Abstract
There is an urgent need to identify signs that harbinger onset of borderline personality disorder (BPD). Advancement in this area is required to refine developmental theories, discover etiological mechanisms, improve early detection, and achieve our ultimate goal of prevention. Though many studies have supported a wide range of factors that increase subsequent risk for BPD, this literature has yet to be critically evaluated, and there are no comprehensive reviews that examine and integrate these findings. To address this limitation, we conducted a systematic review to summarize and synthesize the current literature. Electronic databases were systematically searched for prospective, longitudinal studies that examined risk factors of subsequent BPD outcomes (features, symptoms, diagnosis) resulting in a total of 39 studies, reflecting 24 unique samples. Though increased risk for BPD was reliably attributed to multiple factors within social, family, maltreatment, and child domains, the most striking limitation of this research is its lack of disorder-specific findings Additional limitations, including notable heterogeneity in sampling methodology, symptom assessment methodology, and developmental timing of assessments, are discussed in terms of how close are we to pinpointing who is most at risk and why in an attempt to provide a roadmap for future research.
Keywords: systematic review, borderline personality disorder, risk factors, development
Borderline personality disorder (BPD) is a serious mental illness that typically emerges during adolescence or young adulthood and is characterized by multiple debilitating symptoms, including emotional dysregulation, tumultuous interpersonal relationships, and impulsive behaviors (Chanen, 2015; Lieb, Zanarini, Schmahl, Linehan, & Bohus, 2004). The disorder is associated with a high mortality rate: up to 10% of patients commit suicide (Paris & Zweig-Frank, 2001; Zanarini, Frankenburg, Hennen, & Silk, 2003). Furthermore, severe psychosocial impairment can linger for decades after remission (Bagge et al., 2004; Paris & Zweig-Frank, 2001; Skodol et al., 2005). The level of impairment associated with BPD and its public health significance are reflected in its prevalence across adult and adolescent clinical settings, with approximately 10–20% of outpatients and up to 50% of inpatients meeting criteria (Glenn & Klonsky, 2013; Korzekwa, Dell, Links, Thabane, & Webb, 2008; Widiger & Weissman, 1991). These devastating consequences speak to the urgent need to identify signs that harbinger onset of the acute, fully developed illness. Successfully identifying such markers would hasten the refinement of developmental theories, accelerate the discovery of etiological mechanisms, enable early detection and diagnosis, and may provide fruitful targets for early intervention. Advancements in these areas are required to achieve our ultimate goal: deflecting the course of personality development away from BPD outcomes.
Along these lines, there has burgeoning interest in early risk factors for the disorder throughout the past decade (Kongerslev & Chanen, 2015). Much of this work supports a wide range of factors that increase subsequent risk for BPD, including broad social indices, family influences, exposure to maltreatment and trauma, and various child characteristics; however, these findings have yet to be thoroughly evaluated. So while this research may signal progress toward our ultimate goal, a comprehensive examination of the existing literature is critical for integrating our current knowledge, identifying remaining gaps, and providing a roadmap for future research. Therefore, we performed a systematic review of all longitudinal, prospective studies that examined risk factors for the development of BPD. Our goals were two-fold. First, to summarize and synthesize results across identified studies, including detailing risk factors that are consistently supported and discussing strengths and limitations of the existing literature. Second, we sought to determine if prevailing evidence regarding BPD risk factors facilitates sharpening developmental theories, explaining etiology, and identifying those in need of early intervention. In sum, how close are we to pinpointing who is most at risk and why?
Method
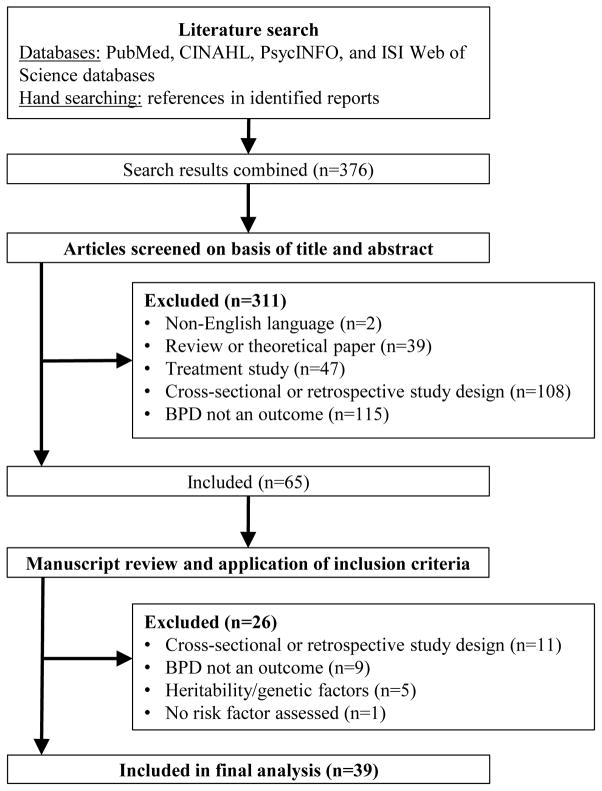
We obtained all peer-reviewed, English-language studies published through September 2015 from (a) PubMed, CINAHL, PsycINFO, and ISI Web of Science databases using the following search algorithm: (borderline personality AND [longitudinal OR follow-up* OR prospect*] AND [precursor* OR risk factor* OR prodrom* OR antecedent* OR predict*] AND [diagnosis OR development]); (b) hand searches of reference lists in identified studies and relevant review papers. Eligibility status for all retrieved articles was determined in two stages. First, all studies were screened based upon title and abstract using EPPI-Reviewer software (Thomas, Brunton, & Graziosi, 2010). Next, studies passing the initial title and abstract screen were reviewed based upon the full manuscript. Articles selected for final analysis met the following criteria: (1) prospective, longitudinal studies of any follow-up duration with at least 2 assessment points (2) outcome included BPD features, symptoms, or diagnosis and (3) the predictor (i.e., putative risk factor) was measured prior to the outcome assessment of BPD. Additionally, studies were excluded if they met the following criteria at either stage: (1) tested an intervention, as its impact on the risk factor and BPD outcome could not be determined; or (2) focused solely on heritability or genetic factors, as these are fixed markers and not sensitive to time of assessment. The three authors performed independent evaluations based on PRISMA-P (Shamseer et al., 2015) guidelines, with methods and inclusion criteria specified in advance and documented in a protocol. Any disagreements between reviewers were resolved by consensus.
We identified a total of 39 studies, resulting from 24 unique samples that met the aforementioned criteria (Figure 1). Participants totaled 43,681 (range = 56 – 6050), the majority of which were female (54%) and Caucasian (69%).1 Only eight of the 39 included studies utilized clinical samples (23%) and the vast majority used community samples (n = 31, 73%), of which 13 (42%) were ‘high-risk’ as defined by selection or oversampling based on a putative specific risk factor (i.e., poverty). Across all included studies, risk factors were assessed, on average, at 13 years (SD = 5.9 years; range = birth – 29 years). Outcome assessments occurred between ages 12 and 43 (M = 20 years; SD = 5.4 years), with the majority of studies examining symptoms (n = 29, 74%), eight studies (21%) examining diagnosis, and one study examining features (Belsky et al., 2012). The time between the risk factor assessment and the follow-up BPD assessment ranged from 1 to 28 years (M = 10.5 years, SD = 7 years). Retention of original sample was acceptable (M = 76%, SD = 16%); however, rates varied substantially (39% – 97%).2
Figure 1.
Study selection flow chart following Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols. All articles retrieved from the literature search were first screened on the basis of title and abstract. Those manuscripts deemed eligible from the screening phase were then reviewed using study inclusion criteria. Reasons for study exclusion are listed at each stage. Forty studies were ultimately eligible and included in the final analysis.
For the purpose of the current systematic review, studies were categorized based on type of risk examined: (1) broader social factors (e.g., poverty, stressful life events); (2) family factors, including parent psychopathology, parenting behavior/style, and family climate/parent-child relationship; (3) maltreatment and other trauma exposures (e.g., physical abuse, sexual abuse, neglect); and (4) child factors, including cognitive ability, attachment to caregiver, temperament and personality, and psychopathology. Results are discussed within each domain; studies including more than one risk factor appear multiple times. Analyses conducted in multiple steps are discussed in terms of findings from final analyses. Significant variability in study characteristics precluded statistical evaluation of predictive power and effect sizes.
