Background:
Quality of life (QoL) is an important outcome in plastic surgery. However, authors use different scales to address this subject, making it difficult to compare the outcomes. To address this discrepancy, the aim of this study was to perform a systematic review and a random effect meta-analysis.
Methods:
The search was made in two electronic databases (LILACS and PUBMED) using Mesh and non-Mesh terms related to aesthetic plastic surgery and QoL. We performed qualitative and quantitative analyses of the gathered data. We calculated a random effect meta-analysis with Der Simonian and Laird as variance estimator to compare pre- and postoperative QoL standardized mean difference. To check if there is difference between aesthetic surgeries, we compared reduction mammoplasty to other aesthetic surgeries.
Results:
Of 1,715 identified, 20 studies were included in the qualitative analysis and 16 went through quantitative analysis. The random effect of all aesthetic surgeries shows that QoL improved after surgery. Reduction mammoplasty has improved QoL more than other procedures in social functioning and physical functioning domains.
Conclusions:
Aesthetic plastic surgery increases QoL. Reduction mammoplasty seems to have better improvement compared with other aesthetic surgeries.
Quality of life (QoL) is an important outcome in health sciences. Because plastic surgeons do not deal with mortality and morbidity in aesthetic procedures, patient perception and the impact on QoL become an important outcome.1 More and more, authors have searched for changes in the scores of patient-related outcomes questionnaires after aesthetic surgery. However, studies’ results show a large heterogeneity. Some authors show a small overall improvement, whereas others demonstrate increased scores just in some specific domains of the questionnaires.2–6 This disparateness may be caused because studies use different instruments, have small samples, and also because they analyze different surgeries that might have different improvements.7 To deal with all this information, systematic reviews and meta-analysis are essential tools to create knowledge and bring information to everyone involved in the decision-making process in healthcare. They increase the power of the analysis as they overcome the weaknesses of clinical trials and can be used to compare results from different instruments.8,9
There are very few reviews of QoL and aesthetic surgery, and they only depict the surgeries made and questionnaires that have been used. None of them gathered data and performed a meta-analysis or measured the size effect.10–13 The lack of this kind of information creates a new research field in plastic surgery. Based on this scenario, the authors performed a review of the literature of QoL evaluation in aesthetic surgery and a continuous data meta-analysis.
MATERIALS AND METHODS
Search Strategy
The search included electronic databases and a reference crosschecking process. The studies were identified through PubMed (which encompasses Medline, Premedline, and HealthSTAR) and Lilacs. The PubMed search was run using the Mesh terms: (quality of life) and (mammoplasty or liposuction or rhinoplasty or abdominoplasty). Additionally, the PubMed search was run with non-Mesh terms: (quality of life) and (rhytidoplasty or facial surgery or aesthetic plastic surgery or mastopexy or facial lift). The same process was repeated in the Lilacs database. We chose these terms because we found that they encompass the most common aesthetic procedures according to the American Society of Plastic Surgeons statistics of 2014 (http://www.plasticsurgery.org/Documents/news-resources/statistics/2014-statistics/plastic-surgery-statsitics-full-report.pdf). Language was limited to English, Spanish, Italian, French, and Portuguese. The search was conducted in June 2015. Additionally, the same search process was redone in January 2016 and no other study was included. The list of references of included studies was searched for additional studies without any article included.
Only prospective studies with pre- and postoperative data of aesthetic surgeries from validated QoL questionnaires were included in this review. Trials of plastic surgery after massive weight loss and breast reconstruction were excluded because they were considered reconstructive surgery.
