Abstract
Background:
The coexistence of chronic mental health conditions with somatic conditions (somatic–mental multimorbidity, or SMM) is common and has been associated with greater symptom burden and functional impairment, higher costs, and excess mortality. However, most existing literature focused on the co-occurrence of an index mental health condition with specific additional conditions. By contrast, we studied the prevalence and patterns of SMM more broadly considering 19 selected conditions, and we focused on differences by age, sex, and race/ethnicity.
Methods:
The Rochester Epidemiology Project (REP) records-linkage system was used to identify all residents of Olmsted County, MN, on April 1, 2010. We identified individuals with each of 19 common chronic conditions, including 5 mental health conditions, using the International Classification of Diseases, ninth revision (ICD-9) codes received from any health care provider between April 1, 2005 and March 31, 2010.
Results:
Among the 138,858 residents of the county, 52.4% were women, and 7.9% had SMM. SMM increased steeply with older age, was 1.7 times more common in women, and was lower in Asians compared with whites. Of the 10,903 persons with SMM, 7,739 (71.0%) were younger than 65 years. Depressive and anxiety disorders were the most common conditions involved in SMM. The dyads that were observed more frequently or less frequently than expected by chance varied in composition by age and sex.
Conclusions:
SMM that reaches medical attention is highly prevalent across all age groups, is more frequent in women, is less frequent in Asians, and encompasses a wide range of conditions.
Keywords: Somatic multimorbidity, Mental health multimorbidity, Age, Sex, Race/ethnicity
Mental health conditions often coexist with chronic somatic conditions (1–4), leading to multimorbidity that includes mental health conditions (somatic–mental multimorbidity; SMM). SMM has been associated with greater symptom burden and functional impairment, poorer quality of life, higher costs, and excess mortality (5,6). Although the prevalence of SMM is high and increasing in clinical practice (7,8), health care programs and clinical research have traditionally focused on individual conditions considered in isolation, or on the co-occurrence of specific comorbid conditions with an index medical or mental health condition, particularly in older adults (9,10). Few studies have examined the prevalence and the patterns of co-occurrence of mental health conditions with a broader range of chronic somatic conditions across the entire life span and using medical record data (11–13). Therefore, we studied the prevalence and patterns of SMM by age, sex, and race/ethnicity across the entire life span in a geographically defined U.S. population.
Methods
Study Population
We used the medical records-linkage system of the Rochester Epidemiology Project (REP) to identify all persons who resided in Olmsted County, MN, on April 1, 2010; however, we excluded those who had not given permission to use their medical records for research (<3% of the overall population). Extensive details about the REP and the study population were reported elsewhere (we included 138,858 people) (14). The study was approved by the Mayo Clinic and the Olmsted Medical Center Institutional Review Boards.
Definition of Chronic Conditions
The diagnostic indices of the REP were searched electronically for all International Classification of Diseases, ninth revision (ICD-9) codes that each person in the Olmsted County population received from any health care institution from April 1, 2005 through March 31, 2010. These ICD-9 codes were used to define the 20 chronic conditions recommended by the U.S. Department of Health and Human Services (DHHS) to study multimorbidity (15–19). However, we modified the list by removing HIV infections and autism spectrum disorders because their frequency was low in the overall population (18). We also added anxiety disorders because they are common across all age strata in the general U.S. population and in primary care practices (20). Our definition of anxiety disorders was based on the ICD-9 codes used in the Medical Expenditure Panel Survey (MEPS) (16,21). The condition labeled “schizophrenia” included other psychoses. Therefore, we considered a total of 19 selected conditions, including 5 mental health conditions. All conditions were defined as chronic and common (15). Supplementary Table 1 provides the list of the 19 conditions used in this study, their abbreviations, and their corresponding ICD-9 codes.
To enhance diagnostic accuracy, only persons who received at least two diagnostic codes for a given condition separated by more than 30 days were considered to have that particular condition (18). We defined general multimorbidity as the presence of 2 or more of the 19 conditions in the 5 years before the prevalence date (April 1, 2010). Similarly, we defined SMM as any combination of two or more conditions in which at least one condition was somatic and at least one condition was mental.
Statistical Analyses for Prevalence
We computed the age-, sex-, and race/ethnicity-specific prevalence of general multimorbidity and of SMM. The prevalence was directly standardized to the total U.S. population by age using the 2010U.S. census data (when appropriate for internal comparison across groups). The prevalence was also directly standardized to the total U.S. population by age, sex, and race/ethnicity to facilitate comparisons with other studies. Because this study covered the target population completely, and no sampling was involved, confidence intervals were not included in the tables and the figures related to prevalence (18). The age- and sex-specific prevalences of the individual chronic somatic and mental health conditions were reported elsewhere (18).
Case–Control Analyses
We formally tested the association of age, sex, and race/ethnicity with prevalent SMM using cross-sectional case–control analyses. These analyses compared persons who had SMM (cases) to persons who had other types of multimorbidity (somatic–somatic or mental–mental; controls). For each association, we computed an odds ratio, a 95% confidence interval, and a two-sided p value with alpha at .05. Analyses were adjusted by age (seven age groups), sex, and race/ethnicity (four groups), when applicable. In addition, we tested the association of increasing number of mental health conditions with the prevalence of one or more somatic health conditions, and conversely, the association of increasing number of somatic health conditions with the prevalence of one or more mental health conditions. For these dose–effect analyses, each condition was given the same weight (simple counts).
