Supplemental Digital Content is available in the text.
Background:
A new closure technique is introduced, which uses strips of macroporous polypropylene mesh as a suture for closure of abdominal wall defects due to failures of standard sutures and difficulties with planar meshes.
Methods:
Strips of macroporous polypropylene mesh of 2 cm width were passed through the abdominal wall and tied as simple interrupted sutures. The surgical technique and surgical outcomes are presented.
Results:
One hundred and seven patients underwent a mesh sutured abdominal wall closure. Seventy-six patients had preoperative hernias, and the mean hernia width by CT scan for those with scans was 9.1 cm. Forty-nine surgical fields were clean-contaminated, contaminated, or dirty. Five patients had infections within the first 30 days. Only one knot was removed as an office procedure. Mean follow-up at 234 days revealed 4 recurrent hernias.
Conclusions:
Mesh sutured repairs reliably appose tissue under tension using concepts of force distribution and resistance to suture pull-through. The technique reduces the amount of foreign material required in comparison to sheet meshes, and avoids the shortcomings of monofilament sutures. Mesh sutured closures seem to be tolerant of bacterial contamination with low hernia recurrence rates and have replaced our routine use of mesh sheets and bioprosthetic grafts.
All high-tension internal surgical closures require that the ultimate tensile strength (UTS) of the repair remains greater than the forces applied. Otherwise, changes at the suture/tissue interface (STI) will lead to acute or chronic suture pull-through and surgical failure. For the abdominal wall, prophylactic flat meshes have been shown to improve outcomes of laparotomy closures and hernia repairs.1,2 Unfortunately, flat planar meshes have their own drawbacks, including increased time for placement, increased foreign material, increased tissue dissection, pain, infection, and cost.
Planar meshes reduce hernia formation by improving the UTS of the repair and by better distributing forces at the STI.3 Yet, all these theoretic benefits of planar meshes could be achieved with a better-designed suture. Based on preclinical studies that demonstrate decreased suture pull-through and increased early tensile strength for a novel designed mesh suture,4,5 presented is a series of “mesh sutured” repairs where a strip of planar mesh is introduced through either side of the abdominal wall with a sharp instrument and simply tied as a suture. This off-label use of a planar mesh has shown great efficiency and efficacy for both simple and complex abdominal wall closures.
METHODS
Determination of Mesh Size and the Number of Knots Required
Mid-weight, macroporous, uncoated polypropylene mesh (PROLENE Soft Prolene Mesh, Ethicon, Somerville, N.J.) of size 12 × 14 inches (30.5 × 35.6 cm) was cut along the blue lines into strips to mimic the UTS of a number 1 polypropylene suture. Based on tensometry data, a 18–20-mm-wide mesh strip tied with a single square knot had no knot failures and an UTS just above that of the target suture strength. An additional throw was added to the square knot for security of these patients.
Physical Characterization
A small rectangle of size 0.3 × 0.98 cm of the same polypropylene mesh underwent synchrotron microcomputed tomography (microCT) at station 2-BM at the Advanced Photon Source, Argonne National Laboratory, Argonne, Ill.6 One thousand one hundred and eighty slices were imported into ImageJ with a BoneJ plugin,7 an open source image analysis software, for determination of surface area.
Clinical Experience
Inclusion Criteria
The decision to perform a mesh sutured repair was made by the senior surgeon (GAD) based on a relative contraindication to the use of sheet mesh including the added time needed for placement, contamination, and/or a lack of a posterior sheath for avoidance of intraperitoneal mesh placement against bowel. For nonmidline and small defects, mesh sutured repairs were performed to avoid the surgical difficulties required for placement of a planar mesh and due to the known failure rates with standard suture closures. Patients were educated preoperatively about the risks and benefits of sutures, meshes, and mesh strips used as sutures.
Surgical Technique
Subcutaneous tissue was elevated off of the abdominal wall to achieve a 1-cm bite of unscarred abdominal wall spaced 1 cm from each other (Fig. 1) for the interrupted closure. A sharp surgical snap is used to pierce the abdominal wall, with care made to minimize the size of the hole (See video, Supplemental Digital Content, a sharp hemostat is used to pierce the abdominal wall approximately 1 cm from the newly debrided edge of the rectus muscle. The mesh strip is then pulled through the substance of the abdominal wall and then tied like a suture with 3 throws to close the defect, http://links.lww.com/PRSGO/A265). Use of cautery to touch the fascia at the site of the entry point lessens the force required to pierce the abdominal wall. Anterior components release with perforator preservation is performed for larger defects (Figs. 2–5).8 Flank defects are generally closed in two layers, approximating the transversus abdominis and internal oblique in the first row, followed by apposition of the external oblique in the second row. Several strips are placed and are snapped long. Tension on all these strips approximates the abdominal wall to facilitate knot tying. A suction drain is required in the subcutaneous tissue and is removed when <20 cm3 per day.
Fig. 1.
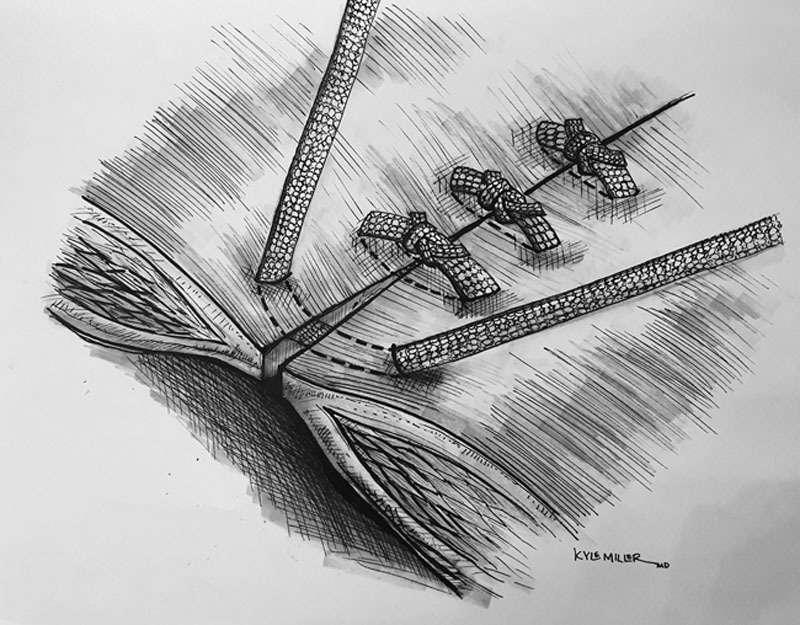
Artist’s drawing of mesh sutured closure of the abdominal wall.