This meta-analysis report methodology was performed according to Preferred Reporting Items for Systematic Reviews and Meta-analyses statement guidelines.14
Data Extraction
Two investigators independently extracted data using a standardized form. Discrepancies were resolved by discussion and, if there was no consensus, the decision was made by a third reviewer. Collected data included the number of subjects, mean and SD of the age, and the type of QoL questionnaire used, along with its statistical parameters (mean, SD, mean variation, variation SD, and p value). As we found different questionnaires, we analyzed each questionnaire to classify the domain according to the Medical Outcome Studies 36-item Short Form Health Survey (SF-36) domains. The SF-36 is well known and widely used in health sciences. This construct is divided in 8 domains, which are role-physical, physical functioning (PF), bodily pain (BP), general health, vitality, social functioning (SF), role-emotional (RE), and mental health. The first 4 domains comprehend the physical summary and the last ones the mental summary.15 The summaries reflect the physical and mental health, respectively. When there was more than one kind of surgery analyzed separately in the study, we considered the results individually in the quantitative analysis. After the qualitative analysis, data were separated and analyzed in 3 different groups. The first group is the overall QoL, which included the studies that have questionnaires with just one reported result (only 1 general domain), the second group is formed with articles that report their results based on both summaries mental and physical, and the third group is formed with studies of the 8 domains of the SF-36. We calculated the standardized mean difference (SMD) between pre- and postoperative QoL among aesthetic surgeries. As the majority of the studies included reduction mammoplasty patients, we compared this procedure with all other aesthetic surgeries together. Efforts were made to reach authors to collect missing data. We made at least three attempts to contact each of the selected articles to review data. Only 3 (15%) replied, 2 (10%) sending their database, and 1 apologizing because he could not find his data.
Statistical Analysis
Summarized results were reported as SMD and 95% confidence interval (95% CI). Authors also performed a random effect meta-analysis with Der Simonian and Laird as variance estimator and used the R software (version 3.1.2, The R Foundation for Statistical Computing), packagemeta version 4.2-0.16
RESULTS
Search results are displayed in Figure 1. All the steps of the systematic review are shown. Of 1,715 studies screened, 20 articles met the inclusion criteria (Table 1) and 16 went through quantitative analysis. There were not enough studies with the Breast-Q, and just 1 article using Euroqol 5 dimensions (EQ-5D); to keep homogeny, we excluded them from the qualitative analysis17–19 and the lack of data prevented us from including another one.20
Fig. 1.
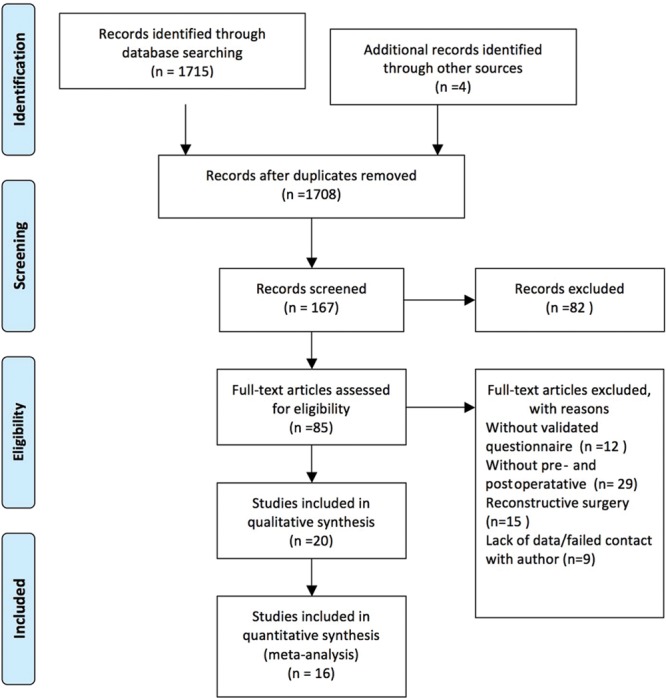
Systematic review flowchart.
Table 1.
