Abstract
Objective
To compare factors considered by parents to those considered by adolescents making decisions about chronic disease treatments.
Methods
We conducted individual interviews with 15 parent–adolescent dyads in which the adolescent had either juvenile idiopathic arthritis or Crohn's disease. Questions focused on treatment decisions, with an emphasis on the factors that influenced each individual's preferences related to biologic therapies. A multidisciplinary team developed a coding structure. All interviews were coded by two people with disagreements resolved through discussion. We used content analysis and coding matrices to examine decision factors within and between parent–adolescent dyads.
Results
Parents and adolescents both participated in decisions about treatment with biologic therapies but considered decision factors differently. In only half of cases did parents and adolescents agree on the factor that most influenced their decision. Although their decision factors often fell into similar categories (e.g. treatment risks, quality of life), in many cases the specifics varied between adolescents and their parents. Adolescents were more likely to focus on immediate treatment effects and quality of life while parents took a longer term view of the decision. Agreement within dyads was most consistent when a special circumstance influenced the treatment decision.
Conclusions
Differences regarding influential decision factors exist within parent–adolescent dyads. Continued research is needed to determine the extent to which such differences are due to individual preferences or to variations in the information available to each person. Future decision support interventions will need to address parents’ and adolescents’ potentially disparate views and information needs.
Keywords: adolescent, biologics, chronic conditions, decision making, parents
Introduction
Decision making for patients with chronic conditions is often complicated by trade‐offs between the risks of poor disease control and the risks of treatment. Additionally, because many decisions in chronic conditions occur over time, 1, 2, 3 they may be more challenging than decisions in acute care.4, 5 The fact that an established relationship often exists between the provider and family, as well as the chance to frequently reconsider decisions, may change the nature of decision making, as compared to ‘classic’ high‐stake decisions such as in adult cancer screening or elective surgery.6, 7, 8, 9 In the context of an adolescent patient whose decision‐making skills are growing as they do, the challenges of medical decision making increase. The difficulty of such situations may lead to poor quality decision making, increased family stress, regret about the decision and potentially reduced treatment adherence.1, 10
The few studies that consider both parent and adolescent perspectives on decision making in chronic disease show discrepancies between parents’ decisions and decision‐making style preferences and those of their adolescents.11, 12 They also find benefits to collaborative decision making between parents and children.13 As they gain autonomy in other areas of their lives, adolescents may also seek increasing autonomy in health‐care settings. Despite this, several studies report that many adolescents want continued parent involvement in medical decisions.14, 15, 16 It is unknown whether adolescents with chronic conditions and their parents consider the same factors when making treatment decisions. Knowing whether or not parents and adolescent consider the same factors may help in developing interventions that facilitate the involvement of parents, adolescents and clinicians in medical decision making.
To study this, we examined decision making in the context of biologic therapies. Tumour necrosis factor‐α inhibitors (TNFαi), a class of biologics, may limit disability and alleviate symptoms but have limited long‐term effectiveness data. They also are associated with immune suppression, risk for opportunistic infections and possible increased risk of malignancy.17, 18 Given these trade‐offs, the decision to initiate treatment with TNFαi, in Crohn's disease (CD) or juvenile idiopathic arthritis (JIA), can serve as a model for comparing the factors parents and adolescents use when making challenging chronic disease treatment decisions. The aim of this study was to compare the factors influencing a given parent to those influencing that parent's adolescent when making decisions about chronic disease treatments.
Methods
Recruitment
Participants were recruited from a large, academic children's hospital. Parents of children diagnosed with CD or JIA were identified, for our initial parent‐focused study,19 through local disease registries and provider referrals. Parents were eligible if they had considered TNFαi treatment in the past year, were English‐speaking, and the patient did not have a co‐morbid diagnosis that could also be treated with TNFαi. Potential participants were sent an introductory letter and then contacted by telephone to arrange for individual interviews. Having established our criteria for information saturation prior to beginning interviews, one parent per family was recruited until we reached information saturation for each disease,20 the point at which no new decision factors were discussed after three consecutive interviews. In total, 34 parents were interviewed, of which 20 had a child with JIA or CD age 12–18 (See Fig. 1).
Figure 1.