Fig. 2.
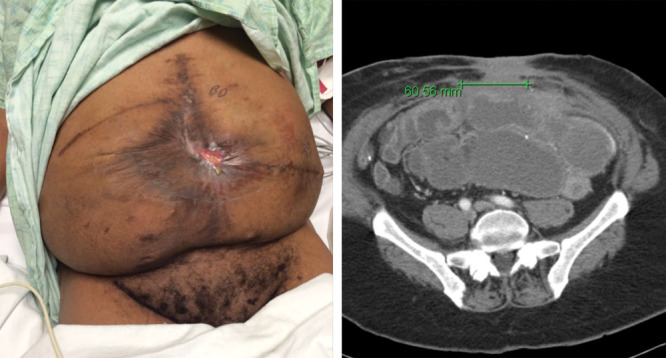
Multiple recurrent enterocutaneous fistula patient with scarred skin and abdominal wall. CT scan shows a bowel obstruction and separation of the rectus muscles of 6 cm. The patient had already undergone an anterior components release.
Fig. 5.
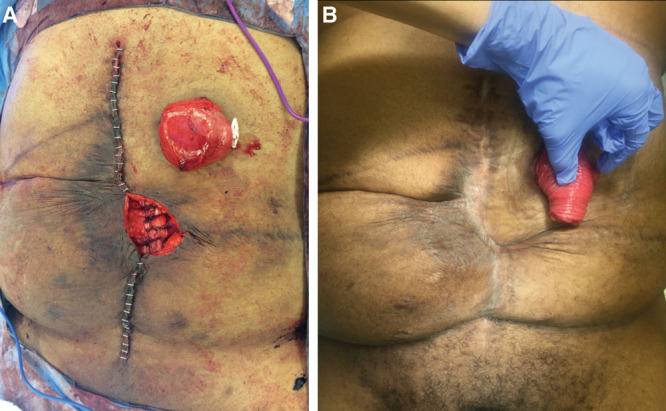
A, Immediate postoperative result. Mesh strips left exposed in a central area due to an inability to close the skin due to prior scarring. B, Four-month result at the time of diverting ostomy takedown showing closure of soft tissues over mesh sutured repair with local wound care.
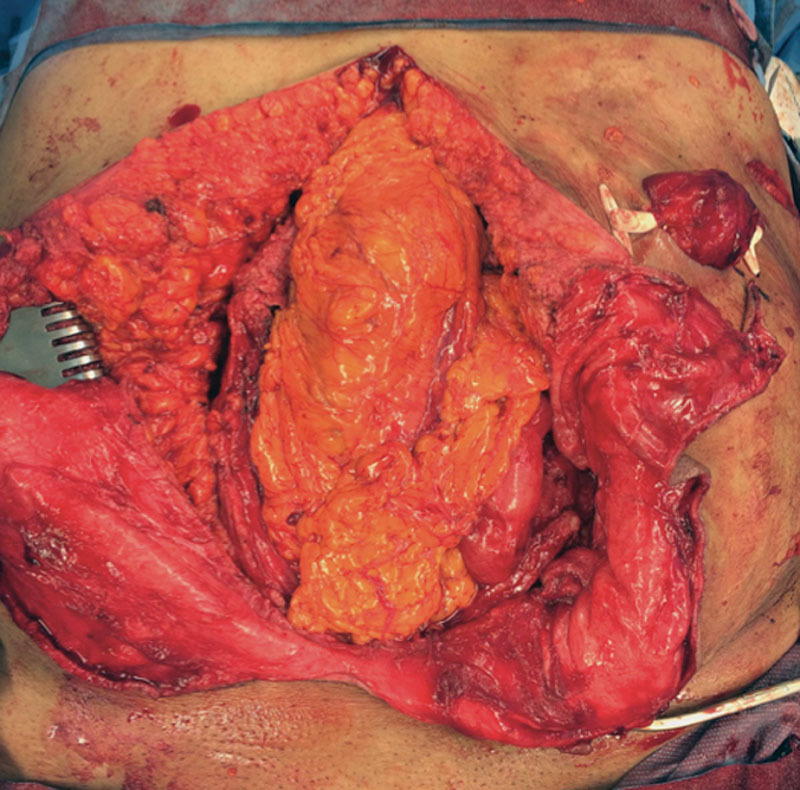
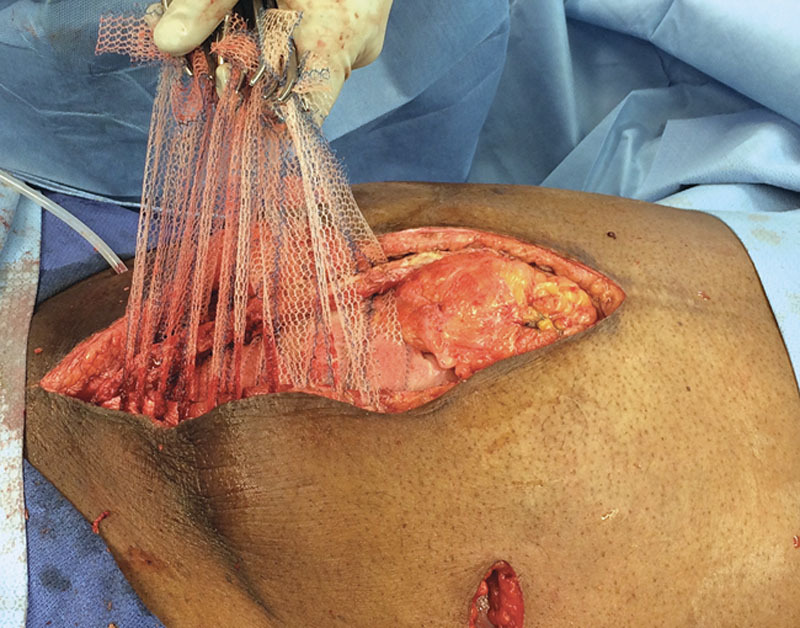
Fig. 3.

