Background:
Reconstruction after mastectomy is an important milestone for many women treated for breast cancer. However, because many surgeons only offer their preferred method of reconstruction, it is not clear which approach women would choose if offered a genuine choice.
Methods:
Between 1998 and 2010, the breast reconstruction service at a major Australian teaching hospital was staffed by a single plastic surgeon trained in both prosthetic and autologous breast reconstruction techniques. The choices of all 837 women who underwent reconstruction were compared across time for publicly and privately funded patients using binary logistic regression.
Results:
Overall, women chose prosthetic over autologous reconstruction at a ratio of 4.7:1. This ratio increasingly favored prosthetic reconstruction over time, though less strongly for private patients who did not face a 3-year waiting list for autologous reconstruction.
Conclusions:
Financial constraints affected these women’s reconstruction choices. Nevertheless, and in contrast to the situation in the United States, these women clearly favored prosthetic over autologous reconstruction.
Breast cancer is the most common cancer for Australian women, excluding nonmelanoma skin cancers.1 Despite recent advances in screening, detection, diagnosis, and treatment, many women with breast cancer still require mastectomy as the mainstay of the treatment for their cancer.2 As the breast is a symbol of femininity, a mastectomy can result in psychological, sexual, and emotional distress with associated aesthetically displeasing appearance. Hence, breast reconstruction is an important part of the treatment and management of the patients with breast cancer.3–5
The aim of breast reconstruction is to recreate a breast mound that restores the physical balance for women after mastectomy and has the appearance of a normal breast in clothing. It also has important psychosexual benefits3–5 and many patients report a sense of “closure” of their cancer treatment and not being reminded of their breast cancer or mastectomy each time they got dressed. The main methods of breast reconstruction methods are as follows: (1) prosthetic (tissue expander followed by implant or implant alone); (2) autologous, that is, pedicled or free transverse rectus abdominis myocutaneous (TRAM) flap, free deep inferior epigastric perforator (DIEP), or other perforator flaps; and (3) a combination of autologous tissue and prosthesis as in a latissimus dorsi (LD) myocutaneous flap with a tissue expander followed by an implant or implant alone.6 Any of these options can be initiated at the time of mastectomy as an immediate breast reconstruction or later as a delayed breast reconstruction. Each of these options is associated with advantages and disadvantages that need to be explained to each patient considering breast reconstruction to assist them in making an informed decision that is personalized and with her best interest in mind, fitting in the overall plan of their treatment of breast cancer rather a particular surgeon’s preference. However, many surgeons favor one method over another and it is not clear which one would women choose if they had a genuine choice.7–9
Historically, breast reconstruction after mastectomy in both the state of New South Wales and the whole of Australia was reported as low, approximately 5%–6%.10 At the Westmead Breast Cancer Institute, we have commenced a dedicated breast reconstruction service since 1998 by a single plastic surgeon (TL), who is trained in both prosthetic and autologous breast reconstruction techniques. In both our private and public hospitals, we were able to offer patients mastopexy, reduction mammoplasty, or augmentation mammoplasty of the contralateral side whenever necessary, as they are not considered a cosmetic procedure.
The aim of this study is to assess the trend of breast reconstruction choices made by the breast cancer patients requiring a mastectomy, who were offered a choice of various breast reconstruction methods by Dr. Lam over a 12.5-year period.
PATIENTS AND METHODS
From June 1998 to December 2010, all breast cancer patients who consulted Dr. Lam and went on to breast reconstruction were included in this study. The research was approved by the hospital’s Human Research Ethics Committee.