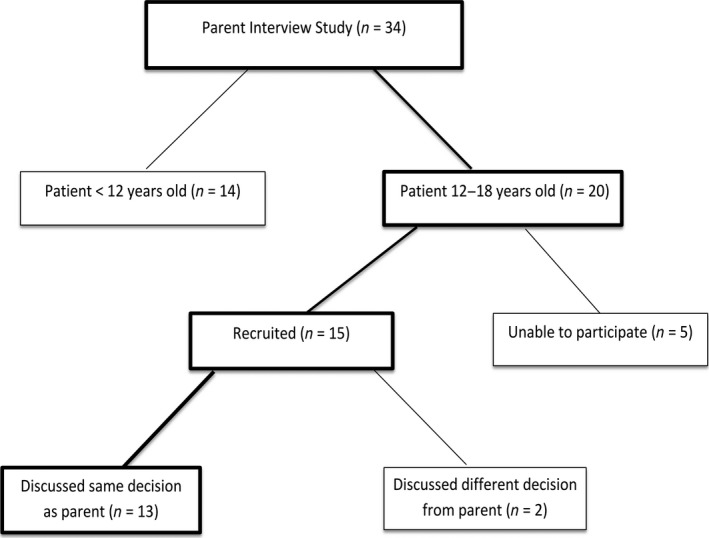
Recruitment.
We then expanded the study to include adolescents. Adolescents of participating parents were sent letters inviting them to participate in the study. Adolescents were contacted by telephone to arrange for individual interviews. They were recruited until we exhausted all potential participants. Data analysis21 showed that this approach also led to information saturation from the adolescents, meaning no new factors arose in the last three interviews.
We conducted individual interviews with parents and adolescents from 15 dyads. The remaining five adolescents of interviewed parents declined to participate or logistics (such as a hospitalized parent) prevented their participation. In two dyads, the parent discussed a different TNFαi decision than the adolescent did. For example, in one dyad, the parent discussed the decision to start TNFαi treatment and the adolescent discussed the subsequent decision to discontinue treatment. Because these interviews focused on different decisions, we were unable to directly compare the factors that influenced these parents’ and adolescents’ decisions. Therefore, they were excluded from our final sample.
The Cincinnati Children's Hospital Medical Center Institutional Review Board approved this study. Parents provided written, informed consent for themselves and their children. Adolescent gave written assent to participate. Parent participants received $30 remuneration; adolescents received $20.
Interview guide and process
Based on existing adult and paediatric literature about treatment decision making,22, 23, 24, 25, 26, 27, 28, 29 and input from clinicians, we developed semi‐structured interview guides (available upon request) focused on decisions related to CD or JIA. Parent and adolescent interviews started with general questions and moved towards an in‐depth discussion about disease‐related decisions, with an emphasis on treatment decisions (see Box 1). In discussing the TNFαi decision, we included questions about the decision process, factors considered in the decision and information used. After reviewing the first four interviews, minor changes were made to the guides.
Box 1. Interview Guide Topics.
-
1
General Experiences with Chronic Illness Typical day; positive and negative experiences with illness
-
2Decisions Made in Relation to Chronic Illness Most challenging decision; people involved in each decision; sequence of decision‐making events
- TNFαi Decision: Decision‐making process including: treatment options; role of each person involved in decision; perceived risks and benefits; information needs; information sources
-
3
Demographic Information Note: Box includes only topic areas related to this study
Parents and adolescents participated in in‐person (13 adolescents, 12 parents) or telephone (two adolescents, three parents) interviews with one of two trained interviewers. Parents met the interviewer at a hospital location. As most adolescents were not of driving age, adolescent interviews were scheduled at their home or to coincide with an existing medical appointment. Telephone interviews were used for participants who lived more than 1 h from Cincinnati Children's Hospital and did not have an upcoming appointment. Adolescents were not present during the parents’ interviews and, with one exception, parents were not present during the adolescents’ interviews. Parent interviews ranged from 28 to 75 min (mean 44 min). Adolescent interviews ranged from 22 to 40 min (mean 32 min). Interviews were audio‐recorded for verbatim transcription. All transcripts were verified by study staff.
