Abstract
Objectives. To assess whether asking questions about a future behavior changes this behavior (i.e., the question–behavior effect) when applied to a population-level intervention to enhance colorectal cancer screening.
Methods. In 2013, text-message reminders were sent to a national sample of 50 000 Israeli women and men aged 50 to 74 years following a fecal occult blood test invitation. Participants were randomized into 4 intervention groups (2 interrogative reminders, with or without reference to social context; 2 noninterrogative reminders, with or without social context) and a no-intervention control group. The outcome was fecal occult blood test uptake (n = 48 091, following attrition).
Results. Performance of fecal occult blood test was higher in the interrogative-reminder groups than in the other 3 groups (odds ratio = 1.11; 95% confidence interval = 1.05, 1.19); the effect size was small, varying in the different group comparisons from 0.03 to 0.06.
Conclusions. The question–behavior effect appears to be modestly effective in colorectal cancer screening, but the absolute number of potential screenees may translate into a clinically significant health promotion change.
Colorectal cancer (CRC) is a leading cause of cancer mortality.1 Undergoing screening, a medically recommended health behavior, leads to diagnosis at earlier stages of CRC, with better treatment options and subsequent reduction in mortality.2–4 Organized CRC screening programs that use the fecal occult blood test (FOBT) as the screening test modality have been established in many countries5; however, individuals respond variably to the invitation to screen, often adhering at a less than desirable degree to the recommendations.
As part of the National Colorectal Cancer Early Detection Program in Israel, individuals in the target population of average risk, aged 50 to 74 years, are regularly invited for an annual FOBT (colonoscopy is recommended for high-risk individuals’ screening). The program team collaborates internationally with other organized programs,6 and continuously monitors the process from test to diagnosis. Uptake is studied,7 and new interventions to increase participation are introduced, assessed, and adopted.8 These attempts equally address insured members of all walks of life,9 free of charge, under the National Health Insurance Law.10 This is a report of a study attempting to enhance adherence to CRC screening by using the question–behavior effect (QBE); employed on a population level, the QBE technique was streamlined from a survey into a single text-line message in an mHealth (mobile phone–related) intervention.
The QBE refers to the phenomenon of posing behavior-related questions that may change the individual’s behavior in the referred-to domain. This has been demonstrated in various circumstances11: purchasing products, volunteering time for a charitable cause,12 donating to one’s alma mater, voting behavior,13 recycling behavior, and enacting normative and nonnormative health behaviors.14–16 Among these studies were laboratory experiments, controlled field experiments, and panel-based field data; question phrasing varied, with different response modalities: paper and pencil, telephone, face-to-face interview, mass communicated “ask yourself” advertisement, and individual mailer.11 The dependent measures have been self-reported behavior, choice, or observable behavior.
The dominant explanation for QBE is that the mere fact of being “measured” (asked, in this case) influences the formation of attitudes toward the behavior itself or makes specific aspects of performing a behavior more accessible, thereby fostering performance.11,17–19 There is evidence that surveyed respondents form a broad range of inferences that can later affect behavior20; even though the exact process underlying the effect is still under study,11,18,21 there is agreement that the QBE is the result of a nonconscious, automatic,16,22 effortless processing.23 Studies on the QBE in the domain of health behaviors used self-reports and objective measures, and ranged from physical activity,14 blood donation,24 flossing,22 and screening,25 as examples of socially normative health-promoting behaviors, to alcohol use,26 choice of food, and risky sexual behavior,27 as examples of nonnormative, health-compromising behaviors.