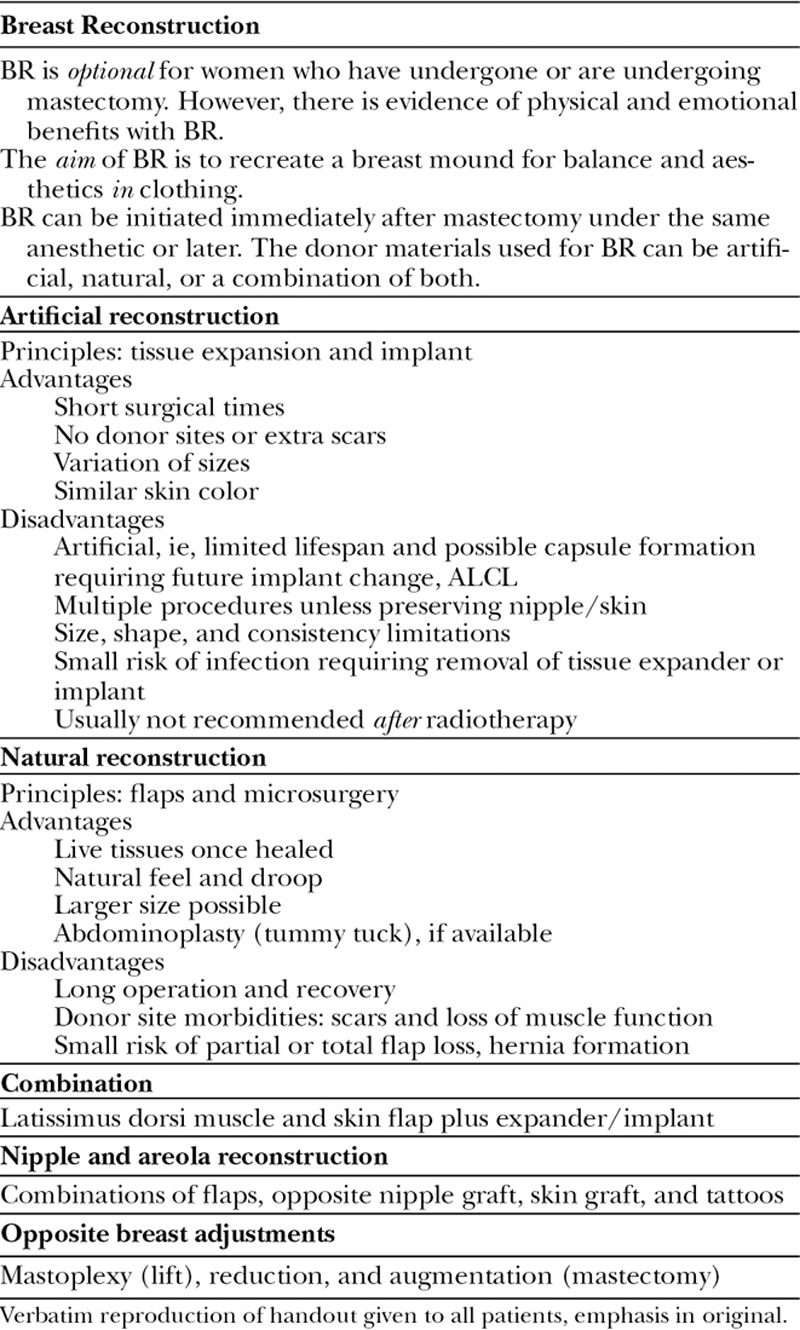
All patients received the same, standard written information about the aim and options of the various methods of breast reconstruction (Table 1). This is supplemented by the surgeon verbally going through the information sheet accompanied by clinical photographs of previous patients, and then concluded by questions and answers. A typical initial consultation takes approximately 1 hour. Delayed breast reconstruction patients often return for the second consultation before undergoing surgery.
Table 1.
Standard Breast Reconstruction Discussion Information Sheet
The trend of the breast reconstruction choices is analyzed over the first two 5-year periods and the remaining 2.5-year period, each included approximately equal proportions of patients. In addition, the trend is analyzed to assess if there is a difference between immediate breast reconstruction and delayed breast reconstruction groups, and also public- versus private-hospital patients.