Complex abdominal wound after bowel repair.
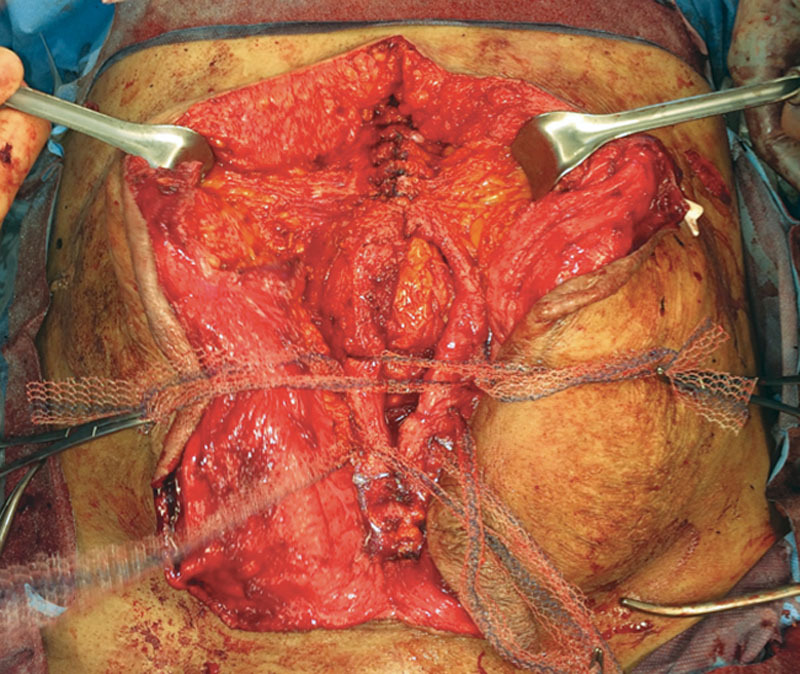
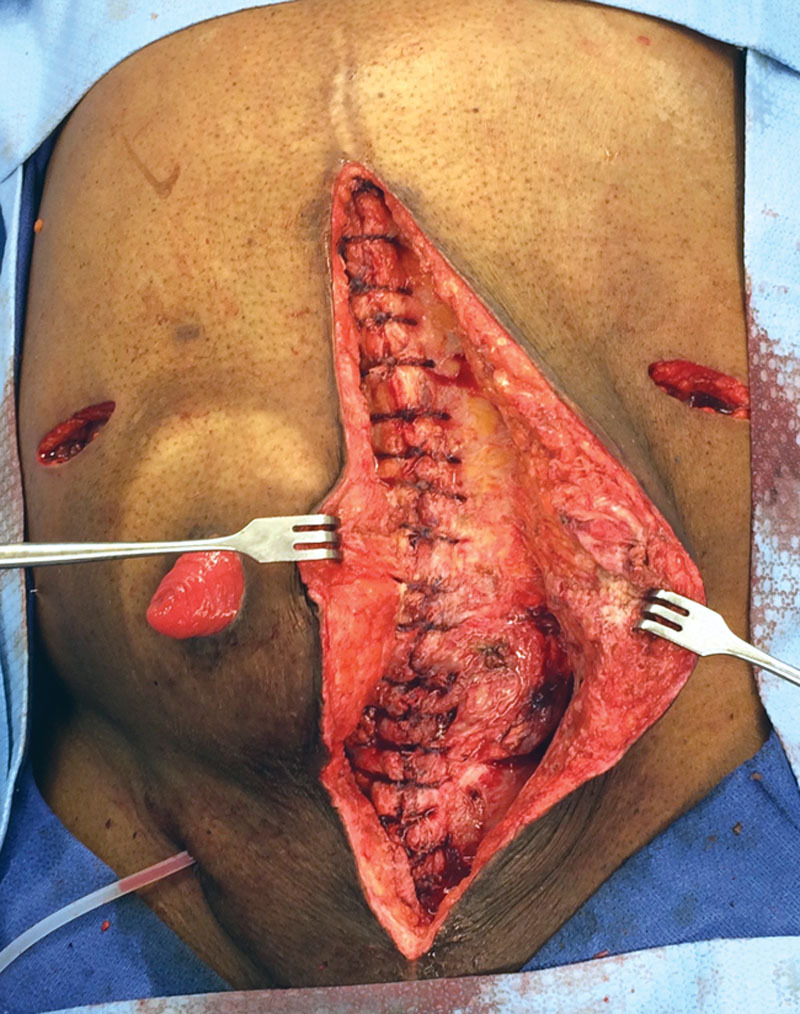
Fig. 4.