Two recent meta-analyses examined the effect on subsequent behavior. The first21 was conducted on all behavioral domains and included 116 studies; it yielded an effect size of 0.24 in all studies and 0.15 when unreported studies were taken into account (Cohen’s d = 0.15; 95% confidence interval [CI] = 0.08, 0.21). It called for more studies in field settings to determine how the effect can be harnessed to promote “real-life” behavior change.21 A second meta-analysis28 of 41 studies focusing on health behaviors found a small significant effect (d = 0.09; 95% CI = 0.04, 0.13), with moderate heterogeneity. This review concluded that “the evidence for sending questionnaires to increase behavioral uptake is limited,”28(p15) especially with evidence of publication bias, namely that studies with no effects or smaller effects were less likely to be published, and implications for practice are “difficult to identify at this stage.”28(p15)
The present intervention took place as part of a routine procedure of the National Program for the Early Detection of Colorectal Cancer. We examined whether this intervention can be adapted effectively to a population. Accordingly, we constructed a “lean” mode of a QBE intervention, examining whether a single, short text message would enhance CRC screening via FOBT. Recent work has documented that a mailed questionnaire in the health behaviors domain containing 6 items resulted in increased uptake of blood donation24; the present work examined whether only 1 item would yield more CRC screening, compared with the control standard care of no intervention. We used an available technology29 of mobile telephone texting, currently a ubiquitous technique in everyday life, adopted by individuals in all age groups. Electronic messages have been shown to promote CRC screening30 and to improve risk factor indicators31 (e.g., cardiovascular disease) and health behaviors, yet the engagement with the participants in these studies was long and interactive, whereas the present study examined a minimal intervention.
We included 2 additional issues raised in work by Godin et al.24,32 First, we investigated whether the grammatical form of the message affects behavior uptake; that is, does a question (interrogative) “produce greater changes in [health] behavior than simply sending reminders to perform the behavior”28 as in declarative wording. Second, we examined whether invoking a daily-life social context (norm, in Godin et al. terms) would have an effect on CRC screening; Godin et al. found that invoking a moral norm had no effect on subsequent behavior whereas the present work focused on an aspect of participants’ social context, referring to “others their age.”24 Finally, having the QBE (especially the conditions with no social context) in such a lean mode decreases the threat of bias emerging from possible interaction between the QBE and content of a behavioral intervention.18
Thus, the study included 2 interrogative text message reminders (with or without social reference), which were the experimental conditions. We compared these QBE conditions with a no-intervention control group, which constituted the standard care of no reminder. We also compared the experimental conditions with 2 noninterrogative text messages (with or without social reference), which represented mere reminders. This design allows a comparison among a question mode (QBE), a noninterrogative (declarative) reminder, and a no reminder condition (i.e., standard care).
The study hypotheses were (1) screening uptake would be higher in the intervention interrogative groups than in the noninterrogative reminder and no-intervention condition; (2) because of the lean mode of the study, the effect size (ES) of the intervention would be similar or smaller than the one found in the meta-analysis28; and (3) the embedding of the messages in a social context would yield more screening uptake than messages without reference to a social context.
METHODS
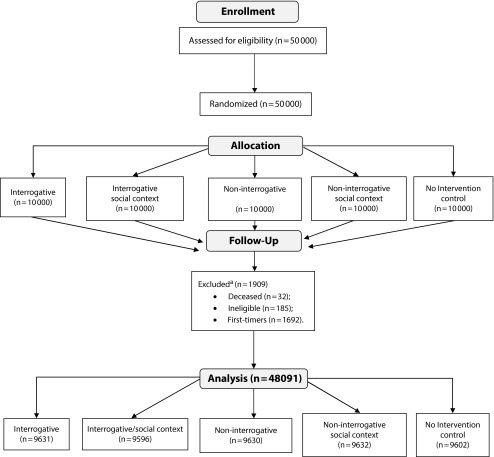
The study platform was a routine mailed-invitation wave of the National Israeli Colorectal Cancer Early Detection program; all addressees (= population) were included, 50 000 Israeli women and men aged 50 to 74 years, with no diagnosis of an inflammatory bowel disease or a bowel malignancy, who had not undergone colonoscopy within the previous 3 years, and who had not performed FOBT in the previous year. We excluded a small minority of the participants, 3.34% (1692 individuals), first-time invitees, from the analysis as they belonged to a different segment of invited participants. Ineligible (no longer HMO members; n = 32) or deceased individuals (n = 185) were equally distributed in the study conditions and we excluded them from the analysis, with a final number of 48 091. Figure 1 displays the study flowchart.
