Purpose:
The incidence and cost of nonmelanoma skin cancers are skyrocketing. Five million cases cost $8.1 billion in 2011. The average cost of treatment per patient increased from $1000 in 2006 to $1600 in 2011. We present a study of the economics and costs of skin cancer management in Medicare patients.
Methods:
We studied data released by the Centers for Medicare and Medicaid Services in 2014. Treatment modalities for the management of skin cancer were reviewed, and costs of treatment were quantified for a sample of 880,000 providers.
Results:
Review of Medicare payment records related to the management of skin cancer yielded data from over 880,000 health care providers who received $77 billion in Medicare payments in 2012. From 1992 to 2009, the rate of Mohs micrographic surgery (MMS) has increased by 700%, and these procedures typically have Medicare payments 120% to 370% more than surgical excision, even when including pathology fees. From 1992 to 2009, MMS increased by 700%, whereas surgical excisions increased by only 20%. In 2009, 1800 providers billed Medicare for MMS; in 2012, that number increased to 3209. On average, 1 in 4 cases of skin cancer is treated with MMS.
Conclusion:
Mohs excision is more expensive than surgical excision in an office setting. Procedures requiring the operating room are much more expensive than office procedures. In an era of high deductible health plans, patients’ financial burden is much less with simple excisions of skin cancers done in a clinic when compared with Mohs surgery or operative interventions.
In 2006, an average of 3.4 million nonmelanoma skin cancers (NMSCs) were diagnosed in the United States. By 2011, 4.9 million NMSCs were diagnosed, a 144% increase. One in 5 Americans will develop skin cancer in a lifetime.1
Plastic surgeons play an important role in the management of skin cancer. According to statistics of the American Society of Plastic Surgeons, tumor removal makes up a significant portion of all plastic surgery practices and is the most common reconstructive procedure that is performed.2
The purpose of this study is to provide readers with an appropriate medical and financial understanding of surgical skin cancer management. Our goal is to better facilitate improved clinical care while minimizing the financial burden of our patients. This article will complete the following: (1) review the surgical treatment for NMSC; (2) review comparative effectiveness of different surgical modalities; (3) review the economic impact of surgical NMSC treatment; and (4) review the costs related to skin cancer treatment.
SURGICAL TREATMENT FOR NMSC
The treatment of NMSC is multifaceted. A comprehensive review of treatments is beyond the scope of this article. Readers are advised to review an excellent overview by Rogers and Bentz.3 The 2 surgical treatment modalities are surgical excision (SE) and Mohs micrographic surgery (MMS), also sometimes called micrographic surgery.4 These treatments are different from the nonsurgical treatments because they provide histologic examination of margins. A review of the literature for SE shows cure rates of 90% to 98% for basal cell cancer (BCC) and squamous cell (SCC) cancer.4 The National Comprehensive Cancer Network (NCCN) currently recommends 4-mm margins for BCC and 4- to 6-mm margins for SCC. Pathology examination for SE is with “bread loafing,” where slices out of a specimen are assessed. The challenge with this method of processing is that the entire margin is unable to be assessed. Frederick Mohs, a surgeon at the University of Wisconsin in Madison, Wisc., first developed MMS. In MMS, the physician who performs the excision and the pathologic analysis is one and the same. Five-year cure rates have been reported as high as 99% for BCC and 97% for SCC. The main advantage of MMS over SE is in the pathologic assessment. Mohs specimens are removed at a 45-degree angle, allowing for 100% of the margin of the specimen to be processed, whereas bread loafing only allows for portions of the specimen to be assessed.