Articles Included for Qualitative Analysis According to Surgery
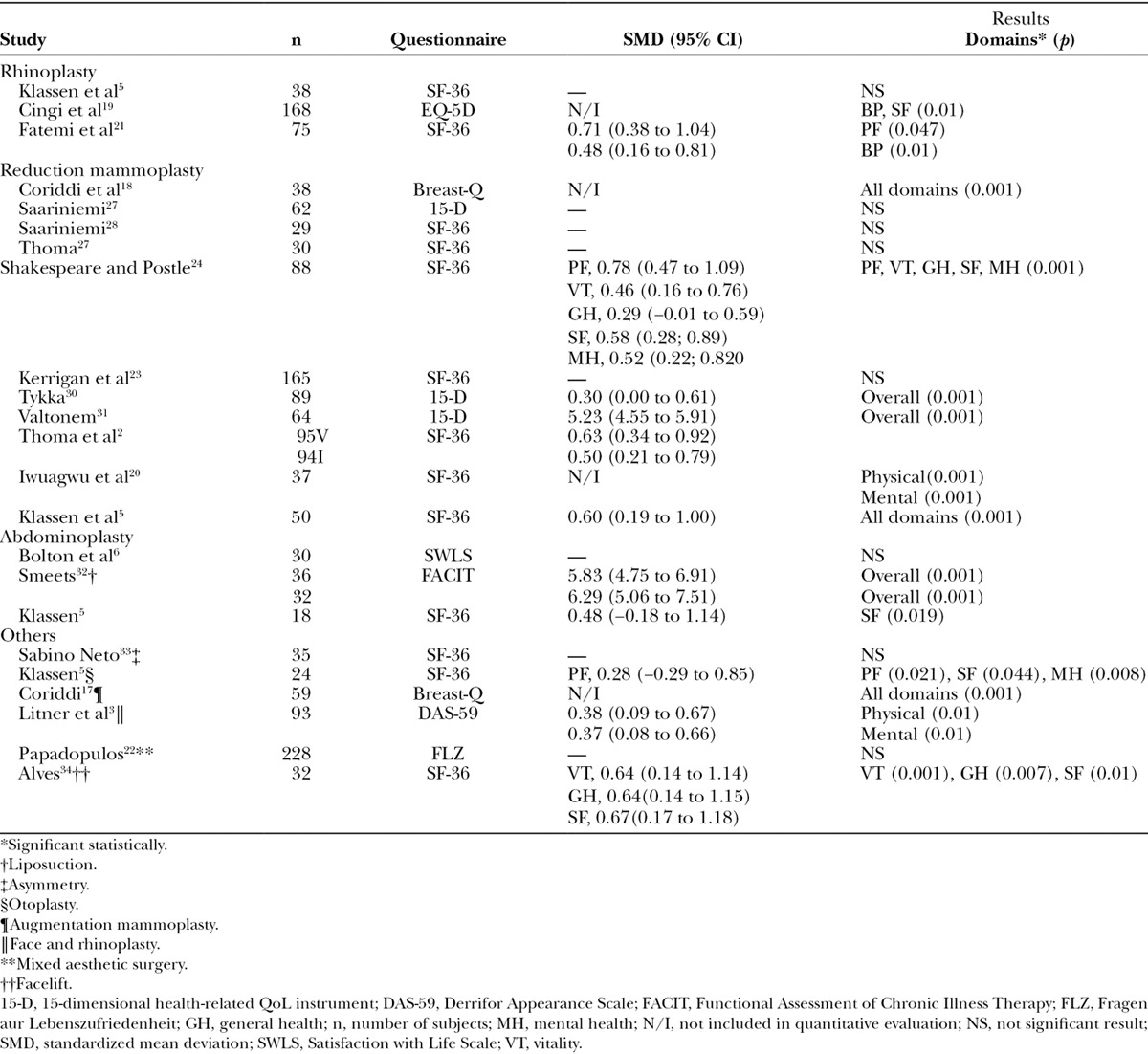
The majority of the authors chose the SF-36 questionnaire (n = 10) to assess QoL. It is a general instrument and largely used in health sciences. Other scales used were Breast-Q (n = 2), Derrifor Appearance Scale (n = 1), 15-dimensional health-related QoL instrument (n = 3), EQ-5D (n = 1), the Satisfaction with Life Scale (n = 1), Functional Assessment of Chronic Illness Therapy (n = 1), and Fragen aur Lebenszufriedenheit (n = 1). Reduction mammoplasty was evaluated in 12 studies, and it was the most common procedure evaluated.