FIGURE 1—
Flowchart of Study Participants: National Colorectal Cancer Early Detection Program, Israel, 2013
aConducted at the follow-up stage of the study, in preparation for data analysis, rather than immediately after eligibility assessment.
Design and Procedure
All individuals received (in 2013) an identical letter inviting them to perform an FOBT, asking them to mail back an FOBT kit order or to pick up a kit at their primary-care neighborhood clinic. We randomized them into 5 equal-sized groups of the independent variable (Table 1). In the “2 × 2 plus no intervention” design, we manipulated grammatical form (interrogative vs noninterrogative) and social context reference (yes or no). The 2 experimental conditions consisted of interrogative reminders, with or without reference to social context. The 3 other groups included 1 condition with no intervention (no reminder) and the other 2 conditions included noninterrogative reminders, with or without social context.
TABLE 1—
Experimental Conditions: National Colorectal Cancer Early Detection Program, Israel, 2013
| Experimental Condition | Phrasing of Text Sent |
| Interrogative | “Following the invitation to screen for CRC, recently sent to you, do you intend to mail-order an FOBT kit and be tested? At your service, CHS” |
| Interrogative + social context | “Following the invitation to screen for CRC, recently sent to you, do you intend to mail-order an FOBT kit and be tested, as others your age do? At your service, CHS” |
| Noninterrogative | “Following the invitation to screen for CRC, recently sent to you—it is important to mail-order a kit and be tested. At your service, CHS” |
| Noninterrogative + social context | “Following the invitation to screen for CRC, recently sent to you—people your age mail-order an FOBT kit and undergo the test. At your service, CHS” |
| No intervention | None |
Note. CHS = Clalit Health Services; CRC = colorectal cancer; FOBT = fecal occult blood test.
A week following the mailing of the invitation letter, 1 of 4 text messages (or none, for the no-intervention control group, standard care) was randomly sent to the mobile telephones of participants by group assignment. We assessed the dependent variable, participants’ FOBT performance, at 6 months following the mailing of the invitation, based on the National Israeli Colorectal Cancer Early Detection program’s database.
Materials
Demographic information included gender, age, participants’ neighborhood clinic’s socioeconomic status (SES) used as proxy for individual SES, and past FOBT performance retrieved from Clalit Health Services’ (CHS, the HMO involved) computerized database.
Brief text messages, consisting of 122 to 135 characters (in Hebrew), began with “Following the invitation to screen for CRC, recently sent to you. . . ,” ending with “at your service, CHS.”
The central part of the messages conveyed the condition to which a participant was randomly assigned. In a 2 × 2 design, the first variable was grammatical form (interrogative vs noninterrogative) and the second was the social context of performing FOBT (yes or no). In the fifth condition, the control standard care group, participants received no text message from the study administration. The questions were: “. . . do you intend to mail-order an FOBT kit and be tested?” or “. . . do you intend to mail-order an FOBT kit and be tested, as others your age do?”; the statements were: “. . . it is important to mail-order a kit and be tested,” or “. . . people your age mail-order an FOBT kit and undergo the test.”
The independent variable was the condition to which an individual was assigned. Auxiliary independent variables were demographic variables. The dependent variable was FOBT performance at 6 months following the invitation mailing, based on the computerized database of CHS’s National Program for the Early Detection of Colorectal Cancer.
Statistical Analysis
Data analysis consisted of 2 stages. For the first stage, we described demographic and past FOBT screening characteristics of participants, with continuous variables presented by mean and SD and categorical variables presented in percentages. We compared the study’s 5 conditions in terms of these characteristics by using the χ2 test for the categorical variables and analysis of variance for the continuous variables as well as Cohen’s effect size for the difference between 2 independent population proportions.
In the second stage, we examined the effect of the grammatical form and of social context in the 4 message types on screening by using a multivariable logistic regression with FOBT performance measured at 6 months as the dependent variable. We reported odds ratios (ORs) with 95% confidence intervals (CIs).