DETERMINING THE APPROPRIATE TREATMENTS: EXCISION VERSUS MMS
In 2012, a coalition of physicians issued a comprehensive report of appropriate criteria for the use of MMS. This was a compilation of 70 experts, including dermatologists and Medicare care organizations. Over 200 scenarios were reviewed, which were to encompass 85% of all clinical situations, including 69 scenarios involving BCC and 143 scenarios involving SCC. Of more than 200 clinical situations, 83% of all scenarios were deemed “appropriate” for MMS. However, the MMS appropriate-use criteria address “the merits of the MMS modality alone and not in comparison with other modalities. That is, the appropriate-use criteria are not to be translated as a comparative effectiveness document.”5 Although Mohs can be used for many scenarios, there were no conclusions drawn about what is the best modality for any given clinical scenario and no comparisons between Mohs and any of the wide range of therapeutic interventions are available.
A review of the literature shows that there are no level I studies that provide comparative effectiveness data. However, some conclusions can be made from existing studies. Mosterd et al6 in 2008 published the results of their prospective randomized control trial with 5-year follow-up. They took 612 facial primary basal cell carcinomas (pBCC) and recurrent basal cell carcinomas (rBCC) and randomized the patients to either SE or MMS. Margin assessment, rates of recurrence, cosmetic outcomes, and complication rates were documented. Formal assessment at 6 months, 18 months, and 5 years was performed. The carcinomas were on average 1 cm in diameter and located in the cosmetically sensitive H zone of the face. Overall, SE was inadequate in 18% of pBCC and 32% of all rBCC requiring re-excision. There was no difference in complication rates or aesthetic outcomes between excision and MMS, although it was noted that primary tumors had better aesthetic outcomes than recurrent tumors. Recurrence rates for pBCC at 5 years were the same between MMS and SE (4.1% and 2.5%, P > 0.05). However, recurrence rates for rBCC were significantly higher with SE, as compared to MMS (12.1% vs 2.4%, P < 0.05). They concluded that MMS is superior to simple excision in patients with rBCC but is equivocal in clinical outcome for pBCC of the face. Chren et al7 in 2012 reviewed a prospective cohort of 1458 consecutive primary NMSCs (basal and squamous cells) with 7-year follow-up. Patients were treated with destruction, SE, and MMS.7 The authors found that the recurrence rates were the same between MMS and SE at 5 years (3.3% vs 1.7%, P = 0.26). This was true even in high-risk patients. Although in patients with HIV, multiple tumors, and multiple visits, recurrence was more likely, the rate of recurrence did not differ based on the treatment. Even tumors classically thought to be at high risk for recurrence, such as those >2 cm in diameter and those with invasive histologic characteristics, had equivocal recurrence rates regardless of treatment type. The authors concluded that SE and MMS are equivocal in clinical outcome for primary NMSC. In the setting of an equivocal clinical outcome, the decision for the most appropriate treatment modality must be based on many factors.
THE ECONOMIC IMPACT OF SKIN CANCER MANAGEMENT
Over the past 5 years, the cost of health care has progressively shifted to the patient. The use of consumer-directed plans, otherwise known as “skin in the game insurance,” has skyrocketed. Although these are advantageous for their relatively lower premiums, they are characterized by significant deductibles, coinsurance, and copays. The average deductible for a single person in the United States is $2098 and for a family of 4, it is $4037. A deductible is a predetermined monetary amount a patient is responsible for before an insurance company will begin to pay their medical fees. More and more patients are required to pay a significant amount of upfront costs for their health care. The percentage of companies offering only high deductible plans has increased from a mere 10% in 2010 to 33% in 2015.8 Our judicious use of medical resources is critical to providing our patients with not only the best clinical care possible but also financially the most reasonable choice that is appropriate.