Data coding and analysis
We used content analysis30, 31, 32 for data coding and analysis. The first four parent transcripts were annotated and open‐coded by a research team that included clinicians from gastroenterology, rheumatology, general paediatrics and adolescent medicine. These transcripts were used to develop a coding structure that was applied to all the parent interviews. Similarly, for the adolescent interviews, we started with the parent coding structure, to facilitate comparison between the two groups, and modified it based on the first two adolescent interviews. No major themes were added at this stage, but a few subthemes (such as short‐term quality of life) were added. In addition to the team listed above, an undergraduate summer student participated in the coding of the adolescent interviews. The coding structures (see Box 2) were approved by all study team members, applied to the initial transcripts and used for the remainder of coding. We also coded for the most influential factor in each person's decision, defined as the one participants either mentioned most often or specifically stated was most important. Two researchers independently reviewed the remaining transcripts and resolved differences through discussion.
Box 2. Major Themes: Factors Contributing to Decision Making.
Disease characteristics
Quality of life
Treatment benefits
Treatment risks
Provider recommendation
Using a sequential matrix approach, 33 we compared parents’ decision influences, the facts and preferences that influenced their decision, to those of their children and then made comparisons among parent–adolescent dyads. The first set of matrices was structured to compare the decision factors within each parent–adolescent dyad. We then created a large matrix in which we colour‐coded dyads’ areas of agreement and disagreement. This facilitated a visual overview of our data and comparisons between parent–adolescent dyads. Except where otherwise specified, dyads were said to agree if both mentioned a specific category of information, even if the details were not identical. For example, if an adolescent with CD mentioned persistent diarrhoea and his mother mentioned weight loss as decision factors, they would be said to agree that ‘disease factors’ influenced the decision. NVivo 8 (QSR International, Doncaster, Vict., Australia) was used for coding.
Results
Participant demographics
The demographics of the included 13 parent–adolescent dyads, all of whom discussed the decision to initiate TNFαi treatment, are shown in Table 1. We found no differences by disease or gender. The median number of months between the decision and the interview was 4 for parents and 14 for adolescents. This difference reflects the order in which participants were recruited. Due to scheduling difficulties, one parent was interviewed 15 months after having made the decision.
Table 1.
Participants
| Characteristic | |
|---|---|
| Parent, n | |
| Mom | 12 |
| Dad | 1 |
| Adolescent, n | |
| Female | 8 |
| Male | 5 |
| Juvenile idiopathic arthritis, n | 7 |
| Inflammatory bowel disease, n | 6 |
| Adolescent age at decision, median (range) | 13 (10–15) |
| Age at interview, median (range) | |
| Parent | 42 (36–57) |
| Adolescent | 14 (13–18) |
| Months since decision, median (range) | |
| Parent | 4 (1–15) |
| Adolescent | 14 (13–18) |
| Parent Education, n | |
| <College degree | 5 |
| 4‐year college degree | 3 |
| >College degree | 5 |
Participation in the decision
In all but one case, both the parent and the adolescent had participated in the decision about initiating TNFαi treatment. The exception was a case where the mother, who participated in our interview, had been hospitalized at the time of the decision. In this situation, the adolescent felt that he also had no role in the decision because it was based on a change in health insurance. All other parents and adolescents felt they each had participated in the decision.
Most influential decision factor
We first analysed the participant's most influential decision factor, the one mentioned most often or specifically stated as most important. In approximately half of the dyads, the most influential decision factor, such as worsening symptoms or a desire to avoid side‐effects, was the same for the parent and the adolescent. As an example, consider the 16‐year‐old girl with JIA who said, ‘[my jaw] would hurt really bad and that's what the challenge is itself, it was just miserable pretty much’ and her mother who said, ‘she would use a heating pad and just curl up in a ball on the couch, she would use a heating pad right there on her joints’. These cases of agreement included two where the decision was based on very specific circumstances, such as the one mentioned above whose decision was based on a change in insurance coverage. One adolescent was most influenced by the provider's recommendation, which was not mentioned at all by her mother. In all other dyads, the adolescents’ most influential factors were always mentioned by their parent, even if they were not the most influential factor. The converse was not true; in many cases, factors mentioned by parents as strongly influencing their decisions were never mentioned by their adolescents. Comparing between, rather than within, parent–adolescent dyads revealed that no one factor, or category of factors, was consistently emphasized across the sample.
The remainder of the results discusses the diversity of factors that influenced decision making, but were not necessarily emphasized in each interview. They are organized according to the major coding themes (see Box 2). For a comparison of the number of dyads vs. individuals mentioning decision factors in each theme, please see the Table S1.
