Abstract
Objectives. To estimate the simultaneous effects of social isolation and loneliness on mortality.
Methods. We analyzed a representative Finnish sample (n = 8650) from the cross-sectional Living Conditions Survey of 1994, with a 17-year follow-up period (1995–2011), by using Cox regression models adjusted for several possible confounding variables. We examined the possible nonlinear threshold effect of social isolation on mortality.
Results. The analyses revealed that social isolation predicted mortality even after we controlled for loneliness and control variables. The connection between social isolation and mortality was linear in nature and there was no synergistic effect between social isolation and loneliness. The effect of loneliness became nonsignificant when studied simultaneously with social isolation.
Conclusions. This study reveals strong evidence for an adverse effect of social isolation on mortality. Social isolation and loneliness seem to have distinct pathways to mortality and health. The results imply that the risk of mortality exists along a continuum, affecting not only those who experience extreme social isolation, but also those who suffer from mild to progressively increasing intensity of isolation.
A substantial body of empirical evidence shows that involvement in social relationships benefits health. Recent meta-studies demonstrate that there is a connection between social relationships and mortality1–3 and that the lack of social connections is as influential a mortality risk factor as traditional health-related indicators such as use of alcohol, smoking, or obesity.4,5 The lack of social relationships—defined as social isolation or loneliness—has frequently been the focus of research. The concepts of social isolation and loneliness have often been used interchangeably. They are, however, distinct but, nonetheless, interrelated concepts.
Small social networks, infrequent social contacts, absence of confidante connections, living alone, and lack of participation in social activities are criteria that have been used to define social isolation.2,6 Social isolation is concerned more with environmental impoverishment or restriction than with the individual’s ability to create and maintain social relationships. Loneliness is a subjective feeling of being without the type of relationships one desires. It may also describe a deficit between the actual and desired quality and quantity of social engagement.7,8 However, it is possible for one not to feel lonely despite objectively low frequency or quality of social contacts.9,10 Whereas loneliness is understood as a subjective concept, social isolation can be defined objectively. It is important to distinguish between social isolation and loneliness, although the former condition may, indeed, lead to the latter. Several studies have established that there is a low correlation between loneliness and social isolation.6,11,12
When examined separately, the effects of social isolation2,5,13–15 and loneliness2,16–19 on mortality are well established. Several studies have demonstrated6,12,20 that social isolation and loneliness, when studied simultaneously, have their own distinct effects on health. However, with respect to mortality, commentators highlight the necessity for further research2,6 as, currently, only 2 studies—identified in the meta-analysis2—have examined the effects of social isolation and loneliness concurrently on mortality, yielding mixed results. More information is needed, especially regarding both the relative and synergistic influences of social isolation and loneliness. The recent meta-study2 revealed another shortcoming in the literature: a substantial proportion of the research—89%—regarding social isolation and mortality has been conducted with participants who are older than 50 years. There is a need for further investigation with participants from a broader range of age groups.
Previous research indicates that social relationships can affect health and mortality in different ways. There are 3 general pathways by which social ties operate to influence health: behavioral, psychosocial, and physiological.21,22 Social ties might affect health-related behaviors, in part because they provide information and create norms that further influence health habits. Psychosocial mechanisms include, for example, social support, personal control, symbolic meanings and norms, and mental health. Physiological processes refer to immune, endocrine, and cardiovascular functions of the body, all of which are related to physiological systems engaged in stress responses. Socially active and connected persons are found to be characterized by lower stress levels than those who are socially isolated and lonely.21,23
It has been argued that the association between social relationships and mortality may have been overlooked by the major health organizations and by the general public because social relationships have been measured with various fuzzy variables that lack biomedical accuracy and control.4 The spectrum of different social isolation measurements in previous research has been wide, even though numerous studies have measured social isolation with the Berkman–Syme Social Networks Index,5,14,24 which sums 4 different types of social contacts: marital status (yes or no), sociability (frequency of contacts with other people), church group membership (yes or no), and membership in other community organizations (yes or no). Also, the studies that used the Berkman–Syme Social Networks Index have used various different measures of social contacts and different cut-off values to indicate social isolation.