Heat Maps for Co-occurrence of Conditions
We developed a series of heat maps stratified by age and sex to display the absolute frequencies of specific somatic–mental health dyads. Hotter colors (darker orange) correspond with a higher prevalence of a dyad. We also developed a second series of heat maps to show the observed-to-expected ratios (OERs) for each somatic–mental health dyad, accounting for age in single-year increments. We only displayed OERs for dyads that occurred in five or more persons and that reached statistical significance. These ratios can be interpreted as cross-sectional measures of association. Dyads that were observed more frequently than expected are shown in shades of orange (OER > 1.0). Dyads that were observed less frequently than expected are shown in shades of purple (OER < 1.0). OERs were calculated based on the assumption that the occurrence of the two chronic conditions was independent. These heat maps were developed to explore SMM patterns and to suggest hypotheses; therefore, concerns about multiple comparisons do not apply. Only persons aged ≥ 20 years were included in the heat maps because the prevalence of multimorbidity before age 20 years was low. All analyses were performed using SAS version 9.3.
Results
Prevalence of SMM
The mean number of conditions, the prevalence of general multimorbidity, and the prevalence of SMM in the 138,858 people included in the study are presented in Table 1. The mean number of conditions was higher among persons aged ≥ 65 years than in persons aged < 65 years for both men (5.6 times higher) and women (4.9 times higher). The prevalence of SMM was also higher among persons aged ≥ 65 years than in persons aged < 65 years for both men (2.8 times higher) and women (2.7 times higher). However, the absolute number of individuals with SMM was higher among persons aged < 65 years than in persons aged ≥ 65 years for both men (2.7 times higher) and women (2.3 times higher). These differences in absolute numbers in younger versus older persons were greater for SMM than for general multimorbidity.
Table 1.
Mean Number of Chronic Conditions and Prevalence (per 100 people) of General and Somatic–Mental Health Multimorbidity by Age, Sex, and Race/Ethnicity
| Age (y) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Total Population | Number of Conditions, Mean (SD) | Multimorbidity Prevalencea | Total Population | Number of Conditions, Mean (SD) | Multimorbidity Prevalencea | |||
| General, n (%) | Somatic– Mental, n (%) | General, n (%) | Somatic– Mental, n (%) | |||||
| All races/ethnicities | ||||||||
| 0–19 | 19,316 | 0.15 (0.43) | 372 (1.9) | 143 (0.7) | 18,709 | 0.14 (0.45) | 450 (2.4) | 177 (0.9) |
| 20–39 | 18,028 | 0.36 (0.82) | 1,586 (8.8) | 607 (3.4) | 21,051 | 0.51 (0.92) | 2,604 (12.4) | 1,289 (6.1) |
| 40–49 | 8,978 | 0.85 (1.29) | 1,984 (22.1) | 777 (8.7) | 9,650 | 0.89 (1.28) | 2,180 (22.6) | 1,144 (11.9) |
| 50–59 | 9,036 | 1.43 (1.63) | 3,526 (39.0) | 1,008 (11.2) | 9,944 | 1.41 (1.61) | 3,754 (37.8) | 1,601 (16.1) |
| 60–69 | 5,506 | 2.27 (1.94) | 3,297 (59.9) | 596 (10.8) | 6,248 | 2.22 (1.92) | 3,699 (59.2) | 1,104 (17.7) |
| 70–79 | 3,359 | 3.45 (2.19) | 2,685 (79.9) | 402 (12.0) | 3,921 | 3.28 (2.17) | 3,086 (78.7) | 699 (17.8) |
| ≥80 | 1,903 | 4.58 (2.51) | 1,674 (88.0) | 428 (22.5) | 3,209 | 4.18 (2.40) | 2,784 (86.8) | 928 (28.9) |
| 0–64 | 58,419 | 0.62 (1.19) | 9,146 (15.7) | 2,886 (4.9) | 62,838 | 0.68 (1.22) | 10,868 (17.3) | 4,853 (7.7) |
| ≥65 | 7,707 | 3.45 (2.34) | 5,978 (77.6) | 1,075 (13.9) | 9,894 | 3.35 (2.29) | 7,689 (77.7) | 2,089 (21.1) |
| All ages | 66,126 | 0.95 (1.65) | 15,124 (22.9) | 3,961 (6.0) | 72,732 | 1.05 (1.68) | 18,557 (25.5) | 6,942 (9.5) |
| Age std.b | — | — | (24.5) | (6.3) | — | — | (25.3) | (9.4) |
| Age, sex, race/ethnicity std.c | — | — | (23.2) | (6.1) | — | — | (26.7) | (9.9) |
| Blacks | ||||||||
| 0–19 | 1,535 | 0.13 (0.43) | 22 (1.4) | 9 (0.6) | 1,487 | 0.14 (0.40) | 22 (1.5) | 10 (0.7) |
| 20–39 | 1,133 | 0.33 (0.82) | 86 (7.6) | 29 (2.6) | 1,201 | 0.41 (0.84) | 118 (9.8) | 61 (5.1) |
| 40–49 | 384 | 1.04 (1.61) | 100 (26.0) | 41 (10.7) | 351 | 1.21 (1.75) | 106 (30.2) | 60 (17.1) |