RESULTS
Participants were 51.1% women, their mean age was 60.44 years (±6.04), and the majority were married (69.7%). Frequency distribution along clinics’ SES scores was 26.1% in low SES, 45.7% in middle SES, and 28.1% in high SES. The majority of the study participants (73.5%) had not performed FOBT in the 7 years before the study although it is recommended to individuals in the target population to undergo the test annually. These characteristics were uniformly distributed along the 5 study conditions, with no significant differences among the conditions (Table 2).
TABLE 2—
Demographic Characteristics by Conditions and Cumulative Fecal Occult Blood Test Performance of Participants in Each Text Message Group Compared With the No-Intervention Group: National Colorectal Cancer Early Detection Program, Israel, 2013
| Variable | Interrogative (n = 9631) | Interrogative + Social Context (n = 9596) | Noninterrogative (n = 9630) | Noninterrogative + Social Context (n = 9632) | No-Intervention Control (n = 9602) | Statistic χ2/F | P |
| Demographic variables | |||||||
| Age, y, mean ±SD | 60.5 ±6.0 | 60.5 ±6.0 | 60.6 ±6.0 | 60.4 ±6.0 | 60.7 ±6.1 | 1.9 | .101 |
| Women, no. (%) | 5001 (51.9) | 4838 (50.4) | 4858 (50.4) | 4945 (51.3) | 4911 (51.1) | 6.3 | .181 |
| SES, no. | 9604 | 9561 | 9595 | 9604 | 9567 | 1.3 | .995 |
| Low, no. (%) | 2534 (26.3) | 2502 (26.2) | 2505 (26.1) | 2486 (25.9) | 2514 (26.3) | ||
| Medium, no. (%) | 4393 (45.7) | 4353 (45.5) | 4369 (45.5) | 4429 (46.1) | 4370 (45.7) | ||
| High, no. (%) | 2687 (28.0) | 2706 (28.3) | 2721 (28.4) | 2689 (28.0) | 2683 (28.0) | ||
| Married no. (%) | 6722 (69.8) | 6635 (69.1) | 6673 (69.3) | 6779 (70.4) | 6710 (69.9) | 4.5 | .347 |
| Performed FOBT in the past, no. (%) | 2673 (27.8) | 2601 (27.1) | 2668 (27.7) | 2528 (26.2) | 2624 (27.3) | 7.3 | .123 |
| Test performance | |||||||
| At 6 mo, no. (%) | 942 (9.8) | 988 (10.3) | 884 (9.2) | 923 (9.6) | 817 (8.5) | ||
| χ2 | 9.4 | 18.0 | 2.69 | 6.74 | |||
| P | .002 | < .001 | .101 | .009 | |||
| Effect sizea (95% CI) | 0.05 (0.04, 0.06) | 0.06 (0.05, 0.07) | 0.02 (0.01, 0.03) | 0.04 (0.03, 0.05) | |||
Note. CI = confidence interval; FOBT = fecal occult blood test; SES = socioeconomic status.
Effect size for the difference between 2 independent population proportions, specifically a difference between arc sin transformations of the proportions. Each proportion is transformed:
Ø1 = 2arcsin√P1
Ø2 = 2arcsin√P2
And the effect size is:
ES = Ø1- Ø2
The arc sin transformation allows for equal “units of detectability.”33(p181)
Intervention Findings
We compared the 2 interrogative text-message conditions with the no-intervention control on participation rates, which were, in both the interrogative and interrogative-with-social-context conditions, higher (9.8% and 10.3%, respectively) than the control (8.5%). Table 2 displays participation rates at 6 months, cumulatively, across the 5 conditions, including χ2 and ES (compared with the no-intervention control).