Quantitative analysis is shown in Figures 1 to 4. All 3 groups had improvement in QoL. Reduction mammoplasty showed a statistically higher increase in QoL compared with other aesthetic surgeries in PF and SF domains of SF-36.
Fig. 4.
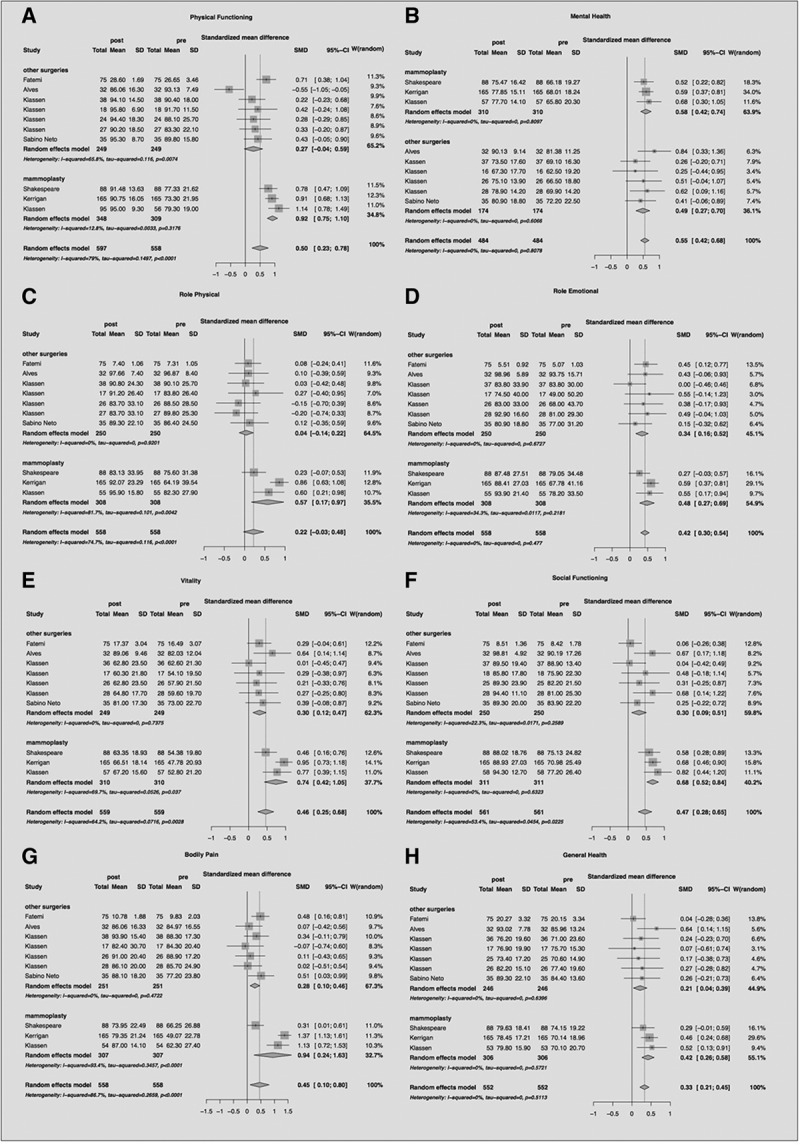
SF-36 domains forest plot. W, weight.
Fig. 2.
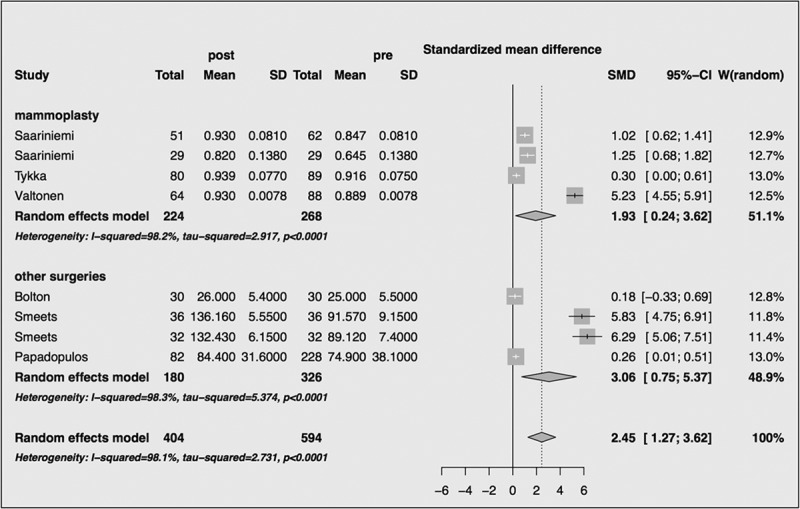
Forest plot of overall group. W, weight.