Analysis consisted of binary logistic regression computing the odds of choosing prosthetic over autologous reconstruction. Comparisons were considered significant at p ≤ 0.05. Analysis was performed using Statistical Package for the Social Sciences 22.0.
RESULTS
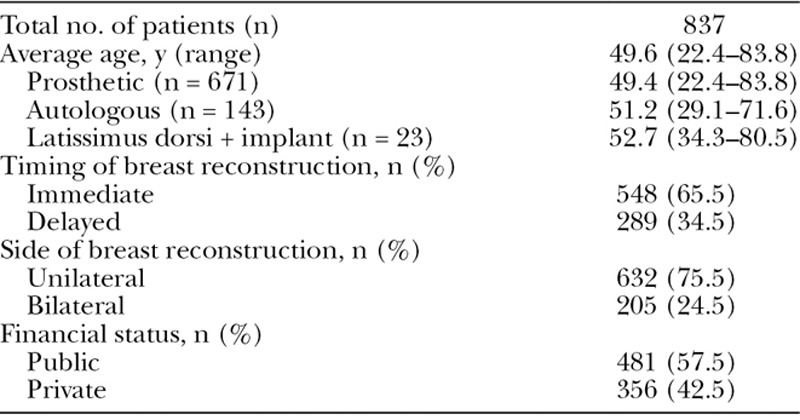
During the review period between June 1998 and December 2010, 837 breast reconstructions were carried out by Dr. Lam. The average age of these patients was 49.6 years (range 22.4–83.8). The largest group of patients, totaling 671 (80.1%), underwent prosthetic breast reconstruction with an average age of 49.4 years (range 22.4–83.8). The prosthetic-only breast reconstruction patients, totaling 181, received radiotherapy: 32 (20.0%) in the initial 5-year period, 81 (28.8%) in the second 5-year period, and 68 (29.4%) in the final 2.5 years. There were 189 (28.1%) bilateral cases in the prosthetic-only group overall, and 143 patients (17.1%) who underwent autologous TRAM or DIEP flap breast reconstructions with an average age of 51.2 years (range 29.1–71.6). The remaining 23 patients underwent a combination of an LD myocutaneous flap and an implant, with their average age of 52.7 years (range 34.3–80.5; Table 2). There were 632 (75.5%) unilateral cases, whereas the remaining 205 (24.5%) were bilateral breast reconstructions.
Table 2.
Breast Reconstruction Patient Demographics between 1998 and 2010
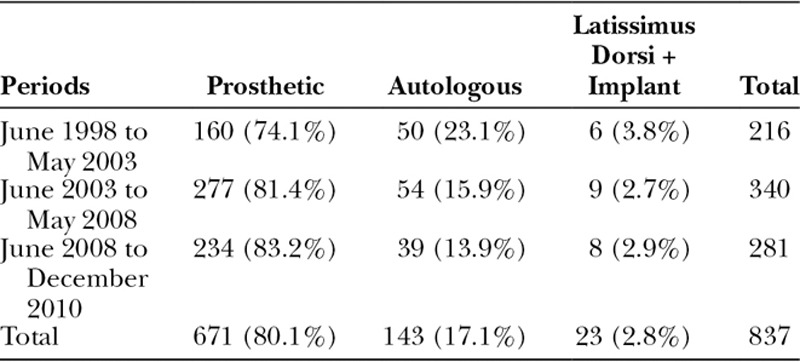
In the initial 5-year period, there were 160 (74.1%) prosthetic, 50 autologous (23.1%), and 6 combined (3.8%) breast reconstructions, with a prosthetic-to-autologous ratio (excluding combined) of 3.2:1. In the second 5-year period, the count was 277 (81.4%), 54 (15.9%), and 9 (2.7%) breast reconstructions, respectively, with a prosthetic-to-autologous ratio of 5.1:1. The increase in the ratio was statistically significant, (odds ratio [OR] = 1.60, 95% confidence interval [CI]: 1.04–2.47, p = 0.03). The final 2.5 years had 234 (83.2%), 39 (13.9%), and 8 (2.9%) breast reconstructions, respectively, resulting in a prosthetic-to-autologous ratio of 6:1. Although, this did not constitute a significant change compared to the second 5-year period (OR = 1.17, 95% CI: 0.75–1.83, p = 0.49). The prosthetic-to-autologous ratio for the overall period was 4.7:1 (Table 3).