It has also been suggested25,26 that social relationships have a nonlinear threshold effect on mortality, meaning that only those who are extremely socially isolated are at risk. However, the preponderance of current research evidence does not support the idea of a threshold effect,2,5,11 notwithstanding the publication of several studies13–15 that have found a threshold effect between social isolation and mortality.
Socioeconomic factors tend to be insufficiently considered in the studies analyzing the health effects of social relationships.27 Both the structural and functional characteristics of social ties vary in patterned ways in different demographic and status groups.21,28 Individuals having better education are found to have larger and more diverse confidante networks than their less-well-educated counterparts.28 Those in higher socioeconomic groups are more likely to be married, to have more friends, and to enjoy higher levels of social support.3,29 In addition, socioeconomic differences in health outcomes of social isolation may vary between men and women. With respect to men, 1 study showed that being in the lowest socioeconomic category increased the association between social isolation and death compared with belonging to the highest category.30
The aim of this study was to examine the concurrent effects of social isolation and loneliness on mortality. The study was based on a representative whole population sample, which provided the possibility of establishing whether social relationships had an effect on mortality in the general population. The social isolation index utilized in this study resembled the Berkman–Syme Social Networks Index and other previous isolation scales in that it compiled different ways of being socially isolated but also went a step further by measuring more dimensions of social isolation. Multidimensional approaches better represent the multiple pathways between social relationships and mortality.4 Multidimensional measurement also performs better as a proxy for real-world social isolation. We adjusted the analyses for several possible confounding variables. In addition, we used novel nonparametric statistical methods to investigate social relationships’ possible nonlinear threshold effect on mortality. We considered whether only high levels of social isolation were connected to mortality or whether, in fact, the mortality risk was linearly dependent on the level of social isolation.
METHODS
We derived the empirical data used for the research both from the cross-sectional Living Conditions Survey of 1994, which was collected by Statistics Finland, and the yearly official registry follow-up of the participants up to 2011 (n = 8650). We obtained the mortality information from the yearly registry-based follow-up data set. The combination of the survey data and registry-based mortality data was carried within Statistics Finland. We obtained the information on the participants in the Living Conditions Survey in 1994 by following the information logged against their personal social security number by Statistics Finland. The survey and the combined material did not include any identification data. The Living Conditions Survey is a representative sample of those older than 15 years in the Finnish population. The age of the participants ranged between 16 and 93 years, with a mean of 44.97 years (SD = 16.35) and the gender distribution was equal as 50.40% participants were women.
Interviews used in the gathering of the data had a relatively high response rate of 73%. According to a memorandum of Statistics Finland31 the data were generally representative, but those living in the metropolitan area, those who were older than 75 years, pensioners, and those having only basic education were slightly overrepresented among nonrespondents. Also, divorced and unmarried men were slightly underrepresented in the sample, but the lower representation was only because of problems with contacting them, not because of their refusal to participate.
Measurements
Mortality.
We obtained the possible year of death for every respondent from the registry follow-up data, which covered the years 1994 to 2011. In all, 1472 (17%) of the respondents died in the follow-up period and their average survival time after 1994 was 9.26 years (SD = 5.07).
Social isolation.
The multidimensional social isolation index parallels the Berkman–Syme Social Network Index and was developed to reflect different types of social connections that have, in the existing literature, been proven to be important indicators of isolation. We assigned all measures of social connection a dummy code indicating whether the respondent was isolated in a specific way or not. The social isolation index used in this study was designed to gauge 4 dimensions of isolation: (1) living alone, (2) not being in contact with family members that do not live with them, (3) isolation from friends, and (4) not participating in associational life. We assigned isolation dimensions a different number of measurements, but the overall scale was weighted such that each dimension contributed 25% to the overall social isolation index. The index varied between 0 and 100 with higher values indicating stronger isolation.
We assigned respondents isolation points regarding family connections for living alone and for meeting or being in a phone connection less than monthly with parents, children, and siblings not belonging to the same household. We assessed isolation from friends with 4 measurements: not having any close friends, not having a confidante, having less than a monthly meeting with friends, and having less than a monthly meeting with coworkers outside the work place. We measured isolation from associational life by 4 criteria: not having any responsibility or confidential posts in an organization, not participating in associations or other civic or social action, not participating in volunteer work, and not participating in neighborhood activities. There were no major validity issues concerning the social isolation index because the items were simple to answer (e.g., marital status or organizational membership). The isolation index used in this study functions as a proxy variable for the real social isolation.