We carried out a multivariable logistic regression with FOBT performance at 6 months as the dependent variable (Table 3). The predictors were demographic variables and message type. All versions but 1 (the noninterrogative) had a significant effect, compared with the no-intervention control (coded 0), as well as age (OR = 1.13; 95% CI = 1.06, 1.20; P < .001), gender (OR = 1.21; 95% CI = 1.13, 1.28; P < .001), and clinic SES (OR = 1.14; 95% CI = 1.06, 1.22; P = .001 and OR = 1.19; 95% CI = 1.1, 1.3; P < .001, respectively, for the medium- and low-SES clinics), so that older participants, women, and individuals of lower SES screened more often than younger participants, men, and individuals of higher SES. An analysis comparing the 2 interrogative groups to the other 3 groups yielded a significant difference (χ2 = 12.07; OR = 1.11; 95% CI = 1.05, 1.19; P < .001) with a small ES of 0.03.
TABLE 3—
Multivariable Logistic Regression Predicting Fecal Occult Blood Test Performance at 6 Months: National Colorectal Cancer Early Detection Program, Israel, 2013
| Variable | OR (95% CI) |
| Text message version | |
| No-intervention control (Ref) | 1 |
| Interrogative | 1.17 (1.06, 1.29) |
| Interrogative + social context | 1.24 (1.12, 1.36) |
| Noninterrogative | 1.09 (0.99, 1.21) |
| Noninterrogative + social context | 1.14 (1.04, 1.26) |
| Age > 60 y | 1.13 (1.06, 1.20) |
| Gender, women | 1.21 (1.13, 1.28) |
| SES | |
| High (Ref) | 1 |
| Low | 1.19 (1.10, 1.30) |
| Medium | 1.14 (1.06, 1.22) |
Note. CI = confidence interval; OR = odds ratio; SES = socioeconomic status.
Grammatical Form and Social Context Effects
To examine the effects of grammatical form and social context, we carried out a multivariable logistic regression with FOBT performance at 6 months cumulatively as the dependent variable. This analysis excluded the no-intervention control group, analyzing the data according to a 2 × 2 design. The predictors were demographic variables and 2 combinations of message type: grammatical form (interrogative vs noninterrogative, coded 1 or 0), social context (with or without reference to social context, coded 1 and 0), and the interaction between them in the next step.
After we controlled for age, SES, and gender, the question mode had an OR of 1.07 (95% CI = 1.004. 1.150; P = .038), whereas social context had no significant effect, with an OR of 1.06 (95% CI = 0.99, 1.13; P = .115), nor did the interaction, with an OR of 1.02 (95% CI = 0.89, 1.16; P = .827).
DISCUSSION
This work presents an attempt to assess theoretically based hypotheses concerning CRC screening enhancement on a population level, carried out with a current mHealth technology. We examined the applicability and limits of QBE, using an mHealth intervention; a lean mode of a single, short text message (sent over cellular telephones) was carried out in a public health environment (vs laboratory). The examination of the minimal QBE compared 4 versions of the text message: interrogative and noninterrogative reminders, each combined with a social context reminder, or without one.
The main finding was that screening uptake was higher in the interrogative groups than the other groups, thus supporting the first hypothesis pertaining to the message’s grammatical form. The results indicate that the interrogative grammatical form yielded a higher rate of participation, even in this minimal intervention, than a mere reminder or prompt (the noninterrogative conditions), with a small effect size. This comparison allowed us to conclude that it is not merely cuing to action or behavioral simulation that enhances screening, but rather the posing of a question.
The ES found for the interrogative text messages (compared with the control) was 0.05 to 0.06, somewhat smaller than the one expected according to the meta-analysis on health behaviors,28 yet within the reported range, supporting the second hypothesis. We examined the third hypothesis pertaining to social context of the screening message by comparing the messages with social reference to those without social context, yielding a nonsignificant difference, as found by Godin et al.24
The characteristics of participants adhering in the reported studies are similar to those reported in other studies34,35: they are women and older individuals, within the age range of 50 to 74 years. Although younger individuals may seem to be more likely to engage in “new” behaviors, the group aged 60 to 74 years in (breast and colorectal) cancer screening tends to adhere to the invitation to screen more than the group aged 50 to 59 years. One reason may be that, by the age of 60 years, individuals have begun paying more attention to their health and have adopted a healthier lifestyle, which facilitates adopting additional health behaviors. Another is that invitees in the younger age group do not associate themselves yet with an “older people’s” disease, as CRC may be viewed.