Disease characteristics
In a few dyads, both the parent and the adolescent mentioned that disease characteristics influenced their decision about TNFαi treatment. In these cases, it was typically a very specific disease characteristic, such as poor growth or eye inflammation, rather than a general statement about disease severity. For example, in one dyad, the mother said ‘the [TNFαi] [would be] better in growth, and we clarified where [our son] was in the puberty stages and so he was within the area that he could still benefit from it’. Her 15‐year‐old son said ‘so as we got older everyone else was getting bigger and stuff, and as of like last year I wasn't growing as much’.
In contrast when only one member of the dyad commented on disease characteristics influencing their decision, it was almost always the parent. It was most often a comment on a specific symptom such as the mother of a 15 year old with JIA that said, ‘she does have the joint damage, her body is in essence attacking itself, we have to do something’ or the general severity of the adolescent's disease such as the mother of a 16 year old with JIA who said, ‘[she] was in such bad shape at that point that we knew–I didn't have time to question’.
Treatment benefits
Other than in the situations where a specific disease characteristic influenced the decision, few parents or adolescents commented about precise treatment benefits when discussing factors used to make the decision to initiate TNFαi treatment. Instead benefits were discussed in more general terms. In this context, both the parent and the adolescent in approximately half of dyads made general statements about treatment benefits factoring into their decision. For example, one father said, ‘I hope it works’ and his 13‐year‐old daughter said ‘one of the pros [of Remicade] is that it would help my system’. Included in the dyads where both members mentioned treatment benefits were two where both the parent and adolescent mentioned a sibling who benefited from TNFαi treatment. In only a few dyads did anyone comment on specific data showing benefits such as, ‘[TNFαi] was supposed to have the best benefit’ and ‘it had a relatively long term successful record’. Of these dyads in which someone did discuss data, the parent always mentioned it and in only one case did the adolescent. There were no instances where an adolescent discussed data and his or her parent did not.
Treatment risks
In contrast to treatment benefits, most references to treatment risks, particularly by parents, were fairly specific. Although all parents mentioned treatment risks, in just over half of dyads did both the parent and adolescent state that treatment risks influenced their decision. For example, in one dyad, the mother referred to, ‘the cancer concerns, I mean how much more crippling it would be to his immune system’ and her 15‐year‐old son said, ‘the only [side effect] I really remember was like the 5% chance of getting cancer or whatever it was. That was the only one that was serious enough that me and my parents talked about it in depth’. Among the adolescents who did not mention risks, some commented that they thought ‘about the pros and cons of it’. However, when asked, they were unable to name any cons. Of note, no adolescent under age 14 named a specific risk as a decision factor, although they may have commented generally about treatment risks. For example, one 13‐year‐old girl with JIA said, ‘yeah, I mean [both options] could have side effects and other things’.
In the dyads where both parent and adolescent mentioned risks, they did not always mention the same risks and parents tended to be more specific in their discussion of risks. For example, although the most commonly mentioned risk was malignancy, nearly all parents mentioned it but only two of their adolescents did. Among the parents who mentioned malignancy, but whose adolescent did not, was a mother who specifically said, ‘[the doctor] told [my son] about the cancer… And I had to talk to him and have her talk to him again because he got so upset…’ Parents who did not discuss malignancy included a couple that mentioned general long‐term side‐effects but gave no specifics. As one mother said, ‘I don't even like to talk about what could happen, but there's increased percentages of things’. Similar to malignancy, immunosuppression was mentioned by about a quarter of parents but by none of their adolescents. It was often discussed in the context of increased vulnerability to common infections, as in the mother who said, ‘[TNFαi] reduces your immune system so you are more likely to pick up other viruses and things….’
Quality of life
The most often mentioned decision factor related to the patient's quality of life was the fact that TNFαi treatment is currently only available as an injection or intravenous infusion. Parents and adolescents mentioned multiple decision factors related to the effects that receiving injections or infusions would have on the patient's short‐term quality of life. These included pain from injections or infusions, the frequency of injections and logistical challenges of intravenous infusions. In almost half of dyads, both the parent and adolescent mentioned the relationship between route of administration and quality of life as a decision factor. Most agreed about the direction of this influence. However, in one dyad, the mother was concerned that for infusions ‘…the time issue is a factor. How much time it takes….’ Whereas her adolescent preferred infusions because he felt, ‘… we collectively waste less time doing [TNFαi infusion] than we do with taking pills each day’. In the rest of the dyads, the adolescent mentioned route of administration but the parent did not. To illustrate, one 13‐year‐old boy with CD stated, ‘I wanted to know if [TNFαi] actually stings more… so I wanted to know if it actually hurt’. Only one adolescent's concern about the route of administration was not about TNFαi but rather that the alternative, nasogastric tube feeding, was ‘nasty’.