| 50–59 | 262 | 1.68 (1.91) | 118 (45.0) | 36 (13.7) | 226 | 2.08 (2.08) | 121 (53.5) | 50 (22.1) |
| 60–69 | 87 | 2.00 (1.95) | 44 (50.6) | 11 (12.6) | 113 | 2.30 (1.93) | 69 (61.1) | 18 (15.9) |
| 70–79 | 48 | 3.04 (2.71) | 35 (72.9) | 7 (14.6) | 59 | 2.90 (2.61) | 38 (64.4) | 12 (20.3) |
| ≥80 | 14 | 4.14 (2.63) | 12 (85.7) | 2 (14.3) | 22 | 3.14 (2.80) | 17 (77.3) | 5 (22.7) |
| 0–64 | 3,358 | 0.45 (1.08) | 347 (10.3) | 122 (3.6) | 3,326 | 0.52 (1.17) | 407 (12.2) | 193 (5.8) |
| ≥65 | 105 | 2.85 (2.47) | 70 (66.7) | 13 (12.4) | 133 | 2.64 (2.37) | 84 (63.2) | 23 (17.3) |
| All ages | 3,463 | 0.52 (1.22) | 417 (12.0) | 135 (3.9) | 3,459 | 0.60 (1.31) | 491 (14.2) | 216 (6.2) |
| Age std.b | — | — | (24.1) | (6.7) | — | — | (26.6) | (10.4) |
| Asians | ||||||||
| 0–19 | 1,082 | 0.10 (0.34) | 9 (0.8) | 3 (0.3) | 1,095 | 0.09 (0.33) | 13 (1.2) | 3 (0.3) |
| 20–39 | 945 | 0.24 (0.61) | 49 (5.2) | 11 (1.2) | 1,254 | 0.25 (0.64) | 64 (5.1) | 31 (2.5) |
| 40–49 | 394 | 0.63 (0.98) | 64 (16.2) | 12 (3.0) | 426 | 0.51 (0.92) | 51 (12.0) | 17 (4.0) |
| 50–59 | 258 | 1.13 (1.32) | 81 (31.4) | 10 (3.9) | 317 | 1.33 (1.67) | 112 (35.3) | 37 (11.7) |
| 60–69 | 137 | 2.01 (2.02) | 69 (50.4) | 13 (9.5) | 205 | 1.87 (1.69) | 104 (50.7) | 21 (10.2) |
| 70–79 | 70 | 2.63 (2.21) | 46 (65.7) | 5 (7.1) | 107 | 3.17 (1.98) | 84 (78.5) | 21 (19.6) |
| ≥80 | 27 | 3.96 (2.89) | 21 (77.8) | 3 (11.1) | 47 | 4.11 (2.65) | 39 (83.0) | 19 (40.4) |
| 0–64 | 2,754 | 0.37 (0.87) | 239 (8.7) | 46 (1.7) | 3,207 | 0.39 (0.93) | 292 (9.1) | 101 (3.1) |
| ≥65 | 159 | 2.61 (2.32) | 100 (62.9) | 11 (6.9) | 244 | 2.95 (2.19) | 175 (71.7) | 48 (19.7) |
| All ages | 2,913 | 0.49 (1.13) | 339 (11.6) | 57 (2.0) | 3,451 | 0.57 (1.25) | 467 (13.5) | 149 (4.3) |
| Age std.b | — | — | (19.3) | (3.0) | — | — | (20.2) | (6.4) |
| Whites | ||||||||
| 0–19 | 14,781 | 0.16 (0.44) | 317 (2.1) | 122 (0.8) | 14,302 | 0.16 (0.47) | 391 (2.7) | 153 (1.1) |
| 20–39 | 14,463 | 0.39 (0.85) | 1,377 (9.5) | 548 (3.8) | 17,225 | 0.55 (0.94) | 2,326 (13.5) | 1,152 (6.7) |
| 40–49 | 7,734 | 0.86 (1.29) | 1,746 (22.6) | 688 (8.9) | 8,474 | 0.90 (1.28) | 1,956 (23.1) | 1,031 (12.2) |
| 50–59 | 8,215 | 1.44 (1.63) | 3,246 (39.5) | 935 (11.4) | 9,117 | 1.40 (1.59) | 3,433 (37.7) | 1,480 (16.2) |
| 60–69 | 5,137 | 2.30 (1.93) | 3,132 (61.0) | 566 (11.0) | 5,781 | 2.25 (1.92) | 3,462 (59.9) | 1,053 (18.2) |
| 70–79 | 3,167 | 3.49 (2.17) | 2,555 (80.7) | 382 (12.1) | 3,695 | 3.29 (2.16) | 2,921 (79.1) | 656 (17.8) |
| ≥80 | 1,839 | 4.61 (2.50) | 1,626 (88.4) | 420 (22.8) | 3,115 | 4.20 (2.39) | 2,711 (87.0) | 900 (28.9) |
| 0–64 | 48,053 | 0.67 (1.23) | 8,280 (17.2) | 2,622 (5.5) | 52,344 | 0.74 (1.25) | 9,857 (18.8) | 4,427 (8.5) |
| ≥65 | 7,283 | 3.50 (2.33) | 5,719 (78.5) | 1,039 (14.3) | 9,365 | 3.39 (2.29) | 7,343 (78.4) | 1,998 (21.3) |
| All ages | 55,336 | 1.04 (1.72) | 13,999 (25.3) | 3,661 (6.6) | 61,709 | 1.14 (1.74) | 17,200 (27.9) | 6,425 (10.4) |
| Age std.b | — | — | (25.0) | (6.6) | — | — | (25.8) | (9.7) |
Note: SD = standard deviation.
aMultimorbidity was defined as the presence of 2 or more of 19 conditions in the 5 years before April 1, 2010. Only persons who received at least two codes for a given condition separated by more than 30 days were considered prevalent. Somatic–mental multimorbidity was defined as all combinations of two or more conditions in which at least one condition was somatic and at least one condition was mental.
bThe prevalence was directly standardized to the total U.S. population by age using the 2010U.S. census data. These age-standardized prevalence figures may be used to compare across groups within our population (eg, men to women). However, they should not be used as national projections.
cThe prevalence was directly standardized to the total U.S. population by age, sex, and race/ethnicity using the 2010U.S. census data. The age-, sex-, and race/ethnicity-standardized prevalence for men and women combined was 25.0 for general multimorbidity and 8.0 for somatic–mental multimorbidity. These standardized prevalence figures may be used to facilitate comparisons with other populations.