Fig. 3.
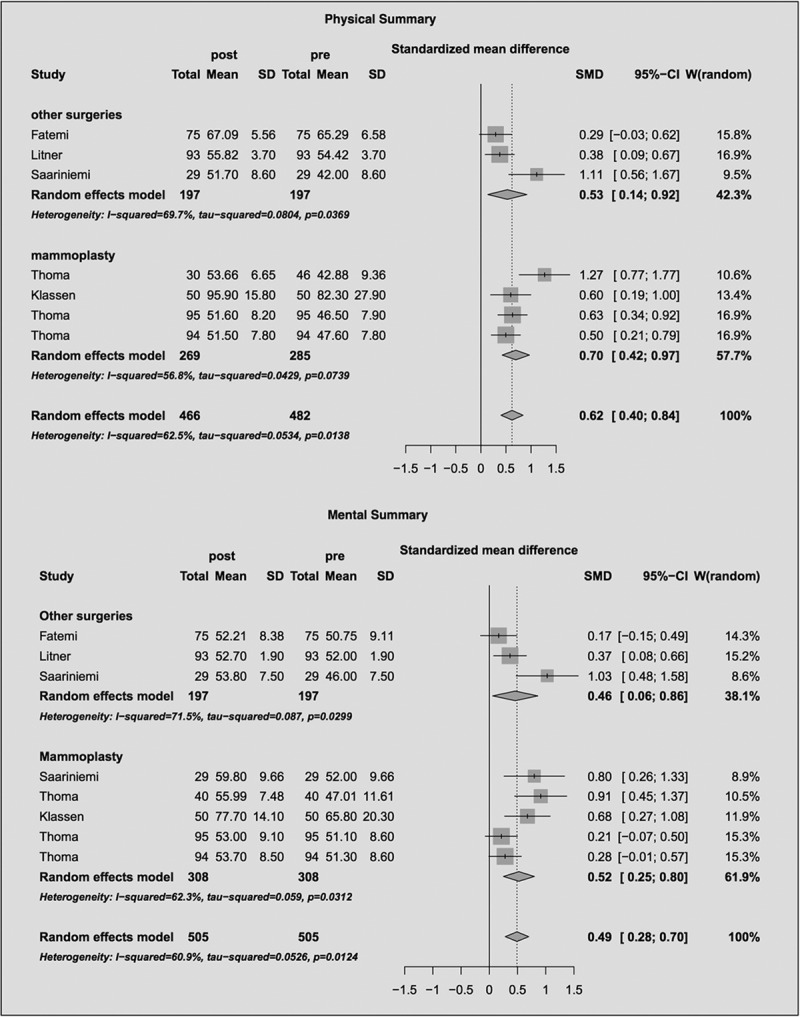
Mental and physical summaries forest plot. W, weight.
DISCUSSION
To our knowledge, this is the first meta-analysis of QoL and aesthetic surgery. Even though there is controversy in the literature,2,6,21,22 our analysis shows that aesthetic plastic surgery improves QoL in overall aspects, even in physical or mental domain. It is an important outcome to assess, to quantify the success of the treatment. Studies identified in our search had sample sizes between 18 and 228 individuals, and only 4 articles have more than 100 subjects.2,19,22,23 Small studies tend to present beta error, so meta-analysis addresses this limitation, increasing the statistical power.
