Abstract
Background
Telemedicine can facilitate delivery of thrombolysis in acute stroke. The aim of this qualitative study was to explore patients’ and carers’ views of their experiences of using a stroke telemedicine system in order to contribute to the development of reliable and acceptable telemedicine systems and training for health‐care staff.
Method
We recruited patients who had, and carers who were present at, recent telemedicine consultations for acute stroke in three hospitals in NW England. Semi‐structured interviews were conducted using an interview guide based on normalization process theory (NPT). Thematic analysis was undertaken.
Results
We conducted 24 interviews with 29 participants (16 patients; 13 carers). Eleven interviews pertained to ‘live’ telemedicine assessments (at the time of admission); nine had mock‐up telemedicine assessments (within 48 h of admission); four had both assessments. Using the NPT domains as a framework for analysis, factors relating to coherence (sense making) included people's knowledge and understanding of telemedicine. Cognitive participation (relational work) included interaction between staff and with patients and carers. Issues relating to collective action (operational work) included information exchange and support, and technical matters. Findings relating to reflexive monitoring (appraisal) included positive and negative impressions of the telemedicine process, and emotional reactions.
Conclusion
Although telemedicine was well accepted by many participants, its use added an additional layer of complexity to the acute stroke consultation. The ‘remote’ nature of the consultation posed challenges for some patients. These issues may be ameliorated by clear information for patients and carers, staff interpersonal skills, and teamworking.
Keywords: acute stroke, telemedicine, remote consultation, thrombolysis, patient satisfaction, carer satisfaction
Background
Stroke is a time‐dependent medical emergency in which rapid access to specialist care reduces death and dependency.1 Up to 26% of patients with acute stroke could potentially be treated with intravenous thrombolysis.2 Thrombolysis improves patients’ chances of regaining functional independence with minimal or no disability3 and is more effective if administered early after symptom onset within a maximum of 4.5 h.4 In addition, all patients with stroke benefit from early stroke‐specialist diagnosis and the implementation of a targeted management plan.5
Cost and staffing issues make it unfeasible for all acute stroke units in the UK to provide 24/7 cover for these unpredictable neurological emergencies, particularly outside large conurbations. Telemedicine (TM), the use of communication and information technologies in the provision of clinical care where patient and clinician are at different locations, may be a cost‐effective and sustainable way for staff to deliver a specialist service for low frequency but high‐impact events.6, 7, 8, 9 The introduction of TM ‘hub and spoke’ networks can increase the number of patients gaining timely assessment and thrombolysis, and several networks have been set up in the UK. These typically entail videoconsultation between the patient in the emergency department (ED), supported by an on‐site health professional, and an on‐call stroke‐specialist physician via a dedicated link. The on‐call specialist may be based on a central ‘hub’ location, or the hub may rotate between different locations. The on‐call specialist may also view the patient's CT head scan images via the link. The system removes the need for either patient or specialist to waste valuable time travelling to a different hospital site. It means that the patient, carer and health‐care team at the receiving hospital can access specialist advice within minutes of the patient's arrival in the ED.10
The introduction of new working practices and technology into health care is complex and can be challenging for staff. This is exacerbated for patients and carers, who lack familiarity with the health‐care setting and who have to engage with health‐care systems and technology whilst also experiencing a serious and potentially life‐changing illness episode, particularly in emergency care. Home internet access has now reached 80% of UK households, and teleconferencing and video calls are now used by 32% of the UK population for social or business purposes. However, 64% of older adults (>65 years) living alone do not have internet access, 89% of people over 65 years have never made a video call, and 43% of families in the lowest income decile do not have a home computer.11 The high incidence of stroke in older people and in socio‐economically deprived groups means that many patients with stroke and their carers are likely to be unfamiliar with videoconferencing technology.
The National Stroke Strategy12 recommends that people with stroke, and their carers, should be meaningfully involved in the planning, development, delivery and monitoring of services. A recent clinical guideline13 has highlighted the importance of patient‐based evidence in the design and delivery of high‐quality health care.14 Public perceptions of TM,15 and patients’ experiences of TM in other clinical settings such as dermatology,16 joint primary–secondary care consultations,17 elderly care18 and stroke rehabilitation,19 have all been previously studied, and the ethical implications of home telecare systems for older people have also been explored.20 However, there has been little exploration of patients’ and carers’ perspectives of TM for service provision in acute stroke.
The aim of this study was to explore patients’ and carers’ perceptions of TM in the assessment of acute stroke. The study formed part of a multiphase project: Acute Stroke Telemedicine: Utility, Training and Evaluation (ASTUTE). This project ran alongside the development and implementation of the Lancashire and Cumbria Telestroke Network which provides ‘out of hours’ specialist assessment, via TM, of patients with acute stroke who are potentially suitable for treatment with thrombolysis In the Telestroke Network, 15 NHS consultant stroke physicians from the eight participating acute hospitals across the region take part in an on‐call rota. The on‐call consultant can be contacted by staff on behalf of a patient admitted with suspected stroke to the Emergency Department at any participating hospital. The consultant then provides a teleconsultation and can view CT scan images via a secure internet link to the consultant's home. The patient receives direct clinical care from the admitting hospital's ED and stroke team. The on‐call consultant and patient do not have subsequent face‐to‐face contact unless the patient has been admitted to the consultant's own stroke unit.