Table 3.
Types of Breast Reconstruction Performed between 1998 and 2010
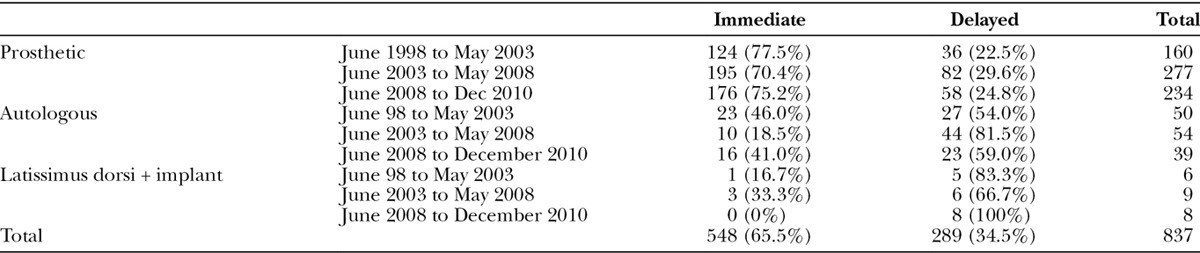
There were 548 (65.5%) immediate and 289 (34.5%) delayed breast reconstruction cases. Based on the timing of the breast reconstruction for each type, subdivision of the data over the 3 study periods is as follows. For prosthetic, there were 124 (77.5%), 195 (70.4%), and 176 (75.2%) immediate and 36 (22.5%), 82 (29.6%), and 58 (24.8%) delayed breast reconstruction patients. For autologous, there were 23 (46.0%), 10 (18.5%), and 16 (41.0%) immediate and 27 (54.0%), 44 (81.5%), and 23 (59.0%) delayed breast reconstruction patients. The autologous reconstructions were significantly more likely to be delayed than prosthetic reconstructions (OR = 5.40, 95% CI: 3.67–7.94, p < 0.0005). The remaining 23 combined breast reconstruction patients were mostly delayed breast reconstruction cases (Table 4).
Table 4.
Immediate versus Delayed Breast Reconstructions between 1998 and 2010
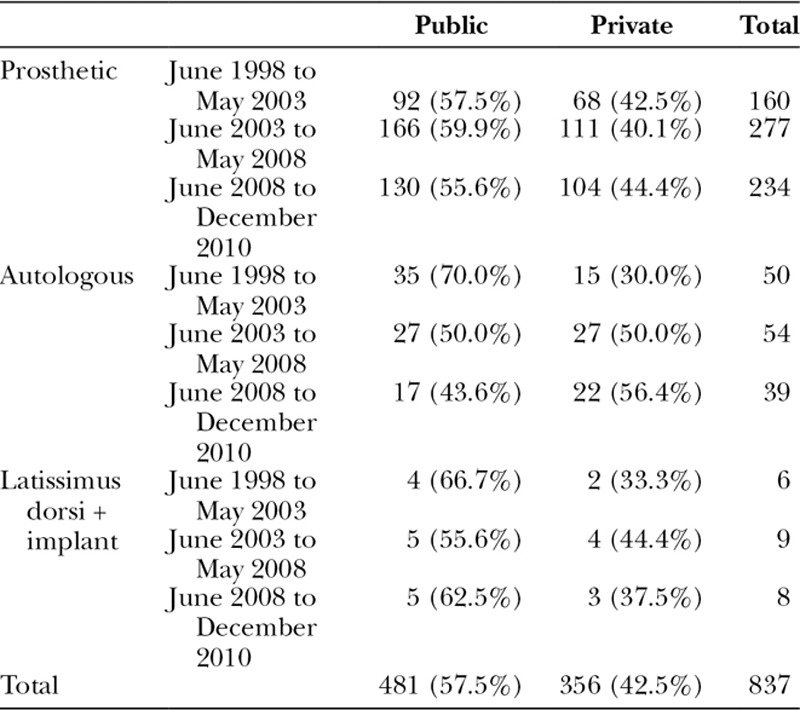
As to the financial status of our patients, 481 (57.5%) were treated in a public hospital setting, whereas 356 (42.5%) were treated in private hospitals. The number of prosthetic breast reconstruction patients treated in the public hospitals versus private hospitals were 92 (57.5%)/68 (42.5%), 166 (59.5%)/111 (40.1%), and 130 (55.6%)/104 (44.4%), respectively, for the 3 study periods. For autologous cases, the corresponding numbers were 35 (70.0%)/15 (30.0%), 27 (50.0%)/27 (50.0%), and 17 (43.6%)/22 (56.4%). That is, compared to patients in private hospitals, women in public hospitals increasingly chose prosthetic over autologous reconstructions in the second 5-year period than the first (OR = 2.58, 95% CI = 1.05–6.33, p = 0.04). There was no further significant change in preference from the second 5-year period to the final 2.5-year period (OR = 1.08, 95% CI: 0.44–2.66, p = 0.86). There were slightly more public over private patients for the remaining 23 LD myocutaneous plus implant patients (Table 5).
Table 5.
Financial Status of Breast Reconstruction Patients between 1998 and 2010
DISCUSSION
Breast reconstruction has been established to be an integral part of breast cancer treatment after mastectomies.3–9 This study showed an increase in breast reconstruction in the Westmead Hospital in Western Sydney since the service started in 1998. It is believed that a dedicated plastic surgery service in breast reconstruction is the basis of this increase, as part of a multidisciplinary team approach.11 In addition, there are also patient advocate groups that promote better breast cancer treatment and reconstruction leading to improved patient awareness of breast reconstruction.12 At present, the immediate breast reconstruction rate in newly diagnosed breast cancer patients at the Westmead Breast Cancer Institute is estimated to be around 40–50%, which is a significant increase from the reported historical lows of around 5%.10
