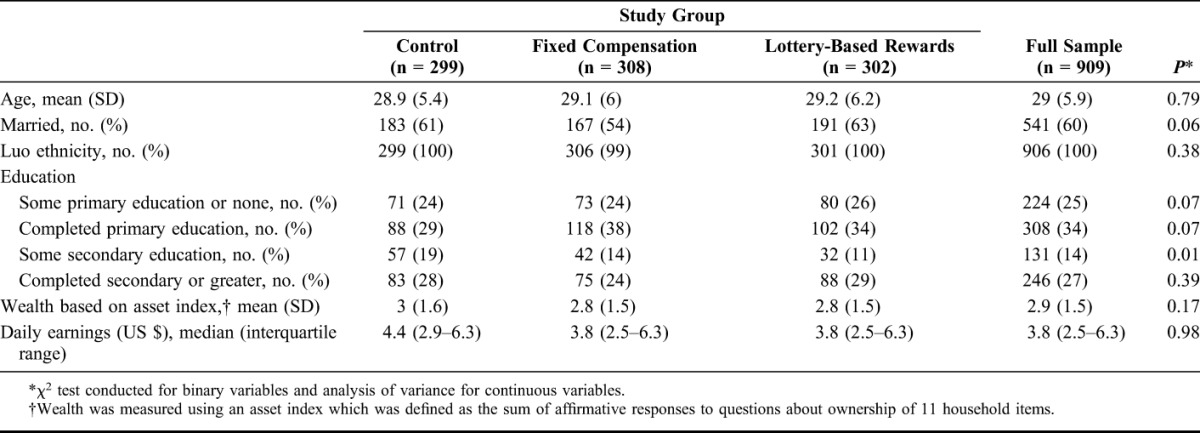
Table 1 summarizes demographic and socio-economic characteristics of study participants. The mean age of participants was 29 years and 60% were married. The proportion of participants who reported completing some secondary education differed significantly among the 3 groups, from 19% in the control group to 11% in the lottery-based rewards group. Many participants reported being economically active; the median of daily earnings was US $3.80 (interquartile range, US $2.50–$6.30).
TABLE 1.
Baseline Characteristics of Study Participants
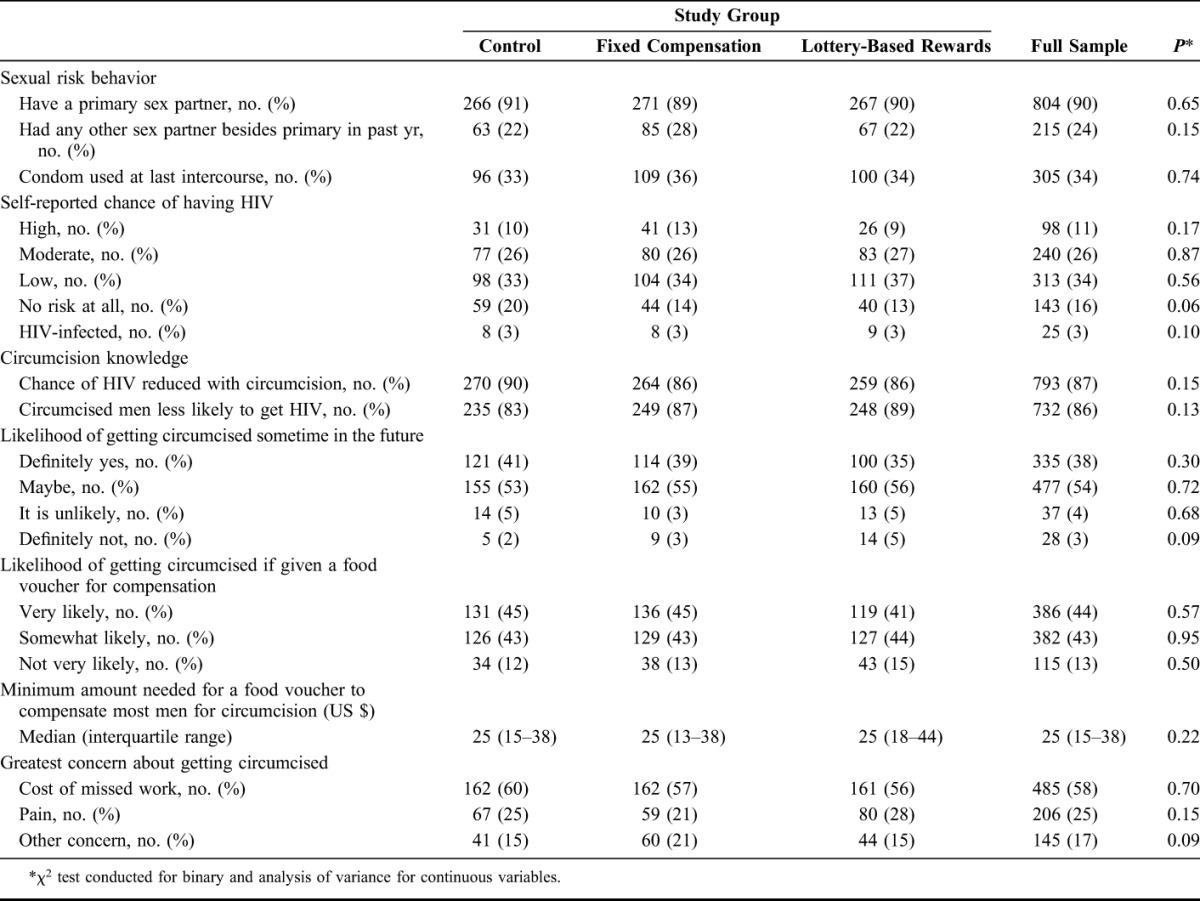
Participants' self-reported sexual behavior and male circumcision attitudes were similar across the 3 study groups (Table 2). Overall, 90% of participants reported having a primary sexual partner and 24% reported having a sexual partner in addition to their primary partner in the past year. Many participants felt that they were at high or moderate risk of acquiring HIV (37%). Nearly 90% of participants had knowledge of the benefits of circumcision at baseline and 38% indicated they were definitely likely to get circumcised sometime in the future (54% said “maybe”). Most of the participants (58%) reported the possibility of being unable to work temporarily as their greatest concern about getting circumcised; 25% reported fear of pain, and 17% reported other factors.