Method
Design
Qualitative interview‐based study utilising normalization process theory (NPT) as a framework for analysis.
Sample/Participants
We recruited a convenience sample of patients admitted with suspected or confirmed stroke to three NHS hospitals in NW England, who had recently experienced a TM consultation, and/or carers who had been present at the time of the consultation. We recruited patients who had received a TM assessment as part of the standard ‘out of hours’ care pathway on admission to the ED (‘live’). We also interviewed some patients who had been admitted within normal working hours and had therefore had a face‐to‐face consultation, but who subsequently had a recorded mock‐up TM consultation (‘mock‐up’) within 48 h of their admission. The ‘mock‐up’ consultations were conducted and video‐recorded specifically for inclusion in a training package which was devised as part of the ASTUTE project. As far as was practicable, the ‘live’ and ‘mock‐up’ consultations followed the same process, but due to ethical approval restrictions, the ‘live’ consultations could not be video‐recorded. Some patients had both ‘live’ and ‘mock‐up’ consultations.
Eligibility criteria were as follows:
Patients: had suffered a suspected or confirmed stroke and been assessed via TM; aged 18 or over; able to provide informed consent, or assent provided by a relative or authorized carer; medically stable; able to understand and speak English.
Carers: had been present at all or part of a stroke TM consultation: aged 18 or over; able to provide informed consent; carer for a patient who was currently medically stable; able to understand and speak English.
Data collection
Data collection took place between 16 December 2011 and 21 August 2012. Interviews were conducted by a member of the research team who was not connected with the patient's clinical care. Participants were interviewed within 4 weeks of the TM consultation. Interviews were conducted at the patient's or carer's home, or in a quiet location at the hospital. Interviews were digitally audio‐recorded. A semi‐structured interview guide, with questions based on the domains of NPT,21 was used. NPT provides a toolkit to understand and explain the social processes through which new work practices are implemented, embedded and integrated in health‐care and other settings. It has been used in a number of studies, mainly in telecare and e‐health.22 NPT was used as an overall model to analyse the development and implementation of TM system in acute stroke from the differing perspectives of organizations, clinical staff and patients and carers.23 There has been little previous research which uses NPT to understand patients’ and carers’ views of new health‐care practices, and our study also explored the benefits and limitations of this method.
Ethical considerations
Ethical approval was obtained via the National Research Ethics Service and from the host institution. The ‘live’ TM consultations were carried out as part of standard out‐of‐hours practice in the ED. Patients and carers had received written and verbal information about the TM process during their clinical care and had provided verbal consent/assent at the time of the assessment, in line with standard clinical governance procedures. Those having ‘mock‐up’ recordings gave informed consent for the additional consultation and for the consultation to be video‐recorded. Informed consent or assent, as appropriate, was given for the interviews for all participants.
Data analysis
Interviews were digitally audio‐recorded, fully transcribed, anonymized and coded using ATLAS.ti software (ATLAS.ti Scientific Software Development GmbH. Berlin, Germany). Although the domains of NPT had been used in devising the semi‐structured interview schedule, it became apparent during early analysis that there was an imperfect fit between the interview content and the NPT domains. It was therefore agreed to undertake initial thematic analysis via open coding in order to develop codes which enabled a detailed interpretation of the data. These codes were then mapped onto the NPT domains.
Rigour
Coding was undertaken independently by two researchers, and discrepancies were resolved by discussion. The coding framework was modified to reflect emerging themes.
Findings
We undertook 24 interviews in total, with a mean duration of 19.27 min (range 5.59–57.01 min). Eleven interviews were conducted with the patient alone; eight were with a carer alone; five were with both patient and carer. There were therefore 29 participants who took part in interviews (16 of the 24 patients and 13 carers). Participation was based on patient and carer preference: several patients had little or no recall of the telemedicine process but were willing for a carer to participate instead; others wished to be interviewed with a carer. All carers had been present at the time of the telestroke consultation. Of the patients, 16 were male and eight were female, with a median age of 64 years (range 40–76), and there were eight female and five male carers. We did not record the ages of carers, but the majority (10/13) were patients’ spouses or siblings and could therefore be assumed to be of a similar age to the patient. Figure 1 further illustrates participant characteristics.
Figure 1.
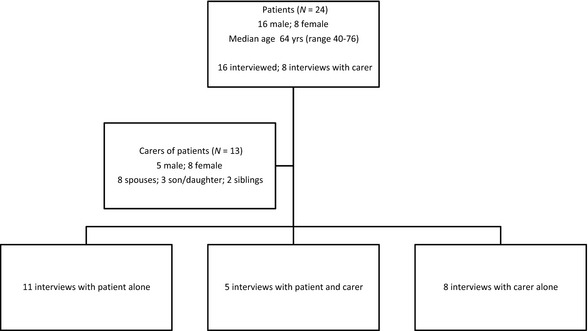
Flow diagram of participation in study and participant characteristics.
All 24 patients had a suspected stroke when admitted to the ED; 21 had a confirmed stroke at final diagnosis. Ten had received thrombolysis; none had significant post‐thrombolysis complications.
Fifteen patients had a telestroke assessment in the ED on admission to hospital (‘live’). Four of these patients also had a ‘mock‐up’ telestroke assessment within 48 h of their admission, either in the ED or on the stroke unit. A further nine patients had only a ‘mock‐up’ consultation. Staff followed the same assessment procedures in both ‘live’ and ‘mock‐up’ consultations, except that the ‘mock‐ups’ were recorded using the telestroke system for use in future research and training.
Initial thematic analysis via open coding produced 16 codes. These were then mapped onto the NPT domains and subdomains (Table 1). Representative quotations are given in Table 2.
Table 1.
Identified codes mapped onto NPT domains
1. Coherence (individual and collective sense‐making work)
|
2. Cognitive participation (relational work to build and sustain a new practice)
|
3. Collective action (Operational work to enact a new practice)
|
4. Reflexive monitoring (appraisal of how the practice has affected self and others)
|
Table 2.
Examples of quotes for each Normalization Process Theory domain
| Theme and relevant questions from interview schedule | Examples of participants’ responses |
|---|---|
| 1. Coherence (sense making) | |
|
1a. Prior experience of telemedicine ‘Had you had any experience of a consultation by telemedicine before’? ‘Did you know what telemedicine was or what to expect prior to this experience’? |
‘I hadn't heard of it beforehand’ (P8: ‘live’ and mock‐up, male patient, age 45)
‘I didn't know what it was’ (P22: ‘live’, patient's daughter) ‘I knew about it (from TV), I had never experienced it but I knew about it’ (P5: ‘live’ and mock‐up, patient's wife) |
|
1b. Understanding of reason ‘What can you remember about using the telemedicine system’? ‘What did you understand the system was for’? |
‘because it was weekend…and consultants have got to have some time off…when they get patients in that need checking and some urgent treatment, the consultant would link via this live thing so they could ask questions, view the patient and then they would come to a decision with the doctors who were already on site as to what treatment they could give’ (P3: ‘live’, patient's husband)
‘Everything was being shown to him (consultant) on the computer, probably where he was living, and all the scans and everything like that, and then he was making a diagnosis, and then they…thrombolysed’ (P10: ‘live’, male patient, age 53) ‘I was actually being used by possibly a computer model that was going to look for potential benefits in the future’ (P4: mock‐up, male patient, age 62) ‘I don't want to find out that it's to save money’ (p7: mock‐up, patient, age 69) |
|
1c. Telemedicine vs. other modalities ‘How would you describe it compared with a face to face consultation?’ |
‘well I think a face‐to‐face consultation is always preferable, but if that's not possible then that's not possible’ (P1: ‘live’, patient's son)
‘I think personal one to one, face to face with the doctors has got to be better…if there's any questions it must seem easier’ (P23: ‘live’, patient's brother) ‘he (doctor) couldn't have done any more I don't think, because he asked all the questions…he looked in his eyes and he checked his weight, he asked what height and everything… so if he'd have been there I don't think it could have been much different’ (P2: ‘live’, patient's wife) |
| 2. Cognitive participation | |
|
2a. Interaction between staff ‘Can you remember how many and what staff were involved in the consultation – who did what’? ‘Was there someone with you who took the lead in talking to the doctor on the screen?’ |
‘the (remote) doctor was asking what I could do at present, and the nurses were doing what he said’ (P12: mock up, male patient, age 68)
‘The two doctors’ discussion … that would (be heard by) the patient, so they (staff) would have to take that into account’ (P8: mock‐up, male patient, age 45) ‘They moved the bed a little bit more toward (the camera), and then he moved the screen…he just kept asking the (bedside) doctor to do things’ (p11: ‘live’, patient's sister) ‘He (remote assessor) said have you got a (stroke severity) score for me…do you agree with me that we can use this clot‐busting drug, and they said yes, we do agree’ (p3: ‘live’; patient's husband) |
|
2b. Patient and carer involvement ‘Did you feel involved’? ‘Did you have anyone with you? Were they involved? How did they feel about being involved or about the telemedicine itself’? ‘Were you/the people with you able to say what you/wanted and take enough time? Did anyone ask questions’? |
‘Involved, yeah I would say so because I was getting feedback directly off the consultant on the screen. He wasn't just saying yeah, I think this, he was actually telling me why, what was going on’ (p9; ‘live’; male patient, age 49)
‘We were kept in the picture the whole time, and especially when they made that final decision’ (p18; ‘live’ and mock‐up; patient's husband) ‘If that person says ‘now is there anything you want to ask’, you get the feeling because it's on the screen, you've only got a very limited amount of time, it'll go ‘click’, it's gone’ (p13; mock‐up; male patient, age 62) ‘(the patient) couldn't answer and he couldn't respond, but he understood… so it was a great help that he could be part of the decision…I asked him either to blink or press my hand…I felt he very much gave the consent to it as much as myself’ (p5; ‘live’ and mock up; patient's wife) |
|
2c. Staff presence ‘Can you remember how many and what staff were involved in the consultation’? |
‘There were plenty of other people around… that were looking at her and were very hands on with her’ (p3: ‘live’; patient's husband)
‘The nurse with me, I think she was a little bit out of practice or something, so she was a bit unsure’ (P8: mock‐up, male patient, age 45) ‘They (nurses) seemed very well informed and I couldn't complain at all’ (p24: ‘live’, patient's wife) ‘right the way through we felt there was somebody there with us, explaining what was happening’ (p24: ‘live’, patient's wife) |
|
2d. Privacy ‘How would you describe the consultation in terms of privacy’? |
‘they had screens round… no other visitors or no one else could see, there was only the people there that really you felt needed to be there’ (P11: ‘live’, patient's sister)
‘I don't think that (privacy) made any difference to me. At that particular time I was more bothered about getting whatever they were going to do, to get it, make sure that it was put right’ (P10: ‘live’, male patient, age 53) ‘[it was] just like a normal consultation in a cubicle’ (P9: ‘live’, male patient, age 49) |
|
2e. Recording ‘Was your consultation recorded’? ‘How did you/would you feel about that’? |
‘It was just ordinary, it wasn't like big cameras in your face, it was just one to one – that little camera on the top’ (p16: mock‐up, female patient, age 46 –recorded)
‘To be honest I just thought it was recorded. It wouldn't matter’ (p11: ‘live’, patient's sister – not recorded) ‘I would rather be consulted first…but I'd consent to it (recording), yes’ (p19: mock up; female patient, age 70) |
| 3. Collective action | |
|
3a. Information exchange pre/during consultation ‘What did the staff tell you about what would happen’? ‘Can you remember who it was that explained it to you, and what they said’? ‘Did they give you any leaflets or anything about it’? ‘Did you understand what was being asked of you/what would happen’? |
‘the nurses explained who it was when (consultant) came on, and why he was going to ask us all the questions’ (P24: ‘live’, patient's wife)
‘the doctor told me what they was going to do through the “Tele” thing to see this consultant’ (P6: ‘live’, male patient, age 71) (Interviewer: ‘Did anyone explain to you what was going to happen?’) Participant: ‘No, I was just wheeled to another bay, and there was this television with…probably a camera or something on the top, looked like a big torpedo, and they just wheeled it in front of me, then they told me that they was doing a link with this (consultant name) so that was the end of that’ (P14: ‘live’, male patient, age 64) |
|
3b. Technical and audio‐visual issues ‘Was the process easy’? ‘Could you see the consultant on screen? Was it clear/visible’? ‘Could you (and those with you) hear what was being said well enough’? ‘Were there any problems with the machine at the time, or did it all go smoothly’? ‘Did you feel that the staff were comfortable with using the telemedicine system’? |
‘Considering how noisy it is in A+E, you could still hear it all and you didn't have any problems’ (p11: ‘live’, patient's sister)
‘The machine wasn't working properly‐ the video link wasn't coming on – it came up but it wasn't properly working’ (p2: ‘live’; patient's wife) ‘I'd seen it before at my niece's when we were talking to her son in Australia, but whether it would affect people who have never used it before – and of course anybody your age (researcher), they're used to it aren't they’ (p24: ‘live’, patient's wife) ‘(To see myself on screen was) pretty weird really’ (p10: ‘live’, male patient, age 53) ‘I could see my big stomach (on the screen) and I was thinking, oh my God’ (p11: ‘live’, patient's sister) ‘They'd explained he'd be on the screen… I couldn't make his face out, but as soon as they got it set up it were brilliant’ (p6: ‘live’; male patient, age 71, partially sighted) |
|
3c. Support ‘Did it feel organised and clear what you were supposed to be doing’? ‘Did you feel supported throughout the process? By whom’? (consultant/on site staff) ‘Is there anything that could have been done differently that would have made you feel more informed/supported’? |
‘They were really good, they were supporting us all the time’ (p24: ‘live’, patient's wife)
‘Once I was introduced to the doctor, I didn't have a problem, I was alright talking to him’ (p9; ‘live’; male patient, age 49) ‘This Doctor (name), he was wonderful, he was so nice to us’ (p2: ‘live’; patient's wife) ‘The only person I would want next to my bed is somebody qualified to comment, to pass judgement on the problem I'm in hospital for’ (p7: mock‐up, patient, age 69) |
|
3d. Trust ‘Did you trust the system’? ‘Did you feel confident in the staff using the system’? ‘Did you feel comfortable talking to the screen’? |
‘they (staff) seemed confident in what they were doing’ (P17: mock‐up, male patient, age 72)
‘I would say nine out of ten at least I would trust them, yeah I mean it didn't cross my mind not to trust them’ (P13: mock‐up, male patient, age 62) ‘if I'm in that situation…I would hope that there will be some sort of qualified doctor that's got experience in that problem, that's the main thing’ (P7: Mock‐up, Male Patient, 69) |
| 4. Reflexive monitoring | |
|
4a. Process (positive/negative issues) ‘What do you think are the pros and cons of using a system like that?’ |
‘the speedy getting in touch with somebody who knows what they're doing… and the efficiency…it was absolutely amazing’ (p6: ‘live’; male patient, age 71)
‘All they could do was wait for the scan to be taken… he said we've got to wait for a porter, so it was a little bit frustrating’ (p22: ‘live’; patient's daughter) ‘I was surprised that within a couple of seconds of somebody speaking to me, I just talked back into the screen, automatically’ (p23: ‘live’; patient's brother) ‘He was at home and he was looking at my scans that I'd had done 10–15 minutes prior, it was quite amazing’ (p14: ‘live’; male patient, age 64) ‘They had one or two problems with the camera moving, they asked the (remote) doctor can you take control of this, and he said yes, he could operate it from his end’ (p14: ‘live’; male patient, age 64) |
|
4b. Emotional reaction ‘Can you tell me about your experience with the telemedicine system’? |
I felt all moithered (flustered/worried) but I think I was just grateful that he had the best care’ (p2: ‘live’; patient's wife)
‘(The mock‐up) was different because I wasn't under stress… it was very interesting, and of course I was in a completely different situation than the first time round’ (p5; ‘live’ and mock up; patient's wife) ‘it was slightly detached because you're not actually talking to somebody, but it wasn't a frightening experience, it was just unusual’ (p9; ‘live’; male patient, age 49) ‘I think face to face if there's any questions it must seem easier’ (p23: ‘live’; patient's brother) |
|
4c. Impression of TM ‘Do you think the telemedicine process helped in terms of your diagnosis and treatment’? ‘Did you like having a consultation this way? Would you use it again’? ‘Do you have any reservations about this way of working in health care’? ‘Can you think of anything that could be improved? What would you suggest could be done to improve it’? |
‘I think it's brilliant…it feels like they're in the room’ (P16: mock‐up, female patient, age 46)
‘the way that you use it was easy and simple’ (P9: ‘live’, male patient, age 49) ‘I would have thought that an older person could be quite reticent to talk to what she considers to be an inanimate body’ (P13: mock‐up, male patient, age 62) ‘It'd be alright for a mild stroke but I don't know how you'd go on if it was something serious’ (P20: ‘live’ and mock‐up, male patient, age 74) |
|
4d. Other telemedicine uses ‘Would you recommend telemedicine to others in a similar situation’? ‘Do you think telemedicine could be used for different things in healthcare’? |
‘when there's complications…something that you might need a specialist to look at’ (P18: ‘live’ and mock‐up, patient's husband) |
Coherence (sense making)
Three codes were identified under the heading of coherence: Prior experience of TM; Understanding of reason; and TM vs. other modalities. There were no data elicited that could be coded to the NPT subdomain relating to communal specification.
The majority of participants (n = 21) stated that they had no prior experience or knowledge of TM, whilst one participant stated that they had heard about it on TV but had never experienced it. Despite their lack of prior knowledge, most participants (n = 18) articulated the rationale for TM in terms of speeding up patient assessment, or enabling treatment when a consultant couldn't be there:
‘Consultants have got to have some time off… when they get patients in that need checking and some urgent treatment, the consultant would link via this live thing so they could ask questions, view the patient and then they would come to a decision with the doctors who were already on site as to what treatment they could give’ (P3: ‘live’, patient's husband).
Others (n = 12) referred to an understanding of the process of TM. However, some participants (n = 6) did not understand, or had a poor understanding of, its purpose. Others (n = 8) mentioned purposes such as cost‐cutting rather than expediting assessment.
Many participants (n = 13) felt that TM was comparable to a face‐to‐face consultation in terms of the consultation process and the opportunity for two‐way communication:
‘he (doctor) couldn't have done any more I don't think, because he asked all the questions…he looked in his eyes and he checked his weight, he asked what height and everything… so if he'd have been there I don't think it could have been much different’ (P2: ‘live’, patient's wife).
TM was also compared favourably to telephone consultation (n = 5), because it enabled patient participation and direct evaluation of the patient's condition, rather than relying on a verbal description of the patient's problem via a telephone intermediary. Others (n = 8) stated that a face‐to‐face consultation would have been preferable or superior, because the TM process was slightly detached and did not allow the same degree of personal interaction, particularly if the patient or carer had any queries.
Cognitive participation (enrolment – relational work to build and sustain the practice)
Five codes were located in this domain: interaction between staff; patient and carer involvement; staff presence; privacy; and recording.
The ‘remote’ assessor (consultant physician) was felt to take the lead in the TM process (n = 7), in line with their seniority and expertise, despite not being physically present:
‘the (remote) doctor was asking what I could do at present, and the nurses were doing what he said’ (P12: mock up, male patient, age 68).
The importance of three‐way communication between remote staff, bedside staff and patient was also noted (n = 5). Participants’ recollection of the content of staff–staff interaction included relaying practical matters (n = 6) and was centred on clinical decision making relating to the use of thrombolysis (n = 3).
Many carers (n = 11), as well as patients (n = 12), reported that they felt involved in the process and decision. This was facilitated by being able to speak directly to the consultant via the video link, rather than receiving advice through an intermediary. However, it was felt that involvement was more challenging than it would have been in a face‐to‐face consultation (n = 7), due to the need to interact with the remote assessor via a video link, which was an unfamiliar experience for all participants in the context of receiving health care. Nonetheless, even when the patient had a communication difficulty, for example due to aphasia, staff made efforts to involve them in the consultation:
‘(the patient) couldn't answer and he couldn't respond, but he understood… so it was a great help that he could be part of the decision…I asked him either to blink or press my hand…I felt he very much gave the consent to it as much as myself’ (p5; ‘live’ and mock up; patient's wife)
Some participants (n = 9) commented on the large number of people present at the bedside:
‘There were plenty of other people around… that were looking at her and were very hands on with her’ (p3: ‘live’; patient's husband).
It was felt that either nursing or medical staff were appropriate and acceptable health professionals to perform the role of the ‘bedside’ member of staff, provided they had the necessary skills and knowledge. One participant also mentioned the importance of having a continuous staff presence.
There were positive comments about the level of privacy (n = 10): participants felt that the setting was sufficiently private and that only the appropriate personnel were present:
‘they had screens round… no other visitors or no one else could see, there was only the people there that really you felt needed to be there’ (P11: ‘live’, patient's sister).
However, others (n = 4) felt that concerns about privacy were over‐ridden by the need for emergency treatment. Some (n = 4) felt that privacy was similar to a face‐to‐face consultation.
None of the participants stated that they would have had any objections to a recording being made of the consultation:
‘To be honest I just thought it was recorded. It wouldn't matter’. (p11: ‘live’, patient's sister – not recorded).
Those who had a recording of a mock‐up consultation felt that this process was routine and unobtrusive. Two participants suggested that the need for informed consent was an important caveat to recordings being obtained. Four participants suggested possible uses for recordings, such as helping to improve future patient care, or retention as part of the patient's health record.
Collective action
Five codes were identified in this domain: Information exchange before or during consultation; Technical and audio–visual issues; Support; and Trust. There were no data elicited that could be coded to the NPT subdomain relating to contextual integration.
Most participants (n = 19) felt that both bedside and remote staff provided them with sufficient information and adequately explained the procedure. They recalled being given information mostly about the TM process (n = 15), and details of the consultant's name, location and role (n = 6):
‘the nurses explained who it was when (consultant) came on, and why he was going to ask us all the questions’ (P24: ‘live’, patient's wife).
However, three participants felt that they were not made aware of the process or that they needed more forewarning.
Many participants commented that the teleconsultations ran smoothly without technical problems, but some experienced problems (n = 11) such as technical issues, or problems with staff familiarity and expertise in using the system. Participants felt that it was important that the technical aspects of the consultation operated smoothly. Some patients and carers expressed feelings of embarrassment at seeing an image of themselves, as well as the remote assessor, on screen. A participant who was partially sighted felt that receiving a clear explanation from staff was particularly important.
Participants’ previous experiences of other audio–visual communication systems (e.g. Skype) were valuable in aiding familiarity with the TM system (n = 8), and it was also felt that people without such experience, especially older people, might find the system more daunting:
‘I'd seen it before at my niece's when we were talking to her son in Australia, but whether it would affect people who have never used it before – and of course anybody your age (researcher), they're used to it aren't they’. (p24: ‘live’, patient's wife).
There were many positive comments about the level of support received from staff at the bedside (n = 14). The remote consultant was also felt to be supportive, despite not being present in person (n = 7). It seemed important that patients and carers were told the consultant's name and that he or she displayed good interpersonal skills:
‘Once I was introduced to the doctor, I didn't have a problem, I was alright talking to him’ (p9; ‘live’; male patient, age 49).
The quality of support from clinicians was attributed to clinical expertise of the local staff and remote staff (n = 8), as well as their interpersonal skills (n = 7). Many participants expressed confidence or trust in the system or the staff members present (n = 12). However, three participants were concerned about the identity and professional qualifications of the doctor at the ‘remote’ end of the consultation.
Reflexive monitoring (evaluation)
Four codes were located in this domain: process (positive/negative issues); emotional reaction; impression of TM; other TM uses. There were no data elicited that could be coded to the NPT subdomains relating to systematization and communal appraisal.
The TM system was felt to be smooth, simple and fast (n = 13):
‘the speedy getting in touch with somebody who knows what they're doing… and the efficiency…it was absolutely amazing’ (p6: ‘live’; male patient, age 71).
Only one participant, a carer in a ‘live’ consultation, reported significant delays. Participants commented positively about their own role in the clinical or technical aspects of the process (n = 8), and on the roles of bedside or remote staff (n = 7).
Many of the participants who had had ‘live’ telestroke consultations discussed the emotions they had experienced at the time of the telestroke consultation. The emergency admission and the serious nature of the diagnosis, rather than the telestroke system itself, were found to be upsetting and stressful (n = 9). The provision of expert assessment and advice via telestroke was felt to reduce this stress:
‘I felt all moithered (flustered/worried) but I think I was just grateful that he had the best care’ (p2: ‘live’; patient's wife).
However, four participants felt that the TM system was daunting because of its unfamiliarity, and two felt that a face‐to‐face consultation would have been less stressful.
TM was generally well received by patients and carers. Many highly positive terms, such as ‘good’, ‘brilliant’, ‘wonderful’, ‘fantastic’ and ‘amazing’, were used (n = 17) to describe their overall impression of the system:
‘I think it's brilliant….it feels like they're in the room’ (P16: mock‐up, female patient, age 46).
However, some disadvantages were also identified. Three participants felt that an older person might find it daunting, and one felt that its acceptability and workability might depend on the severity of stroke.
Many other potential uses for TM were mentioned (n = 17), such as accessing a second opinion (n = 2), or use in other specialist areas (n = 9).
Discussion
In the development of TM and other new technologies in health care, the experiences and perspectives of patients and carers might be overlooked in the rush to adopt new ways of working. Although the hypothetical acceptability of TM in stroke for patients and carers has been explored,15 the reality of having a TM consultation, especially in an emergency care situation, may be very different from people's expectations. To our knowledge, this is the first study of the lived experiences of patients and carers who have undergone actual TM consultations for acute stroke. Similar high levels of satisfaction and acceptance, as expressed by our participants, have previously been found in studies of stroke telerehabilitation,19 joint primary–secondary care consultations for dermatology,17 and elderly care.18 Our findings also support previously reported issues, such as the perceived superiority of face‐to‐face consultation,18 the need for staff to have excellent technical skills,18 the importance of staff interpersonal skills17 and a sense of alienation arising from the use of TM17 [described in our study as being ‘detached’ (participant 9) or ‘weird’ (participant 10)].
NPT is a valuable framework to analyse people's illness experiences and has been used recently in a large systematic review of qualitative studies of the treatment burden of stroke.24 However, the applicability of NPT to an emergency, one‐time event like acute stroke assessment has not previously been explored. Although NPT has been used in a number of studies of telecare and e‐health,22 this body of literature contains little previous work on patients’ and carers’ perspectives. We found that, although the overall NPT domains of coherence, cognitive participation, collective action and reflexive monitoring emerged from our data, there was an imprecise fit with the NPT subdomains. There were no data that could be coded to four of the 16 subdomains (communal specification, contextual integration, systematization and communal appraisal). This may reflect the short‐lived role played by individual patients and carers in the health setting. Saturation of the other subdomains was achieved, however. Our use of open coding and thematic analysis of the interviews may have helped to overcome the imprecise fit between the data and the NPT framework. However, as the interview schedule itself was based around NPT, it is possible that some important themes did not emerge. The NPT framework may require adaptation to fully realize its potential in the context of patients’ experiences of emergency and acute health care. In health settings with which patients and carers have multiple or sustained contact, such as in primary care settings or services for long‐term conditions, there might be more scope for them to engage in the types of work in these missing subdomains.
Limitations of this study include the fact that all participants were recruited from one UK TM network, and from only three of the eight hospital sites within the network. This limits generalizability of the findings to other settings where working practices and staff training may be very different. Furthermore, the recollection of some of the patients who participated was limited by a fluctuating conscious level or cognitive impairment at the time of the consultation. Some who were approached to take part in this study had little or no recollection of having had the consultation at all, despite having since regained consciousness and cognitive capacity. Carers tended to have a clearer recall of events, and the inclusion of their perspectives added another important dimension to the study for this population group. Due to ethical approval restrictions, we were not able to include patients who had persistent cognitive impairment and who lacked capacity to consent, or their carers.
Although the largest group of participants (n = 11) was those who had a TM consultation as a standard element of their care out‐of‐hours (‘live’), we also included some patients who had the consultation solely for this research programme (‘mock‐up’) (n = 9), and a small number who had both ‘live’ and ‘mock‐up’ consultations (n = 4). It is possible that the additional information and support which they received for the research consent process and participation in ‘mock‐ups’ may have influenced their views. It was notable that those who had both ‘live’ and ‘mock‐up’ consultations articulated views that the two were very different. This may have implications for the value of ‘mock‐up’ recordings for staff training purposes.
Despite their lack of familiarity with videoconferencing technology, and the urgency of the situation, most of our participants coped well with being subjected to telestroke. However, this may have been partly because of its relative novelty: staff may have taken great pains to explain the system and to put the patient and carer at ease during the consultation. Those who had ‘mock‐up’ consultations received additional explanation and the opportunity to ask further questions as part of the informed consent process for recording.
The findings from this study suggest that patients and carers can engage well with telemedicine programmes in acute stroke, and find their use acceptable. However, there are several aspects which need attention from clinical staff in order for the benefits of such systems to be maximized. It seems important that patients and carers are given information about the telemedicine system and procedure by bedside staff; that the identity and credentials of the ‘remote’ practitioner are made explicit to the patient and carer; that remote and bedside practitioners communicate well with each other and with the patient and carer; that privacy is maintained; and that staff are able to use the technology competently. As the use of video technologies becomes more widespread in the future, it is vital that assumptions are not made about patients’ familiarity with such systems and the acceptance of their use in a health‐care context. Even someone who is familiar with videoconferencing in a business context, for example, might find it disconcerting to be faced with similar technology when experiencing an acute, distressing and life‐threatening illness. An important feature with the telestroke system is that a ‘head‐to‐toe’ image of the patient is transmitted to enable the consultant to assess neurological function, whereas most everyday uses of videoconferencing utilize only head‐and‐shoulders images. While most of our participants had generally positive views, the TM consultation was felt to be ‘different’ from a face‐to‐face one. Analysis of the actual content of TM consultations would enable further exploration of this finding.
Conclusion
TM consultations for assessment and treatment planning in acute stroke appear to be generally acceptable to patients and carers. However, there is a trade‐off between the need for immediate expert medical advice, and a preference for face‐to‐face consultation. This compromise can be ameliorated to some extent, and patients’ and carers’ experiences enhanced, by excellent communication from and between staff. Our study suggests that clinical and technical competences alone are not sufficient; staff selected to use such technologies need also to have excellent communication skills. Training in the use of telestroke should include development of interpersonal skills specific to the challenge of using such systems. Patients’ and carers’ familiarity with new technologies should not be assumed, especially in older people and others from hard‐to‐reach groups.