The rate of breast reconstruction has also increased recently in the United States, from a low of 3.4% in the 1980s to a high of 59% in some centers.13–21 Passing of the Women’s Health and Cancer Right Act in 1998 may have provided the stimulus of the increase.22 Interestingly, previous studies of US population reported a ratio of 3:1 autologous to implant breast reconstruction.15,23 However, in this Australian sample, the ratio was reversed, with three times as many women undergoing prosthetic reconstructions from 1998 to 2003, increasing to six times by 2010. This trend toward a greater relative proportion of prosthetic reconstructions has been observed in the United States, with Albornoz et al21 reporting that the increased breast reconstruction rate between 1998 and 2008 was only in the prosthetic breast reconstruction, a massive 203%. The autologous reconstruction rate has remained unchanged,21 which would roughly bring the ratio of autologous-to-implant to about even. Although silicone implants had continuous approval by the U.S. Food and Drug Administration for use in breast reconstruction, the authors proposed that the reapproval of the silicone implant for cosmetic breast surgery might have led to more general acceptance. They also thought that increasingly more and more breast cancer sufferers are younger women who may not have adequate abdominal soft tissue available for autologous breast reconstruction such as a TRAM or DIEP flap, or simply not wanting to take time off work or family for extended recovery after such major undertakings. In addition, cultural shifts may have led to preference of the nonptotic appearance of implants as opposed to the natural appearance of the flaps. Our data suggest a further financial explanation: women in public hospitals were more likely to choose immediate prosthetic reconstruction over time to prevent a long wait for delayed reconstruction especially with autologous flaps, at least between 1998–2003 and 2003–2008. Other changes include the relative contraindication of adjuvant radiation therapy in implant type breast reconstruction seems to have been decreasing as increasing number of reports have confirmed satisfactory results in the majority of these patients.9,24–26 Finally, the recent interests in nipple or skin-sparing mastectomies and direct-to-implant breast reconstruction have already raised the percentage of breast reconstruction in this group of patients.27 It is expected that this rate will continue to increase with public educational initiatives such as the inaugural Breast Reconstruction Awareness Day on October 17, 2012 in the United States after a similar initiative in Canada the year before.