In addition to pain associated with treatment, other aspects of the adolescents’ near‐term quality of life were also mentioned frequently by virtually all adolescents, but by only two of their parents. As a 15 year old with CD said, ‘I kind of just want to feel better now’. Factors such as school attendance, athletics, avoiding hospitalization, avoiding the pain associated with disease and generally feeling better were among the near‐term quality of life aspects named.
In contrast to decision factors related to short‐term quality of life, in only one dyad did both individuals mention long‐term quality of life as a decision factor. However, several other parents mentioned related topics, such as social interactions, as influencing their decision. As one parent said, ‘I worry about the social and the emotional aspects and continuing normal activities’.
Provider recommendation
The health‐care provider's recommendation was the least frequently mentioned of the major decision factor themes. For one dyad, both the parent and adolescent felt that the recommendation influenced their decision, as the mother said, ‘we had to rely completely on the doctor's suggestion and recommendations…I had to trust her judgment completely on that because I didn't know’ and the adolescent said, ‘I didn't know what was the best…well, the doctor knows the most obviously’. A few other parents and adolescents mentioned the provider's recommendation, although the other half of their dyads did not.
Discussion
Although parents and adolescents were often influenced by the same categories of decision factors, for example treatment risks, we found the specifics and the weight given to each factor varied. Moreover, by evaluating matched parent–adolescent dyads, we demonstrated that discrepancies between the decision factors considered by parents and adolescents often occur within families. This led to frequent mismatches between the most influential decision factor for a parent and the one that most influenced their adolescent, with some factors being considered by only one member of the dyad. This incongruity in the factors considered in a real‐life decision is consistent with prior research focused on hypothetical decisions.11, 34
The contrast between adolescents’ focus on short‐term quality of life, such as the impact of pain associated with the route of administration, and many parents’ focus on longer term risks, such as malignancy, is likely rooted in two distinct but crucial aspects of medical decision making. The first is that, consistent with their developmental level,35, 36 adolescents may be more likely to focus on near‐term effects while parents have a longer term perspective. In fact, in our previous analysis focused exclusively on adolescents’ roles in decision making, we found that when considering future decision making, many recognized their need for an improved long‐term perspective.21 Second, it may be that some adolescents were unaware of long‐term side‐effects. Other studies have shown that parents may limit the information given to their children.37 Parents may be uncomfortable discussing the risks with their child or may be unsure how to fully include their adolescent in medical decision making.10, 38, 39
The divide between parents and adolescents was less striking in other quality of life aspects than in side‐effects, but there was still a difference in the relative emphasis on near‐term and long‐term quality of life. While perhaps not surprising, this difference highlights an area of potential conflict if parents and adolescents are unaware of the factors the other is considering. Thus, decision support tools need to both promote informed decision making and provide support for families in which there may be disagreement about the goals of treatment.
Although mentioned by both parents and adolescents, we were surprised that, in most cases, neither specific disease factors nor treatment benefits were discussed as being highly influential in treatment decision making. We suspect that this may reflect both discomfort with discussing specific disease symptoms, as well as participants’ potential assumptions that the role of disease and treatment benefits were so apparent that they did not warrant mention. To truly know what factors are considered, both during and after clinical discussions about TNFαi, prospective observation and longitudinal follow‐up of the decision process will be needed.
While parents and adolescents often differed, when there were very specific circumstances or goals, parents and adolescents were typically in agreement. For instance, in decisions strongly influenced by insurance coverage, participation in athletics or the experience of a sibling who took the medication, parents and adolescents were both influenced by this same specific factor. This suggests that parents and adolescents may have engaged in some discussion of the goals of treatment and factors influencing their decisions or that such decision factors reflect their general family values. However, the degree to which such discussions occurred among our study participants is unknown as our interview guide did not include this topic. Alternatively, such agreement may reflect later discussions that have led to bias in recalling the pre‐decision influences.