Results
Broader Social Risk Factors
We identified nine studies that examined one or more indices of broader social risk (Table 1). Four studies assessed low socioeconomic status (SES) and results consistently supported a prospective relationship with later BPD outcomes. Crawford and colleagues (2009) found family SES at age 5 to predict BPD symptoms more than 20 years later. Relatedly, Cohen and colleagues (2008) demonstrated a protracted and stable relationship between family SES and BPD symptom trajectories across adolescence and adulthood. Finally, Stepp and colleagues (2014a; 2014b) found receipt of public assistance to predict BPD symptoms across adolescence.
Table 1.
Summary of Longitudinal Research Investigating Broader Social Risk Factors Predicting Borderline Personality Disorder (BPD)
| Study | Sample
|
Risk factor
|
BPD Outcome
|
Summary of results | ||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Type (cohort) | Follow-up (retention) | Construct | Age in years | Construct (measure) | Age in years | ||
| Cohen et al. (2008) | n=680; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (70%) | SES | 13, 16, 22 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Lower SES predicted BPD sxs and effect magnitude remained stable over time. |
| Stressful Life Events | 13, 16, 22 | Stressful life events predicted BPD sxs. | ||||||
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Life Stress | 3–42 mos, 6–11 | BPD sxs (SCID-II) | 28 | Life stress in infancy/childhood predicted higher BPD sxs. |
| Family Disruption | 1–18 | NO ASSOCIATION in final analyses. (Family disruption significant in bivariate analyses) | ||||||
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | SES | 5 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Lower SES predicted BPD sxs. |
| Marital Conflict | 13 | NO ASSOCIATION in analyses. | ||||||
| Winsper et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Family Adversity | PREG: 8, 12, 18, 32 wks | BPD sxs (CI-BPD) | 12 | Family adversity predicted BPD sxs and was mediated by IQ. |
| Stepp et al. (2014a) | n=2282; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 14 yrs (93%) | Poverty: Public Assist | 6.5 | BPD sxs (IPDE-B) | 14–19 | Public assistance predicted BPD sxs at age 14. |
| Stepp et al. (2014b) | n=2212; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | Poverty: Public Assist | 14 | BPD sxs (IPDE-B) | 14–17 | Public assistance predicted BPD sxs at age 14 and increases in BPD sxs. |
| Greenfield et al. (2015) | n=204; 69% female; 70% Caucasian |
Clinical: Inpt | 4 yrs (71%) | Stressful Life Events | 15 | BPD dx (Ab-DIB) | 18 | No ASSOCIATION in analyses. |
| Stepp et al. (2015) | n=113; 100% female; 33% Caucasian |
Community: High-Risk (PGS) | 10–13 yrs (97%) | Adversity, Public Assist, Single-Parent | 5–16 | BPD sxs (IPDE-B) | 16–18 | Adversity predicted increases in BPD sxs. |
| Conway et al. (2015) | n=700; 52% female; 92% Caucasian |
Community: High Risk (Mater-U) | 5 yrs (86%) | Acute Life Stress | 15 | BPD sxs (SCID-II) | 20 | NO ASSOCIATION in final analyses. (Acute stressors significant in bivariate analyses) |
| Chronic Stress | 15 | Family & school stressors predicted BPD sxs. (All stressors significant in bivariate analyses) | ||||||
Note. Ab-DIB=Abbreviated Diagnostic Interview for Borderlines, ALSPAC=Avon Longitudinal Study of Parents and Children, BPD=borderline personality disorder, CI-BPD=Childhood Interview for DSM BPD, CIC=Children in the Community, CIC-SR=CIC Self-Report Scale, dx=diagnosis, Inpt=inpatient; IPDE-B=International Personality Disorders Examination-Borderline Screener, mos=months, Mater-U=Mater University Study, NR=not reported, PGS=Pittsburgh Girls Study, PREG=during pregnancy, SCID-II=Structured Clinical Interview for DSM Axis II Disorders, SES= socioeconomic status, sxs= symptoms, wks=weeks, yrs=years.
Results from an additional four studies demonstrated a fairly consistent link between life stress and later BPD. Stressful life events (i.e., various psychosocial stressors) as measured in infancy, childhood, and adolescence predicted BPD symptoms in adulthood (Carlson, Egeland, & Sroufe, 2009; Cohen et al., 2008). Additionally, chronic (but not acute) family and school stressors in adolescence were linked to BPD symptoms in adulthood (Conway, Hammen, & Brennan, 2015). In contrast, Greenfield and colleagues (2015) did not find an effect of stressful life events measured at age 15 on the likelihood of BPD diagnosis approximately 3 years later. Stark differences in sampling strategies may explain these disparate findings.3
Four studies examining the association between family adversity and BPD symptoms produced mixed results, which may be attributable to variability in measurement of family adversity. Positive findings were evident in two community studies examining family adversity (broadly defined) during pregnancy (Winsper, Zanarini, & Wolke, 2012) and across childhood and adolescence (Stepp, Scott, Jones, Whalen, & Hipwell, 2015). Two additional community samples examined more specific indices, namely family disruption (Carlson et al., 2009) and marital conflict (Crawford et al., 2009), no significant prospective associations were found.
Family Factors
Nineteen studies assessed family factors (Table 2) and seven examined multiple indices.
Table 2.
Summary of Longitudinal Research Investigating Family Risk Factors Predicting Borderline Personality Disorder (BPD)
| Study | Sample | Risk factor | BPD Outcome | Summary of results | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristics | Type (Cohort) |
Follow-up (Retention) |
Construct | Age in years |
Construct (Measure) |
Age in years |
||
|
Parent/Family Psychopathology
| ||||||||
| Bezirganian et al. (1993) | n=776; 48% female; 90% Caucasian |
Community: Population | 3 yrs (79%) | Maternal Ego Integration; Interpersonal Difficulty; Impulsivity | 14 | BPD dx (SCID) | 16 | NO ASSOCIATION in final analyses. (Maternal ego integration significant in bivariate analyses) |
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Maternal hx of Medical Problems | Prenatal | BPD sxs (SCID-II) | 28 | NO ASSOCIATION in final analyses. (Maternal hx of serious medical problems significant in bivariate analyses) |
| Crawford et al. (2009) | n=776; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Maternal Interpersonal Difficulties | 13 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | NO ASSOCIATION in analyses. |
| Barnow et al. (2013) | n=286; 55% female; % Caucasian NR |
Community: Population (Greifswald) | 5 yrs (88%) | Maternal BPD & Depression | 15 | BPD sxs (SCID-II) | 20 | Maternal BPD predicted BPD sxs. (Maternal BPD and depression significant in bivariate analyses) |
| Belskey et al. (2012) | n=1116; 55% female; % Caucasian NR |
Community: Population (E-Risk) | 7 yrs (96%) | Family hx Psychiatric Hospitalization | 12 | BPD features (SWAP) | 12 | Family hx interacted with maltreatment & maternal negative expressed emotion to predict BPD dimensionally & categorically. |
| Stepp et al. (2013) | n=816; 59% female; % Caucasian NR |
Community: Population (OADP) | 16 yrs (87%) | Maternal/Paternal Depression, Anxiety, BPD, ASPD, Substance Use | 24 | BPD sxs (IPDE) | 30 | Maternal BPD and paternal substance use predicted BPD sxs. (Maternal depression & BPD and maternal & paternal anxiety, substance use and ASPD significant in bivariate analyses) |
| Reinelt et al. (2014) | n=295; 55% female; % Caucasian NR |
Community: Population (Greifswald) | 5 yrs (77%) | Maternal BPD sxs | 15 | BPD sxs (SCID-II) | 19 | Maternal BPD sxs predict offspring BPD sxs and this association was mediated by maladaptive parenting style/behavior. |
| Stepp et al. (2014b) | n=2212; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | Caregiver ASPD & Depression | 11 | BPD sxs (IPDE) | 14–17 | NO ASSOCIATION in final analyses. (Caregiver ASPD and depression significant in bivariate analyses) |
| Conway et al. (2015) | n=700; 52% female; 92% Caucasian |
Community: High Risk (Mater-U) | 5 yrs (86%) | Maternal Internalizing & Externalizing | 15 | BPD sxs (SCID-II) | 20 | Maternal externalizing dx predicted BPD sxs. |
| Maternal BPD sxs | 15 | NO ASSOCIATION in analyses. | ||||||
| Winsper et al. (2015) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Maternal Alcohol/Tobacco Use, Anxiety & Depression | PREG: 18, 32 wks | BPD sxs (CI-BPD) | 12 | Prenatal maternal anxiety and depression at 18wks predicted BPD sxs. (All prenatal risks were significant in bivariate analyses) |
|
| ||||||||
|
Parenting Behavior/Style
| ||||||||
| Bezirganian et al, (1993) | n=776; 48% female; 90% Caucasian |
Community: Population | 3 yrs (79%) | Involvement, Inconsistency, Punishment | 14 | BPD dx (SCID) | 16 | Maternal inconsistency predicted BPD dx and interacted with maternal over-involvement to predict BPD dx. |
| Involvement & Discipline | 14 | NO ASSOCIATION in analyses. | ||||||
| Johnson et al. (2006) | n=593; % female NR; 90% Caucasian |
Community: Population (CIC) | ~28yrs (61%) | Aversive Behaviors & Low Affection | 16 | BPD dx (DISC; PDQ; SCID-II) | 22, 33 | NO ASSOCIATION in final analyses. (Parenting behaviors significant in bivariate analyses) |
| Cohen et al. (2008) | n=680; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (70%) | Poor Parenting | 13, 16 | BPD sxs (NR) | 13, 16, 22, 33 | Poor maternal parenting predicted higher BPD sxs. |
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Hostility & Boundary Dissolution | 42 mos | BPD sxs (SCID-II) | 28 | Maternal hostility in early childhood uniquely predicted BPD sxs. |
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Maternal Child Satisfaction | 13 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Maternal satisfaction with child predicted BPD sxs. |
| Inconsistency | 13 | NO ASSOCIATION in final analyses. (Inconsistency significant in bivariate analyses) | ||||||
| Belskey et al. (2012) | n=1116; 55% female; % Caucasian NR |
Community: Population (E-Risk) | 7 yrs (96%) | Negative Emotion | 5, 10 | BPD features (SWAP) | 12 | Maternal negative emotion predicted BPD dimensionally & categorically. |
| Winsper et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Poor Parenting: | birth-8 | BPD sxs (CI-BPD) | 12 | Poor parenting predicted BPD sxs. |
| Wolke et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Hostility, Harsh Discipline | 2–7 | BPD sxs (CI-BPD) | 12 | Maternal hostility and harsh punishment predicted BPD sxs. |
| Lynos-Ruth et al. (2013) | n=56; 41% female; 73% Caucasian |
Community: High-Risk | 21 yrs (74%) | Disrupted Communication | 18 mos | BPD sxs (SCID-II) | 19 | Communication withdrawal predicted BPD sxs. |
| Reinelt et al. (2014) | n=295; 55% female; % Caucasian NR |
Community: Population (Greifswald) | 5 yrs (77%) | Rejection, Warmth, Overprotection | 15 | BPD sxs (SCID-II) | 19 | Maladaptive parenting (latent factor including both parenting constructs) predicted BPD sxs. |
| Mother-Child Discrepancies | 15 | |||||||
| Stepp et al. (2014b) | n=2212; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | Harsh Punishment, Low Warmth | 14–17 | BPD sxs (IPDE) | 14–17 | Significant reciprocal relationships between harsh discipline/low warmth and BPD sxs. |
| Hallquist et al. (2015) | n=2228; 100% female; 39% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | Harsh Discipline | 5–14 | BPD sxs (IPDE) | 14–17 | Harsh discipline predicted BPD sxs at 14. NO ASSOCIATION with change in BPD sxs. |
|
| ||||||||
|
Family Climate & Parent-Child Relationship
| ||||||||
| Bezirganian et al, (1993) | n=776; 48% female; 90% Caucasian |
Community: Population | 3 yrs (79%) | Parent-Child Closeness | 14 | BPD dx (SCID) | 16 | NO ASSOCIATION in analyses. |
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Parent-Child Relationship | 13 | BPD sxs (SCID-II) | 28 | NO ASSOCIATION in final analyses. (Parent-child relationship significant in bivariate analyses) |
| Stepp et al. (2013) | n=816; 59% female; % Caucasian NR |
Community: Population (OADP) | 16 yrs (87%) | Cohesion, Discord, Support | 17 | BPD sxs (IPDE) | 30 | Mother-child discord predicted BPD sxs. (M-C discord, family cohesion and maternal support significant in bivariate analyses) |
| Greenfield et al. (2015) | n=204; 69% female; 70% Caucasian |
Clinical: Inpt | 4 yrs (71%) | Family Relations | 15 | BPD dx (Ab-DIB) | 18 | NO ASSOCIATION in analyses. |
| Hammen et al. (2015) | n=385; 61% female; 92% Caucasian |
Community: High Risk (Mater-U) | 5 yrs (47%) | Relationship Quality | 15 | BPD sxs (SCID-II) | 20 | NO ASSOCIATION with relationship quality. |
| GxE Interaction (OXTR) × (Relationship Quality) | Relationship quality & OXTR genotype interacted to predict BPD sxs: relationship quality predicted BPD sxs for those with AA/AG genotype, not GG genotype. | |||||||
Note. ABC=Antisocial Behavioral Checklist, Ab-DIB=Abbreviated Diagnostic Interview for Borderlines, ALSPAC=Avon Longitudinal Study of Parents and Children, ASPD=antisocial personality disorder, BPD=borderline personality disorder, CI-BPD=Childhood Interview for Diagnostic and Statistical Manual BPD, CIC=Children in the Community, CIC-SR=Children in the Community Self-Report Scale, dx=diagnosis, E-Risk=Environmental Risk Twin Study, FES=Family Environment Scale, GxE=Gene X Environment Interaction, hx=history, Inpt=inpatient, IPDE=International Personality Disorder Examination-Borderline Screener, Mater-U=Mater-University Study, NR=not reported, OADP=Oregon Adolescent Depression Project, OXTR=oxytocin receptor gene, PD=personality disorder, PGS = Pittsburgh Girls Study, PREG=during pregnancy, SCID=Structured Clinical Interview for DSM Axis I Disorders, SCID-II=Structured Clinical Interview for DSM Axis II Disorders, SCID-NP=Structured Clinical Interview for DSM-Nonpatient Version, SCID-Q=Self-Report Personality Disorder Questionnaire, SWAP=The Shelder-Westen Assessment Procedure, sxs=symptoms, wks=weeks, yrs = years.
Parent/Family psychopathology
Ten studies assessed family psychopathology as a risk factor, with seven studies reporting significant positive associations. Six of these studies focused on maternal (or caregiver) psychopathology and found significant associations with offspring BPD. These risk factors included maternal internalizing (Stepp et al., 2014b; Winsper, Wolke, & Lereya, 2015) and externalizing (Conway et al., 2015; Stepp et al., 2014b) disorders as well as maternal BPD (Barnow, Aldinger, Arens, & Ulrich, 2013; Reinelt et al., 2014; Stepp et al., 2014b). Furthermore, Reinelt and colleagues (2014) found an indirect effect of maternal BPD symptoms on offspring BPD symptoms via maladaptive parenting behaviors. Stepp and colleagues (2013) also found that paternal substance use predicted offspring BPD symptoms. Lastly, Belskey and colleagues (2012) found family history of psychiatric hospitalization interacted with maltreatment and maternal negative emotion to predict BPD characteristics.
Three studies examined other maternal characteristics, including maternal ego integration, impulsivity, interpersonal difficulties, and history of serious medical problems (Bezirganian, Cohen, & Brook, 1993; Carlson et al., 2009; Crawford et al., 2009). There were no associations between these maternal factors and later BPD.
Parenting behavior/style
Twelve studies examined risk factors in this subdomain, with the majority focusing on affective parenting dimensions. Results provided consistent evidence for prospective associations between higher BPD symptoms and affective dimensions, such as low warmth, rejection, and low maternal satisfaction with the child (Crawford et al., 2009; Reinelt et al., 2014; Stepp et al., 2014b) as well as hostility and harsh discipline/punishment (Hallquist, Hipwell, & Stepp, 2015; Stepp et al., 2014b; Winsper et al., 2012; Wolke, Schreier, Zanarini, & Winsper, 2012). Moreover, Stepp and colleagues (2014b) found evidence of reciprocal associations between low warmth, harsh punishment, and BPD symptoms across adolescence, such that low warmth and harsh punishment predicted subsequent increases in BPD symptoms; in turn, BPD symptoms predicted subsequent increases in parental levels of low warmth and harsh punishment. While two studies failed to find predictive associations with low affection and harsh discipline (Bezirganian et al., 1993; Johnson, Cohen, Chen, Kasen, & Brook, 2006), it is noteworthy that these were two of the only studies that predicted onset of BPD rather than greater mean levels or increases in BPD symptoms.
Those studies examining affective parenting dimensions as they unfold in moment-to-moment observational paradigms found similar results. Specifically, Lyons-Ruth and colleagues (2013) showed disrupted maternal communication at 18 months to predict BPD symptoms at age 18, and Carlson and colleagues (2009) found maternal hostility at 42 months to predict BPD symptoms at age 28. Similarly, Belskey and colleagues (2012) found that maternal expressed negative emotion in middle childhood significantly predicted BPD features at age 12.
Two additional studies examined the influence of behavioral control dimensions of parenting, though findings were somewhat mixed. Bezirganian and colleagues (1993) found a significant interaction between maternal inconsistency and over-involvement at age 14, such that higher levels of both predicted BPD diagnosis at age 16. Conversely, Crawford and colleagues (2009) failed to find an association between inconsistent parenting and BPD symptoms. One final study found a significant association between poor parenting (i.e., both affective and behavioral dimensions) and BPD symptoms in adolescence and adulthood (Cohen et al., 2008).
Family climate and parent-child relationship
Only two of five studies found evidence supporting a prospective link between this sub-domain and subsequent BPD. Stepp and colleagues (2013) found that mother-child discord in adolescence predicted BPD symptoms at age 30 and Hammen and colleagues (2015) found that a broad index of family relationship quality predicted BPD symptoms for those with the OXTR risk genotype. However, the majority of studies did not find support for this risk factor (Bezirganian et al., 1993; Carlson et al., 2009; Greenfield et al., 2015). Overall, these studies used broad observational and self-report measures that may have obfuscated the dynamic, bidirectional nature of parent-child relationships.
Maltreatment and Other Trauma
Fifteen studies examined exposure to maltreatment and other trauma, including forms of child abuse (i.e., physical, sexual, emotional, or verbal abuse) and neglect (i.e., poor parental care, poor supervision, maternal separation); “other” traumatic experiences; and peer victimization (Table 3). Eight studies found fairly consistent evidence supporting abuse as a risk factor, including associations with physical abuse (Belsky et al., 2012; Bornovalova et al., 2013b; Carlson et al., 2009; Johnson, Cohen, Brown, Smailes, & Bernstein, 1999), verbal abuse (Johnson et al., 2001), emotional abuse (Bornovalova et al., 2013b), and sexual abuse (Bornovalova et al., 2013b; Carlson et al., 2009; Johnson et al., 1999; Stepp et al., 2015). Similarly, evidence consistently supported the link between BPD and neglect, defined broadly (Johnson et al., 1999), or by specific neglectful experiences: early maternal separation (Crawford et al., 2009), inadequate supervision (Johnson, Smailes, Cohen, Brown, & Bernstein, 2000) and poor parental care (Lyons-Ruth et al., 2013). Three of the five studies which examined maltreatment as a composite of types of abuse and neglect also provided support for increased risk for BPD outcomes (Carlson et al., 2009; Crawford et al., 2009; Johnson et al., 1999).
Table 3.
Summary of Longitudinal Research Investigating Maltreatment and Other Trauma Predicting Borderline Personality Disorder (BPD).
| Study | Sample | Risk factor | BPD Outcome | Summary of results | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristics | Type (Cohort) | Follow-up (Retention) | Construct (Measure) | Age in years | Construct (Measure) | Age in years | ||
| Johnson et al. (1999) | n=738; 48% female; 90% Caucasian |
Community: Population (CIC) | ~17yrs (79%) | Maltreatment: PA, SA, NEG | <10 | BPD sxs & dx (CIC-SR) | 22 | Maltreatment composite predicted BPD dx and PA, SA and NEG predicted BPD sxs. |
| Johnson et al. (2000) | n=738; 48% female; 90% Caucasian |
Community: Population (CIC) | ~17yrs (79%) | NEG: Emotional, Physical, Supervision | <18 | BPD sxs & dx (CIC-SR) | 22 | Supervision NEG predicted BPD sxs. (All forms of NEG significant in bivariate analyses) |
| Johnson et al. (2001) | n=793; 49% female; 90% Caucasian |
Community: Population (CIC) | ~17yrs (81%) | VA | 5, 13 16 | BPD sxs & dx (CIC-SR) | 22 | VA predicted BPD sxs & BPD dx. |
| Thatcher et al. (2005) | n=524; 44% female; 85% Caucasian |
Clinical: Inpt, Outpt, Incarcerated (PAARC) & CC | 8–12 yrs (NR) | PA or SA | <12 | BPD sxs (SCID-II) | 18+ | NO ASSOCIATION in analyses. |
| Cohen et al. (2008) | n=680; % female NR; 91% Caucasian |
Community: Population (CIC) | ~30 yrs (87%) | PA, SA, NEG & Other Trauma | 13, 16, 22 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Cumulative trauma (maltreatment & other trauma) predicted BPD sxs. |
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Maltreatment: PA, VA, NEG | birth-18 mos | BPD sxs (SCID-II) | 28 | Maltreatment predicted BPD sxs. |
| PA, SA or NEG | 4 -18 | PA and SA predicted BPD sxs. | ||||||
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Maternal Separation | <5 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Maternal separation predicted BPD sxs in adolescence and adulthood. |
| Maltreatment: PA, SA, NEG | NR | Maltreatment predicted BPD sxs. | ||||||
| Widom et al. (2009) | n=892; 49% female; 90% Caucasian |
Community: High-Risk & CC | ~ 10 yrs (75%) | Maltreatment: PA, SA, NEG | <11 | BPD dx (DIPD-R) | 29, 40 | NO ASSOCIATION in final analysis. (Maltreatment significant in bivariate analyses for sxs and dx (OR: 1.65 )) |
| Belskey et al. (2012) | n=1116; 55% female; % Caucasian NR |
Community: Population (E-Risk) | 7 yrs (96%) | PA | 5, 7, 10 | BPD features (SWAP) | 12 | PA predicted BPD dimensionally & categorically. |
| Wolke et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Peer Victimization | 8, 10 | BPD dx (CI-BPD) | 12 | Peer victimization was predictive of BPD dx: chronic victimization robust effects. |
| SA | 2–9 | NO ASSOCIATION in analyses. | ||||||
| Lynos-Ruth et al. (2013) | n=56; 41% female; 73% Caucasian |
Community: High-Risk | 21 yrs (74%) | Poor Parental Care | birth - 18 mos | BPD sxs (SCID-II) | 19 | Poor parental care predicted BPD sxs. |
| Bornovalova et al. (2013b) | n=2764; 55% female; 95% Caucasian |
Community: Population (MTS) | 7–13 yrs (NR) | PA, SA, or EA | 11, 17 | BPD sxs (MBPD) | 24 | PA, SA, & EA predicted BPD sxs: this was mediated by internalizing & externalizing sxs. |
| Greenfield et al. (2015) | n=204; 69% female; 70% Caucasian |
Clinical: Inpt | 4 yrs (71%) | Maltreatment: PA, SA, NEG | 15 | BPD dx (Ab-DIB) | 18 | No ASSOCIATION in final analyses. (Maltreatment significant in bivariate analysis) |
| Krabbendam et al. (2015) | n=184; 100% female; 64% Caucasian |
Clinical: Incarcerated | 3–6 yrs (55%) | PA, SA & Other Trauma | 16 | BPD dx (SCID-II) | 20 | NO ASSOCIATION in analyses. |
| Stepp et al. (2015) | n=113; 100% female; 33% Caucasian |
Community: High-Risk (PGS) | 10–13 yrs (97%) | SA | 12–16 | BPD sxs (IPDE) | 16–18 | SA predicted increases in BPD sxs over time. |
Note. Ab-DIB=Abbreviated Diagnostic Interview for Borderlines, ALSPAC=Avon Longitudinal Study of Parents and Children, BPD=borderline personality disorder, CC=community controls, CI-BPD=Childhood Interview for DSM Borderline Personality Disorder, CIC=Children in the Community, DIPD-R=Diagnostic Interview for Personality Disorders- Revised, dx=diagnosis, EA= Emotional abuse, E-Risk=Environmental Risk Twin Study, Inpt=inpatient, IPDE=International Personality Disorders Examination-Borderline Screener, mos=months, MBPD=Minnesota Borderline Personality Disorder Scale, MTS=Minnesota Twin Study, NEG=neglect, NR=not reported, Outpt=Outpatient, PA=physical abuse, PAARC= Pittsburgh Adolescent Research Center, PD=personality disorder, PGS=Pittsburgh Girls Study, SA=sexual abuse, SCID-II= Structured Clinical Interview for DSM-Axis II Disorders, SWAP=The Shelder-Westen Assessment Procedure, sxs=symptoms, VA=verbal abuse, yrs = years.
Five studies failed to find an association between abuse or neglect and later BPD: physical and sexual abuse (Thatcher, Cornelius, & Clark, 2005; Wolke et al., 2012), neglect (Carlson et al., 2009), and combined indices of maltreatment (Greenfield et al., 2015; Widom, Czaja, & Paris, 2009). Additionally, two studies that combined indices of maltreatment and other trauma had discrepant findings. Cohen and colleagues (2008) examined “cumulative trauma” (e.g., parent arrest or imprisonment, family suicide, death of a parent), and found a significant association with BPD across adolescence and early adulthood. Conversely, Krabbendam and colleagues (2015) did not find their combined index (i.e., physical or sexual abuse and “other” trauma, e.g., car accident) to predict BPD symptoms in an incarcerated sample of adolescents.
One final study examined exposure to maltreatment and trauma in the form of peer victimization in late childhood (Wolke et al., 2012). Findings demonstrated that both the severity and chronicity of bullying was prospectively associated with BPD symptoms at age 12.
Child Factors
Child factors were examined in 29 studies (Table 4), and eight assessed multiple factors.
Table 4.
Summary of Longitudinal Research Investigating Child Factors Predicting Borderline Personality Disorder (BPD).
| Study | Sample | Risk factor | BPD Outcome | Summary of results | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristics | Type Cohort) |
Follow-up (Retention) |
Construct (Measure) |
Age in years |
Construct (Measure) |
Age in years |
||
|
Cognitive function
| ||||||||
| Cohen et al. (2008) | n=680; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (70%) | IQ | 13, 16 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Lower IQ predicted BPD sxs. |
| Belskey et al. (2012) | n=1116; 55% female; %Caucasian NR |
Community: Population (E-Risk) | 7 yrs (96%) | IQ | 5 | BPD (SWAP) | 12 | Lower IQ predicted higher BPD dimensionally & categorically. |
| Executive Fx | 5 | NO ASSOCIATION in analyses. | ||||||
| Theory of Mind | 5 | Poor Theory of Mind predicted BPD dimensionally & categorically. | ||||||
| Winsper et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | IQ | 8 | BPD sxs (CI-BPD) | 12 | Lower IQ predicted BPD sxs. |
| Wolke et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | IQ | 8 | BPD dx (CI-BPD) | 12 | Lower IQ predicts BPD dx. |
|
| ||||||||
|
Attachment
| ||||||||
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Attachment | 12, 18 mos | BPD sxs (SCID-II) | 28 | NO ASSOCIATION in final analyses. (Disorganization significant in bivariate analyses, mediated by self-representation) |
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Attachment | 16 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Insecure attachment predicted BPD sxs. |
| Lynos-Ruth et al. (2013) | n=56; 41% female; 73% Caucasian |
Community: High-Risk | 21 yrs (74%) | Attachment | 18 mos | BPD sxs (SCID-II) | 19 | NO ASSOCIATION in analyses. |
| Disorganized/Controlling | 8 | Disorganized/controlling behavior predicted BPD sxs. | ||||||
|
| ||||||||
|
Temperament and Personality
| ||||||||
| Lenzenweger et al. (2005) | n=250; 53% female; 72% Caucasian |
Community: Population | 3 yrs (97%) | Agency, Negative Emotionality, Fear, Affiliation, Constraint | 19 | BPD sxs (IPDE) | 19–22 | Negative emotionality & agency and low fear & constraint predicted BPD sxs (age 19) & increases in BPD sxs. |
| BPD sxs (MCMI-II) | 19–22 | Negative emotionality and lower agency constraint predicted BPD sxs (age 19) & lower agency predicted increases in BPD | ||||||
| Tragesser et al. (2007) | n=350; 55% female; 84% Caucasian |
Community: High Risk | 2 yrs (86%) | Instability, Impulsivity/Self-Harm | 18 | BPD sxs (PAI-BOR) | 20 | Affective instability and impulsivity/self-harm predicted BPD sxs: affective instability most robust predictor. |
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Crying/Demanding; Angry/Tantrum | 5 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Anger/tantrums predicted BPD sxs. (All temperament measures significant in bivariate analyses) |
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Behavior During Feeding | 3 mos | BPD sxs (SCID-II) | 28 | NO ASSOCIATION in final analyses. (Muscle tone significant in bivariate analyses) |
| Temperament | 3, 6, 30 mos | NO ASSOCIATION in final analyses. (Infant activity at 6 mos & emotionality at 30 mos significant in bivariate analyses) | ||||||
| Behavioral, Emotional Attentional & Relational | 12 | NO ASSOCIATION in final analyses. (Behavioral and emotional instability and attentional and relational disturbance significant in bivariate analyses) | ||||||
| Functioning & Representation | 8–12 | Self-representation predicts BPD sxs. | ||||||
| Crawford et al. (2009) | n=766; % female NR; 91% Caucasian |
Community: Population (CIC) | ~20 yrs (78%) | Crying/Demanding; Angry/Tantrum | 5 | BPD sxs (CIC-SR) | 13, 16, 22, 33 | Anger/tantrums predicted BPD sxs. (All temperament measures significant in bivariate analyses) |
| Tragesser et al. (2010) | n=353; 55% female; 84% Caucasian |
Community: High Risk | 2 yrs (86%) | Negative Affect, Impulsivity | 18 | BPD sxs (DIB-R) | 20 | Negative affect and impulsivity predicted BPD sxs; negative affect was the most robust predictor. |
| Belskey et al. (2012) | n=1116; 55% female; % Caucasian NR |
Community: Population (E-Risk Twin Study) | 7 yrs (96%) | Self-control, Approach, Inhibition | 5 | BPD (SWAP) | 12 | Lower self-control predicted BPD dimensionally & categorically. |
| Impulsivity | 5 | Higher impulsivity predicted BPD dimensionally & categorically. | ||||||
| Jovev et al. (2013) | n=205; 51% female; 96% Caucasian |
Community: High-Risk | 3 yrs (84%) | Affect, Surgency, Affiliation, Control | 13 | BPD sxs (CIC-SR) | 15 | Effortful control predicted BPD sxs. Associations between affiliation and BPD sxs moderated were by maltreatment. |
| Stepp et al. (2014a) | n=2282; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 14 yrs (93%) | Emotionality, Activity, Sociability, Shyness | 5–8 | BPD sxs (IPDE) | 14–19 | Temperament predicted BPD sxs at age 14. Higher activity and lower sociability predicted increases in BPD sxs, higher shyness predicted decreases in BPD sxs. |
| Stepp et al. (2014b) | n=2212; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | Negative Affectivity; Impulsivity | 11, 14 | BPD sxs (IPDE) | 14–17 | Negative affectivity and impulsivity predicted BPD sxs at age 14. |
| Hallquist et al. (2015) | n=2228; 100% female; 60% Caucasian |
Community: High Risk (PGS) | 4 yrs (90%) | Negative Emotionality | 5–8, 11 | BPD sxs (IPDE) | 14–17 | Negative emotionality & poor self-control predicted BPD sxs at 14 and worsening self-control from predicted increases in BPD sxs. |
| Poor Self-Control | 5–8, 10–14 | The effects of poor self-control on age 14 BPD sxs was mediated by reciprocal effects between poor self-control and harsh discipline. | ||||||
| Sharp et al. (2015) | n=730; 56% female; 30% Caucasian |
Community: Population | 1 yr (83%) | Experiential Avoidance | 16 | BPD sxs (BPFS-C) | 17 | Experiential avoidance predicted BPD sxs. |
| Stepp et al. (2015) | n=113; 100% female; 33% Caucasian |
Community: High-Risk (PGS) | 10–13 yrs (97%) | Negative Affectivity | 16 | BPD sxs (IPDE) | 16–18 | The effect of negative affectivity on BPD sxs was moderated by family adversity: higher levels of both predicted BPD sxs. |
|
| ||||||||
|
Psychopathology
| ||||||||
| Thomsen et al. (1993) | n=96; 33% female; % Caucasian NR |
Clinical: Inpt, Outpt & Controls | 16 yrs (85%) | OCD | 12 | BPD dx (SCID-II) | 27 | NO ASSOCIATION in analyses. |
| Rey et al. (1995) | n=250; 44% female; % Caucasian NR |
Clinical: Inpt | 5–8 yrs (39%) | Internalizing & Externalizing | 14 | BPD dx (PDE) | 20 | Adolescent ADHD (either alone or with CD) predicted BPD dx. |
| Ramklint et al. (2003) | n=158; 60% female; % Caucasian NR |
Clinical: Inpt | 16 yrs (44% RR) | MDD, Disruptive Disorder, Substance Use | 14 | BPD dx (DIP-Q) | 31 | MDD and substance use disorder predicted adult BPD dx. |
| Thatcher et al. (2005) | n=524; 44% female; 85% Caucasian |
Clinical: Inpt, Outpt, Incarcerated (PAARC) | 8–12 yrs (NR) | Alcohol Dependence MDD, CD, ADHD | 14–17 | BPD sxs (SCID-II) | 18+ | MDD and ADHD predicted ‘severe’ BPD sxs as characterized by latent-class analysis after accounting for covariates. |
| Miller et al. (2008) | n=181; 12% female; 23% Caucasian |
Clinical: Outpt & CC | 10 yrs (NR) | ADHD, Internalizing & Externalizing | 9 | BPD dx (SCID-II) | 18 | Childhood ADHD predicted BPD. NO ASSOCIATION between persistent ADHD and BPD. |
| Belskey et al. (2012) | n=1116; 55% female; % Caucasian NR |
Community: Population (E-Risk) | 7 yrs (96%) | Internalizing & Externalizing | 5 | BPD (SWAP) | 12 | Internalizing & externalizing sxs predicted higher BPD dimensionally & categorically. |
| Burke et al. (2012) | n=142; 0% female; 70% Caucasian |
Clinical: Outpt (DTS) | 12–18 yrs (80%) | ODD, CD, ADHD, Depression, Anxiety | 7–22 | BPD sxs (SCID-II) | 24 | ODD (behavioral dimension) & ADHD sxs through adolescence predicted BPD sxs. |
| ASPD | 18, 19 | ASPD sxs predicted BPD sxs and accounted for association between ADHD and BPD. | ||||||
| Alcohol & Drug Use | 10–22 | NO ASSOCIATION in final analyses. (Marijuana use significant in bivariate analyses) | ||||||
| Stepp et al. (2012) | n=1233; 100% female; 42% Caucasian |
Community: High-Risk (PGS) | 6–9 yrs (94%) | ADHD, ODD | 5–13 | BPD sxs (IPDE) | 14 | ADHD and ODD sxs predicted BPD sxs. Growth in ADHD sxs (10–13yrs) and ODD sxs (8–10yrs) predicted BPD sxs. |
| Winsper et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Axis I dx | 8 | BPD sxs (CI-BPD) | 12 | NO ASSOCIATION in final analyses. |
| Wolke et al. (2012) | n=6050; 46% female; 48% Caucasian |
Community: Population (ALSPAC) | ~12 yrs (43%) | Axis I dx | 8 | BPD sxs (CI-BPD) | 12 | Any dx predicts BPD sxs. |
| Bornovalova et al. (2013a) | n=1280; 100% female; 96% Caucasian |
Community: Population (MTS) | 3–4 yrs (NR) | Substance Use | 14, 18 | BPD sxs (MBPD) | 14, 18 | NO ASSOCIATION in final analyses (Substance use significant in bivariate analyses) |
| Stepp et al. (2013) | n=816; 59% female; % Caucasian NR |
Community: Population (OADP) | 16 yrs (87%) | Depression, Anxiety, Suicidality, Substance Use, CD/ODD, ADHD | 16, 17 | BPD sxs (IPDE) | 30 | Depression, substance use and suicidality predicted BPD sxs. (All dx were significant in bivariate analyses) |
| Bornovalova et al. (2013a) | n=2764; 55% female; 95% Caucasian |
Community: Population (MTS) | 7–13yrs (NR) | Externalizing & Internalizing | 11, 17 | BPD sxs (MBPD) | 24 | Internalizing & externalizing sxs predicted BPD sxs. |
| Stepp et al. (2014b) | n=2212; 100% female; 41% Caucasian |
Community: High-Risk (PGS) | 4 yrs (90%) | CD/ODD sxs | 14 | BPD sxs (IPDE) | 14–17 | CD/ODD sxs predicted BPD sxs at age 14 and increases in BPD sxs. |
| Conway et al. (2015) | n=700; 52% female; 92% Caucasian |
Community: High Risk (Mater-U) | 5 yrs (86%) | Internalizing & Externalizing | 15 | BPD sxs (SCID-II) | 20 | Internalizing dx predicted BPD sxs. (Internalizing & externalizing dx significant in bivariate analyses) |
| Greenfield et al. (2015) | n=204; 69% female; 70% Caucasian |
Clinical: Inpt. | 4 yrs (71%) | Depression, Suicide, CD, Alcohol/Drug | 15 | BPD dx (Ab-DIB) | 18 | NO ASSOCIATION in analyses. |
| Age of Hospitalization & ER Visits | 15 | Older admission age for suicidality predicted BPD dx. (Admission age and prior hospitalizations significant in bivariate analyses) | ||||||
| Global Functioning | 15 | Global functioning predicted BPD dx. | ||||||
| Krabbendam et al. (2015) | n=184; 100% female; 64% Caucasian |
Clinical: Incarcerated | 3–6 yrs (55%) | PTSS Depression, Dissociation, & Externalizing | 16 | BPD dx (SCID-II) | 20 | Dissociation predicted BPD dx. (PTSS, depression & dissociation significant in bivariate analyses) |
| Sharp et al. (2015) | n=730; 56% female; 30% Caucasian |
Community: Population | 1 yr (83%) | Anxiety, Depression sxs | 16 | BPD sxs (BPFS-C) | 17 | Anxiety & depression predicted BPD sxs. |
|
| ||||||||
|
Other Infant Factors
| ||||||||
| Carlson et al. (2009) | n=162; 49% female; 67% Caucasian |
Community: High-Risk | 28 yrs (NR) | Behavior, Motor Fx | 7, 10 days | BPD sxs (SCID-II) | 28 | NO ASSOCIATION in analyses. |
| Infant Anomalies | birth | NO ASSOCIATION in analyses. | ||||||
Note. Ab-DIB=Abbreviated Diagnostic Interview for Borderline, ADHD=attention deficit hyperactivity disorder, ALSPAC=Avon Longitudinal Study of Parents and Children, APSD=antisocial personality disorder, BPD=borderline personality disorder, BPFS-C=Borderline Personality Disorder Features Scale for Children, CC=community controls, CD=conduct disorder, CI-BPD=Childhood Interview for DSM Borderline Personality Disorder, CIC=Children in the Community, DIB-R=Diagnostic Interview for Borderlines-Revised, DIP-Q=Diagnostic and Statistical Manual-IV and International Classification of Diseases-10 Personality Questionnaire, DIS=Diagnostic Interview Schedule, DISC=Diagnostic Interview Schedule for Children, DTS=Developmental Trends Study, dx=diagnosis, E-Risk=environmental risk, fx=functioning, HR=hospital record Inpt=inpatient, INT=interview, INT-ASST=interviewer-assisted measure, IPDE=International Personality Disorder Examination, IPDE-BOR=International Personality Disorders Examination-Borderline Screener, IQ=intelligence quotient, MBPD=Minnesota Borderline Personality Disorder Scale, MCMI-II=Millon Clinical Multiaxial Inventory-II, MDD=major depressive disorder, mos=months, MTS=Minnesota Twin Study, NR=not reported, OBS=observation, OCD=obsessive-compulsive disorder, ODD=oppositional defiant disorder, Outpt=outpatient, PAARC=Pittsburgh Adolescent Research Center, PAI-BOR=Personality Assessment Inventory- Borderline Features scale, PDE=Personality Disorder Examination, PGS=Pittsburgh Girls Study, PTSS=post-traumatic stress symptoms, RR=response rate, SCID = Structured Clinical Interview for DSM Axis I Disorders, SCID-II=Structured Clinical Interview for DSM Axis II Disorders, SWAP=Shelder-Westen Assessment Procedure, sxs=symptoms, WM=working memory, yrs=year.
Cognitive function
Findings from four studies (three unique samples) supported low IQ, measured from age 5 through adolescence, as a risk factor in adolescence and adulthood (Belsky et al., 2012; Cohen et al., 2008; Winsper et al., 2012; Wolke et al., 2012).
Attachment
Findings were mixed from three studies examining insecure or disorganized attachment. Positive associations were noted when attachment was measured in late childhood and adolescence; disorganized/controlling behavior at age 8 predicted BPD symptoms at age 19 (Lyons-Ruth et al., 2013), and insecure attachment, assessed at age 16 via a questionnaire about peer relationships, predicted BPD across adolescence and adulthood (Crawford et al., 2009). However, attachment disorganization and security, assessed in infancy and toddlerhood, was not associated with BPD symptoms in adulthood (Carlson et al., 2009; Lyons-Ruth et al., 2013).
Temperament/Personality
All 12 studies examining temperament or personality factors demonstrated positive associations with later BPD. Consistent links between negative affectivity (e.g., emotionality, affective instability, angry/tantrums), impulsivity (e.g., low constraint, low self-control, effortful control) and BPD symptoms in adolescence and adulthood were demonstrated (Belsky et al., 2012; Carlson et al., 2009; Crawford et al., 2009; Hallquist et al., 2015; Jovev et al., 2013; Lenzenweger & Desantis Castro, 2005; Stepp et al., 2015; Stepp, Keenan, Hipwell, & Krueger, 2014a; Stepp et al., 2014b; Tragesser et al., 2010; Tragesser, Solhan, Schwartz-Mette, & Trull, 2007). In an examination of more complex processes, Hallquist and colleagues (2015) found poor self-control predicted BPD symptoms via reciprocal effects between poor self-control and parental harsh discipline. Using the same sample, Stepp and colleagues (2015) showed an interaction between negative affectivity and family adversity, such that higher levels of both predicted the highest levels of BPD symptoms across adolescence.
Sharp and colleagues (2015) found that a higher level of experiential avoidance (e.g., tendency to avoid unpleasant thoughts, emotions) was associated with an increase in BPD features over 1 year. Additionally, Carlson and colleagues (2009) demonstrated that disturbances in self-representation (rated from narrative projective tests) predicted BPD symptoms at age 28.
Psychopathology
Sixteen of the 19 studies examining psychopathology as a predictor of later BPD detected at least one significant prospective relationship. In studies examining internalizing psychopathology (i.e., anxiety, depression, dissociation, suicide), consistent links with subsequent BPD were reported (Belsky et al., 2012; Bornovalova et al., 2013b; Conway et al., 2015; Krabbendam et al., 2015; Ramklint, Knorring, Knorring, & Ekselius, 2003; Sharp et al., 2015; Stepp et al., 2013; Thatcher et al., 2005; Widom et al., 2009). Though three studies did not find any evidence of a prospective association between internalizing disorders and BPD (Burke & Stepp, 2012; Miller et al., 2008; Rey, Morris-Yates, Singh, Andrews, & Stewart, 1995), it is notable that these studies utilized clinical samples that were mostly male.
Studies of externalizing psychopathology (i.e., attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, substance use) produced consistent associations with BPD outcomes (Belsky et al., 2012; Bornovalova et al., 2013b; Bornovalova, Hicks, Iacono, & McGue, 2013a; Burke & Stepp, 2012; Conway et al., 2015; Miller et al., 2008; Ramklint et al., 2003; Rey et al., 1995; Stepp et al., 2013; Stepp, Burke, Hipwell, & Loeber, 2012; Stepp et al., 2014b; Thatcher et al., 2005). The only study that did not detect a prospective relationship between externalizing disorders and BPD was in an incarcerated sample of adolescents, with high rates of behavioral and emotional problems at baseline (Krabbendam et al., 2015).
Two studies that failed to find any relationship between psychopathology and BPD were conducted in clinical samples. Thomsen and Mikkelsen (1993) did not find an association between obsessive-compulsive disorder and BPD diagnosis using an inpatient sample. Similarly, in sample of adolescents recruited from a psychiatric hospital, internalizing and externalizing disorders failed to predict BPD diagnosis (Greenfield et al., 2015). Finally, Winsper and colleagues (2012) did not find a relationship between DSM-IV Axis I disorders at 8 years and BPD symptoms at age 12. However, using the same community sample, Wolke and colleagues (2012) reported bivariate associations between any childhood disorder and BPD symptoms.
Other infant factors
Carlson and colleagues (2009) examined two additional infant characteristics as BPD risk factors (i.e., infant anomalies at birth and overall “non-optimal” functioning) and neither factor was significantly associated with BPD symptoms in adulthood.
Discussion
Results clearly supported multiple factors across social, family, maltreatment, and child domains that increase risk for subsequent BPD outcomes. The most robust risk indicators were low SES, stressful life events, and family adversity in the social domain; maternal psychopathology and affective parenting dimension (low warmth, hostility, harsh punishment) in the family domain; exposure to physical or sexual abuse or neglect in the maltreatment domain; and low IQ, high levels of negative affectivity and impulsivity, and internalizing and externalizing psychopathology, in the child domain. In and of itself the very existence of research capable of examining the development of BPD signals progress in the field, and the plethora of longitudinal studies conducted in both community (e.g., Children in the Community, CIC; Pittsburgh Girls Study, PGS) and clinical samples is remarkable. Taken together, this body of research has improved our understanding of early risk factors of BPD and further strengthened the construct validity of the disorder in adolescence and adulthood (Chanen, 2015).
At the same time, the most striking limitation of this research is its lack of specificity. Previous research demonstrates a nearly identical risk profile for a broad range of internalizing (Hankin, 2006; Murray, Creswell, & Cooper, 2009; Sander & McCarty, 2005) and externalizing (Deater-Deckard, Dodge, Bates, & Pettit, 1998; Shaw, Owens, Vondra, Keenan, & Winslow, 1996) disorders. Consequently, we can conclude that there is a shared set of risk factors that predict poor mental health outcomes (World Health Organization, 2012) and thus, at some level, these factors operate in a similar fashion across many psychiatric disorders. This highlights the concept of multifinality (Cicchetti & Rogosch, 1996), suggesting that we are missing critical elements required to explain divergent trajectories for unique disorder outcomes. Additionally, there was tremendous heterogeneity across several critical study features, including approaches to sample and assessment methodology, and the developmental timing of these assessments. The current systematic review provides an ideal opportunity to weigh the strengths and limitations inherent across study designs as we develop a roadmap for future research endeavors.
Effects of Sampling Methodology
First and foremost, it is imperative to highlight that while 39 studies met our inclusion criteria, only 24 unique samples are represented. For example, almost half of studies demonstrating a positive link between maltreatment and BPD were conducted in the same sample (i.e., 5 of 11 studies used the CIC cohort: Johnson et al., 1999, 2000, 2001; Cohen et al., 2008; Crawford et al., 2009). Similarly, a third of those studies reporting a positive association between temperament and later BPD utilized the PGS (Hallquist et al., 2015; Stepp et al., 2014a; 2014b; 2015). While this does not necessarily negate these findings, it highlights a potential bias in our interpretation of the strength and consistency of effects. Moving forward, it is critical that we attend to the reproducibility of findings across unique samples as opposed to merely counting the sheer number of studies demonstrating significance.
In addition, the consideration of sample ascertainment methods, with regard to interpretation of the current literature and future study design, is imperative as this provides the foundational parameters for the questions we are able to be address. For example, the current review highlights a pattern whereby studies with clinical samples or matched community controls (CC) appeared less likely to detect significant prospective associations between certain risk factors and BPD. Those studies reporting null findings with regard to child psychopathology utilized samples selected on the presence of clinically significant levels of psychopathology (Thomsen et al., 1993; Greenfield et al., 2015). Similarly, maltreatment and trauma were not supported as risk factors of BPD in studies selecting participants based on exposure to maltreatment or incarceration status (Widom et al., 2009; Krabbendam et al., 2015). This can likely be attributed to the sampling of extreme groups based on the very risk factor of interest, which precludes examination of the full range of variability. However, since clinical studies are characterized by high levels of clinical severity and are more likely to capture onset of the fully developed illness, they are ideal to examine onset. Moving forward, it is important to consider the strengths and limitations of the study design and critically evaluate its ability to uncover the mechanisms that explain the eventual manifestation of BPD.
Effect of Assessment Methodology
Measurement precision is essential as imprecise measurement leads to faulty or incomplete data that can yield flawed conclusions (Rose & Fischer, 2011). Consider two studies examining seemingly similar constructs, family relations (Greenfield et al., 2015) and family relationship quality (Hammen et al., 2015); note their drastically different operationalization: a single “overall measure of intra-family stresses” versus “a multi-method, multi-informant index…of ongoing marital and parental relationship quality,” respectively. It is highly likely that these studies are suffering from the jingle fallacy, as they are utilizing common terms to reference different underlying constructs (Thorndike, 1904). Relatedly, the current literature lacked consistency in the measurement of risk factors, including use of informants (parent, child, official documentation), and assessment method (questionnaire, interview, observation). The notable exception was in the domain of child temperament and was the one area in which all identified studies demonstrated complete consistency in their findings. Finally, there was considerable heterogeneity in the measurement of BPD. Specifically, several studies utilized aggregated post-hoc measures of BPD (i.e., CIC) for which the clinical utility is currently unknown. Moreover, it is imperative that we consider the developmental sensitivity of current measures developed for adults being used during adolescence.
In addition to improving data collection methods, we can also strive to improve our statistical approach to understanding the complex nature of risk processes. Research to date has generally examined risk factors as static, unidirectional influences on subsequent BPD. However, a minority of studies reviewed here sought to uncover more nuanced risk processes and found evidence of moderating (Belskey et al., 2012; Bezirganian et al., 1993; Hammen et al., 2015; Jovev et al., 2013; Stepp et al., 2015) and mediating (Bornovalova et al., 2013b; Hallquist et al., 2015; Reinelt et al., 2014; Winsper et al., 2012) mechanisms. These findings highlight the dynamic, transactional progression of risk across development and caution against the use of statistical approaches that inherently reflect the notion that risk factors exist in a vacuum. Moving forward, we must be cognizant of the balance between the breadth and depth when assessing risk factors. The examination of one risk factor in isolation fails to adequately reflect the innate complexity of the development of BPD. Conversely, the inclusion of too many risk factors may obfuscate key prospective relationships. In sum, examining a parsimonious set of theory-driven risk factors can illuminate processes by which and through which BPD develops.
Effects of Developmental Timing
Though the current review highlighted a fairly similar risk profile regardless of the developmental stage at which risk factors and outcomes were assessed, it may be premature to conclude that this signifies insensitivity to the developmental timing of risk or the manifestation of BPD. An alternative explanation may be rooted in the protracted follow-up periods assessing risk at a single time point, which could obscure sensitive developmental periods. For instance, a null finding at a single time point does not necessarily reflect a lack of association during developmental periods outside the sampling frame. This is highlighted in discrepant findings regarding exposure to maternal hostility in early childhood (Carlson et al., 2009) versus adolescence (Johnson et al., 2006). On the other hand, a positive association does not necessarily signify a developmentally critical window. It is possible that the positive association is driven by (1) persistence or change in the risk factor that was not captured (2) that the onset of the BPD outcome could have occurred earlier. Both of these scenarios signal that we are missing the mark with the latter being arguably more vital to refining developmental theories of BPD.
Along these lines, the developmental timing of the disorder must also be considered. If our ultimate goal is to prevent BPD, we must prioritize the identification of risk factors and processes that predict onset (either of the disorder or of its symptoms). Given that onset is a distinct phase in the course of the illness and may be distinguished by its unique risk profile, it is crucial to discriminate onset from other phases (i.e., prodromal, maintenance, remission, recurrence). We appear to have completely ignored this developmental dimension and thus, have fallen victim to the jangle fallacy (Kelley, 1973): equating all BPD outcomes as synonymous regardless of phase variation. In fact, only one study reviewed here considered phase of the disorder as an outcome (Greenfield et al., 2015). As we shift our focus to capture the onset phase, we must also shift away from examining distal factors indicative of shared risk for general psychopathology and instead identify precursors (i.e., unique proximal indicators) that are specific BPD (Eaton, Badawi, & Melton, 1995). While this point is certainly applicable to the onset of both symptoms and disorder, it is most urgent to examine precursors of the acute, fully developed illness if our ultimate goal is to prevent BPD and deflect trajectories of chronic illness. Therefore, future studies should consider stage of the disorder in tandem with developmental timing, which requires (1) repeated assessments of BPD during developmentally sensitive windows that encompass periods of peak prevalence (i.e., adolescence; Miller, Muehlenkamp, & Jacobson, 2008); (2) ascertainment of a sample with a heightened proclivity to onset during the sampling frame; and (3) the retrospective identification of a prodromal phase to determine the most robust set of precursors (Eaton et al., 1995).
In sum, the current state of the field provides little in the way of identifying who is most at risk and why BPD (versus some other psychiatric disorder) develops and many unanswered questions remain. Given the public health significance concerning the identification, prevention, and intervention of BPD, we have only a meager amount of research on its causes, developmental trajectory, and response to treatment. Although empirically supported treatments are available, very few psychiatric clinics provide this care, which could account for poor treatment outcomes and heightened use of emergency and inpatient services. In terms of refining developmental theories, what are the mechanisms that explain the etiology of BPD? If our goal is early detection, how do we select those at high risk for BPD? Once identified, how do we intervene with children and youth before they develop the full-blown disorder? Progress in answering these questions may come from addressing these gaps. We have highlighted several key avenues for future endeavors pursuing these research priorities in the hopes of encouraging research that will hasten the pace of these discoveries.
Supplementary Material
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health.
Footnotes
Notably, the number of participants was reduced to 18,238 when examining only the unique samples (n=24); the majority remained female (51%) and Caucasian (69%).
Clinical samples had lower retention rates compared to community samples, (clinical: M = 62%, SD = 13.5%; community: M = 79%, SD = 19.2%; F(1, 33) = 6.8, p = 0.008); other characteristics did not significantly vary by sample type. Retention rate was not significantly correlated with any other sample characteristic.
Studies examined community (Carlson et al. 2009; Cohen et al., 2008; Conway et al., 2015) versus clinical samples (i.e., Greenfield et al., 2015). It is also noteworthy that a sizeable portion of the clinical sample already met criteria for BPD at baseline, resulting in a small group of adolescents with emerging BPD between the baseline and follow-up period (n = 7; 3.43% of the sample).
Portions of this manuscript were presented at the International Society for the Study of Personality Disorders XIV Conference in Montreal, Quebec, Canada (October, 2015).
References
- Bagge C, Nickell A, Stepp SD, Durrett C, Jackson K, Trull TJ. Borderline personality disorder features predict negative outcomes 2 years later. Journal of Abnormal Psychology. 2004;113(2):279–288. doi: 10.1037/0021-843X.113.2.279. [DOI] [PubMed] [Google Scholar]
- Chanen AM. Borderline personality disorder in young people: Are we there yet? Journal of Clinical Psychology. 2015;71(8):778–791. doi: 10.1002/jclp.22205. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8(4):597–600. [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10(3):469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Badawi M, Melton B. Prodromes and precursors: epidemiologic data for primary prevention of disorders with slow onset. The American Journal of Psychiatry. 1995;152(7):967. doi: 10.1176/ajp.152.7.967. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Reliability and validity of borderline personality disorder in hospitalized adolescents. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2013;22(3):206–211. [PMC free article] [PubMed] [Google Scholar]
- Hankin BL. Adolescent depression: description, causes, and interventions. Epilepsy & Behavior: E&B. 2006;8(1):102–114. doi: 10.1016/j.yebeh.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Kelley TL. Interpretation of Educational Measurements. Oxford: World Book Co; 1973. [Google Scholar]
- Kongerslev MT, Chanen AM. Personality disorder in childhood and adolescence comes of age: A review of the current evidence and prospects for future research. Scandinavian Journal of Child and Adolescent Psychiatry and Psychology. 2015;3(1):31–48. [Google Scholar]
- Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Comprehensive Psychiatry. 2008;49(4):380–386. doi: 10.1016/j.comppsych.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet (London, England) 2004;364(9432):453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28(6):969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Murray L, Creswell C, Cooper PJ. The development of anxiety disorders in childhood: an integrative review. Psychological Medicine. 2009;39(9):1413–1423. doi: 10.1017/S0033291709005157. [DOI] [PubMed] [Google Scholar]
- Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry. 2001;42(6):482–487. doi: 10.1053/comp.2001.26271. [DOI] [PubMed] [Google Scholar]
- Gordon RSJ. An operational classification of disease prevention. Public Health Reports. 1983;98(2):107. [PMC free article] [PubMed] [Google Scholar]
- Rose LT, Fischer KW. Garbage in, garbage out: Having useful data is everything. Measurement: Interdisciplinary Research & Perspective. 2011;9(4):222–226. [Google Scholar]
- Sander JB, McCarty CA. Youth depression in the family context: Familial risk factors and models of treatment. Clinical Child and Family Psychology Review. 2005;8(3):203–219. doi: 10.1007/s10567-005-6666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. British Medical Journal. 2015;349:1–25. [Google Scholar]
- Shaw DS, Owens EB, Vondra JI, Keenan K, Winslow EB. Early risk factors and pathways in the development of early disruptive behavior problems. Development and Psychopathology. 1996;8(04):679–699. [Google Scholar]
- Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive–compulsive personality disorder over two years. Psychological Medicine. 2005;35(03):443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4: Software for research synthesis. London: EPPI-Centre Software; 2010. [Google Scholar]
- Thorndike EL. An Introduction to the Theory of Mental and Social Measurements. Oxford: Science Press; 1904. [Google Scholar]
- Widiger TA, Weissman MM. Epidemiology of borderline personality disorder. Hospital & Community Psychiatry. 1991;42(10):1015–1021. doi: 10.1176/ps.42.10.1015. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Risks to mental health: An overview of vulnerabilities and risk factors. Geneva: WHO; 2012. [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. The American Journal of Psychiatry. 2003;160(2):274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.