This study had several strengths. First, we used an objective outcome measure of actual screening as recorded in an HMO database. Second, we carried out the assessment of screening participation on a relatively large group of individuals in the community. Third, the study included participants from community samples that were not self-selected in any way, as often practiced in QBE studies, and we carried out analyses on an intention-to-treat basis. Fourth, the study addressed an older population, less often studied in the context of QBE studies; recent qualitative data indicates this group to be receptive to receiving cancer screening text messages from health care providers.36 Fifth, the intervention has an additional potential for expansion, as engaging in a health behavior, at least once, is a strong predictor of repeating this behavior in the future by the same individual. An additional advantage of the lean mode of the intervention is that it decreased the methodological threat (to internal validity) of an interaction between intervention and QBE.18 Finally, the mHealth method—simple, inexpensive, and parsimonious—has potentially wide applications.
The study has several limitations. First, participants may not have read the telephone message. Second, the message carried an organizational signature; a personal one could have been more effective. Third, we did not address the mechanisms underlying the QBE, because of the lean mode of the intervention.
The study documented a relatively minor rise in FOBT performance rate in the interrogative conditions’ groups, and a low ES of this change. This can be explained by some of the study characteristics: participants were a distinct subgroup of the least responsive in the target population to CRC screening invitations, thus being most difficult to motivate to respond; according to the meta-analysis,21 field studies and intention (rather than prediction) questions are associated with lower effect size. However, population-level interventions aiming at heterogeneous audiences seldom result in revolutionary outcomes. Rather, they increase adherence incrementally. Such interventions need to be as cheap as possible, and the minimal mode used here is one such example; it exemplifies that “even effects that are small in conventional terms can be hugely valuable in public policy and public health terms”21(p20) The small effect in this work translates to about 12 000 more screeners in a population of approximately 800 000 (1.5%, the difference between experimental and the no-intervention condition); combined with other intervention methods used with the same target population, this may enhance CRC screening participation on the aggregate level.
Further research could explore additional options of translating the QBE to population-level cancer prevention in different subgroups; for example, past performers who received mailed test kits (rather than letters inviting them to order a kit) and are therefore more likely to screen. The mHealth scene offers opportunities, for example, in the interface between health care organizations and insured members, which can be then compared with the paper–pencil mode. Rodrigues et al.28 concluded in the meta-analysis of the QBE in health behaviors that “the evidence for sending questionnaires to increase behavioral uptake is limited” 28(p15); however, sending short text messages or using other mHealth possibilities is a new frontier in current attempts at behavior change.
Policy recommendations on the basis of the study findings suggest that the routine use of the relatively low-cost method of text messages to encourage CRC screening should preferably be in the interrogative-with-social-context form. Translating QBE methods into mHealth interventions applies theories to mass practice. Although the rate of increased screening test performance is modest, on the population-level, as part of “multifactor interventions targeting multiple levels,”37(p1158) incremental benefits38 could translate to a clinically significant increase in individuals agreeing to screen. It should be noted that mHealth messages are not a 1-time, unidirectional intervention. When addressed, individuals react, and they may sometimes reply. This continues the interaction cycle with a program’s team, thereby enhancing screening as well as satisfaction from the service.
ACKNOWLEDGMENTS
This work was supported by the Israeli Cancer Association (grant 20132129).
The authors thank the 3 anonymous reviewers and appreciate their helpful comments.
HUMAN PARTICIPANT PROTECTION
Human participants’ approval (021–26513, 5.5.13) includes the study protocol (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org) and a specifically granted exemption from the use of consent forms (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org).
REFERENCES
- 1.World Health Organization. Cancer. 2014. Available at: http://www.who.int/mediacentre/factsheets/fs297/en. Accessed October 10, 2014.