In addition to the skyrocketing clinical burden of skin cancer, the economic burden of skin cancer has increased significantly. From 2002 to 2006, the annual cost of skin cancer averaged $3.6 billion, but by 2007 to 2011, the annual cost averaged $8.1 billion, a 126.2% increase. In contrast, the management of all other cancers increased by only 25.1%. Although the absolute number of skin cancer cases has increased, which accounts for part of the increase in treatment costs, the average cost of treatment per patient has also increased significantly, from $1000 per patient in 2006 to $1600 per patient in 2011.1
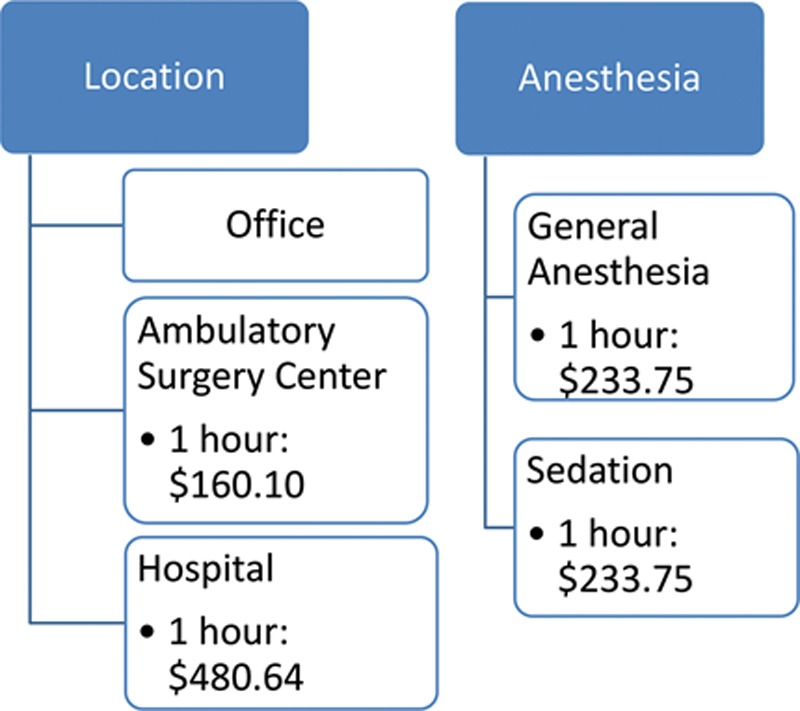
The costs related to skin cancer treatments are multifactorial (Figs. 1, 2). Perhaps, most relevant to the plastic surgeon is the cost related to the location in which care is administered. In a review in 2010, Marks et al9 found that the same treatment in the hospital was up to 4 times more expensive than the treatment in the office. As the charge and payment to the physician for a procedure are the same regardless of location, the extra cost goes to the facility, whether a hospital or ambulatory surgery center.