In two cases, the decisions discussed by the parent and by the adolescent were different. Although these cases were excluded from further analyses, they highlight the longitudinal and iterative nature of decision making in chronic disease. Over time, decision factors may change, as does an adolescent's decision‐making capacity.40 Such parallel changes may complicate the decision‐making process and further challenge parents and providers striving to include adolescents in medical decision making.
The retrospective nature of the interviews and lag time between parent and adolescent interviews limits our ability to know how accurate the recollection of decision factors was. Although participants did not articulate any difficulty remembering the decision, the time since the decision may have led to a modified recollection in order to be more consistent with the decision they made. For example, cognitive dissonance theory41 would suggest that, given the challenge of this decision, those who chose to start TNFαi may downplay risks in their recollection of the decision and those who chose not to start TNFαi may downplay benefits. In this way, it is possible that some decision factors named by parents or adolescents were not considered at the time of the decision, but were used later to support their decision.
Our adolescent sample size was limited by the parents who had been interviewed. As such, it may have been too small to detect any differences by age and gender. We note two additional, specific limitations to the interview structure. The first is that members of the dyads were not asked if they knew what influenced the other person's decision making. Therefore, we may be misestimating the degree of agreement within dyads. Second, we may have underestimated consideration of specific side‐effects because, for ethical reasons, we did not tell participants about any side‐effects they did not mention. Our study also does not reveal whether physicians provide similar information to parents and adolescents, especially regarding such side‐effects. We also do not have information on other participants in the decision, such as the other parent or extended family. In the future, prospective methods should be used to determine the information presented to each participant and to further elucidate the decision‐making process by gathering information on clinical interactions, as well as decision‐making steps that occur outside of such encounters. Although our study was conducted at a single institution and not intended to be generalizable, we believe that these parent and adolescent participants are not dissimilar to others with chronic conditions. Other research has shown that adolescents with diverse conditions have similar health‐care preferences.42 As such, this study may help generate hypotheses for future quantitative work or research about decision making in other paediatric chronic conditions.
Despite the limitations, the use of paired parent–adolescent data about a real‐life treatment decision is a key step towards understanding decision making and developing interventions to improve the decision process for families of adolescents with chronic conditions. Although paediatric medical decision making typically involves a patient–provider–parent triad,43 most studies have considered only one viewpoint. If decision support is to be as successful in paediatrics as it has been in adult medicine,44 all members of the triad must be considered. Our results suggest that parents and adolescents consider the same categories of information when making treatment decisions but may have different perspectives. Moreover, no single factor dominated either parents’ or adolescents’ decision making, suggesting the need for customizable interventions that address the developmentally appropriate differences in parents’ and adolescent's information needs and desires. Fully engaging both parents and adolescents in the decision process will require the ability to provide for the needs of all parties and to assist them in communicating, not only with the health‐care provider, but also with each other.
Sources of funding
This work was supported by an Academic Pediatric Association Young Investigator Award to Dr. Ellen Lipstein.
Conflicts of interest
Dr. Lovell has served as a consultant for study trial design or principal investigator for trials with multiple manufacturers of biologics, including TNFα inhibitors (Centocor, Inc.; Wyeth Pharmaceuticals; Bristol‐Myers Squibb; Regeneron; Abbott; Amgen; Hoffman‐La Roche, Inc.; UBS; Novartis; Xoma Inc.). He is also on the speakers’ bureau for Genentech. The other authors have indicated that they have no financial relationships relevant to this article to disclose.
Supporting information
Table S1. Number of dyads or individuals who considered each category of decision factors.