- 2.Kronborg O, Fenger C, Olsen J, Jørgensen OD, Søndergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 3.Mandel JS, Bond JH, Church TR et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. N Engl J Med. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 4.Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(9):659–669. doi: 10.7326/0003-4819-149-9-200811040-00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Cancer Screening Network. Colorectal cancer screening activities in ICSN countries. 2009. Available at: http://appliedresearch.cancer.gov/icsn/colorectal/screening.html. Accessed July 7, 2013.
- 6.Klabunde C, Blom J, Bulliard J-L et al. Participation rates for organized colorectal cancer screening programmes: an international comparison. J Med Screen. 2015;22(3):119–126. doi: 10.1177/0969141315584694. [DOI] [PubMed] [Google Scholar]
- 7.Hagoel L, Feder-Bubis P. Mind the cancer screening gap between medical rationale and laypersons’ reasoning. J Intern Med. 2016;279(6):563–565. doi: 10.1111/joim.12472. [DOI] [PubMed] [Google Scholar]
- 8.Neter E, Stein N, Barnett-Griness O, Rennert G, Hagoel L. From the bench to public health: population-level implementation intentions in colorectal cancer screening. Am J Prev Med. 2014;46(3):273–280. doi: 10.1016/j.amepre.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Gupta S, Sussman D, Doubeni C et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014;106(4):dju032. doi: 10.1093/jnci/dju032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.State of Israel, Ministry of Health. Rights of the insured under the National Health Insurance Law. Available at: http://www.health.gov.il/English/Topics/RightsInsured/RightsUnderLaw/Pages/default.aspx. Accessed November 24, 2015.
- 11.Dholakia UM. A Critical Review of Question-Behavior Effect Research. Rochester, NY: Social Science Research Network; 2009. [Google Scholar]
- 12.Sherman SJ, Gorkin L. Attitude bolstering when behavior is inconsistent with central attitudes. J Exp Soc Psychol. 1980;16(4):388–403. [Google Scholar]
- 13.Greenwald AG, Carnot CG, Beach R, Young B. Increasing voting behavior by asking people if they expect to vote. J Appl Psychol. 1987;72(2):315–318. [Google Scholar]
- 14.Godin G, Sheeran P, Conner M, Germain M. Asking questions changes behavior: mere measurement effects on frequency of blood donation. Health Psychol. 2008;27(2):179–184. doi: 10.1037/0278-6133.27.2.179. [DOI] [PubMed] [Google Scholar]
- 15.Spangenberg E. Increasing health club attendance through self-prophecy. Mark Lett. 1997;8(1):23–31. [Google Scholar]
- 16.Williams P, Block LG, Fitzsimons GJ. Simply asking questions about health behaviors increases both healthy and unhealthy behaviors. Soc Influ. 2006;1(2):117–127. [Google Scholar]
- 17.Chandon P, Morwitz VG, Reinartz WJ. Do intentions really predict behavior? Self-generated validity effects in survey research. J Mark. 2005;69(2):1–14. [Google Scholar]
- 18.McCambridge J. From question-behaviour effects in trials to the social psychology of research participation. Psychol Health. 2015;30(1):72–84. doi: 10.1080/08870446.2014.953527. [DOI] [PubMed] [Google Scholar]
- 19.Morwitz VG, Fitzsimons GJ. The mere-measurement effect: why does measuring intentions change actual behavior? J Consum Psychol. 2004;14(1-2):64–74. [Google Scholar]
- 20.Aarts H, Gollwitzer PM, Hassin RR. Goal contagion: perceiving is for pursuing. J Pers Soc Psychol. 2004;87(1):23–37. doi: 10.1037/0022-3514.87.1.23. [DOI] [PubMed] [Google Scholar]
- 21.Wood C, Conner M, Miles E et al. The impact of asking intention or self-prediction questions on subsequent behavior: a meta-analysis. Pers Soc Psychol Rev. 2016;20(3):245–268. doi: 10.1177/1088868315592334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levav J, Fitzsimons GJ. When questions change behavior: the role of ease of representation. Psychol Sci. 2006;17(3):207–213. doi: 10.1111/j.1467-9280.2006.01687.x. [DOI] [PubMed] [Google Scholar]