Loneliness.
We measured loneliness with a single-item measurement: “Do you ever feel lonely?” The responses were recorded according to the scale 1 (never), 2 (very rarely), 3 (sometimes), 4 (very often), or 5 (constantly).
Control variables.
We adjusted the analyses for several demographic variables and behavioral, psychological, and clinical risk factors that might have an influence on mortality or social behavior. We factored into consideration the baseline effects of age, gender, self-reported health, body mass index, frequency of heavy alcohol consumption (subjective estimate of being clearly drunk), exercise or sports, educational level, employment or student status, and household income level per consumption unit. Adjusting the effect of self-reported health was especially important because of the possible reverse causality.2
Statistical Analyses
We estimated the survival time with a Cox regression that used general additive models (GAMs) in which we used data to determine the functional forms of the effects (linear or curvilinear).32 The use of the GAM models facilitated the examination of the curvilinear associations of loneliness and social isolation on mortality. We estimated GAMs with an MGCV package in the statistical program R version 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria). In GAMs, we used thin plate regression splines and we estimated an appropriate degree of spline smoothness from the data by using generalized cross-validation. We modeled the respondents still alive after 2011 as censored observations. The study variables had only few missing observations (social isolation, zero; loneliness, 27; and control variables, 0 to 38 missing observations) and, therefore, we applied listwise deletion of missing data in the analysis.
We examined the associations of social isolation and loneliness with mortality by estimating unadjusted, partially adjusted (age- and gender-adjusted), and fully adjusted (all control variables–adjusted) models. We analyzed the independent, relative, and synergistic effects of social isolation and loneliness.
RESULTS
Poor health, frequent heavy drinking, not working or studying, and low household incomes were connected to evaluated levels of loneliness and social isolation (Table 1). Women and the highly educated experienced greater loneliness, whereas those less well educated suffered higher degrees of social isolation. Also, those who never engaged in physical exercise reported higher levels of social isolation. Young people and senior citizens were also particularly socially isolated. The correlation between social isolation and loneliness was small (r = 0.18).
TABLE 1—
Mean Levels of Social Isolation and Loneliness in Different Groups: Living Conditions Survey of 1994, With Follow-Up to 2011, Finland
| Characteristic | Social Isolationa (95% CI) | Lonelinessb (95% CI) |
| Gender | ||
| Male | 39.98 (39.49, 40.47) | 2.00 (1.97, 2.02) |
| Female | 40.22 (39.74, 40.71) | 2.12 (2.09, 2.15) |
| Age, y | ||
| 15–24 | 44.07 (43.28, 44.87) | 2.08 (2.02, 2.13) |
| 25–44 | 36.44 (35.97, 36.91) | 2.09 (2.06, 2.12) |
| 45–64 | 38.07 (37.47, 38.66) | 2.02 (1.99, 2.05) |
| ≥ 65 | 53.04 (52.04, 54.04) | 2.04 (1.98, 2.10) |
| Perceived health | ||