TABLE 2.
Attitudes Related to Demand for VMMC and Self-Reported Sexual Behavior
Effect on VMMC Uptake
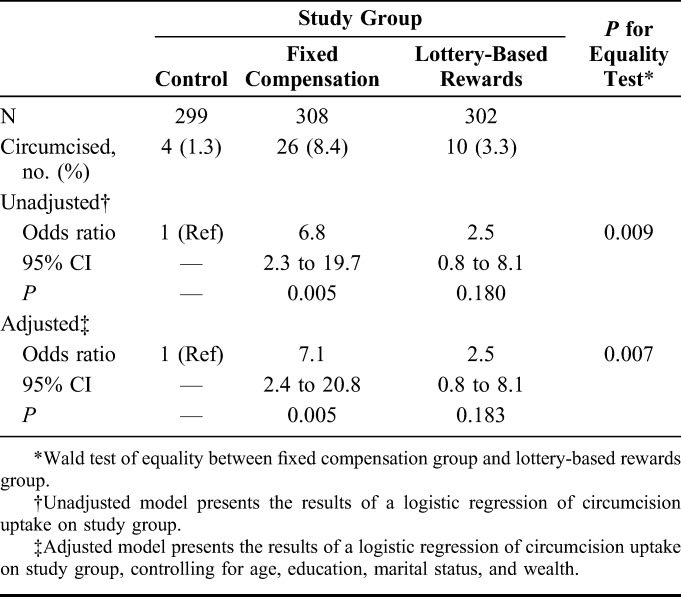
Table 3 shows that VMMC uptake in the 3 months after enrollment was higher among participants randomized to receive fixed compensation (26/308, 8.4%) and lottery-based rewards (10/302, 3.3%) than in the control group (4/299, 1.3%). Logistic regression analysis of VMMC uptake indicated that compared with the control group, the fixed compensation group was significantly more likely to get circumcised [odds ratio 6.8; 95% CI: 2.3 to 19.7]. The lottery-based rewards group, however, was not significantly more likely to uptake VMMC (odds ratio 2.5; 95% CI: 0.8 to 8.1). Effect sizes for the fixed compensation and lottery-based rewards groups differed significantly (P = 0.009). Results were similar after controlling for demographic and economic characteristics; the fixed compensation group has significantly higher VMMC uptake than the control group [adjusted odds ratio 7.1; 95% CI: 2.4 to 20.8], whereas the lottery-based rewards group did not (adjusted odds ratio 2.5; 95% CI: 0.8 to 8.1), respectively.
TABLE 3.
