Abstract
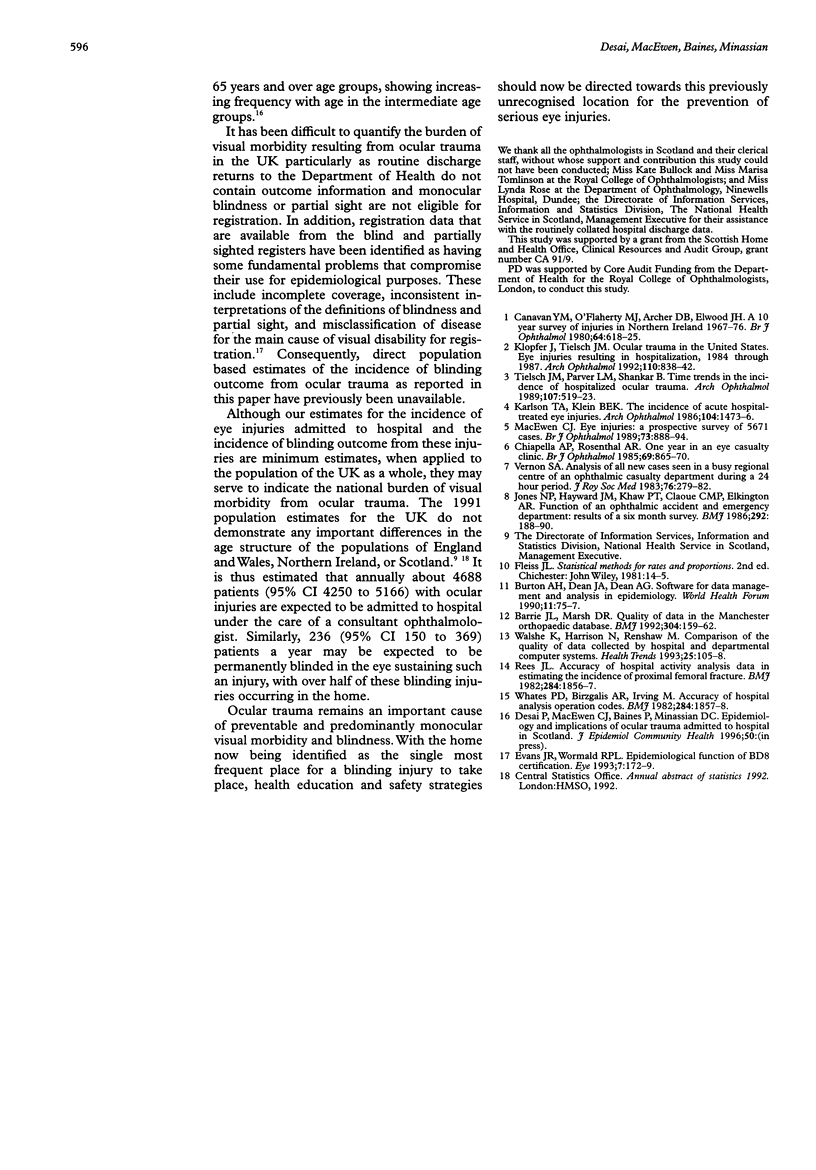
AIMS: To provide epidemiological data on the current burden of serious eye injuries utilising the hospital eye service, to inform the planning and provision of eye health care, and health and safety strategies for the prevention of ocular injuries. METHODS: A prospective observational study was carried out of all patients with ocular trauma admitted to hospitals in Scotland, under the care of a consultant ophthalmologist, during a 1 year period. The population of Scotland represented the population at risk of injury. Visual outcome (Snellen visual acuity in the injured eye) was measured at the time of final discharge from ophthalmic care and at follow up. RESULTS: All ophthalmic departments in Scotland participated and a total of 415 residents of Scotland were admitted. The 1 year cumulative incidence of ocular trauma necessitating admission to hospital is estimated to be 8.14 per 100 000 population (95% CI 7.38 to 8.97). Some 13.2% (n = 26/197) of patients discharged from follow up had a poor visual outcome with a visual acuity less than 6/12 in the injured eye. Some 10.7% (21/197) patients at this time had a blinding outcome in the injured eye (visual acuity less than 6/60). No patient was registered blind or partially sighted during the study period. The home was the single most frequent place for blinding injuries to occur (52%, n = 11/21), followed by the workplace 24% (n = 5/21). The 1 year cumulative incidence of blinding outcome from serious ocular trauma is estimated to be 0.41 per 100 000 population per year (95% CI 0.26 to 0.64). CONCLUSION: The current burden of serious ocular trauma presenting to the hospital eye service has been quantified from this population based study, and for the first time, a direct estimate of the incidence of the subsequent blinding outcome from these injuries has been provided. Ocular trauma remains an important cause of avoidable and, predominantly, monocular visual morbidity (visual impairment and blindness), with over half of the blinding injuries now occurring in the home. Health education and safety strategies should now consider targeting the home for the prevention of the serious eye injuries in addition to the traditional work, sports, and leisure environments and their related activities.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barrie J. L., Marsh D. R. Quality of data in the Manchester orthopaedic database. BMJ. 1992 Jan 18;304(6820):159–162. doi: 10.1136/bmj.304.6820.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton A. H., Dean J. A., Dean A. G. Software for data management and analysis in epidemiology. World Health Forum. 1990;11(1):75–77. [PubMed] [Google Scholar]