| Poor | 48.90 (47.40, 50.40) | 2.35 (2.25, 2.44) |
| Fair | 42.34 (41.68, 43.00) | 2.14 (2.10, 2.18) |
| Good | 38.10 (37.69, 38.50) | 1.99 (1.97, 2.01) |
| BMI, kg/m2 | ||
| < 30 | 39.99 (39.62, 40.35) | 2.05 (2.03, 2.07) |
| ≥ 30 | 40.73 (39.64, 41.83) | 2.09 (2.03, 2.16) |
| Heavy drinking frequency | ||
| Never | 43.07 (42.47, 43.68) | 2.02 (1.98, 2.05) |
| < monthly | 36.96 (36.48, 37.45) | 2.05 (2.02, 2.08) |
| Once or twice a month | 39.85 (39.03, 40.66) | 2.12 (2.08, 2.17) |
| Once a week | 42.64 (40.82, 44.46) | 2.16 (2.06, 2.26) |
| Several times a week | 45.29 (41.55, 49.04) | 2.51 (2.30, 2.72) |
| Physical activity | ||
| Never | 50.30 (49.14, 51.46) | 2.10 (2.03, 2.17) |
| Casually | 40.10 (39.43, 40.78) | 2.09 (2.05, 2.13) |
| < weekly, but regularly | 38.71 (37.76, 39.67) | 2.08 (2.03, 2.14) |
| Weekly | 38.39 (37.93, 38.84) | 2.03 (2.01, 2.06) |
| Education | ||
| Basic level | 44.26 (43.69, 44.83) | 2.02 (1.99, 2.06) |
| Secondary level | 38.35 (37.88, 38.83) | 2.07 (2.04, 2.09) |
| High level | 34.67 (33.82, 35.52) | 2.13 (2.08, 2.17) |
| Working or studying | ||
| No | 46.10 (45.50, 46.70) | 2.14 (2.10, 2.17) |
| Yes | 36.61 (36.22, 37.00) | 2.01 (1.99, 2.04) |
| Income per consumption unit | ||
| Lowest quartile | 43.75 (43.03, 44.47) | 2.09 (2.05, 2.14) |
| 2nd quartile | 41.03 (40.34, 41.72) | 2.06 (2.02, 2.10) |
| 3rd quartile | 38.72 (38.05, 39.38) | 2.01 (1.98, 2.05) |
| Highest quartile | 36.91 (36.25, 37.57) | 2.07 (2.03, 2.10) |
Note. CI = confidence interval.
Social isolation was measured with a scale from 0 to 100 in which bigger numbers indicate more isolation.
Loneliness was measured with a 5-step scale: 1 (never), 2 (very rarely), 3 (sometimes), 4 (very often), 5 (constantly).
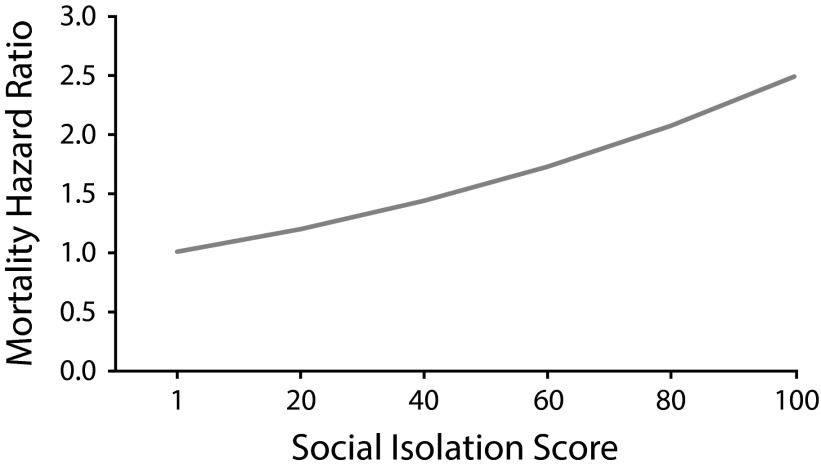
The curvilinear (GAM) analysis revealed that standard linear modeling (e.g., linear Cox regression) was sufficient for modeling connections between social isolation, loneliness, and mortality. The logarithms of hazard functions had linear forms when we modeled the effects of isolation and loneliness. These results suggest that social isolation is gradiently connected to mortality along the whole spectrum of the social isolation index, meaning that not only those who are highly isolated in several ways, but also the less isolated, face risks of mortality.
In separate unadjusted analyses, social isolation (hazard ratio [HR] = 1.040; 95% confidence interval [CI] = 1.037, 1.043) and loneliness (HR = 1.065; 95% CI = 1.007, 1.126) showed significant connections with mortality. The HR of social isolation (1.040) means that the mortality hazard increases 4% for every 1-unit increase on the social isolation scale. The hazard increase does not seem to be big, but on a scale of 0 to 100 the effect multiplies substantially. When we took age and gender into account (partial adjusting), the HR of social isolation dropped substantially (1.015; 95% CI = 1.011, 1.018), but the HR of loneliness increased (1.107; 95% CI = 1.053, 1.164). Examination of social isolation and loneliness simultaneously, in partially adjusted situations, revealed that the HR of social isolation (1.014; 95% CI = 1.010, 1.017) did not appreciably change and the HR of loneliness (1.054; 95% CI = 1.002, 1.109) become almost insignificant.