According to our findings, reduction mammoplasty is the most studied aesthetic surgery concerning QoL. As there were few studies with each one of the other aesthetic procedures, it was not possible to compare the differences between each surgery technique. However, we could compare reduction mammoplasty to all other surgeries together.
This review found a lack of standardization of instruments, as we observed that 8 different questionnaires for QoL were used in the selected articles. Only 2 studies used Breast-Q; unfortunately, this prevented us from comparing both specific and generic scales to find out if there is a difference between their capacities to measure the QoL findings. Otherwise, the use of a generic scale such as SF-36 has some advantages; it is the most commonly used instrument in the literature assessing QoL, and it allows comparisons of the effect size to other conditions not related to mammoplasty that may have an important impact on QoL, such as plastic surgeries other than breast procedures, psychiatric conditions, and dermatological disease. Besides, this fact could raise the idea that the impact of aesthetic surgery in QoL has external validity. If it is possible to show improvement using a generic questionnaire, this improvement should not be underestimated.
Our data show that reduction mammoplasty had better improvement in SF and PF domains of SF-36 compared with the other aesthetic surgeries (Fig. 4A, F). Domains’ scores such as BP, vitality, and role-physical (Fig. 4C, E, G) showed a tendency to be higher in mammoplasty; however, this difference did not reach a significant level. In a closer view of these studies, it could be seen that the study of Shakespeare and Postle24 had the lowest scores, forcing down the SMD. New research could address if cultural differences such as body image concerns could explain this discrepancy, as it is a British study, whereas the others are from North America. Another find in this study is that the majority of the patients had been advised to seek mammoplasty by a health professional or because of physical discomfort. Only a few patients had emotional complaints like depression or dissatisfaction with their body.
We also expected that the domains related to physical health would improve more in patients with enlarged breasts because physical symptoms used to be important complaints.25,26 According to our findings, only PF of the physical summary of SF-36 questionnaire showed statistical difference, that is, improved even more in mammoplasty than in other surgeries.
To increase the number of subjects, we had to compare similar domains of different scales to measure QoL. For example, Cingi et al19 (2011) applied the EQ-5D scale and one of its domains is pain/discomfort; we compared this to the BP domain of SF-36. It is possible that we have done some misinterpretation, although this was an alternative to include and compare the data of these studies.
The few studies with other aesthetic surgeries did not allow us to perform comparative analysis between each aesthetic procedure. Such information may help surgeons to be prepared for the patients’ reactions after surgery, because patients undergoing reduction mammoplasty show more satisfaction with the postoperative result compared to liposuction or facelift patients.
CONCLUSIONS
Our study shows that aesthetic plastic surgery improved patients’ QoL. Patient-reported outcomes are a key factor in addressing the effectiveness of plastic surgery. Although most researchers used general health scales of QoL, specific questionnaires should be developed to discriminate peculiarities of each procedure and determine if they are more reliable at addressing QoL in aesthetic plastic surgery. We still need more studies with aesthetic surgeries, other than reduction mammoplasty, to compare the magnitude of different procedures, thereby helping surgeons to understand what aids patients’ health the most.