Fig. 1.
Medicare payment data—skin cancer reimbursement (face).
Fig. 2.
Medicare payment data—skin cancer reimbursement (trunk).
In a historic release of data, the Centers for Medicare and Medicaid Services released information on over 880,000 health care providers who received $77 billion in Medicare payments in 2012, under the Medicare Part B Fee-For-Service program. Although this did not include facility and hospital fees, this release provided new insight into the types of procedures delivered and subsequent charges.10
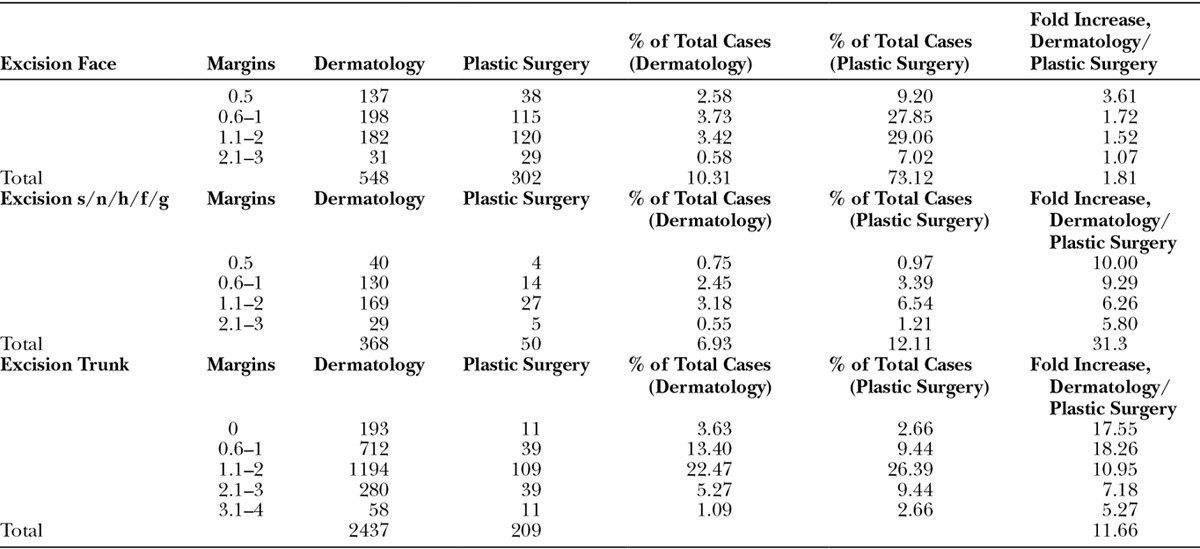
The majority of skin cancer excisions, both benign and malignant, are performed by dermatologists. Excision of malignant lesions is much more common than excision of benign lesions. Excisions of malignant lesions of the trunk are more common than those involving the face, scalp, neck, hands, feet, and genitalia. Plastic surgeons do proportionately more excisions on face (Tables 1 and 2).
Table 1.
Excision of Malignant Lesions
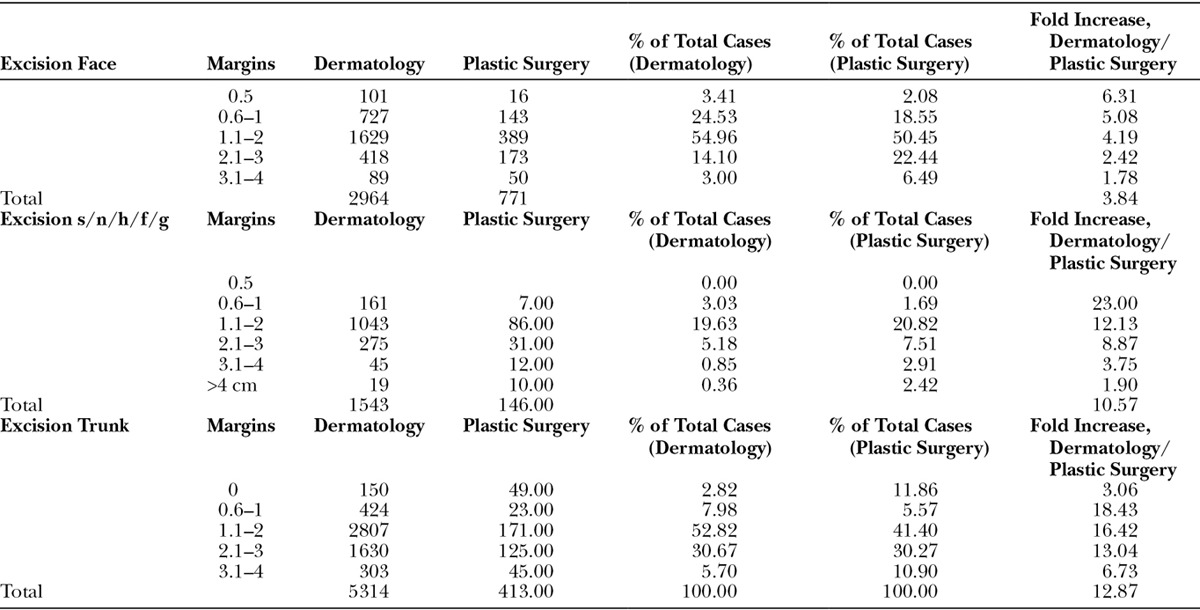
Table 2.
Excision of Benign Lesions
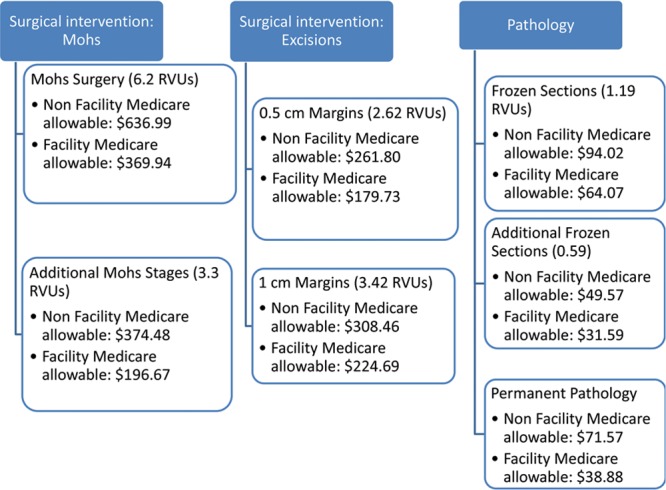
The average Medicare payment amount for a first-stage Mohs of the head, neck, hands, feet, or genitalia is $424 ± $90 ($156.70–$639.70) (Table 3). For subsequent stages, amount is $306.90 ± $48.87 ($140.20–$395.20) (Fig. 3). The average Medicare payment amount for a first-stage Mohs of the trunk, arm, or leg is $412.30 ± $83.87 ($179–$578). For subsequent stages in this area of the body, the amount is $294.30 ± $39.62 ($137–$365) (Fig. 4).
Table 3.
Medicare Payments
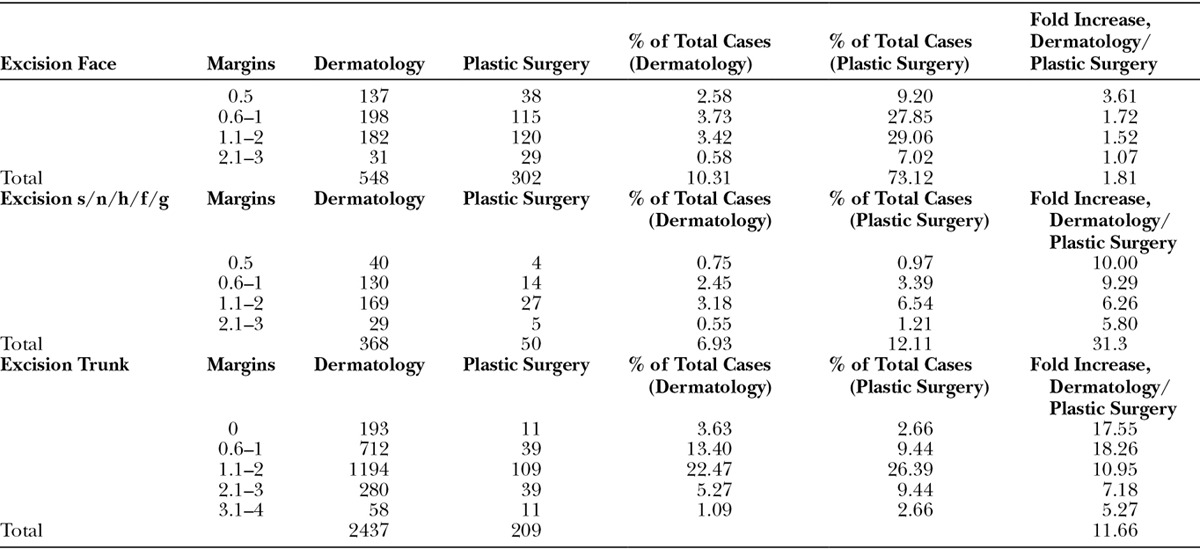
Fig. 3.
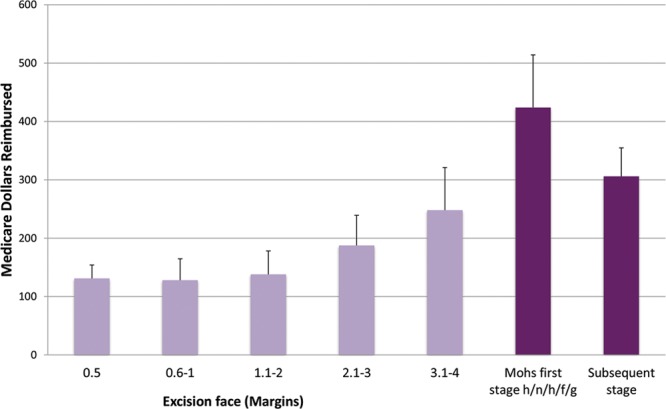
Reimbursement for skin cancers on the face.
Fig. 4.

Reimbursement for skin cancers on the trunk.
By contrast, simple SE of a malignant lesion on the face, eyes, ears, and neck with margins ranges from $131.90 ± $23.11 ($75.90–$187.00) for 0.5- to 1-cm margins up to $240.50 ± $73.02 ($101.90–$360.90) for 4-cm margins. As expected, 4-cm margins are uncommon, with only 50 excisions requiring such aggressive margins performed by all plastic surgeons in 2012. The pathology fee is $68.37 ± $11.00 ($24.00–$90.70) (Fig. 3).
A review of internal data demonstrates that the cost of MMS can be more than 2 to 3 times the cost of SE, even when incorporating pathology fees, when performed in the office. However, the use of an OR or anesthesiologist significantly alters the cost (Fig. 5).
Fig. 5.
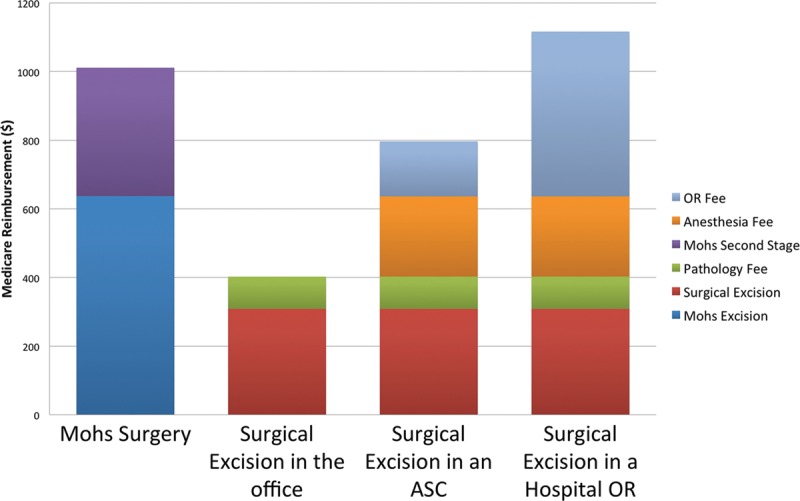
Medicare payment data for treatment of a skin cancer of the face.
If both procedures are performed in the office, the cost differential is likely reasonable in the setting of high-risk tumors. Mosterd et al found that the additional cost of preventing 1 recurrence by employing Mohs surgery in the Dutch healthcare system was €23,454 for pBCC and €3171 for rBCC and concluded that the Mohs surgery was cost-effective over SE for the treatment of recurrent facial BCC. However, the overall financial impact of MMS is particularly amplified if you evaluate the overall growth of MMS. From 1992 to 2009, MMS increased by 700%. In contrast, in that same period, SEs increased by 20%. In 2009, 1800 providers billed Medicare for MMS. In our review of the Medicare data, by 2012, that number had increased to 3209. One in 4 skin cancers is now treated by MMS.
MMS utilization varies widely in the United States. In the state of New Mexico, only 12% of NMSCs of the face, scalp, neck, hands, feet, and genitalia are treated by MMS. In Minnesota, MMS is used in 53% of all instances of skin cancer. This dramatic difference in utilization is difficult to explain clinically.
CONCLUSIONS
The clinical burden of skin cancer has increased. We have a duty as physicians to educate our patients regarding the risks of skin cancer and the most appropriate methods to prevent skin cancer. Health care costs are becoming more transparent, and patients want to know what they are paying for. It is critical not only on a global level but also on an individual level for the patient who is faced with a high deductible. For a patient, the choice of treatment can be a significant financial decision and burden. Cost of skin cancer is multifactorial. As plastic surgeons, judicious use of hospital and ambulatory surgery centers can be a significant cost savings for our patients, when used in clinically appropriate situations. Furthermore, careful consideration of our finite time and resources is required. Idle time spent in the operating room waiting for frozen sections may be costly, not only for the health care system and our patients but also for our own productivity.
The type of treatment deserves careful thought. In general, SE of a malignant skin lesion is less expensive when done in an office or ambulatory surgical center than at a hospital. SE with pathologic examination is less expensive than MMS. However, doing these procedures at a hospital or in the operating room significantly increases costs. There are many situations where MMS is clinically superior to other treatment modalities, such as in rBCC. In those situations, not only is it clinically superior but also it is likely nearly financially equivocal to SE, given the high rates of recurrence associated with excision and associated costs. However, the majority of NMSC is not high-risk tumors and may be treated effectively with excision in office or out-patient surgery center settings. In this era of rising health care costs, our patients bear a direct financial impact from the care that we deliver. We have a duty to provide our patients with superb clinical care at the lowest possible cost.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Guy GP, Jr, Machlin SR, Ekwueme DU, et al. Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. Am J Prev Med. 2015;48:183–187. doi: 10.1016/j.amepre.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Surgeons, A.S.o.P. Top 5 Reconstructive Procedures. 2012 [cited December 7, 2014]. Available at http://www.plasticsurgery.org/Documents/news-resources/statistics/2012-Plastic-Surgery-Statistics/Top-5-Reconstructive-Surgery-Procedures-2012.pdf.
- 3.Rogers CR, Bentz ML. An evidence-based approach to the treatment of nonmelanoma facial skin malignancies. Plast Reconstr Surg. 2011;127:940–948. doi: 10.1097/PRS.0b013e318204aeb2. [DOI] [PubMed] [Google Scholar]
- 4.NCCN Clinical Practice Guidelines in Oncology Basal Cell Cancer. Available at: https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#nmsc. Accessed August 2016.
- 5.Connolly SM, Baker DR, Coldiron BM, et al. Ad Hoc Task Force. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531–550. doi: 10.1016/j.jaad.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Mosterd K, Krekels GA, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149–1156. doi: 10.1016/S1470-2045(08)70260-2. [DOI] [PubMed] [Google Scholar]
- 7.Chren MM, Linos E, Torres JS, et al. Tumor recurrence 5 years after treatment of cutaneous basal cell carcinoma and squamous cell carcinoma. J Invest Dermatol. 2013;133:1188–1196. doi: 10.1038/jid.2012.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernard T. High health plan deductibles weigh down more employees. New York Times. 2014 Sep; [Google Scholar]
- 9.Ponsford MW, Goodman G, Marks R. The prevalence and accuracy of diagnosis of non-melanotic skin cancer in Victoria. Australas J Dermatol. 1983;24:79–82. doi: 10.1111/j.1440-0960.1983.tb00256.x. [DOI] [PubMed] [Google Scholar]
- 10.Services, C.f.M.a.M. Medicare Provider Utilization and Payment Data. 2014. Available at: https://data.cms.gov/Public-Use-Files/Medicare-Provider-Utilization-and-Payment-Data-Phy/ee7f-sh97. Accessed August 2016. [DOI] [PubMed]