After we adjusted for all control variables, social isolation and loneliness, when examined separately, were connected to an elevated all-cause mortality risk (model 1 and model 2 in Table 2). When isolation and loneliness were estimated simultaneously (model 3), the effect of loneliness became insignificant, whereas that of social isolation maintained a significant mortality risk (HR = 1.009; 95% CI = 1.006, 1.013). Figure 1 represents the mortality risks of social isolation. For example, the most isolated participants had approximately double the risk of mortality (HR = 2.49) compared with those who were not isolated in any way (Figure 1). Table 2 also presents the HRs for the quintiles of social isolation index to ease the interpretation.
TABLE 2—
Hazard Ratios of Loneliness, Social Isolation and Control Variables in Different Models: Living Conditions Survey of 1994, With Follow-Up to 2011, Finland
| Variable | Model 1, HR (95% CI) | Model 2, HR (95% CI) | Model 3, HR (95% CI) |
| Social isolation | |||
| At 1 scorea | 1.010 (1.006, 1.013) | 1.009 (1.006, 1.013) | |
| At 20 scores | 1.212 (1.208, 1.216) | 1.200 (1.196, 1.204) | |
| At 40 scores | 1.469 (1.464, 1.473) | 1.441 (1.436, 1.446) | |
| At 60 scores | 1.780 (1.774, 1.785) | 1.729 (1.723, 1.735) | |
| At 80 scores | 2.157 (2.150, 2.164) | 2.076 (2.069, 2.082) | |
| At 100 scores | 2.613 (2.605, 2.622) | 2.491 (2.483, 2.500) | |
| Loneliness | 1.064 (1.012, 1.119) | 1.030 (0.978, 1.085) | |
| Age | 1.083 (1.077, 1.089) | 1.087 (1.081, 1.092) | 1.083 (1.077, 1.089) |
| Gender: male | 1.803 (1.608, 2.023) | 1.776 (1.582, 1.993) | 1.816 (1.617, 2.039) |
| Perceived health | |||
| Good (Ref) | 1 | 1 | 1 |
| Fair | 1.317 (1.163, 1.491) | 1.308 (1.155, 1.482) | 1.313 (1.159, 1.488) |
| Poor | 1.863 (1.586, 2.190) | 1.851 (1.573, 2.179) | 1.863 (1.583, 2.193) |
| BMI ≥ 30 kg/m2 | 0.960 (0.831, 1.108) | 0.935 (0.810, 1.080) | 0.951 (0.824, 1.099) |
| Heavy alcohol consumption | |||
| Never (Ref) | 1 | 1 | 1 |
| < monthly | 1.001 (0.866, 1.158) | 0.979 (0.846, 1.132) | 0.995 (0.860, 1.151) |
| Once or twice a month | 1.126 (0.927, 1.367) | 1.114 (0.916, 1.354) | 1.110 (0.913, 1.351) |
| Once a week | 1.320 (0.964, 1.810) | 1.317 (0.958, 1.811) | 1.294 (0.941, 1.780) |
| Several times a week | 1.618 (1.090, 2.400) | 1.595 (1.071, 2.375) | 1.565 (1.050, 2.331) |
| Physical activity | |||
| Weekly (Ref) | 1 | 1 | 1 |
| < weekly, but regularly | 1.051 (0.864, 1.277) | 1.054 (0.867, 1.282) | 1.054 (0.867, 1.282) |
| Casually | 1.051 (0.908, 1.217) | 1.059 (0.914, 1.226) | 1.047 (0.904, 1.212) |
| Never | 1.254 (1.091, 1.440) | 1.351 (1.777, 1.549) | 1.253 (1.089, 1.441) |
| Education | |||
| High level (Ref) | 1 | 1 | 1 |
| Secondary level | 1.151 (0.926, 1.431) | 1.199 (0.964, 1.491) | 1.154 (0.928, 1.436) |
| Basic level | 1.236 (1.000, 1.528) | 1.294 (1.047, 1.601) | 1.248 (1.009, 1.543) |
| Not working or studying | 1.479 (1.264, 1.730) | 1.544 (1.319, 1.806) | 1.495 (1.277, 1.751) |
| Income per consumption unit | |||
| Highest quartile (Ref) | 1 | 1 | 1 |
| 3rd quartile | 1.081 (0.919, 1.271) | 1.081 (0.919, 1.271) | 1.079 (0.917, 1.268) |
| 2nd quartile | 1.131 (0.963, 1.328) | 1.162 (0.990, 1.364) | 1.126 (0.959, 1.322) |
| Lowest quartile | 1.201 (1.016, 1.421) | 1.261 (1.067, 1.490) | 1.194 (1.009, 1.413) |
Notes. CI = confidence interval; HR = hazard ratio.