Footnotes
Disclosure: Dr. Dreher received a governmental fund (CAPES) as a postgraduate Master of Science Degree student. None of the other authors have any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg. 2009;123:98e–106e. doi: 10.1097/PRS.0b013e31819565c1. [DOI] [PubMed] [Google Scholar]
- 2.Thoma A, Ignacy TA, Duku EK, et al. Randomized controlled trial comparing health-related quality of life in patients undergoing vertical scar versus inverted T-shaped reduction mammaplasty. Plast Reconstr Surg. 2013;132:48e–60e. doi: 10.1097/PRS.0b013e3182910cb0. [DOI] [PubMed] [Google Scholar]
- 3.Litner JA, Rotenberg BW, Dennis M, et al. Impact of cosmetic facial surgery on satisfaction with appearance and quality of life. Arch Facial Plast Surg. 2008;10:79–83. doi: 10.1001/archfaci.10.2.79. [DOI] [PubMed] [Google Scholar]
- 4.Coriddi MR, Koltz PF, Chen R, et al. Changes in quality of life and functional status following abdominal contouring in the massive weight loss population. Plast Reconstr Surg. 2011;128:520–526. doi: 10.1097/PRS.0b013e31821b62f0. [DOI] [PubMed] [Google Scholar]
- 5.Klassen A, Jenkinson C, Fitzpatrick R, et al. Patients’ health related quality of life before and after aesthetic surgery. Br J Plast Surg. 1996;49:433–438. doi: 10.1016/s0007-1226(96)90025-9. [DOI] [PubMed] [Google Scholar]
- 6.Bolton MA, Pruzinsky T, Cash TF, et al. Measuring outcomes in plastic surgery: body image and quality of life in abdominoplasty patients. Plast Reconstr Surg. 2003;112:619–625; discussion 626. doi: 10.1097/01.PRS.0000070972.57000.08. [DOI] [PubMed] [Google Scholar]
- 7.von Soest T, Kvalem IL, Roald HE, et al. The effects of cosmetic surgery on body image, self-esteem, and psychological problems. J Plast Reconstr Aesthet Surg. 2009;62:1238–1244. doi: 10.1016/j.bjps.2007.12.093. [DOI] [PubMed] [Google Scholar]
- 8.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 9.Panic N, Leoncini E, de Belvis G, et al. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS One. 2013;8:e83138. doi: 10.1371/journal.pone.0083138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kosowski TR, McCarthy C, Reavey PL, et al. A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. 2009;123:1819–1827. doi: 10.1097/PRS.0b013e3181a3f361. [DOI] [PubMed] [Google Scholar]
- 11.Jones SA, Bain JR. Review of data describing outcomes that are used to assess changes in quality of life after reduction mammaplasty. Plast Reconstr Surg. 2001;108:62–67. doi: 10.1097/00006534-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Reavey PL, Klassen AF, Cano SJ, et al. Measuring quality of life and patient satisfaction after body contouring: a systematic review of patient-reported outcome measures. Aesthet Surg J. 2011;31:807–813. doi: 10.1177/1090820X11417426. [DOI] [PubMed] [Google Scholar]
- 13.Ching S, Thoma A, McCabe RE, et al. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111:469–480; discussion 481. doi: 10.1097/01.PRS.0000036041.67101.48. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Behmand RA, Tang DH, Smith DJ., Jr Outcomes in breast reduction surgery. Ann Plast Surg. 2000;45:575–580. doi: 10.1097/00000637-200045060-00001. [DOI] [PubMed] [Google Scholar]
- 16.Schwarzer G. Package Meta. The R Foundation for Statistical Computing. 2015 Available at: http://cran.r-project.org/web/packages/meta/index.html. Accessed 2016. [Google Scholar]
- 17.Coriddi M, Angelos T, Nadeau M, et al. Analysis of satisfaction and well-being in the short follow-up from breast augmentation using the BREAST-Q, a validated survey instrument. Aesthet Surg J. 2013;33:245–251. doi: 10.1177/1090820X12472980. [DOI] [PubMed] [Google Scholar]
- 18.Coriddi M, Nadeau M, Taghizadeh M, et al. Analysis of satisfaction and well-being following breast reduction using a validated survey instrument: the BREAST-Q. Plast Reconstr Surg. 2013;132:285–290. doi: 10.1097/PRS.0b013e31829587b5. [DOI] [PubMed] [Google Scholar]