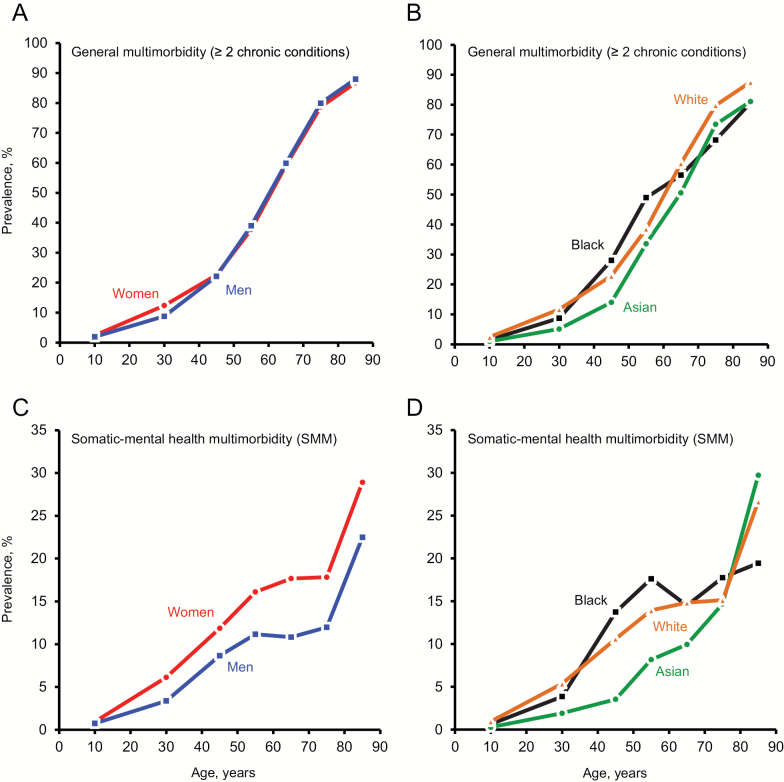
The prevalence of SMM increased steadily through age 50 years, plateaued between ages 50 and 79 years, and increased sharply thereafter in both men and women (Figure 1C). By contrast, the prevalence of general multimorbidity increased steeply with older age without an apparent plateau (Figure 1A). The prevalence of SMM was consistently higher in women than in men (Table 1 and Figure 1C), whereas the prevalence of general multimorbidity was similar for men and women (Figure 1A). A lower prevalence of SMM was observed in Asians than in other race/ethnicity groups (Table 1 and Figure 1). The prevalence was particularly low for Asian men (Table 1).
Figure 1.
Prevalence (per 100 population) of combinations of 2 or more of the 19 chronic conditions (general multimorbidity) by sex (panel A) and by race/ethnicity (panel B). Prevalence of somatic–mental multimorbidity (SMM) by sex (panel C) and by race/ethnicity (panel D).
Case–Control Analyses
Table 2 shows the association of age, sex, and race/ethnicity with prevalent SMM compared with somatic–somatic multimorbidity or mental–mental multimorbidity considered combined (cross-sectional case–control analyses). Women were at significantly higher risk of SMM than men. For both men and women, persons younger than the referent group of 50–59 years were at significantly increased risk of SMM, whereas those who were ≥ 60 years old were at significantly lower risk. Asian race/ethnicity was associated with significantly lower risk of SMM as compared with white race/ethnicity; however, no other statistically significant race/ethnicity differences were observed. Supplementary Table 2 shows the corresponding case–control analyses comparing SMM to somatic–somatic multimorbidity and to mental–mental multimorbidity considered separately.
Table 2.
Case–Control Study of Somatic–Mental Multimorbidity (SMM; Cases) Versus Other Types of Multimorbidity (Somatic–Somatic and Mental–Mental; Controls)
| Characteristic | Cases With SMM, n (%) | Controls With Other Multimorbidity, n (%) | OR (95% CI)a | p Value |
|---|---|---|---|---|
| Sexb | ||||
| Men | 3,961 (36.3) | 11,163 (49.0) | 1.00 (reference) | — |
| Women | 6,942 (63.7) | 11,615 (51.0) | 1.70 (1.62–1.78) | <.001 |
| Men | ||||
| Age group (y)c | ||||
| 0–19 | 143 (3.6) | 229 (2.1) | 1.56 (1.25–1.95) | <.001 |
| 20–39 | 607 (15.3) | 979 (8.8) | 1.56 (1.38–1.77) | <.001 |
| 40–49 | 777 (19.6) | 1,207 (10.8) | 1.62 (1.44–1.82) | <.001 |
| 50–59 | 1,008 (25.4) | 2,518 (22.6) | 1.00 (reference) | — |
| 60–69 | 596 (15.0) | 2,701 (24.2) | 0.55 (0.49–0.62) | <.001 |
| 70–79 | 402 (10.1) | 2,283 (20.5) | 0.44 (0.39–0.50) | <.001 |
| ≥80 | 428 (10.8) | 1,246 (11.2) | 0.85 (0.75–0.97) | .02 |
| Race/ethnicityd | ||||
| White | 3,661 (92.4) | 10,338 (92.6) | 1.00 (reference) | — |
| Black | 135 (3.4) | 282 (2.5) | 1.04 (0.84–1.28) | .75 |
| Asian | 57 (1.4) | 282 (2.5) | 0.50 (0.37–0.67) | <.001 |
| Othere | 108 (2.7) | 261 (2.3) | 0.95 (0.76–1.21) | .70 |
| Women | ||||
| Age group (y)c | ||||
| 0–19 | 177 (2.5) | 273 (2.4) | 0.88 (0.72–1.07) | .19 |
| 20–39 | 1,289 (18.6) | 1,315 (11.3) | 1.32 (1.19–1.46) | <.001 |
| 40–49 | 1,144 (16.5) | 1,036 (8.9) | 1.48 (1.33–1.65) | <.001 |
| 50–59 | 1,601 (23.1) | 2,153 (18.5) | 1.00 (reference) | — |
| 60–69 | 1,104 (15.9) | 2,595 (22.3) | 0.57 (0.52–0.63) | <.001 |
| 70–79 | 699 (10.1) | 2,387 (20.6) | 0.39 (0.35–0.44) | <.001 |
| ≥80 | 928 (13.4) | 1,856 (16.0) | 0.67 (0.60–0.74) | <.001 |
| Race/ethnicityd | ||||
| White | 6,425 (92.6) | 10,775 (92.8) | 1.00 (reference) | — |
| Black | 216 (3.1) | 275 (2.4) | 1.05 (0.87–1.27) | .60 |
| Asian | 149 (2.1) | 318 (2.7) | 0.77 (0.63–0.94) | .01 |
| Othere | 152 (2.2) | 247 (2.1) | 0.87 (0.70–1.07) | .18 |
Note: CI = confidence interval; OR = odds ratio.