Our study is unique in that the majority (at least 95%) of newly diagnosed breast cancer patients seen at a major regional multidisciplinary breast cancer clinic over a 12.5-year period were referred to the same surgeon [TL] for discussion of a possible breast reconstruction. As he is trained in both prosthetic and autologous breast reconstruction and is commencing a new breast reconstruction service without much budgetary restrictions, all patients desiring breast reconstruction were accommodated. The standardized information sheet (Table 1) was designed to assist in retention of information and providing potential patients option of their choices. This sheet has virtually been unchanged until recently when we added the possibility of anaplastic larger cell lymphoma (ALCL) for discussion.
Our data showed the ratio of patients undergoing prosthetic breast reconstruction to autologous started in the first study period at 3.2:1 and ended at 6:1, with an overall ratio of 4.7:1. We are fortunate in Australia that all breast reconstructions are covered in both the public and private hospital systems, so financial consideration is not necessarily a deterrent to having breast reconstruction. However, as the public hospital resources is less than ideal, patients who opted for autologous breast reconstruction in a public hospital generally had a 3-year waiting time, which explains the trend of the ratio stretching out to 6:1 as the numbers build up in the public hospital waiting list because our study only counted patients who have had their breast reconstruction already. This is shown by the decreasing proportion of public autologous breast reconstruction from a high of 70.0% in the first study period down to 43.6% by the last study period. On the other hand, the waiting time for prosthetic breast reconstruction in the public sector is much shorter as a number of cases can be performed for the same amount of time used for an autologous free flap. As a result, the proportion of public patients undergoing prosthetic breast reconstruction was consistent over the 3 study periods ranging from 55.6% to 59.9%.
The majority of our patients who chose prosthetic breast reconstruction generally prefer a lesser surgical procedure without the sequelae of a surgical donor site, even though it involves more frequent visits and a second procedure. The rest were mainly interested in avoiding prosthetic material or desiring the additional benefits of a concomitant abdominoplasty. As a result, we have performed only a small number of combination of an LD myocutaneous flap and an implant, except for patients who did not have a suitable abdominal donor site and that the chest wall tissue was not adequate for tissue expansion.
Despite our best efforts, there are always potential for bias in our discussions with our patients. Putting the prosthetic option before the autologous breast reconstruction in the information sheet may lead to preoccupation of the patients’ mind with this method. However, reversing the order may lead to bias the other way around. Surgeon preference may also play a part although the senior author certainly do not shrink from performing autologous breast reconstruction with publications of cases made more difficult than the average free TRAM or DIEP by having a lower abdominal midline scar from previous operations.28,29 On the contrary, it is more likely that when patients in the public system who choose delayed breast reconstruction with the option of a free flap are informed of the waiting time of up to 3 years or 6–9 months for delayed prosthetic breast reconstruction, they might change their decision and lean toward an immediate prosthetic option. This study was conducted at one institution, which means the results should be considered preliminary until replicated elsewhere in Australia.