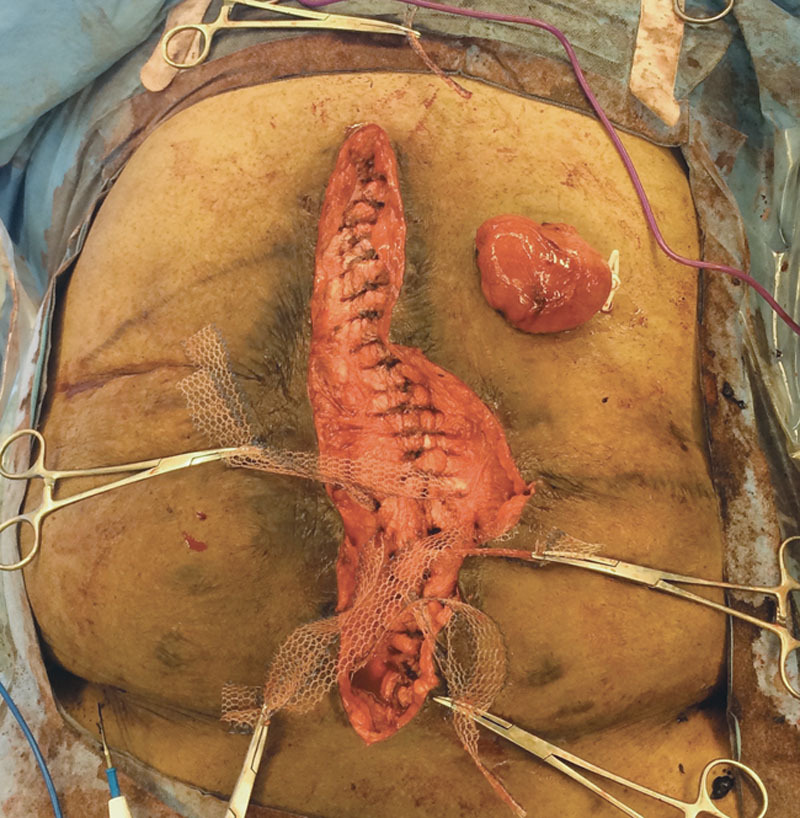
Closure of abdominal defect using interrupted strips of polypropylene mesh that are tied as simple sutures.
Video Graphic 1.
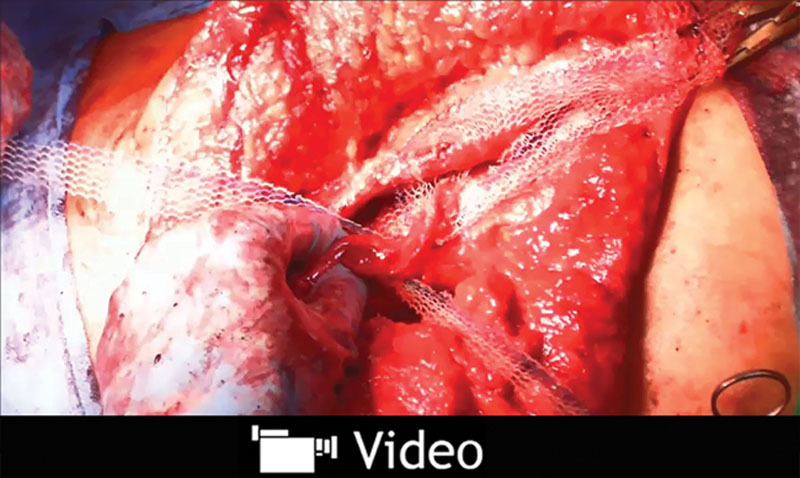
See video, Supplemental Digital Content, a sharp hemostat is used to pierce the abdominal wall approximately 1 cm from the newly debrided edge of the rectus muscle. The mesh strip is then pulled through the substance of the abdominal wall and then tied like a suture with 3 throws to close the defect, http://links.lww.com/PRSGO/A265.
Analysis of Outcomes
A comprehensive retrospective institutional review board–approved review was performed for all patients who underwent a mesh sutured repair and who had 30-day follow-up for this retrospective review. The widest separation of the medial aspect of the rectus muscles was recorded for midline defects for hernia size. Operative reports were reviewed for indications for a mesh sutured repair and the CDC wound classification9 and Ventral Hernia Working Group (VHWG)10 category. Surgical site occurrence (SSO) is defined as any surgical site infection (SSI), seroma, hematoma, delayed wound healing, enterocutaneous fistula, reoperation, or dehiscence. SSI was defined as a clinical diagnosis of wound infection based on the appearance of wound erythema, drainage, and need for postoperative antibiotics. Seroma was defined as any appreciable subcutaneous fluid collection in the postoperative period that was opened to accelerate healing and not treated with antibiotics. All medical complications requiring an intervention and readmission or reoperation within 30 days were recorded. Hernia recurrence was assessed by physical examination by a physician, routine surveillance of CT scan, and in 4 patients by telephone interview. Length of follow-up was defined as the time from surgery to the last documented abdominal wall examination as described above.
RESULTS
Surface Area
The surface area of a number 1 polypropylene suture (0.4 mm in diameter) for a 1-cm length is calculated to be 0.126 cm2 (SA = length × diameter × π). Using microCT, the surface area of a 1-cm length of a 20-mm-wide mesh strip was measured to be 4.31 cm2, for a 34-fold increase.