aORs and 95% CIs adjusted by age, sex, and race/ethnicity (as applicable).
bORs adjusted by age (seven groups) and race/ethnicity (four groups).
cORs adjusted by race/ethnicity (four groups).
dORs adjusted by age (seven groups).
e“Other” included persons of unknown race/ethnicity and persons other than white, black, and Asian.
We also studied the association between the number of mental health conditions and the risk of somatic conditions for men and women separately in two broad age groups. Similarly, we studied the association between the number of somatic conditions and the risk of mental health conditions for men and women separately in two broad age groups. In both the younger and the older age groups, and for both men and women, there was a dose–effect trend in the association between increasing number of mental health conditions and the risk of at least one somatic condition, and between increasing number of somatic conditions and the risk of at least one mental health condition (data not shown).
Heat Maps for Co-occurrence of Conditions
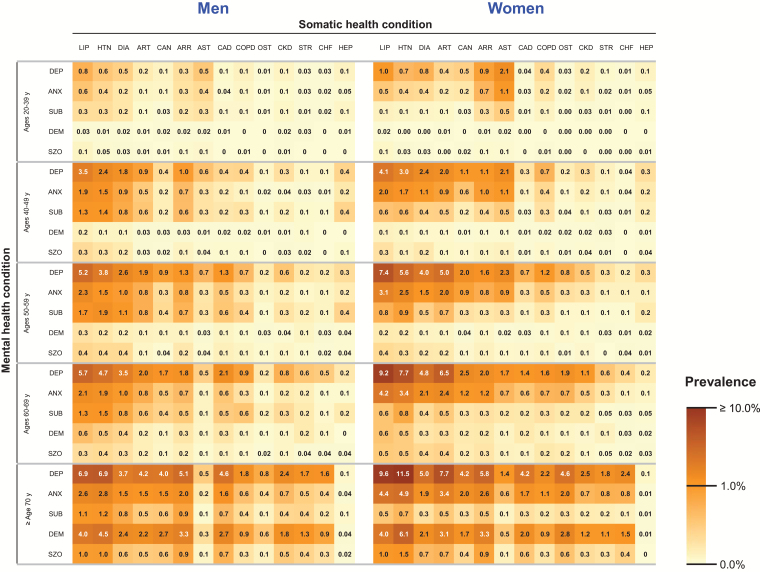
Figure 2 shows a series of heat maps representing the co-occurrence of conditions in terms of absolute frequency, stratified by age and sex. Among mental health conditions, depression was the most common condition involved in SMM for both men and women, and in all age groups. Overall, the most common somatic conditions co-occurring with depression were hyperlipidemia, hypertension, diabetes, cardiac arrhythmias, and arthritis. Depression co-occurred frequently with asthma in the 20- to 39-year-old age group, particularly among women. As expected, dyads that included depression and cancer, coronary artery disease, and chronic kidney diseases were more common among persons ≥ 70 years of age than in younger age groups.
Figure 2.
Heat maps of the prevalence of somatic–mental multimorbidity dyads (number of dyads per 100 population) stratified by age and sex. The value in each square is the percentage of co-occurrence in the population (prevalence of a given dyad). The 5 mental health conditions are presented in rows, and the 14 somatic health conditions are presented in columns; the color scale is shown on the right. The definitions of acronyms or abbreviations are: ANX = anxiety disorders; ARR = cardiac arrhythmias; ART = arthritis; AST = asthma; CAD = coronary artery disease; CAN = cancer; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; CKD = chronic kidney disease; DEM = dementia and cognitive disorders; DEP = depressive disorders; DIA = diabetes; HEP = hepatitis; HTN = hypertension; LIP = hyperlipidemia; OST = osteoporosis; STR = stroke; SUB = substance abuse disorders; SZO = schizophrenia.
Anxiety and substance use disorders were the second and third most common mental health conditions involved in SMM after depression in both men and women, particularly in the younger age groups. However, in the oldest age group, dementia and cognitive disorders were the second most common mental health condition (after depression) in both men and women. Although the overall patterns of somatic–mental health dyads were similar in men and women, women had more dyads including anxiety and somatic health conditions.