- 19.Cingi C, Songu M, Bal C. Outcomes research in rhinoplasty: body image and quality of life. Am J Rhinol Allergy. 2011;25:263–267. doi: 10.2500/ajra.2011.25.3649. [DOI] [PubMed] [Google Scholar]
- 20.Iwuagwu OC, Walker LG, Stanley PW, et al. Randomized clinical trial examining psychosocial and quality of life benefits of bilateral breast reduction surgery. Br J Surg. 2006;93:291–294. doi: 10.1002/bjs.5234. [DOI] [PubMed] [Google Scholar]
- 21.Fatemi MJ, Rajabi F, Moosavi SJ, et al. Quality of life among Iranian adults before and after rhinoplasty. Aesthetic Plast Surg. 2012;36:448–452. doi: 10.1007/s00266-011-9820-y. [DOI] [PubMed] [Google Scholar]
- 22.Papadopulos NA, Kovacs L, Krammer S, et al. Quality of life following aesthetic plastic surgery: a prospective study. J Plast Reconstr Aesthet Surg. 2007;60:915–921. doi: 10.1016/j.bjps.2007.01.071. [DOI] [PubMed] [Google Scholar]
- 23.Kerrigan CL, Collins ED, Kneeland TS, et al. Measuring health state preferences in women with breast hypertrophy. Plast Reconstr Surg. 2000;106:280–288. doi: 10.1097/00006534-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Shakespeare V, Postle K. A qualitative study of patients’ views on the effects of breast-reduction surgery: a 2-year follow-up survey. Br J Plast Surg. 1999;52:198–204. doi: 10.1054/bjps.1999.3106. [DOI] [PubMed] [Google Scholar]
- 25.Schnur PL, Schnur DP, Petty PM, et al. Reduction mammaplasty: an outcome study. Plast Reconstr Surg. 1997;100:875–883. doi: 10.1097/00006534-199709001-00008. [DOI] [PubMed] [Google Scholar]
- 26.Miller AP, Zacher JB, Berggren RB, et al. Breast reduction for symptomatic macromastia: can objective predictors for operative success be identified? Plast Reconstr Surg. 1995;95:77–83. doi: 10.1097/00006534-199501000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Saariniemi KM, Kuokkanen HO, Rasanen P, Sintonen H, Tukiainen EJ. The cost utility of reduction mammaplasty at medium-term follow-up: a prospective study. J Plast Reconstr Aesthet Surg. 2012;65:17–21. doi: 10.1016/j.bjps.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 28.Saariniemi K, Luukkala T, Kuokkanen H. The outcome of reduction mammaplasty is affected more by psychosocial factors than by changes in breast dimensions. Scand J Surg. 2011;100:105–9. doi: 10.1177/145749691110000207. [DOI] [PubMed] [Google Scholar]
- 29.Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;12:13–26. doi: 10.1097/01.prs.0000263370.94191.90. [DOI] [PubMed] [Google Scholar]
- 30.Tykka E, Rasanen P, Tukiainen E, Asko-Seljavaara S, Heikkila A, Sintonen H, et al. Cost-utility of breast reduction surgery--a prospective study. J Plast Reconstr Aesthet Surg. 2010;63:87–92. doi: 10.1016/j.bjps.2008.08.067. [DOI] [PubMed] [Google Scholar]
- 31.Valtonen JP, Setala LP, Mustonen PK, Blom M. Can the efficacy of reduction mammoplasty be predicted? The applicability and predictive value of breast-related symptoms questionnaire in measuring breast-related symptoms pre- and postoperatively. J Plast Reconstr Aesthet Surg. 2014;67:676–81. doi: 10.1016/j.bjps.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Smeets R, Noah EM, Seiferth NY, Groger A, Bozkurt A, Fuchs PC, et al. Bioelectric impedance analysis and quality of life after body-contouring procedures in plastic surgery. J Plast Reconstr Aesthet Surg. 2009;62:940–5. doi: 10.1016/j.bjps.2007.10.084. [DOI] [PubMed] [Google Scholar]
- 33.Sabino Neto M, Dematte MF, Freire M, Garcia EB, Quaresma M, Ferreira LM. Self-esteem and functional capacity outcomes following reduction mammaplasty. Aesthet Surg J. 2008;28:417–20. doi: 10.1016/j.asj.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Alves MC, Abla LE, Santos Rde A, Ferreira LM. Quality of life and self-esteem outcomes following rhytidoplasty. Ann Plast Surg. 2005;54:511–4; discussion 5–6. doi: 10.1097/01.sap.0000155274.59248.57. [DOI] [PubMed] [Google Scholar]