Clinical Results
Patient Cohort Description
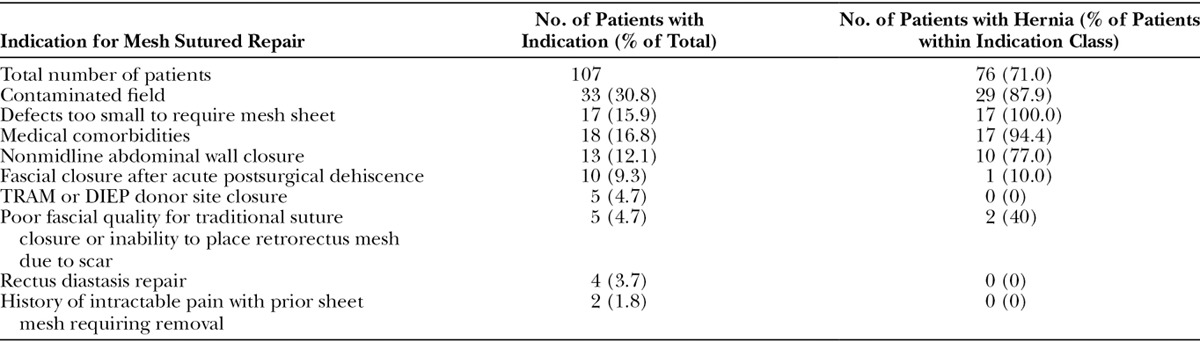
One hundred and fifteen consecutive patients underwent mesh sutured closures of the abdominal wall without an underlying planar mesh, and 107 had at least 30-day follow-up. The prime indication for use of mesh strips is a contaminated midline closure (Table 1). For the 76 patients with documented preoperative hernias, the average midline rectus muscle separation for the 41 available CT scans was 9.1 ± 5.5 cm (range 2–21 cm).
Table 1.
Indication for Mesh Sutured Repair
Over 40% of patients were ASA 3 or above (Table 2). Almost 10% of patients had a prior or concurrent prosthetic mesh infection. Nonsterile surgical fields (CDC Class 2 and above) were present in 49 patients (Figs. 6–10), and these patients had an average transverse separation of their rectus muscles of 10.2 cm for those with CT scans. Of the patients treated, 28% were VHWG 2, 38% grade 3, and 6% grade 4 (Table 3). There were 30 cases with preexisting wounds or stomas at the time of surgery, and 17 cases with entry into the gastrointestinal or genitourinary tract. Ten patients had closure of an acute abdominal wall dehiscence. One-fourth of the patients underwent components releases.
Table 2.
Patient Demographics, Comorbidities, and Surgical History
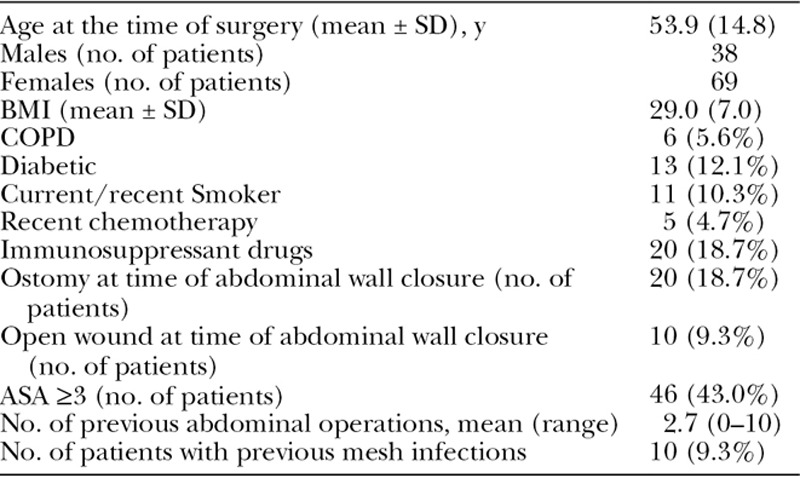
Fig. 6.

Large skin grafted abdominal wall hernia with end colostomy.
Fig. 10.

Three-month postoperative result showing closed abdominal defect and diverting ileostomy.
Table 3.
Patient Risk Stratification
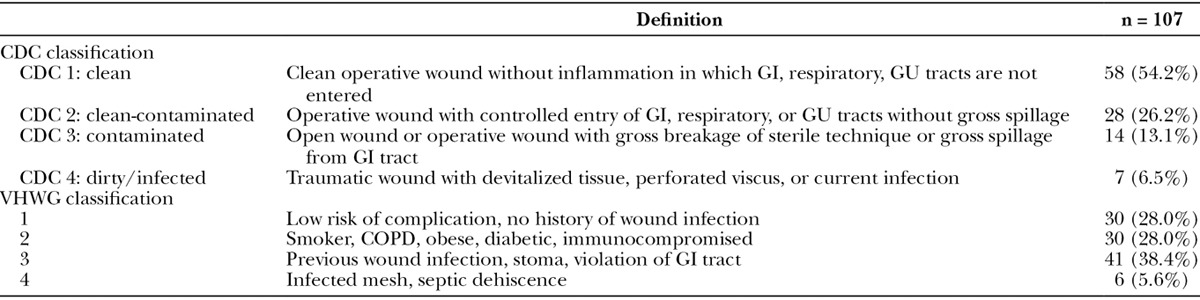
Fig. 7.
Abdomen after end colostomy takedown and placement of diverting ileostomy.
Fig. 8.
Closure of abdominal wall hernia with mesh strips. A components release was not required in this compliant abdominal wall.
Fig. 9.
Closed abdominal wall with mesh strips.
Clinical Outcomes
Follow-up ranges from 30 to 1043 days, with an average follow-up of 234 days and a median follow-up of 178 days. As 9 patients did not have full thickness defects, hernia rates were calculated for the remaining 98 patients. Four of these 98 patients went on to develop an incisional hernia (4.1%). One patient had a recurrence after repair of an umbilical hernia. Two patients with full midline closures were found each to have a single 1-cm asymptomatic defect by surveillance CT scan (but not on physical examination). The fourth patient with diabetes, obesity, and a 14.8-cm hernia underwent a colostomy takedown early in the study. After the colostomy takedown and components release, her midline was closed with a sequence of a mesh strip followed by two interrupted 0-polypropylene sutures repeated for the length of the midline defect (in this series of patients, she was the only patient treated in this manner, whereas 4 others had alternating sutures and mesh strips). At the time of her hernia rerepair, an unusual surgical finding of hernia defects interspersed with well-approximated abdominal wall segments were noted. Biopsy of the joined areas of abdominal wall revealed the presence of the mesh strips still holding the rectus muscles in apposition (Table 4).