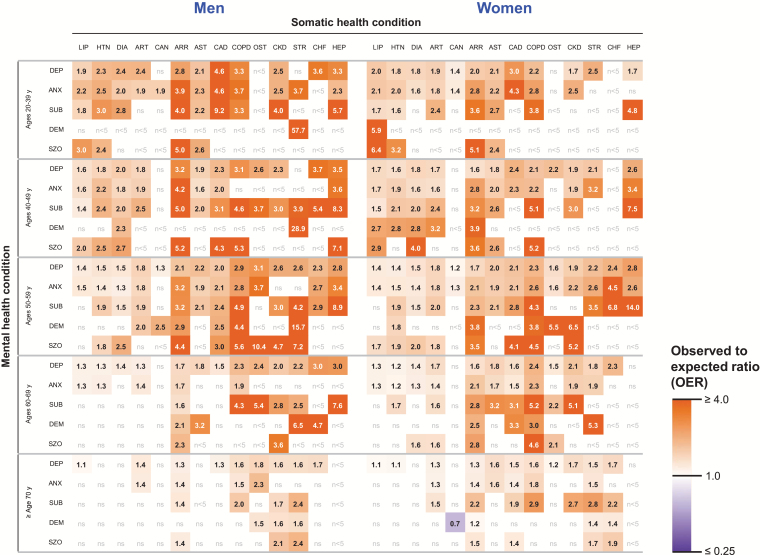
Figure 3 shows a series of heat maps of OERs for each somatic–mental health dyad, assuming independent probabilities, stratified by age and sex. Both depression and anxiety disorders were associated with hyperlipidemia, hypertension, diabetes, arthritis, arrhythmias, asthma, coronary artery disease, and chronic obstructive pulmonary disease in the younger age groups. In general, these associations became weaker with increasing age and were stronger in men than in women especially in the younger age groups. Substance use disorders were associated with hepatitis, chronic obstructive pulmonary disease, and arrhythmias in both men and women in most age groups, and with coronary artery disease in younger men (20–59 years) and in older women (50+ years). Dementia and cognitive disorders were associated with stroke in men of all ages and in older women. By contrast, dementia and cognitive disorders co-occurred with cancer less frequently than expected in women (purple square). Schizophrenia was associated with arrhythmias in both men and women in most age groups.
Figure 3.
Heat maps of a risk ratio obtained by dividing the observed frequency of each pair of conditions by the frequency expected assuming independent probabilities stratified by age and sex (observed-to-expected ratios; OERs). We only displayed OERs for dyads that occurred in five or more persons and that reached statistical significance. The hotter colors (orange) correspond to higher frequencies of co-occurrence than expected, whereas the cooler colors (purple) correspond to lower frequencies than expected. The 5 mental health conditions are presented in rows, and the 14 somatic health conditions are presented in columns; the color scale is shown on the right. The definitions of acronyms or abbreviations are: ANX = anxiety disorders; ARR = cardiac arrhythmias; ART = arthritis; AST = asthma; CAD = coronary artery disease; CAN = cancer; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; CKD = chronic kidney disease; DEM = dementia and cognitive disorders; DEP = depressive disorders; DIA = diabetes; HEP = hepatitis; HTN= hypertension; LIP = hyperlipidemia; OST = osteoporosis; STR = stroke; SUB = substance abuse disorders; SZO = schizophrenia. N < 5 = the dyad was present in fewer than five patients. ns = the OER was not statistically significant.
Discussion
Discussion of Principal Findings
In this U.S. population-based study, SMM was common, it was 1.7 times higher in women than men, and it increased with older age with an apparent plateau between ages 50 to 79 years. By contrast, the prevalence of general multimorbidity increased in a linear fashion with older age. Sex differences were greater for SMM than for general multimorbidity. The absolute number of persons affected by SMM was substantially higher in persons < 65 years of age than in persons 65 years old or older; however, we did not assess the severity of the conditions or their functional consequences. Compared with persons with somatic–somatic or mental–mental multimorbidity, SMM was significantly associated with sex (higher prevalence in women), with race/ethnicity (lower prevalence in Asians), and with age (higher prevalence in younger persons). The composition of the most common somatic–mental health dyads varied only slightly between men and women; however, women had higher frequencies of somatic–mental health dyads.
The dyads that were observed more frequently or less frequently than expected by chance varied in composition by age and sex. It is not clear whether the associated conditions are causally related, contribute to the pathophysiology of each other, share common etiologic factors, or contribute to poorer outcomes of each other leading to increased detection and diagnosis. Future examination of these potential relationships is necessary. The sex and gender differences may reflect biological differences (eg, chromosomal or hormonal differences) or social and cultural differences such as higher rates of recognition of psychiatric conditions in women than men (gender-related factors) (12). There may be sex or gender differences in the risk of somatic or mental health conditions, in the clinical presentation of common mental health conditions, or in care-seeking behavior leading to differential detection (11). We also explored patterns of SMM across race/ethnicity groups considering race/ethnicity either as a potential risk factor or simply as a risk marker. For example, the lower SMM rates in Asians deserve further study to determine whether the differences are biological (eg, due to susceptibility genes) or related to cultural factors (eg, socioeconomic status, access to medical care, or racial discrimination) (22,23).
Comparison With Previous Studies
Our findings for both general multimorbidity and SMM are consistent with previously published work. For example, in a systematic review of 39 studies (including 6 conducted in the United States), general multimorbidity was common (with prevalence estimates in nearly all reports exceeding 20%), increased with age, and was more frequent in women (11). This review also emphasized the frequent associations between depression and a variety of somatic conditions including asthma, diabetes, and hypertension (11). Others studies have shown high rates of co-occurrence between mental health conditions (major depression, anxiety disorders, and other mental health problems) and neurological diseases, pain syndromes, asthma, chronic obstructive pulmonary disease, thyroid disease, obesity, gastroesophageal reflux disease, malignancies, and serious chronic infectious diseases (4,24–28).
The observed trends of increasing prevalence of somatic conditions with increasing number of mental health conditions, and of increasing prevalence of mental health conditions with increasing number of somatic conditions, are also consistent with prior studies (12,29–31). However, most previous studies focused on the co-occurrence of depression with several somatic conditions in middle-aged and older individuals (11). By contrast, in our study, depression was also highly comorbid with asthma, arrhythmias, and lipid disorders in cohort members as young as 20–39 years, an age group infrequently included in multimorbidity research. We emphasize the need to extend multimorbidity studies into younger age groups.