Sources of funding
This paper summarises independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit Programme (Grant reference number PB‐PG‐1208‐18280). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of interests
No conflicts of interest have been declared.
Acknowledgements
We thank Mark O'Donnell, Paul Davies, Kausik Chatterjee, and David Hargroves for their support of this project.
References
- 1. National Audit Office, Department of Health . Reducing Brain Damage: Faster Access to Better Stroke Care. London: The Stationery Office, 2005. [Google Scholar]
- 2. Rudd AG, Hoffman A, Grant R, Campbell JT, Lowe D. Stroke thrombolysis in England, Wales and Northern Ireland: how much do we do and how much do we need? Journal of Neurology, Neurosurgery and Psychiatry, 2011; 82: 14–19. [DOI] [PubMed] [Google Scholar]
- 3. Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database of Systematic Reviews, 2009; Art. No.: CD000213. [DOI] [PubMed] [Google Scholar]
- 4. Saver JL, Fonarow GC, Smith EE et al Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. Journal of the American Medical Association, 2013; 309: 2480–2488. [DOI] [PubMed] [Google Scholar]
- 5. Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews 2007; Art. No.: CD000197. [DOI] [PubMed] [Google Scholar]
- 6. Demaeraschalk BM, Miley ML, Kiernan T et al Stroke telemedicine. Mayo Clinic Proceedings, 2009; 84: 53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deshpande A, Khoja S, McKibbon A, Rizo C, Jadad AR. Telehealth for Acute Stroke Management (Telestroke): Systematic Review of Analytic Studies and Environmental Scan of Relevant Initiatives. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health, 2008. [Google Scholar]
- 8. Hailey D, Ohinmaa A, Roine R. Recent Studies on Assessment of Telemedicine: systematic review of study quality and evidence of benefit. Institute of Health Economics Working Paper 03‐04, 2003. Available at: http://www.ihe.ca/publications/library/working-papers/page/6/, accessed 15 October 2013.
- 9. Price CI, Clement F, Gray J, Donaldson C, Ford GA. Systematic review of stroke thrombolysis service configuration. Expert Reviews in Neurotherapy, 2009; 9: 211–233. [DOI] [PubMed] [Google Scholar]
- 10. Intercollegiate Stroke Working Party . National Clinical Guideline for Stroke, 4th edn London: Royal College of Physicians, 2012. [Google Scholar]
- 11. Office for National Statistics . Statistical bulletin: Internet Access – Households and Individuals 2012 part 2, 2012. Available at: http://www.ons.gov.uk/ons/rel/rdit2/internet-access-households-and-individuals/2012-part-2/stb-ia-2012part2.html, accessed 8 April 2014.
- 12. Department of Health . National Stroke Strategy. London: Department of Health, 2007. [Google Scholar]
- 13. NICE Clinical Guideline CG138. Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services. London: NICE, 2012. [Google Scholar]
- 14. Staniszewska S, Crow S, Badenoch D et al The PRIME project: developing a patient evidence‐base. Health Expectations, 2010; 13: 312–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finch T, Mort M, May C, Mair F. Telecare: perspectives on the changing role of patients and citizens. Journal of Telemedicine & Telecare, 2005; 11(Supp. 1): 51–53. [DOI] [PubMed] [Google Scholar]
- 16. Collins K, Walters S, Bowns I. Patient satisfaction with teledermatology: quantitative and qualitative results from a randomized controlled trial. Journal of Telemedicine & Telecare, 2004; 10: 29–33. [DOI] [PubMed] [Google Scholar]
- 17. Harrison R, MacFarlane A, Murray E, Wallace P. Patients’ perceptions of joint teleconsultations: a qualitative evaluation. Health Expectations, 2006; 9: 81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shah M, Morris D, Jones CM et al A Qualitative Evaluation of a Telemedicine‐Enhanced Emergency Care Program for Older Adults. Journal of the American Geriatrics Society, 2013; 61: 571–576. [DOI] [PubMed] [Google Scholar]
- 19. Johansson T, Wild C. Tele‐rehabilitation in stroke care ‐a systematic review. Journal of Telemedicine & Telecare, 2011; 17: 1–6. [DOI] [PubMed] [Google Scholar]
- 20. Mort M, Roberts C, Pols J, Domenech M, Moser I, on behalf of the EFORTT Investigators . Ethical implications of home tele‐care for older people: a framework derived from a multi‐sited participative study. Health Expectations, 2013. doi: 10.1111/hex.12109 [E‐pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology, 2009; 43: 535–554. [Google Scholar]
- 22. McEvoy R, Ballini L, Maltoni S, O'Donnell CA, Mair FS, MacFarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implementation Science, 2014; 9: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. French B, Day E, Watkins C et al The challenges of implementing a telestroke network: a systematic review and case study. BMC Medical Informatics and Decision Making, 2013; 13: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gallacher K, Morrison D, Jani B et al Uncovering treatment burden as a key concept for stroke care: a systematic review of qualitative research. PLoS Medicine, 2013; 10: e1001473. [DOI] [PMC free article] [PubMed] [Google Scholar]