Table 4.
Outcomes
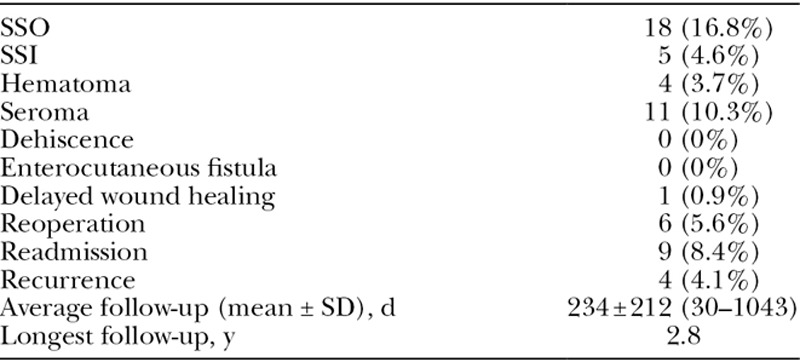
SSO occurred in 8 patients (17%), with the most common postoperative complication being a seroma treated in the office with drainage in 11 (10.3%), whereas 30-day SSI was 4.6%. Three hematomas and two infections required operative treatment of the subcutaneous tissues, and there were no deep infections or fistulas. Nine patients were readmitted within 30 days. Only one knot located at the bottom of a seroma cavity was excised in the office, and no other mesh sutures have required early or late removal. Excluding CDC 1 clean cases, SSO was 22% and SSI was 6.1%.
Two patients died, one from a ruptured bladder and amyloid-induced heart failure and the other on high-dose steroids from sepsis after a colostomy takedown. Neither patient was included in our outcomes as they did not reach a 30-day follow-up (Figs. 11–15).
Fig. 11.

Spontaneous small-bowel lymphoma-induced enterocutaneous fistula emerging through 9-cm hernia defect in a patient with a prior ileal conduit.
Fig. 15.

Early postoperative result demonstrating primary healing.
Fig. 12.

Image after resection and repair of enterocutaneous fistula. Due to chronically inflamed and infected tissues, a polyglactin mesh was placed for 2 days to obtain wound control.
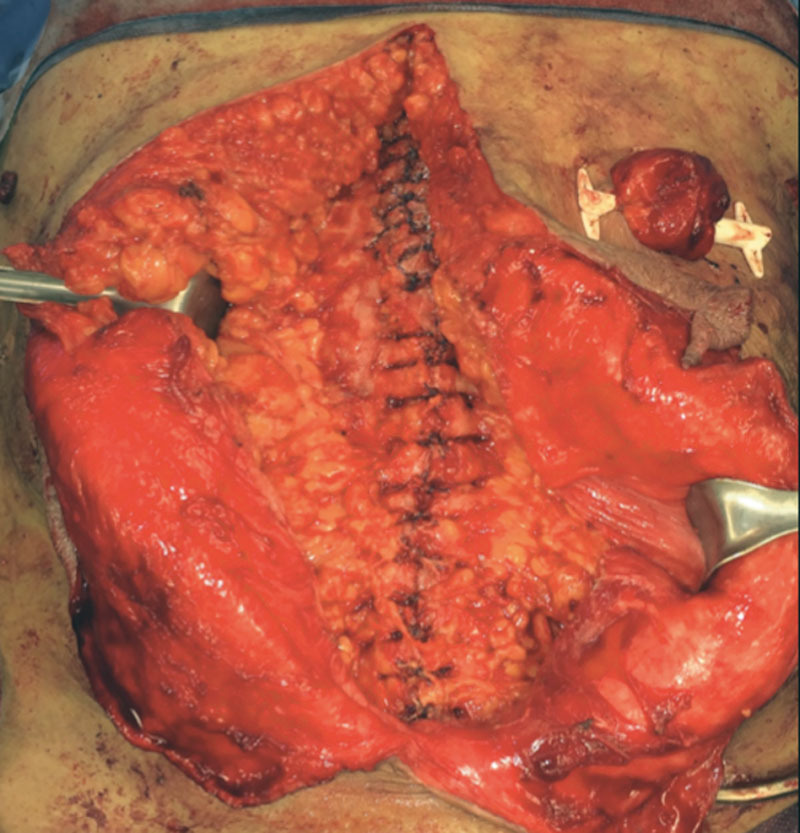
Fig. 13.
After polyglactin mesh removal and bilateral components releases with perforator preservation, mesh sutures were placed across the abdominal defect. The wound was relatively clean, with one pocket of purulence that was debrided.
Fig. 14.
Closure of 9-cm hernia defect with mesh sutured technique.
DISCUSSION
Small-diameter sutures concentrate force and pressure at the STI, leading to acute or chronic suture pull-through and surgical failure.11 Many materials have been implanted in an attempt to achieve a reliable high-tension closure including silver wire,12 dermal autograft strips,13 and collagen ribbon.14 The spacing of sutures to avoid tearing has intensely investigated.15 However, the problem may actually be the 3000-year-old suture design of a flexible linear thread that concentrates forces at the STI to achieve tissue apposition. Stagnant progress in the hernia repair field16 and a failure rate of suture repairs of incisional hernias of 63% at 10 years17 perhaps is explained by this reliance on the standard suture design for tissue approximation.