Effects of Economic Interventions on VMMC Uptake Within 3 Months
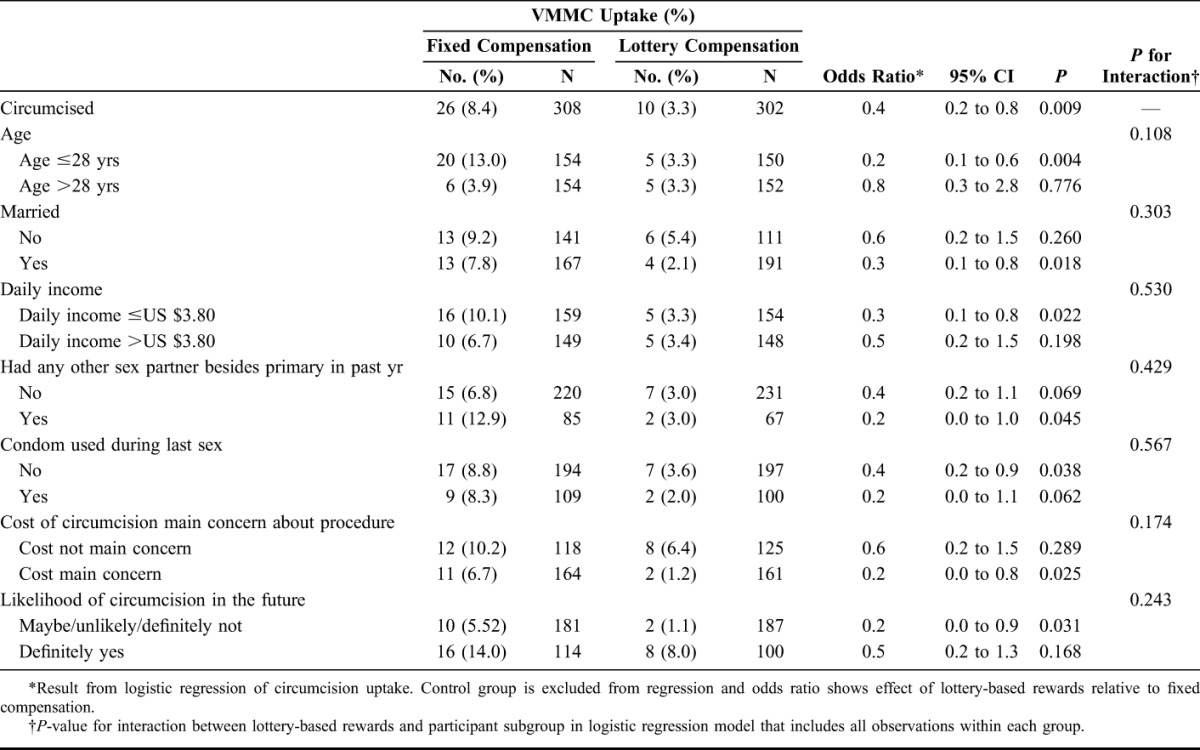
Results from subgroup analyses are presented in Table 4. Among most subgroups we examined, the lottery-based rewards group had significantly lower circumcision uptake as well. This was true for participants who were aged ≤28 years, married, and earned a below-median daily wage. Among participants who self-reported higher risk sexual behaviors at baseline, the lottery-based rewards group also had significantly lower circumcision uptake than the fixed compensation group. However, we could not reject the hypothesis that the effect of lottery-based rewards relative to fixed compensation was significantly different between the subgroups, as indicated by the P-values for the interaction terms between the fixed compensation group and lottery-based rewards group.
TABLE 4.
Comparison of Lottery-Based Rewards to Fixed Compensation Among Participant Subgroups
DISCUSSION
This study adds to an emerging evidence base on demand creation strategies for male circumcision in sub-Saharan Africa. Among 21–39-year-old men, providing compensation for lost wages conditional on undergoing circumcision was effective in increasing circumcision uptake within 3 months. Offering lottery-based rewards, however, did not result in significantly higher male circumcision uptake.
The results of providing fixed compensation are highly consistent with those from a randomized controlled trial we conducted previously in the same region of Kenya.16 In that study, providing compensation of US $8.75 and US $15 led to similar increases in circumcision uptake among 25–49-year-old men. Circumcision uptake in US $8.75 and US $15 study groups was 6.6% and 9.0%, respectively; proportions that are comparable to uptake among participants offered US $12.50 in this study (8.4%). The effect sizes relative to the control groups in each study were also very similar. This study therefore provides further evidence that providing compensation can be an effective strategy for increasing circumcision prevalence among adult men.