Patterns of multimorbidity involving anxiety disorders are less well-studied than those associated with depression, even though anxiety disorders are the most prevalent class of mental disorders and are frequently encountered in primary care settings, where most multimorbidity is identified and managed (20). We found similar patterns of co-occurring somatic conditions associated with anxiety disorders as we did for depression in men and women of all age groups. These results are broadly consistent with other studies showing a high frequency of co-occurring chronic pain, diabetes, cardiovascular and respiratory conditions, and vestibular and gastrointestinal problems with anxiety disorders (32,33).
Strengths and Limitations
A first strength of our study was the access to medical record data for the full spectrum of primary through tertiary care based on billing codes of all conditions for a geographically defined population. The population studied included all age, sex, and race/ethnicity groups regardless of socioeconomic status, insurance status, and health care delivery setting (14). Second, 18 of the 19 health conditions (with the exception of anxiety disorders) were chosen by the DHHS as high public health priorities for the nation (15). The chronic health conditions defined by DHHS have been used by other investigators to assess general multimorbidity patterns in nationally representative samples from the United States (18,34–37). In addition, nearly all of the chronic mental health and somatic conditions used in this study were included among the 40 conditions used in a U.K. study (12) and among the 11 conditions suggested for international multimorbidity research (38).
There are limitations that need to be considered. First, our analyses were purely descriptive and hypothesis generating rather than hypothesis testing. However, we consider our findings an important first step toward understanding the incidence and life course accumulation of SMM. Second, our analyses were restricted to somatic and mental health conditions that were brought to medical attention. Therefore, we may have underestimated those conditions that were asymptomatic or did not uniformly come to medical attention, such as dementia and cognitive disorders, and other mental health disorders. The underascertainment may have varied by age, sex or gender, and race/ethnicity. In addition, the time sequence of the development of the chronic conditions was not considered (eg, condition A preceding condition B). If the time sequence of chronic conditions differed across age, sex, or race/ethnicity groups, it may have led to differences in the estimated prevalence.
Third, we were unable to establish the validity of ICD-9 codes. The use of ICD-9 and other diagnosis codes has clear advantages, including not having to rely on self-report of medical conditions (17). However, these diagnosis codes were assigned during the course of routine medical care and are thus subject to misclassification. We attempted to reduce the risk of false-positive diagnoses by including only those persons who received at least two codes for a given condition separated by more than 30 days and within a 5-year capture frame. Fourth, we did not assess the severity of specific conditions or their cumulative effects on function and prognosis, nor did we study possible interactions between treatment and specific conditions.
Fifth, our study focused on a single geographically defined U.S. population, and the prevalence of SMM may differ in other populations. However, the demographic and socioeconomic characteristics of our population are similar to those of the upper Midwest of the United States (39), and the prevalence of multimorbidity in persons 65 years of age or older was similar in our population compared with the entire U.S. Medicare population (18,34–36). Replication of this study in other populations in the United States and worldwide will allow for useful comparisons (17,18,40). Our analyses did not include a measure of socioeconomic status, an established risk factor for multimorbidity in general (11), and SMM in particular (3,12), and a major determinant of health care costs and quality of care in patients with SMM (41,42). In addition, although the REP is not an insurance-based medical records-linkage system, it is possible that a small segment of the Olmsted County population was not captured adequately. In particular, persons without health insurance coverage who had recently immigrated to the county may have received some simple medical services (eg, immunizations) through local charitable organizations not included in the REP. However, all the remaining services for these persons should have been captured by the REP.
Finally, we used unweighted disease counts (as opposed to a weighted multimorbidity index) to quantify multimorbidity; therefore, our approach did not consider differences in severity or in prognostic impact of the conditions. On the other hand, disease counts are frequently used in multimorbidity research and are considered particularly suitable for cross-sectional multimorbidity studies that use electronic records or administrative data (43).
Supplementary Material
Please visit the article online at http://gerontologist.oxfordjournals.org/ to view supplementary material.
Funding
This work was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health (R01AG034676). However, the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. C.M.B. was supported by the Paul Beeson Career Development Award Program (NIA K23 AG032910), the John A. Hartford Foundation, Atlantic Philanthropies, the Starr Foundation, and an anonymous donor. The funders had no involvement in study design, data collection, analysis, interpretation, manuscript preparation, or the decision to submit for publication. W.V.B. had full access to all study data and final responsibility for the decision to submit for publication.
Conflict of Interest
There are no conflicts of interest to report.
Supplementary Material
References
- 1. Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276:1473–1479. doi:10.1001/jama.1996.03540180029029 [PubMed] [Google Scholar]
- 2. Kronick R, Bella M, Gilmer T. The Faces of Medicaid III: Refining the Portrait of People With Multiple Chronic Conditions. Hamilton, NJ: Center for Health Care Strategies, Inc; 2009. [Google Scholar]
- 3. Neeleman J, Ormel J, Bijl RV. The distribution of psychiatric and somatic III health: associations with personality and socioeconomic status. Psychosom Med. 2001;63:239–247. [DOI] [PubMed] [Google Scholar]
- 4. Davydow DS, Levine DA, Zivin K, Katon WJ, Langa KM. The association of depression, cognitive impairment without dementia, and dementia with risk of ischemic stroke: a cohort study. Psychosom Med. 2015;77:200–208. doi:10.1097/PSY.0000000000000136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51:458–465. doi:10.1176/appi.psy.51.6.458 [DOI] [PubMed] [Google Scholar]
- 6. Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55:752–760. [DOI] [PubMed] [Google Scholar]
- 7. Boyd C, Leff B, Weiss C, Wolff J, Hamblin A, Martin L. Clarifying Multimorbidity Patterns to Improve Targeting and Delivery of Clinical Services for Medicaid Populations. Faces of Medicaid Data Brief 2010. http://www.chcs.org/media/clarifying_multimorbidity_patterns.pdf Accessed January 27, 2016.