The long-term strength of an abdominal wall closure is important, as a number of hernias occur >1 year after closure.18 The strength of any repair is the sum of the physical construct and the scar of biologic healing. Humans have been assessed to encapsulate rather than to incorporate foreign materials than other species,19 and a mesh sutured repair uses this response to its advantage. The authors hypothesize that the mesh suture creates a magnified foreign body response because of its increased surface area in comparison to standard suture. The surface area of a 20-mm-wide mesh strip is over 34 times the surface area of a number 1 polypropylene suture. It is believed that a persistent foreign body response and associated scar formation will be important for the long-term strength of the closure. Experimental evidence shows that the foreign body response recedes when the foreign body disappears,20,21 and this may explain why abdominal wall scars after laparotomy and closure with absorbable sutures are only 70% as strong as unscarred linea alba.22 Foreign body-induced scar from implanted polypropylene23 is localized to the site of abdominal wall closure and magnified by the high surface area. Our hernia recurrence rate of <4% at the early mean follow-up time of 234 days is encouraging and is much less than expected, when compared to a cohort of similarly complex sutured repairs performed by the senior author.24 This ability is attributed to reliably suture wide abdominal defects (and avoid planar mesh) due to this magnified foreign body response, as these strips had the tensile strength of standard number one polypropylene sutures. Numerous types of defects were closed with or without components releases, relying on the distribution of forces to limit or avoid pull-through. The results are similar to that described for polypropylene “bands” that are introduced from semilunar line to semilunar line to close a midline defect, but were not tied to themselves to create a knot.25 Efficacy of the mesh strips is most dramatically demonstrated in the 49 repairs CDC grades 2–4. Only one patient had a hernia in these complex cases despite an average transverse hernia width of 10.2 cm. The remaining 48 patients maintained unscarred tissue planes for a later planar mesh closure if necessary.
The safety of mesh sutured repairs can be assessed with comparisons to both sutured closures of the abdominal wall and planar mesh hernia repairs in contaminated fields. The SSI rate of 4.6% for the entire cohort is less than a recent meta-analysis for sutured ventral hernia closures of 6.6%.26 The SSI rate of 6.1% for the 49 contaminated and clean-contaminated closures compares favorably to a 14–15% 30-day SSI rate in 2 recent studies of nonsterile planar mesh repairs27,28 Of the 31 closures not done for hernias, 10 were for fascial dehiscence after laparotomy—a situation regarded to be challenging with high failure rates.29 Mesh sutured repairs employ far less foreign material and require less tissue dissection than do planar mesh repairs. The fact that the majority of the prosthetic material is incorporated and thus located within tissue, as opposed to lying on its surface as do planar meshes, most probably is protective against infection. There is a minimal contact of the mesh strip with the bowel unlike intra-abdominal meshes. Finally, the authors feel that the physical attributes of the mesh are extremely important. Biomaterials with pores >1 mm generate the most biocompatible tissue response.30 Resistance to infection is evidenced by several patients with exposed mesh strips who healed with local wound care. The polypropylene filaments used in this particular mesh are measured by microCT to be 0.14 mm in diameter, and this compares to 0.4 mm for number 1 polypropylene. There may be a threshold in humans for the ability of a narrow filament foreign body to be cleared of surface bacteria, with the thinner the better. We have observed that small-diameter sutures (3-0 and smaller) do not form deep stitch abscesses, and we question whether the exceedingly low infection rate of intravascular stents despite episodes of transient bacteremia31 is due to the thin size of the metal filaments (0.08 mm) rather than their material composition.
Another issue for tissue tolerance is the physical characteristics of the mesh strip knots. Mesh strips are predominantly air and therefore the filaments collapse when tied to produce a small knot. Unlike the knots of solid sutures, the knots of mesh sutures still maintain an element of porosity (confirmed by microCT) that permit tissue incorporation, and may explain only a single knot being removed in this series.
Our enthusiasm for this technique is tempered by the relatively short follow-up. Categorization of results is difficult considering the varied types of defects closed with this technique. Although the passage of mesh strips with the aid of a sharp clamp is clumsy, a mesh suture with an attached needle is in development. Despite the lack of an attached needle, in our hands, a mesh sutured repair is both versatile and fast, in addition to avoiding the placement of a planar mesh with its required tissue dissection. These repairs avoid the sizeable costs associated with the bioprosthetic meshes often encouraged for use in contaminated situations. Long-term studies incorporating safety, efficacy, and cost will determine the proper place for this new abdominal wall closure technique and are underway.
ACKNOWLEDGMENT
The authors thank Dr. Carmen Soriano for her assistance.
Supplementary Material
Footnotes
Supported by internal funding. The use of the advanced photon source for measurement of mesh suture area was supported by the US Department of Energy, Office of Science, Office of Basic Energy Sciences, under contract number DE-AC02-06CH11357.