Another important result in this study is that offering lottery-based rewards did not lead to a significant increase in circumcision uptake relative to providing a fixed amount of compensation. This is partly at odds with the behavioral economics rationale for the intervention, which includes the theory that individuals place greater decision weights on low probability events and that they may not be very motivated by small economic rewards.21,22 Several explanations can be offered for this result. First, the lottery-based rewards intervention, in contrast to fixed compensation, did not guarantee payments that would defray the costs of circumcision uptake. Qualitative interviews conducted with some participants in the lottery-based rewards group and baseline data on barriers to VMMC provide support for this explanation. Second, participants were risk averse and as such, in accordance with expected utility theory, the uncertain rewards may not have appealed to them as much as compensation with certainty. It is noteworthy that even in subgroup analyses of participants who engaged in riskier sexual behavior, and thus might have been more risk-seeking, we did not find the lottery-based rewards to be effective. This latter finding should be interpreted with caution given limited statistical power. Other explanations follow from the specific design of the lottery-based rewards. Prizes awarded may not have been sufficiently attractive (cash prizes or different items may have been preferred, for example) or there might be inadequate trust in the intervention because few prizes were awarded because of low VMMC uptake.
Although lottery-based rewards have been used in the United States to modify health behaviors,23 few studies have tested their effectiveness in low-income settings or directly compared their effectiveness to fixed compensation. Our findings are consistent with those from a recent study in the United Kingdom that compared lotteries with vouchers, in this case to promote chlamydia screening among young people.25 Vouchers worth ₤5 were more effective in increasing screening than lottery-based rewards. Given the limited evidence base from sub-Saharan Africa, however, further testing of lottery-based rewards is needed. Future efforts to implement lottery-based rewards may also benefit greatly from additional pretesting of prizes and community-based promotion to generate interest in the intervention.
The levels of circumcision uptake observed in this study also underscore that compensation provision alone is insufficient for achieving high circumcision uptake. Some participants may have chosen to undergo circumcision if the intervention remained active for longer than 3 months, if compensation amounts were slightly higher—as suggested by participants' reports of the amount needed to compensate for lost wages—or if compensation was provided as cash. However, it is also likely that other important barriers may explain limited VMMC uptake among this group and that other demand creation interventions are needed.
This study has several limitations. First, this study did not compare the effectiveness of providing compensation in alternative ways such as cash, mobile money, or other forms of in-kind compensation. Some of these modes of compensation may have larger impacts on VMMC uptake and require testing. Second, owing to the small number of participants who became circumcised in the lottery-based rewards group, this study lacked statistical power to test the theory that participants with greater risk tolerance would find lottery-based rewards more appealing than fixed compensation. Finally, the intervention was implemented in a setting where circumcision prevalence is high and those who are uncircumcised represent the “hardest to reach” segments of the population. Testing the effectiveness of the intervention in other settings where early demand creation efforts have not yielded high circumcision prevalence would be worthwhile.
From a programmatic standpoint, the interventions tested here could be implemented on a larger scale by promoting them through mass media or facility- and community-based events rather than door-to-door visits. As with all demand creation interventions, the costs of the interventions also require careful consideration. Providing compensation is particularly promising in this regard because most of the costs would only be incurred if and when circumcisions are performed. Incurring such demand creation costs is likely to be highly cost-effective when considering the HIV infections averted by multiple male circumcisions5 and the efficiency gains from higher demand.
Using economic interventions to promote health behaviors also raises several ethical considerations. There are several reasons why providing compensation may not be ethically problematic. First, the modest amounts we used compensated men for costs they would likely incur as a result of becoming circumcised—a finding that was verified based on participants' daily earnings and qualitative interviews conducted in a companion study.26 Second, among the participants who reported at the outset that they were unlikely to get circumcised in the future, there were none who became circumcised during the study when compensation or lottery rewards were offered. This suggests that the intervention reached primarily those contemplating getting circumcised and further reduces concerns about coercion. Finally, the provision of compensation or lottery-based rewards may nudge participants toward undertaking a health decision they already favored or may have been about to undertake, thereby promoting individual autonomy in health decisions.27–29
In resource-limited settings, economic factors such as lost wages and opportunity costs of time are likely to be important barriers for VMMC uptake and other health behaviors. As such, it is likely that interventions such as compensation provision would be effective outside Kenya as well. At the same time, interventions that address other important barriers to VMMC will also be needed to achieve high levels of circumcision prevalence. The results from this study reveal that low-cost interventions such as compensation provision can significantly increase VMMC uptake. They also provide scientific evidence on the relative effectiveness of different types of economic interventions for promoting health behavior.
Footnotes
The study was funded by the International Initiative for Impact Evaluation (3ie). HT acknowledges support from the National Institute for Child Health and Human Development (grant no. K01HD061605).
The authors have no conflicts of interest to disclose.
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the article; and decision to submit the article for publication.