HRs present a 1-unit increase in social isolation score.
FIGURE 1—
Hazard Function Between Social Isolation and Mortality: Living Conditions Survey of 1994, With Follow-Up to 2011, Finland
The interaction term between loneliness and social isolation was not significant (P = .693), indicating that there was no synergistic effect between social isolation and loneliness on mortality (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). This result supports the idea that social isolation and loneliness have their own separate effects on mortality. The analysis revealed that, besides age, gender was also connected with mortality, the HR for men being almost double that for women. Furthermore, self-reported poor health, frequent heavy alcohol consumption, abstention from physical exercise, low education level, and not working or studying were associated with mortality.
Loneliness, when we examined it simultaneously with social isolation, did not have a significant association with mortality in the final, fully adjusted model. When we omitted control variables 1 at a time, it revealed that self-rated health caused the insignificant effect of loneliness, which may, however, be explained in terms of full mediation between loneliness and mortality via poor self-rated health.
We performed several sensitivity analyses with the fully adjusted model. First, we omitted those who died in the same or following year (n = 129) after baseline measurements from the analysis. Second, we excluded the participants with a long-term illness, inhibiting either substantial (n = 240) or moderate (n = 1036) social interaction, from the analysis. Third, we tested shorter follow-up periods (5 and 10 years) after baseline measurements. The overall results from sensitivity analyses were comparable to the full data results and, more importantly, the effects of social isolation and loneliness were unchanged. The effects of loneliness remained insignificant in all sensitivity analyses and the HR of social isolation remained exactly the same (HR = 1.009) except in the case of the 10-year follow-up period when the HR was slightly higher (HR = 1.011).
DISCUSSION
In this study, the focus was on social relationships and mortality. We selected a large representative sample to examine simultaneously the effects of social isolation and loneliness on mortality over a 17-year follow-up period. The results support the previous studies that established a positive connection between social isolation and mortality.2,5 Furthermore, the results support the contemporary position regarding the functional form of social isolation —to the effect that the connection between social isolation and mortality is clearly linear in nature2—thereby strongly indicating that isolation, even from only a few spheres of social relationship, can have an adverse effect on mortality.
Loneliness, when examined simultaneously with social isolation, did not have a significant effect on mortality in the final, fully adjusted model. This result suggests that loneliness and social isolation have unconnected pathways to mortality. Similar findings were seen in the study of Steptoe et al.,11 in which social isolation had an effect on mortality whereas loneliness was not connected with mortality. The study indicated also that there was no synergistic effect between social isolation and loneliness. The lack of synergistic effect was interesting. One could presume that the mortality risk would escalate for those who are lonely and actually do have a lack of social relationships at the same time, but the interaction effect was not significant. This result supports the standpoint that objective and subjective perspectives of social relationships have their own separate independent pathways to mortality.
A closer examination of the covariates reveal that the nonsignificant effect of loneliness on mortality might be explained by self-rated health, which could act as a full mediator between loneliness and mortality. Similar results have been reported previously.11 Those who reported having poor health also reported the highest levels of loneliness. It is possible that poor health might lead to loneliness, but there is strong evidence showing that loneliness causes poor health.33 Previous studies have established a connection between social relationships and health.21 Specifically, social isolation has been connected to physical or general health whereas loneliness has an impact on mental health.6,12,34 On the other hand, the significance of loneliness may have been overestimated in circumstances in which studies failed to take into account the strength of objective social connections. The low correlation between objective social isolation and the subjective feeling of loneliness indicate that loneliness does not depend on the quantity of social relationships, but rather on the quality and expectations of social relationships.
Strengths and Limitations
This study setting contained some challenges that require new approaches and further research. The first limitation is related to the study design and exposure information. The temporal changes in loneliness and social isolation could not be modeled and, therefore, the analysis was based completely on the baseline measurements of social relationships and covariates. As a consequence, we do not know what other risks (e.g., adverse life events or accumulated social problems) were, possibly, affecting outcomes. However, sensitivity analysis revealed, for example, that the shorter follow-up period did not alter the results.