Patients considering delayed breast reconstruction often have the luxury of returning for a second consultation before making a final decision, whereas most immediate breast reconstruction patients would usually go on with their mastectomy and immediate breast reconstruction within a few weeks. As a result, some patients did report a degree of posttreatment regret in their decisions,30–32 and we have designed an interactive DVD with other patients’ testimonials and relaxation techniques, so that newly diagnosed breast cancer patients can work through their decision at their own pace at home.33
In summary, our study showed that when given the appropriate information and choice, our group of patients chose to undergo breast reconstruction in the ratio of around 4–5 prosthetic to 1 autologous flap reconstruction.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Bray F, McCarron P, Parkin DM. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004;6:229–239. doi: 10.1186/bcr932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmood U, Hanlon AL, Koshy M, et al. Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann Surg Oncol. 2013;20:1436–1443. doi: 10.1245/s10434-012-2732-5. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014–1025. doi: 10.1097/00006534-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg. 2003;111:1060–1068. doi: 10.1097/01.PRS.0000046249.33122.76. [DOI] [PubMed] [Google Scholar]
- 5.Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14:201–208. doi: 10.1016/j.breast.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Howard-McNatt MM. Patients opting for breast reconstruction following mastectomy: an analysis of uptake rates and benefit. Breast Cancer (Dove Med Press) 2013;5:9–15. doi: 10.2147/BCTT.S29142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watterson PA, Bostwick J, 3rd, Hester TR, Jr, et al. TRAM flap anatomy correlated with a 10-year clinical experience with 556 patients. Plast Reconstr Surg. 1995;95:1185–1194. doi: 10.1097/00006534-199506000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004;113:1153–1160. doi: 10.1097/01.prs.0000110328.47206.50. [DOI] [PubMed] [Google Scholar]
- 9.Cordeiro PG, Albornoz CR, McCormick B, et al. The impact of postmastectomy radiotherapy on two-stage implant breast reconstruction: an analysis of long-term surgical outcomes, aesthetic results, and satisfaction over 13 years. Plast Reconstr Surg. 2014;134:588–595. doi: 10.1097/PRS.0000000000000523. [DOI] [PubMed] [Google Scholar]
- 10.Boyages J, Jayasinghe U, Heard G, et al. The Management of Breast Cancer in New South Wales in 1995. Sydney: NSW Breast Cancer Institute and the Cancer Council NSW; 2004. p. p. 22. [Google Scholar]
- 11.Sandelin K, King E, Redman S. Breast reconstruction following mastectomy: current status in Australia. ANZ J Surg. 2003;73:701–706. doi: 10.1046/j.1445-2197.2003.02752.x. [DOI] [PubMed] [Google Scholar]
- 12.Crossing S. A Decade of Success: Cancer Voices NSW 2000–2010. Cancer Voices NSW; 2011. Available at: www.cancervoices.org.au. [Google Scholar]
- 13.Morrow M, Scott SK, Menck HR, et al. Factors influencing the use of breast reconstruction postmastectomy: a National Cancer Database study. J Am Coll Surg. 2001;192:1–8. doi: 10.1016/s1072-7515(00)00747-x. [DOI] [PubMed] [Google Scholar]
- 14.Polednak AP. How frequent is postmastectomy breast reconstructive surgery? A study linking two statewide databases. Plast Reconstr Surg. 2001;108:73–77. doi: 10.1097/00006534-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Alderman AK, McMahon L, Jr, Wilkins EG. The national utilization of immediate and early delayed breast reconstruction and the effect of sociodemographic factors. Plast Reconstr Surg. 2003;111:695–703; discussion 704. doi: 10.1097/01.PRS.0000041438.50018.02. [DOI] [PubMed] [Google Scholar]