- 8. Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–1304. doi:10.1001/jama.2010.381 [DOI] [PubMed] [Google Scholar]
- 9. Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Druss BG, Walker ER. Mental disorders and medical comorbidity. Synth Proj Res Synth Rep. 2011;21:1–26. [PubMed] [Google Scholar]
- 11. Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9:e102149. doi:10.1371/journal.pone.0102149.eCollection 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi:10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 13. Wallace RB, Salive ME. The dimensions of multiple chronic conditions: where do we go from here? A commentary on the Special Issue of Preventing Chronic Disease. Prev Chronic Dis. 2013;10:E59. doi:10.5888/pcd10.130104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41:1614–1624. doi:10.1093/ije/dys195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. doi:10.5888/pcd10.120239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7 suppl 1):S44–S50. doi:10.1097/MLR.0b013e3181a23e3a [DOI] [PubMed] [Google Scholar]
- 17. Posner SF, Goodman RA. Multimorbidity at the local level: implications and research directions. Mayo Clin Proc. 2014;89:1321–1323. doi:10.1016/j.mayocp.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 18. Rocca WA, Boyd CM, Grossardt BR, et al. Prevalence of multimorbidity in a geographically defined American population: patterns by age, sex, and race/ethnicity. Mayo Clin Proc. 2014;89:1336–1349. doi:10.1016/j.mayocp.2014.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. St Sauver JL, Boyd CM, Grossardt BR, et al. Risk of developing multimorbidity across all ages in an historical cohort study: differences by sex and ethnicity. BMJ Open. 2015;5:e006413. doi:10.1136/bmjopen-2014-006413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi:10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 21. Agency for Healthcare Research and Quality and the National Center for Health Statistics. Appendix A - Clinical Classification Software-DIAGNOSES (January 1980 Through September 2013) 2013. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ AppendixASingleDX.txt Accessed January 27, 2016.
- 22. Zhang AY, Snowden LR, Sue S. Differences between Asian and White Americans’ help seeking and utilization patterns in the Los Angeles area. J Community Psychol. 1998;26:317–326. doi:10.1002/(SICI)1520-6629(199807)26:4<317::AID-JCOP2>3.0.CO;2-Q [Google Scholar]
- 23. Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–2716. doi:10.1001/jama.289.20.2709 [DOI] [PubMed] [Google Scholar]
- 24. Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67:254–266. doi:10.1016/j.jclinepi.2013.09.021 [DOI] [PubMed] [Google Scholar]
- 25. Kessler RC, Birnbaum HG, Shahly V, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety. 2010;27:351–364. doi:10.1002/da.20634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ruel G, Lévesque JF, Stocks N, et al. Understanding the evolution of multimorbidity: evidences from the North West Adelaide Health Longitudinal Study (NWAHS). PLoS One. 2014;9:e96291. doi:10.1371/ journal.pone.0096291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith DJ, Martin D, McLean G, Langan J, Guthrie B, Mercer SW. Multimorbidity in bipolar disorder and undertreatment of cardiovascular disease: a cross sectional study. BMC Med. 2013;11:263. doi:10.1186/1741-7015-11-263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Garin N, Koyanagi A, Chatterji S, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016;71:205–214. doi:10.1093/gerona/glv128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29:409–416. doi:10.1016/j.genhosppsych.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 30. St John PD, Tyas SL, Menec V, Tate R. Multimorbidity, disability, and mortality in community-dwelling older adults. Can Fam Physician. 2014;60:e272–e280. [PMC free article] [PubMed] [Google Scholar]
- 31. Scott KM, Bruffaerts R, Tsang A, et al. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007;103:113–120. doi:10.1016/j.jad.2007.01.015 [DOI] [PubMed] [Google Scholar]
- 32. Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70 Suppl 2:20–24. [DOI] [PubMed] [Google Scholar]
- 33. Roy-Byrne PP, Davidson KW, Kessler RC, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30:208–225. doi:10.1016/j.genhosppsych.2007.12.006 [DOI] [PubMed] [Google Scholar]
- 34. Ashman JJ, Beresovsky V. Multiple chronic conditions among US adults who visited physician offices: data from the National Ambulatory Medical Care Survey, 2009. Prev Chronic Dis. 2013;10:E64. doi:10.5888/pcd10.120308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lochner KA, Cox CS. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Prev Chronic Dis. 2013;10:E61. doi:10.5888/pcd10.120137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Steiner CA, Friedman B. Hospital utilization, costs, and mortality for adults with multiple chronic conditions, Nationwide Inpatient Sample, 2009. Prev Chronic Dis. 2013;10:E62. doi:10.5888/pcd10.120292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65. doi:10.5888/pcd10.120203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases–a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66:301–311. doi:10.1093/gerona/glq208 [DOI] [PubMed] [Google Scholar]
- 39. St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, III, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–160. doi:10.1016/j.mayocp.2011.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Goodman RA, Ling SM, Briss PA, Parrish RG, Salive ME, Finke BS. Multimorbidity patterns in the United States: implications for research and clinical practice. J Gerontol A Biol Sci Med Sci. 2016;71:215–220. doi:10.1093/gerona/glv199 [DOI] [PubMed] [Google Scholar]
- 41. McLean G, Gunn J, Wyke S, et al. The influence of socioeconomic deprivation on multimorbidity at different ages: a cross-sectional study. Br J Gen Pract. 2014;64:e440–e447. doi:10.3399/bjgp14X680545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Payne RA, Abel GA, Guthrie B, Mercer SW. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ. 2013;185:E221–E228. doi:10.1503/cmaj.121349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mercer SW, Guthrie B, Furler J, Watt GC, Hart JT. Multimorbidity and the inverse care law in primary care. BMJ. 2012;344:e4152. doi:10.1136/bmj.e4152 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.