Despite the limitations, the study has several strengths. First, we used a large representative sample of the Finnish population to increase the external validity of the study. The survey also had a relatively high (73%) response rate, reducing the risk that nonparticipation by socially isolated participants would distort the results. There is slight underrepresentation of divorced and unmarried men in the sample, but that should not compromise the results because their responses were randomly missing. In addition, we used comprehensive questionnaire controls for most of the important background and health-related factors. The prospective design and the statistical models that controlled for baseline health status and other potential confounders—such as alcohol consumption and body mass index—provided evidence for the directionality of the effects. Several sensitivity analyses indicated stability in the main results. We measured loneliness with a single-item measurement and, although the interest lies in the subjective experience of loneliness, the multidimensional measurement would give access, for example, to different dimensions of loneliness (e.g., social and emotional loneliness). There were only 5.2% of respondents in the sample who felt lonely very often or constantly and this might have had an effect on the power of the analyses.
In future research, it might be fruitful to analyze social isolation and its respective consequences for different subgroups within a selected demographic throughout their related life cycles. Presumably the causal mechanisms between social isolation and mortality vary with different age and life phases.
Conclusions
This study shows strong evidence of the adverse effect of social isolation on mortality. The connection remained significant when studied simultaneously with loneliness and with adjustment for multiple potential confounders. Loneliness was not significantly connected to mortality when examined concurrently with social isolation. The results imply that the risk of mortality exists along a continuum, affecting not only those who experience extreme isolation, but also those who suffer from mild to progressively increasing intensity of social isolation. This result is important in planning of public health interventions as it indicates that health benefits from varied networks. Varied connections are likely to include particularly useful ones that foster responsibility and concern for others or self and possibly provide information on healthy habits. In addition, when we are planning interventions, we should not conflate being isolated and feeling lonely, because these conditions require a particular diagnosis and a specific intervention.
Our study emphasizes the detrimental role of social isolation. We may assume that certain social environments foster social isolation, and, therefore, we need to know how common isolation is among different subpopulations and what the role of social infrastructure is. Our study indicated, and confirmed findings of previous studies, that young people, senior citizens, and the less well educated are particularly socially isolated. These are specific target groups for interventions. In general, policies that focus on social ties may potentially be a cost-effective strategy for enhancing public health and well-being at the population level.
ACKNOWLEDGMENTS
This research was supported by the Kone Foundation.
The authors are grateful to the anonymous reviewers for their constructive comments.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed because there were no human participants in the study.
REFERENCES
- 1.Hyyppä MT, Mäki J, Impivaara O, Aromaa A. Individual-level measures of social capital as predictors of all-cause and cardiovascular mortality: a population-based prospective study of men and women in Finland. Eur J Epidemiol. 2007;22(9):589–597. doi: 10.1007/s10654-007-9153-y. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 3.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 4.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056–2062. doi: 10.2105/AJPH.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss RS. Loneliness: The Experience of Emotional and Social Isolation. Cambridge, MA: MIT Press; 1973. [Google Scholar]
- 8.Victor CR, Scambler SJ, Bowling A, Bond J. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc. 2005;25(6):357–375. [Google Scholar]
- 9.Peplau LA, Miceli M, Morasch B. Loneliness and self-evaluation. In: Peplau LA, Perlman D, editors. Loneliness: A Sourcebook of Current Theory, Research and Therapy. New York, NY: Wiley; 1982. pp. 135–151. [Google Scholar]
- 10.Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health. 2012;24(8):1346–1363. doi: 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- 13.Heffner KL, Waring ME, Roberts MB, Eaton CB, Gramling R. Social isolation, C-reactive protein, and coronary heart disease mortality among community-dwelling adults. Soc Sci Med. 2011;72(9):1482–1488. doi: 10.1016/j.socscimed.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eng PM, Rimm EB, Fitzmaurice G, Kawachi I. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol. 2002;155(8):700–709. doi: 10.1093/aje/155.8.700. [DOI] [PubMed] [Google Scholar]
- 15.Brummett BH, Barefoot JC, