Background:
The importance of analysis of the nasal spine should not be underestimated in the correct planning of rhinoplasty. Deformations in position with respect to the midline and/or in size are often present, and their correction to ensure harmony between the spine and the other components of the nasal pyramid constitutes a key step in rhinoplasty that can lead to excellent results.
Methods:
The study includes 160 patients who underwent surgical treatment of the anterior nasal spine with or without other techniques of nasal reshaping. Eighty-seven of these patients presented with hyperplasia of the nasal spine, 43 with hypoplasia, and 30 with deviation. A combination of deviation and hyperplasia was present in 15 cases.
Results:
No patients developed postoperative complications. Five patients who underwent anterior nasal spine reduction reported postoperative numbness in the premaxillary area, but sensitivity was fully regained within 4 months after surgery in these patients. All the patients reported postoperative improvement of nasal airflow. A total of 142 patients considered their postoperative aesthetic result as excellent and 18 as good.
Conclusion:
The simplicity of the surgical procedures performed on the nasal spine and the marked aesthetic improvements thus achieved suggest that greater attention should be paid to this anatomical region.
The anterior nasal spine (ANS) is a protrusion of the maxilla at the base of the nose. It is important in determining the morphology of the human face as regards support for the nasal tip and projection of the nose and the upper lip. The morphology of this area also determines the correct balance between the upper lip and columella in profile. A morphologically imperfect nasal spine can impair the aesthetic appearance of the nose. Defects of shape or position can have a marked impact on the nasolabial angle and indirectly on the tip. Hyperplasia can mean an unduly wide nasolabial angle and hypoplasia an acute angle that accentuates drooping of the tip, in particular when an individual smiles.
The malformations of the nasal spine also affect projection of the tip. As is known, hyperplasia of the nasal spine can be partially or totally responsible for overprojection of the tip. Nor should we overlook its role in the genesis of deviation of the caudal septum and the columella, a problem visible in basal projection and confirmed by palpation. In the rhinoplasty algorithm, analysis of this small and often overlooked area of the nose can be an important factor to achieve overall better results.
The study illustrates all the conditions in which reshaping of the nasal spine is indicated and puts forward key elements for a precise protocol to that end.
MATERIALS AND METHODS
A review of the authors’ medical records shows that 160 patients underwent rhinoplasty with reshaping of the ANS from 2010 to 2013.
To establish the normal length of the ANS, measurements were made of its length on the computed tomography (CT) in basal projection of 310 patients on whom CT of the nose and the paranasal sinuses had been performed for sinusitis with no evident aesthetic impairment of the subnasal region. The range of measurements was between 3 and 6 mm from the front wall of the maxillary.
Accurate and real measurements of the nasal spine using the CT scan were achieved enlarging the CT images up to a 1:1 ratio. From the clinical point of view, all of the 160 patients of this study presented marked alteration of the nasal spine. They underwent CT of the facial skeleton in coronal and basal projection with no contrast medium (Fig. 1) and were divided on this basis into 3 groups: (a) hyperplasia of the nasal spine (projecting more than 6 mm from the front wall of the maxillary); (b) hypoplasia of the nasal spine (projecting less than 3 mm from the front wall of the maxillary); (c) deviation of the nasal spine. In the last group, by rhinoscopy, the cartilaginous septum appeared almost straight posteriorly, so the deviated nasal spine seemed the primary reason for the deviated nasal base. Eighty-seven patients belonged to group “a,” 43 to group “b,” and 30 to group “c.” Fifteen patients of group c also presented with hyperplasia of the ANS. Three of the 43 patients in group b were suffering from the Binder syndrome.
Fig. 1.

CT in basal projection showing hyperplasia of the ANS.
Hyperplasia of the nasal spine was combined with overprojection of the nasal tip complex in 26 patients (30%) of group a. Hypoplasia of the nasal spine was associated with ptosis or drooping tip in 21 patients (49%) of group b. Finally, the deviation of the spine was combined with marked dislocation of the caudal septum in 90% of the cases in group c.
Clinical examination of patients, based principally on anterior and posterior rhinoscopy, was accompanied by careful appraisal of the cartilaginous structural support of the tip by palpation. The soft-tissue cephalometric analysis described by Arnett et al1 was used to perform an aesthetic analysis of the profile before and after surgery. Anterior active rhinomanometry before and after decongestion was performed according to the method described by Constantian and Clardy.2
Open access was used in 100% of the cases as personal preference of the surgeons. In all cases, once the decision had been taken to operate on the nasal spine, the use of a direct approach with complete exposure of the nasal spine was necessary.
Surgery on the nasal spine was combined with the medial crural overlay technique in 10 cases where the overprojection of the tip was particularly marked. A lateral crural overlay was also performed in the cases where hypoplasia of the nasal spine was accompanied by marked drooping of the tip to obtain the correct degree of tip rotation. In 4 patients, with micrognathia, genioplasty was performed, but none of the patients of these series had maxillary surgery. All the patients underwent regular postoperative checkups at 1 week, 1 month, 3 months, 6 months, and 1 year (mean follow-up: 20.7 mo; range: 15–48 mo).
Surgical Technique
Open transcolumellar access was used with exposure of the cartilage of the tip and nasal dorsum. Separation of the medial crura made it possible to approach the nasal septum and perform septoplasty.
The separation of the medial crura extended as far as their posterior margin. The ANS was exposed by blunt dissection and then with subperiosteal detachment, and the posterior septal angle was freed from the nasal spine.
In the case of patients with hyperplasia, after exposure of the ANS, it was reduced using bone-cutting forceps or a rotary cutter (Fig. 2). Removal of a portion of the ANS leaves the medial crura in a lower position and thus reduces the projection of the nasal tip. There is usually no need to reshape the medial crura on the nasal spine because their feet are placed spontaneously on either side of it because of their natural basal divergence.
Fig. 2.
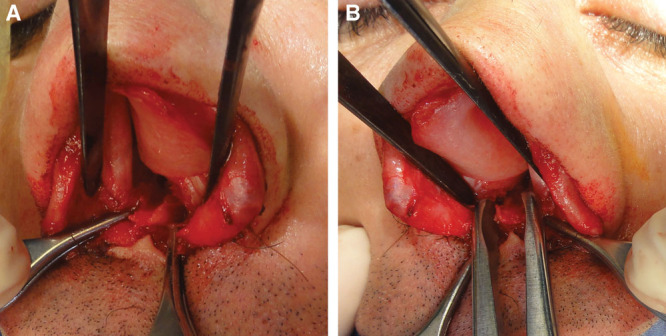
A, Complete exposure of the ANS. B, Use of bone-cutting forceps to reduce the ANS.
Hypoplasia of the nasal spine (group b) was corrected with a cartilaginous columellar strut harvested from the nasal septum and secured by sutures to the nasal spine in an anterior position. In cases where this procedure proved insufficient during the operation, a further plumping graft of diced cartilage was placed in front of the foot of the columellar strut to obtain a correct nasolabial angle. A costal cartilage graft proved necessary in the 3 cases of Binder syndrome to supply a sufficient amount of tissue and support in the deficient area.
In cases of deviation of the nasal spine (group c), repositioning was carried out at the end of the rhinoplasty, and fracturing constituted the first step in median repositioning. The fracture was easily executed with a 4-mm osteotome oriented in a lateromedial direction, and the introduction of a Killian nasal speculum into the contralateral nasal cavity proved useful to counterbalance the fracturing force exerted. A mattress suture of Vicryl 3.0 all the way through securing the spine to the periosteum of the side opposite to the deviation was sufficient to hold it in the correct position until the fracture calcified. The calcification and healing of the fracture were in any case very quick processes due to the intense vascularization of the region.
RESULTS
No patients developed major postoperative complications, and the wounds healed well. Five patients who underwent ANS reduction reported postoperative numbness in the premaxillary area, but sensitivity was fully regained within 4 months after surgery in these patients. The infection (nasal vestibulitis) that occurred in the premaxillary area in 1 case was cured by treatment with local and general antibiotics.
Comparison of the results of preoperative and postoperative rhinomanometry shows substantial, objective improvement in nasal airflow in patients with preoperative airway obstruction. Rhinomanometric data registered an increase of approximately 1.6 times over preoperative flow. No impairment of nasal airflow was registered in the cases of preoperative normal breathing. The measurements of the soft-tissue response after the skeletal alteration of the ANS showed an increase or a reduction of the tip’s soft tissues of 55% (range, 36%–62%) in comparison to the skeletal modifications. No postoperative CT scans were performed because the modification of the ANS was evaluated by anterior rhinoscopy and intranasal manual palpation. The results were stable over time after 1 year.
Positive aesthetic judgments were expressed not only by the operating team but also by the surgeons involved in the control tests, the family physicians, and the patients.
The data were objectified using 2 questionnaires, answered by physicians and patients. Both the patients and the physicians involved in the care of the patients were asked to grade the aesthetic outcome as poor, good, or excellent. All patients graded their aesthetic result, and each patient had at least 1 assessment by a physician. When the patients were asked to grade the aesthetic result as poor, good, or excellent 6 months after surgery, cumulative data showed that 142 graded outcome as excellent and 18 as good. Three typical cases of ANS treatment are shown in Figures 3–8.
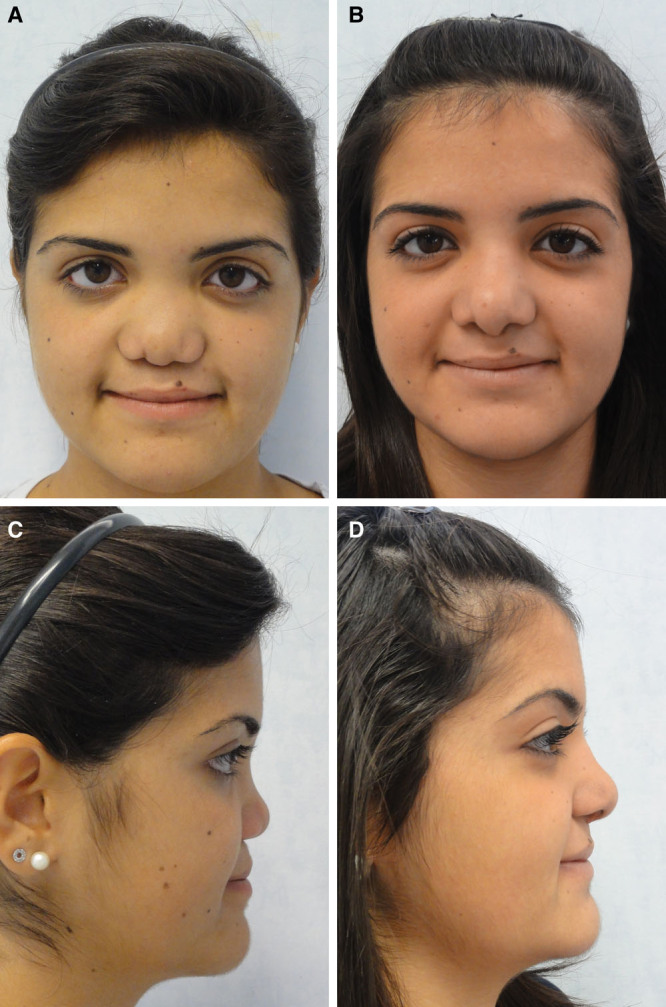
Fig. 3.
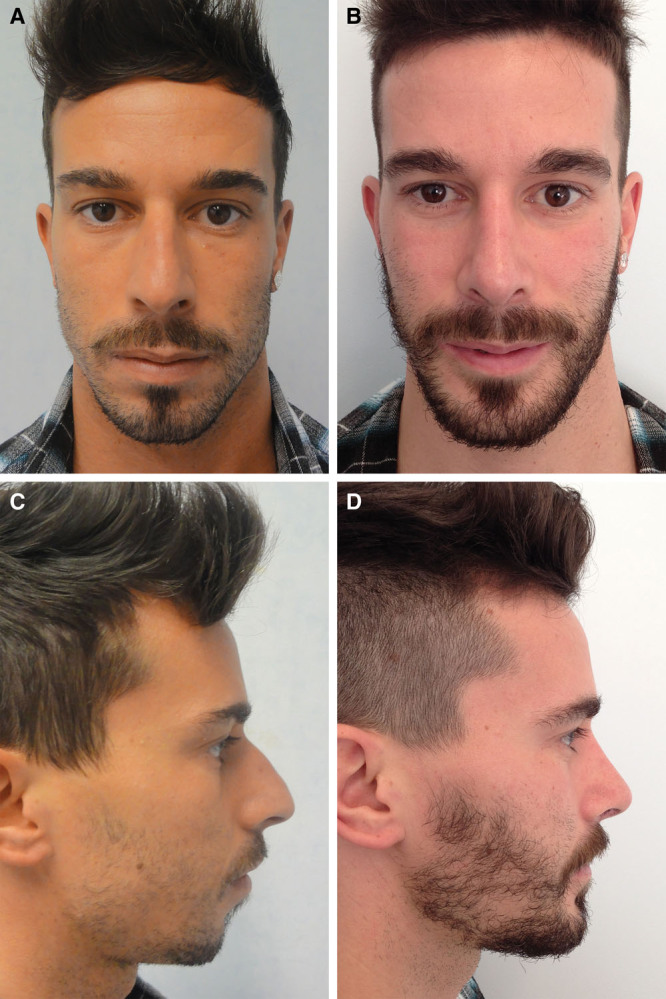
Case 1: Deviation of the nasal spine. Preoperative (A, C) and postoperative (B, D) photographs on frontal and profile views. Correction of the defects involved osteocartilaginous hump excision, osteotomies, genioplasty, fracturing, and median repositioning of the nasal spine combined with suturing to the periosteum of the upper maxillary bone.
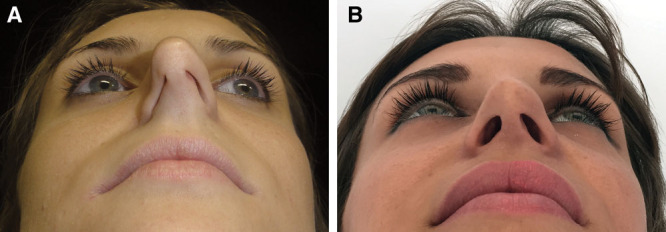
Fig. 8.

Case 3: Preoperative (A) and postoperative (B) basal view and intraoperative (C) image of the costal grafts.
Fig. 4.
Case 1: A, The basal view shows marked deviation of the nasal spine to the left of the midline. The deviated columella was due to a deviated nasal spine because the cartilaginous caudal septum was in the same axis of the spine and not sideways. B, After surgery, the only repositioning of the nasal spine was able to straighten the nasal base.
Fig. 5.

Case 2: Hypertrophy of the nasal spine. Preoperative (A, C) and postoperative (B, D) photographs on frontal and profile views. Correction of the defects present involved osteocartilaginous hump excision, osteotomies, cephalic trimming of the lateral crura, columellar strut, reshaping, and reduction of the ANS.
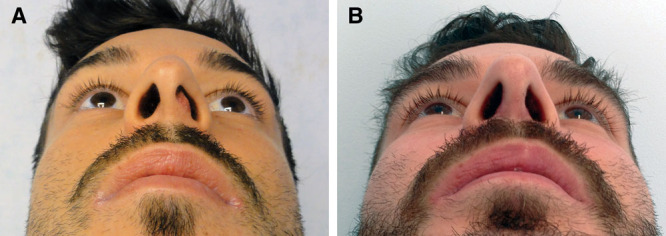
Fig. 6.
Case 2: A, The preoperative basal view shows hyperplasia of the nasal spine combined with collapse of the external nasal valve during inspiration. B, Correction of the defect in the postoperative basal view.
Fig. 7.
Case 3: Binder syndrome with aplasia of the ANS. Preoperative (A, C) and postoperative (B, D) photographs on frontal and profile views. The view in profile clearly shows the marked underprojection of the nasal tip with an extremely acute nasolabial angle. Correction of the defects present involved a graft from the seventh and eighth ribs shaped to reconstruct an L-shaped dorsocaudal structure of support. An osseous costal graft was attached to the caudal pillar of the L-shaped structure and secured with titanium screws and plates to the premaxilla.
DISCUSSION
The ANS is a pointed projection at the anterior extremity of the intermaxillary suture. The anteroinferior edge of the caudal septum is attached to the ANS.3 The ANS can be overdeveloped, underdeveloped, deviated, or both overdeveloped and deviated.
Deformation of the nasal spine is often the cause of various imperfections of the lower third of the nasal pyramid. The importance of identifying and correcting these flaws is often overlooked or underestimated during rhinoplasty, but simple reshaping of the ANS can give excellent results and obviate recourse to far more complex techniques. A situation easier to analyze is columellar deviation caused by deviation of the nasal spine with respect to the midline. Repositioning of the caudal septum with septoplasty or extracorporeal reshaping of the cartilaginous septum is capable of solving the functional problem brilliantly but not capable of completely eliminating the aesthetic blemish in basal view. It is in fact only fracturing of the nasal spine and median repositioning of the same at the end of the operation that can provide the perfect result required. It should also be noted that it is easy to perform this fracture of the ANS with a straight 4-mm chisel and subsequent attachment by sutures to the periosteum.4–7 Other authors suggest attachment of the ANS to the midline with microplates.8
A different situation arises when the ANS causes overprojection or underprojection of the tip. Assessment is less immediate and more complex in cases of overprojection than deviation of the columella from the midline. Attention was drawn to the importance of appraisal of the nasal spine in determining the causes of this flaw by Johnson and Godin9 in 1995. Different measurements have been put forward in the literature for precise and appropriate analysis of the projection of the nasal tip,10,11 and dynamic analysis during the act of smiling can also prove useful to ascertain the possible coexistence of ptosis. In these cases, correction of the defect and the reduction of tip projection are often carried out with dome division, medial crural overlay (with or without lateral crural overlay), and removal of the foot of the medial crura, all of which are tried and tested techniques capable of ensuring excellent results.12–15
We should not, however, underestimate the value of careful anatomical assessment of the length of the ANS. Adjustment of the length of the nasal spine to within its normal range constitutes the true solution in some cases by restoring physiological normality to this anatomical element. In fact, in cases of overly anterior nasal spine, the caudal septum is anatomically placed in a higher position. The surgical correction is carried out also in these cases with a simple maneuver with bone-cutting forceps to remove the surplus portion. Needless to say, the use of this corrective technique on the ANS should always be within the bounds of common sense and sometimes can and should be combined with other techniques or procedures to reduce the length of the medial crura. Medial crural overlay is performed to decrease nasal projection and tip rotation. This procedure involves the division of the medial crura, which are then laid one over the other and sutured in their new position. One possible disadvantage of medial crural overlay is an increase in the width of the columella. Generally speaking, it is preferable to use less-invasive procedures that leave the domal arch intact. Finally, in cases where overprojection is combined with evident drooping of the nasal tip due to excessive length of the lateral crura, lateral crural overlay should also be employed to obtain a pleasant upward rotation of the nasal tip complex.12,15
The last defect to be taken into consideration is marked underprojection of the nasal tip. In these cases too, careful analysis can reveal hypoplasia of the ANS as the primary cause.16 Use of the lateral crural steal procedure combined with a tongue-in-groove technique or the insertion of a robust columellar strut is sufficient to eliminate the deficiency of the nasal spine and give the tip the correct degree of projection. Unfortunately, in cases where this underprojection is due to a very severe deficiency of the ANS (as in the Binder syndrome), the surgical procedures described above prove insufficient and something else is required. The Binder syndrome is a disorder of unknown etiology characterized by hypoplasia of the ANS, midfacial retrusion, and 40% to 50% association of an underdeveloped frontal sinus and cervicospinal abnormalities. The nose is short with hypoplastic alar cartilages and short, retracted columella with an acute nasolabial angle.17,18 The treatment of choice in these situations is reconstruction of the L-shaped dorsocaudal septal structure with an autologous graft of costal cartilage. Further reconstruction can involve an autologous or heterologous bone graft rigidly secured to the premaxilla as a supporting base for the caudal portion of the L-shaped structure.
CONCLUSION
The nasal spine is an often overlooked region of great importance as it determines the morphology of the lower third of the nose. The correction of defects of the nasal spine constitutes an important step in rhinoplasty when these give rise to evident deformation of the nasal tip and nasolabial angle. In the case of an overprojected nose, reshaping of the ANS makes it possible to reduce the projection of the entire complex of the medial crura and the support of the caudal septum without invasive techniques. The results of 160 cases in which the nasal spine was corrected demonstrate the validity and effectiveness of treatment of this anatomical region.
Patient Consent
Patients provided written consent for the use of their images.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Arnett GW, Jelic JS, Kim J, et al. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop. 1999;116:239–253. doi: 10.1016/s0889-5406(99)70234-9. [DOI] [PubMed] [Google Scholar]
- 2.Constantian MB, Clardy RB. The relative importance of septal and nasal valvular surgery in correcting airway obstruction in primary and secondary rhinoplasty. Plast Reconstr Surg. 1996;98:38–54; discussion 55. doi: 10.1097/00006534-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Hafkamp HC, Bruintjes TD, Huizing EH. Functional anatomy of the premaxillary area. Rhinology. 1999;37:21–24. [PubMed] [Google Scholar]
- 4.Constantine FC, Ahmad J, Geissler P, et al. Simplifying the management of caudal septal deviation in rhinoplasty. Plast Reconstr Surg. 2014;134:379e–388e. doi: 10.1097/PRS.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 5.Kim H, Kim YJ, Nam SH, et al. Fracture of the anterior nasal spine. J Craniofac Surg. 2012;23:e160–e162. doi: 10.1097/SCS.0b013e31824cdc8c. [DOI] [PubMed] [Google Scholar]
- 6.Guyuron B, Behmand RA. Caudal nasal deviation. Plast Reconstr Surg. 2003;111:2449–2457; discussion 2458. doi: 10.1097/01.PRS.0000060802.70218.FE. [DOI] [PubMed] [Google Scholar]
- 7.Escada P, Penha RS. Fracture of the anterior nasal spine. Rhinology. 1999;37:40–42. [PubMed] [Google Scholar]
- 8.Gubisch W, Constantinescu MA. Refinements in extracorporal septoplasty. Plast Reconstr Surg. 1999;104:1131–1139; discussion 1140. doi: 10.1097/00006534-199909040-00038. [DOI] [PubMed] [Google Scholar]
- 9.Johnson CM, Jr, Godin MS. The tension nose: open structure rhinoplasty approach. Plast Reconstr Surg. 1995;95:43–51. doi: 10.1097/00006534-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Crumley RL, Lanser M. Quantitative analysis of nasal tip projection. Laryngoscope. 1988;98:202–208. doi: 10.1288/00005537-198802000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Byrd HS, Hobar PC. Rhinoplasty: a practical guide for surgical planning. Plast Reconstr Surg. 1993;91:642–654; discussion 655. [PubMed] [Google Scholar]
- 12.Kridel RW, Undavia SS. Deprojection of the nasal tip in revision rhinoplasty. Facial Plast Surg. 2012;28:440–446. doi: 10.1055/s-0032-1319843. [DOI] [PubMed] [Google Scholar]
- 13.Unger JG, Lee MR, Kwon RK, et al. A multivariate analysis of nasal tip deprojection. Plast Reconstr Surg. 2012;129:1163–1167. doi: 10.1097/PRS.0b013e31824a2e05. [DOI] [PubMed] [Google Scholar]
- 14.Soliemanzadeh P, Kridel RW. Nasal tip overprojection: algorithm of surgical deprojection techniques and introduction of medial crural overlay. Arch Facial Plast Surg. 2005;7:374–380. doi: 10.1001/archfaci.7.6.374. [DOI] [PubMed] [Google Scholar]
- 15.Sajjadian A, Guyuron B. An algorithm for treatment of the drooping nose. Aesthet Surg J. 2009;29:199–206. doi: 10.1016/j.asj.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka Y. Oriental nose occidentalization and perinasal shaping by augmentation of the underdeveloped anterior nasal spine. Plast Reconstr Surg Glob Open. 2014;2:e197. doi: 10.1097/GOX.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keppler-Noreuil KM, Wenzel TJ. Binder phenotype: associated findings and etiologic mechanisms. J Craniofac Surg. 2010;21:1339–1345. doi: 10.1097/SCS.0b013e3181ef2b71. [DOI] [PubMed] [Google Scholar]
- 18.Kansu L, Akkuzu B, Avci S. Case report and surgical solution for nasal spine agenesis in a woman with Binder syndrome. Eur Arch Otorhinolaryngol. 2008;265:847–849. doi: 10.1007/s00405-007-0532-5. [DOI] [PubMed] [Google Scholar]