References
- 1. Brinkman WB, Sherman SN, Zmitrovich AR et al Parental angst making and revisiting decisions about treatment of attention‐deficit/hyperactivity disorder. Pediatrics, 2009; 124: 580–589. [DOI] [PubMed] [Google Scholar]
- 2. Daniel E, Kent G, Binney V, Pagdin J. Trying to do my best as a mother: decision‐making in families of children undergoing elective surgical treatment for short stature. British Journal of Health Psychology, 2005; 10(Pt 1): 101–114. [DOI] [PubMed] [Google Scholar]
- 3. Whitney SN, Ethier AM, Fruge E, Berg S, McCullough LB, Hockenberry M. Decision making in pediatric oncology: who should take the lead? The decisional priority in pediatric oncology model. Journal of Clinical Oncology, 2006; 24: 160–165. [DOI] [PubMed] [Google Scholar]
- 4. Merenstein D, Diener‐West M, Krist A, Pinneger M, Cooper LA. An assessment of the shared‐decision model in parents of children with acute otitis media. Pediatrics, 2005; 116: 1267–1275. [DOI] [PubMed] [Google Scholar]
- 5. Watt S. Clinical decision‐making in the context of chronic illness. Health Expectations, 2000; 3: 6–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Montori VM, Gafni A, Charles C. A shared treatment decision‐making approach between patients with chronic conditions and their clinicians: the case of diabetes. Health Expectations, 2006; 9: 25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Winterbottom A, Bekker HL, Conner M, Mooney A. Choosing dialysis modality: decision making in a chronic illness context. Health Expectations, 2012; doi: 10.1111/j.1369‐7625.2012.00798.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stubblefield C, Mutha S. Provider‐patient roles in chronic disease management. Journal of Allied Health, 2002. Summer; 31: 87–92. [PubMed] [Google Scholar]
- 9. Gruccio D, Steinkrauss L. Challenges of decision making for families of children with single or multiple chronic conditions. Nurse Practitioner Forum, 2000; 11: 15–19. [PubMed] [Google Scholar]
- 10. Angst DB, Deatrick JA. Involvement in health care decisions: parents and children with chronic illness. Journal of Family Nursing, 1996; 2: 174–194. [Google Scholar]
- 11. Knopf JM, Hornung RW, Slap GB, DeVellis RF, Britto MT. Views of treatment decision making from adolescents with chronic illnesses and their parents: a pilot study. Health Expectations, 2008; 11: 343–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Miller VA, Drotar D. Discrepancies between mother and adolescent perceptions of diabetes‐related decision‐making autonomy and their relationship to diabetes‐related conflict and adherence to treatment. Journal of Pediatric Psychology, 2003; 28: 265–274. [DOI] [PubMed] [Google Scholar]
- 13. Miller VA. Parent‐child collaborative decision making for the management of chronic illness: a qualitative analysis. Families, Systems, & Health, 2009; 27: 249–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lyon ME, McCabe MA, Patel KM, D'Angelo LJ. What do adolescents want? An exploratory study regarding end‐of‐life decision‐making. Journal of Adolescent Health, 2004; 35: 529 e1–6. [DOI] [PubMed] [Google Scholar]
- 15. Beresford BA, Sloper P. Chronically ill adolescents’ experiences of communicating with doctors: a qualitative study. Journal of Adolescent Health, 2003; 33: 172–179. [DOI] [PubMed] [Google Scholar]
- 16. Dunsmore J, Quine S. Information, support, and decision‐making needs and preferences of adolescents with cancer: implications for health professionals. Journal of Psychosocial Oncology, 1995; 13: 39–56. [Google Scholar]
- 17. Hoentjen F, van Bodegraven AA. Safety of anti‐tumor necrosis factor therapy in inflammatory bowel disease. World Journal of Gastroenterology, 2009; 15: 2067–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Diak P, Siegel J, La Grenade L, Choi L, Lemery S, McMahon A. Tumor necrosis factor alpha blockers and malignancy in children: forty‐eight cases reported to the Food and Drug Administration. Arthritis and Rheumatism, 2010; 62: 2517–2524. [DOI] [PubMed] [Google Scholar]
- 19. Lipstein EA, Lovell DJ, Denson LA et al Parents’ information needs in tumor necrosis factor‐alpha inhibitor treatment decisions. Journal of Pediatric Gastroenterology and Nutrition, 2013; 56: 244–250. [DOI] [PubMed] [Google Scholar]
- 20. Patton MQ. Qualitative Evaluation and Research Methods, 2nd edn Newbury Park, CA: Sage Publications, 1990: 532 pp. [Google Scholar]