REFERENCES
- 1.Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–666. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–656. [DOI] [PubMed] [Google Scholar]
- 4.Sgaier SK, Reed JB, Thomas A, et al. Achieving the HIV prevention impact of voluntary medical male circumcision: lessons and challenges for managing programs. PLoS Med. 2014;11:e1001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Njeuhmeli E, Forsythe S, Reed J, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med. 2011;8:e1001132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hankins C, Forsythe S, Njeuhmeli E. Voluntary medical male circumcision: an introduction to the cost, impact, and challenges of accelerated scaling up. PLoS Med. 2011;8:e1001127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mwandi Z, Murphy A, Reed J, et al. Voluntary medical male circumcision: translating research into the rapid expansion of services in Kenya, 2008–2011. PLoS Med. 2011;8:e1001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galbraith JS, Ochieng A, Mwalili S, et al. Status of voluntary medical male circumcision in Kenya: findings from 2 nationally representative surveys in Kenya, 2007 and 2012. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S37–S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gray RH, Wawer MJ, Kigozi G. Programme science research on medical male circumcision scale-up in sub-Saharan Africa. Sex Transm Infect. 2013;89:345–349. [DOI] [PubMed] [Google Scholar]
- 10.Westercamp N, Bailey RC. Acceptability of male circumcision for prevention of HIV/AIDS in sub-Saharan Africa: a review. AIDS Behav. 2007;11:341–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herman-Roloff A, Otieno N, Agot K, et al. Acceptability of medical male circumcision among uncircumcised men in Kenya one year after the launch of the national male circumcision program. PLoS One. 2011;6:e19814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herman-Roloff A, Llewellyn E, Obiero W, et al. Implementing voluntary medical male circumcision for HIV prevention in Nyanza Province, Kenya: lessons learned during the first year. PLoS One. 2011;6:e18299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ssekubugu R, Leontsini E, Wawer MJ, et al. Contextual barriers and motivators to adult male medical circumcision in Rakai, Uganda. Qual Health Res. 2013;23:795–804. [DOI] [PubMed] [Google Scholar]
- 14.O'Donoghue T, Rabin M. Doing it now or later. Am Econ Rev. 1999;89:103–124. [Google Scholar]
- 15.Hermann K, Van Damme W, Pariyo GW, et al. Community health workers for ART in sub-Saharan Africa: learning from experience–capitalizing on new opportunities. Hum Resour Health. 2009;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thirumurthy H, Masters SH, Rao S, et al. Effect of providing conditional economic compensation on uptake of voluntary medical male circumcision in Kenya. JAMA. 2014;312:703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schultz TP. School subsidies for the poor: evaluating the Mexican progresa poverty program. J Dev Econ. 2004;74:199–250. [Google Scholar]
- 18.Fernald LC, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico's conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow-up study. Lancet. 2009;374:1997–2005. [DOI] [PubMed] [Google Scholar]
- 19.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 2007;298:1900–1910. [DOI] [PubMed] [Google Scholar]
- 20.Banerjee AV, Duflo E, Glennerster R, et al. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ. 2010;340:c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47:263–291. [Google Scholar]
- 22.Weber BJ, Chapman GB. Playing for peanuts: why is risk seeking more common for low-stakes gambles? Organ Behav Hum Decis Process. 2005;97:31–46. [Google Scholar]
- 23.Volpp KG, Loewenstein G, Troxel AB, et al. A test of financial incentives to improve warfarin adherence. BMC Health Serv Res. 2008;8:272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National AIDS Control Council. Kenya AIDS Response Progress Report. Nairobi: National AIDS Control Council; Nairobi, Kenya, 2014. [Google Scholar]
- 25.Niza C, Rudisill C, Dolan P. Vouchers versus lotteries: what works best in promoting Chlamydia screening? A cluster randomized controlled trial. Appl Econ Perspect Policy. 2014;36:109–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evens E, Lanham M, Murray K, et al. Use of economic compensation to increase demand for voluntary medical male circumcision in Kenya: qualitative interviews with male participants in a randomized controlled trial and their partners. J Acquir Immune Defic Syndr. 2016;72:(suppl 4)S316–S320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Donoghue T, Rabin M. Doing it now or later. Am Econ Rev. 1999;89:103–124. [Google Scholar]
- 28.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298:2415–2417. [DOI] [PubMed] [Google Scholar]
- 29.London AJ, Borasky DA, Jr, Bhan A. Improving ethical review of research involving incentives for health promotion. PLoS Med. 2012;9:e1001193. [DOI] [PMC free article] [PubMed] [Google Scholar]