- 16.Christian CK, Niland J, Edge SB, et al. A multi-institutional analysis of the socioeconomic determinants of breast reconstruction: a study of the National Comprehensive Cancer Network. Ann Surg. 2006;243:241–249. doi: 10.1097/01.sla.0000197738.63512.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reuben BC, Manwaring J, Neumayer LA. Recent trends and predictors in immediate breast reconstruction after mastectomy in the United States. Am J Surg. 2009;198:237–243. doi: 10.1016/j.amjsurg.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 18.Kruper L, Holt A, Xu XX, et al. Disparities in reconstruction rates after mastectomy: patterns of care and factors associated with the use of breast reconstruction in Southern California. Ann Surg Oncol. 2011;18:2158–2165. doi: 10.1245/s10434-011-1580-z. [DOI] [PubMed] [Google Scholar]
- 19.Elmore L, Myckatyn TM, Gao F, et al. Reconstruction patterns in a single institution cohort of women undergoing mastectomy for breast cancer. Ann Surg Oncol. 2012;19:3223–3229. doi: 10.1245/s10434-012-2530-0. [DOI] [PubMed] [Google Scholar]
- 20.Sisco M, Du H, Warner JP, et al. Have we expanded the equitable delivery of postmastectomy breast reconstruction in the new millennium? Evidence from the national cancer data base. J Am Coll Surg. 2012;215:658–666. doi: 10.1016/j.jamcollsurg.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 22.Alderman AK, Wei Y, Birkmeyer JD. Use of breast reconstruction after mastectomy following the Women’s Health and Cancer Rights Act. JAMA. 2006;295:387–388. doi: 10.1001/jama.295.4.387. [DOI] [PubMed] [Google Scholar]
- 23.Polednak AP. Type of breast reconstructive surgery among breast cancer patients: a population-based study. Plast Reconstr Surg. 2001;108:1600–1603. doi: 10.1097/00006534-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 24.Nava MB, Pennati AE, Lozza L, et al. Outcome of different timings of radiotherapy in implant-based breast reconstructions. Plast Reconstr Surg. 2011;128:353–359. doi: 10.1097/PRS.0b013e31821e6c10. [DOI] [PubMed] [Google Scholar]
- 25.Lam TC, Hsieh F, Boyages J. The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg. 2013;132:511–518. doi: 10.1097/PRS.0b013e31829acc41. [DOI] [PubMed] [Google Scholar]
- 26.Ho AL, Bovill ES, Macadam SA, et al. Postmastectomy radiation therapy after immediate two-stage tissue expander/implant breast reconstruction: a University of British Columbia perspective. Plast Reconstr Surg. 2014;134:1e–10e. doi: 10.1097/PRS.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 27.Wong A, Snook K, Brennan M, et al. Increasing breast reconstruction rates by offering more women a choice. ANZ J Surg. 2014;84:31–36. doi: 10.1111/ans.12471. [DOI] [PubMed] [Google Scholar]
- 28.Lam TC, Sellars GD. Free perforator crossover TRAM flap for breast reconstruction. Ann Plast Surg. 2003;50:126–131. doi: 10.1097/01.SAP.0000032307.61429.9E. [DOI] [PubMed] [Google Scholar]
- 29.Hsieh F, Somia N, Lam TC. A new approach to preexisting vertical midline abdominal scars with crossover DIEP flap breast reconstruction. Microsurgery. 2010;30:151–155. doi: 10.1002/micr.20705. [DOI] [PubMed] [Google Scholar]
- 30.Sheehan J, Sherman KA, Lam T, et al. Association of information satisfaction, psychological distress and monitoring coping style with post-decision regret following breast reconstruction. Psychooncology. 2007;16:342–351. doi: 10.1002/pon.1067. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan J, Sherman KA, Lam T, et al. Regret associated with the decision for breast reconstruction: the association of negative body image, distress and surgery characteristics with decision regret. Psychol Health. 2008;23:207–219. doi: 10.1080/14768320601124899. [DOI] [PubMed] [Google Scholar]
- 32.Roder D, Zorbas H, Kollias J, et al. Factors predictive of immediate breast reconstruction following mastectomy for invasive breast cancer in Australia. Breast. 2013;22:1220–1225. doi: 10.1016/j.breast.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 33.Sherman KA, Harcourt DM, Lam TC, et al. BRECONDA: development and acceptability of an interactive decisional support tool for women considering breast reconstruction. Psychooncology. 2014;23:835–838. doi: 10.1002/pon.3498. [DOI] [PubMed] [Google Scholar]