- 21. Lipstein EA, Muething KA, Dodds CM, Britto MT. ‘I'm the One Taking It’: adolescent participation in chronic disease treatment decisions. Journal of Adolescent Health, 2013; 53: 253–259. [DOI] [PubMed] [Google Scholar]
- 22. Davison BJ, Gleave ME, Goldenberg SL, Degner LF, Hoffart D, Berkowitz J. Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nursing, 2002; 25: 42–49. [DOI] [PubMed] [Google Scholar]
- 23. Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Archives of Internal Medicine, 1996; 156: 1414–1420. [PubMed] [Google Scholar]
- 24. Goore Z, Mangione‐Smith R, Elliott MN, McDonald L, Kravitz RL. How much explanation is enough? A study of parent requests for information and physician responses. Ambulatory Pediatrics, 2001; 1: 326–332. [DOI] [PubMed] [Google Scholar]
- 25. Guerriere DN, McKeever P, Llewellyn‐Thomas H, Berall G. Mothers’ decisions about gastrostomy tube insertion in children: factors contributing to uncertainty. Developmental Medicine and Child Neurology, 2003; 45: 470–476. [DOI] [PubMed] [Google Scholar]
- 26. Hummelinck A, Pollock K. Parents’ information needs about the treatment of their chronically ill child: a qualitative study. Patient Education and Counseling, 2006; 62: 228–234. [DOI] [PubMed] [Google Scholar]
- 27. Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health Expectations, 2008; 11: 232–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lambert SD, Loiselle CG. Health information seeking behavior. Qualitative Health Research, 2007; 17: 1006–1019. [DOI] [PubMed] [Google Scholar]
- 29. Vogel BA, Bengel J, Helmes AW. Information and decision making: patients’ needs and experiences in the course of breast cancer treatment. Patient Education and Counseling, 2008; 71: 79–85. [DOI] [PubMed] [Google Scholar]
- 30. Pope C, Mays N (eds). Qualitative Research in Health Care, 3rd edn Malden: Blackwell Publishing, 2006. [Google Scholar]
- 31. Sandelowski M. Whatever happened to qualitative description? Research in Nursing & Health, 2000; 23: 334–340. [DOI] [PubMed] [Google Scholar]
- 32. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research, 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 33. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook, 2nd edn Thousand Oaks: Sage Publications, 1994: xiv, 338 pp. [Google Scholar]
- 34. Hankins J, Hinds P, Day S et al Therapy preference and decision‐making among patients with severe sickle cell anemia and their families. Pediatric Blood & Cancer, 2007; 48: 705–710. [DOI] [PubMed] [Google Scholar]
- 35. McAnarney ER. Textbook of Adolescent Medicine. Philadelphia: W.B. Saunders, 1992: xlii, 1227 pp. [Google Scholar]
- 36. Nurmi JE. How do adolescents see their future – a review of the development of future orientation and planning. Developmental Review, 1991; 11: 1–59. [Google Scholar]
- 37. Young B, Dixon‐Woods M, Windridge KC, Heney D. Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. BMJ, 2003; 326: 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Young B, Moffett JK, Jackson D, McNulty A. Decision‐making in community‐based paediatric physiotherapy: a qualitative study of children, parents and practitioners. Health and Social Care in the Community, 2006; 14: 116–124. [DOI] [PubMed] [Google Scholar]
- 39. Gotz I, Labenbacher I, Eichler I, Wojnarowski C, Gotz M. Health‐independent lung transplantation information of parents of children with cystic fibrosis. Transplantation, 1997; 64: 742–747. [DOI] [PubMed] [Google Scholar]
- 40. Kuther TL. Medical decision‐making and minors: issues of consent and assent. Adolescence, 2003. Summer; 38: 343–358. [PubMed] [Google Scholar]
- 41. Lange PAMV, Kruglanski AW, Higgins ET. Handbook of Theories of Social Psychology. Los Angeles: SAGE, 2012. [Google Scholar]
- 42. Jedeloo S, van Staa A, Latour JM, van Exel NJ. Preferences for health care and self‐management among Dutch adolescents with chronic conditions: a Q‐methodological investigation. International Journal of Nursing Studies, 2010; 47: 593–603. [DOI] [PubMed] [Google Scholar]
- 43. Gabe J, Olumide G, Bury M. ‘It takes three to tango’: a framework for understanding patient partnership in paediatric clinics. Social Science and Medicine, 2004; 59: 1071–1079. [DOI] [PubMed] [Google Scholar]
- 44. Stacey D, Legare F, Col NF et al Decision aids for people facing health treatment or screening decisions. Cochrane Database Systematic Review, 2014; 1: CD001431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Number of dyads or individuals who considered each category of decision factors.