- Canavan Y. M., O'Flaherty M. J., Archer D. B., Elwood J. H. A 10-year survey of eye injuries in Northern Ireland, 1967-76. Br J Ophthalmol. 1980 Aug;64(8):618–625. doi: 10.1136/bjo.64.8.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiapella A. P., Rosenthal A. R. One year in an eye casualty clinic. Br J Ophthalmol. 1985 Nov;69(11):865–870. doi: 10.1136/bjo.69.11.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J. R., Wormald R. P. Epidemiological function of BD8 certification. Eye (Lond) 1993;7(Pt 1):172–179. doi: 10.1038/eye.1993.37. [DOI] [PubMed] [Google Scholar]
- Jones N. P., Hayward J. M., Khaw P. T., Claoué C. M., Elkington A. R. Function of an ophthalmic "accident and emergency" department: results of a six month survey. Br Med J (Clin Res Ed) 1986 Jan 18;292(6514):188–190. doi: 10.1136/bmj.292.6514.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlson T. A., Klein B. E. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol. 1986 Oct;104(10):1473–1476. doi: 10.1001/archopht.1986.01050220067028. [DOI] [PubMed] [Google Scholar]
- Klopfer J., Tielsch J. M., Vitale S., See L. C., Canner J. K. Ocular trauma in the United States. Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol. 1992 Jun;110(6):838–842. doi: 10.1001/archopht.1992.01080180110037. [DOI] [PubMed] [Google Scholar]
- Macewen C. J. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989 Nov;73(11):888–894. doi: 10.1136/bjo.73.11.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees J. L. Accuracy of hospital activity analysis data in estimating the incidence of proximal femoral fracture. Br Med J (Clin Res Ed) 1982 Jun 19;284(6332):1856–1857. doi: 10.1136/bmj.284.6332.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tielsch J. M., Parver L., Shankar B. Time trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol. 1989 Apr;107(4):519–523. doi: 10.1001/archopht.1989.01070010533025. [DOI] [PubMed] [Google Scholar]
- Vernon S. A. Analysis of all new cases seen in a busy regional centre ophthalmic casualty department during 24-week period. J R Soc Med. 1983 Apr;76(4):279–282. doi: 10.1177/014107688307600408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walshe K., Harrison N., Renshaw M. Comparison of the quality of patient data collected by hospital and departmental computer systems. Health Trends. 1993;25(3):105–108. [PubMed] [Google Scholar]
- Whates P. D., Birzgalis A. R., Irving M. Accuracy of hospital activity analysis operation codes. Br Med J (Clin Res Ed) 1982 Jun 19;284(6332):1857–1858. doi: 10.1136/bmj.284.6332.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]