Disclosure: Dr. Dumanian has financial interest and is an officer of the Advanced Suture Co. and the Mesh Suture Co. He could potentially benefit from the outcomes of this research. Neither of the other authors has any financial disclosures. The Article Processing Charge was paid for by the Division of Plastic Surgery, Northwestern Feinberg School of Medicine.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Muysoms FE, Detry O, Vierendeels T, et al. Prevention of incisional hernias by prophylactic mesh-augmented reinforcement of midline laparotomies for abdominal aortic aneurysm treatment: a randomized controlled trial. Ann Surg. 2016;263:638–645. doi: 10.1097/SLA.0000000000001369. [DOI] [PubMed] [Google Scholar]
- 2.Burger JW, Luijendijk RW, Hop WC, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240:578–583. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Höer J, Fischer L, Schachtrupp A. Laparotomy closure and incisional hernia prevention - what are the surgical requirements? Zentralbl Chir. 2011;136:42–49. doi: 10.1055/s-0030-1262682. [DOI] [PubMed] [Google Scholar]
- 4.Souza JM, Dumanian Z, Gurjala D, et al. In vivo evaluation of a novel mesh suture design for abdominal wall closure. Plast Reconstr Surg. 2015;135:322e–330e. doi: 10.1097/PRS.0000000000000910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumanian GA, Tulaimat A, Dumanian ZP. Experimental study of the characteristics of a novel mesh suture. Br J Surg. 2015;102:1285–1292. doi: 10.1002/bjs.9853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stock SR. Recent advances in X-ray microtomography applied to materials. Int Mat Rev. 2008;53:129–181. [Google Scholar]
- 7.Doube M, Kłosowski MM, Arganda-Carreras I, et al. BoneJ: free and extensible bone image analysis in ImageJ. Bone. 2010;47:1076–1079. doi: 10.1016/j.bone.2010.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko JH, Salvay DM, Paul BC, et al. Soft polypropylene mesh, but not cadaveric dermis, significantly improves outcomes in midline hernia repairs using the components separation technique. Plast Reconstr Surg. 2009;124:836–847. doi: 10.1097/PRS.0b013e3181b0380e. [DOI] [PubMed] [Google Scholar]
- 9. Available at: http://www.cdc.gov/hicpac/SSI/table7-8-9-10-SSI.html. Accessed June 24, 2016.
- 10.Breuing K, Butler CE, Ferzoco S, et al. Ventral Hernia Working Group. Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery. 2010;148:544–558. doi: 10.1016/j.surg.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Witherbee OO US Patent 784018, 2/28/1905
- 12.Reid MR, Zinninger MM, Merrell P. Closure of the abdomen with through-and-through silver wire sutures in cases of acute abdominal emergencies. Ann Surg. 1933;98:890–896. doi: 10.1097/00000658-193311000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marchac D, Kaddoura R. Repair of large midline abdominal-wall hernias by a running strip of abdominal skin. Plast Reconstr Surg. 1983;72:341–346. doi: 10.1097/00006534-198309000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Didusch WP US Patent 2143910, 1/17/1939
- 15.Petter-Puchner AH. The state of midline closure of the abdominal wall. Br J Surg. 2015;102:1446–1447. doi: 10.1002/bjs.9932. [DOI] [PubMed] [Google Scholar]
- 16.Fischer John P, Basta Marten N, Mirzabeigi Michael N, et al. A risk modeal and cost analysis of incisional hernia after elective abdominal surgery based upon 12373 cases: the case for targeted prophylactic intervention. Ann Surg. 2016;263:1010–1017. doi: 10.1097/SLA.0000000000001394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burger JWA, Luijendijk RW, Hop WCJ, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240:578–585. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellis H, Gajraj H, George CD. Incisional hernias: when do they occur? Br J Surg. 1983;70:290–291. doi: 10.1002/bjs.1800700514. [DOI] [PubMed] [Google Scholar]
- 19.Sauvage LR, Berger KE, Wood SJ, et al. Interspecies healing of porous arterial prostheses. Arch Surg. 1974;109:698–705. doi: 10.1001/archsurg.1974.01360050092020. [DOI] [PubMed] [Google Scholar]
- 20.Thomson HG. The fate of the pseudosheath pocket around silicone implants. Plast Reconstr Surg. 1973;51:667–671. doi: 10.1097/00006534-197306000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Otto J, Binnebosel M, Pietsch S, et al. Large-pore PDS mesh compared to small-pore PG mesh. J Invest Surg. 2010;23:190–196. doi: 10.3109/08941931003739741. [DOI] [PubMed] [Google Scholar]
- 22.Hollinsky C, Sandberg S. Measurement of the tensile strength of the ventral abdominal wall in comparison with scar tissue. Clin Biomechanics. 2007;22:88–92. doi: 10.1016/j.clinbiomech.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Vogels RR, Lambertz A, Schuster P, et al. Biocompatibility and biomechanical analysis of elastic TPU threads as new suture material. J Biomed Mater Res B Appl Biomater. 2015 doi: 10.1002/jbm.b.33531. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Ko JH, Salvay DM, Paul BC, et al. “Components Separation” technique for the treatment of complex abdominal wall defects: an 11-year experience in 200 patients. Arch Surg. 2009;144:1047–1055. doi: 10.1001/archsurg.2009.192. [DOI] [PubMed] [Google Scholar]
- 25.Sahm M, Kube R, Rose J, et al. Rectusbanding: a method for the repair of incisional hernias. Hernia. 2009;13:481–486. doi: 10.1007/s10029-009-0516-z. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen MT, Berger RL, Hicks SC, et al. Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhapy: a systemic review and meta-analysis. JAMA Surg. 2014;149:415–421. doi: 10.1001/jamasurg.2013.5014. [DOI] [PubMed] [Google Scholar]
- 27.Carbonell AM, Criss CN, Cobb WS, et al. Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg. 2013;217:991–998. doi: 10.1016/j.jamcollsurg.2013.07.382. [DOI] [PubMed] [Google Scholar]
- 28.Bondre IL, Holihan JL, Askenasy EP, et al. Suture, synthetic, or biologic in contaminated ventral hernia repair. J Surg Res. 2016;200:488–494. doi: 10.1016/j.jss.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Abbott DE, Dumanian GA, Halverson AL. Management of laparotomy wound dehiscence. Am Surg. 2007;73:1224–1227. [PubMed] [Google Scholar]
- 30.Zhu LM, Schuster P, Klinge U. Mesh implants: an overview of crucial mesh parameters. World J Gastrointest Surg. 2015;7:226–236. doi: 10.4240/wjgs.v7.i10.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elieson M, Mixon T, Carpenter J. Coronary stent infections: a case report and literature review. Tex Heart Inst J. 2012;39:884–889. [PMC free article] [PubMed] [Google Scholar]