- 23.Jacoby LL. A process dissociation framework: separating automatic from intentional uses of memory. J Mem Lang. 1991;30(5):513–541. [Google Scholar]
- 24.Godin G, Germain M, Conner M, Delage G, Sheeran P. Promoting the return of lapsed blood donors: a seven-arm randomized controlled trial of the question–behavior effect. Health Psychol. 2014;33(7):646–655. doi: 10.1037/a0033505. [DOI] [PubMed] [Google Scholar]
- 25.Sandberg T, Conner M. A mere measurement effect for anticipated regret: impacts on cervical screening attendance. Br J Soc Psychol. 2009;48(pt 2):221–236. doi: 10.1348/014466608X347001. [DOI] [PubMed] [Google Scholar]
- 26.Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: part I. Alcohol use and related consequences. J Stud Alcohol Drugs. 2007;68(4):519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- 27.Knaus CS, Pinkleton BE, Weintraub Austin E. The ability of the AIDS quilt to motivate information seeking, personal discussion, and preventative behavior as a health communication intervention. Health Commun. 2000;12(3):301–316. doi: 10.1207/S15327027HC1203_05. [DOI] [PubMed] [Google Scholar]
- 28.Rodrigues AM, O’Brien N, French DP, Glidewell L, Sniehotta FF. The question–behavior effect: genuine effect or spurious phenomenon? A systematic review of randomized controlled trials with meta-analyses. Health Psychol. 2015;4(1):61–78. doi: 10.1037/hea0000104. [DOI] [PubMed] [Google Scholar]
- 29.Barclay G, Sabina A, Graham G. Population health and technology: placing people first. Am J Public Health. 2014;104(12):2246–2247. doi: 10.2105/AJPH.2014.302334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sequist TD, Zaslavsky AM, Colditz GA, Ayanian JZ. Electronic patient messages to promote colorectal cancer screening: a randomized controlled trial. Arch Intern Med. 2011;171(7):636–641. doi: 10.1001/archinternmed.2010.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chow CK, Redfern J, Hillis GS et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255–1263. doi: 10.1001/jama.2015.10945. [DOI] [PubMed] [Google Scholar]
- 32.Godin G, Bélanger-Gravel A, Vézina-Im L-A, Amireault S, Bilodeau A. Question–behaviour effect: a randomised controlled trial of asking intention in the interrogative or declarative form. Psychol Health. 2012;27(9):1086–1099. doi: 10.1080/08870446.2012.671617. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 34.Blom J, Kilpeläinen S, Hultcrantz R, Törnberg S. Five-year experience of organized colorectal cancer screening in a Swedish population—increased compliance with age, female gender, and subsequent screening round. J Med Screen. 2014;21(3):144–150. doi: 10.1177/0969141314545555. [DOI] [PubMed] [Google Scholar]
- 35.Ore L, Hagoel L, Lavi I, Rennert G. Screening with faecal occult blood test (FOBT) for colorectal cancer: assessment of two methods that attempt to improve compliance. Eur J Cancer Prev. 2001;10(3):251–256. doi: 10.1097/00008469-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Weaver KE, Ellis SD, Denizard-Thompson N, Kronner D, Miller DP. Crafting appealing text messages to encourage colorectal cancer screening test completion: a qualitative study. JMIR Mhealth Uhealth. 2015;3(4):e100. doi: 10.2196/mhealth.4651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Senore C, Inadomi J, Segnan N et al. Optimizing colorectal cancer screening acceptance: a review. Gut. 2015;64(7):1158–1177. doi: 10.1136/gutjnl-2014-308081. [DOI] [PubMed] [Google Scholar]
- 38.Fortuna RJ, Idris A, Winters P et al. Get screened: a randomized trial of the incremental benefits of reminders, recall, and outreach on cancer screening. Gen Intern Med. 2014;29(1):90–97. doi: 10.1007/s11606-013-2586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]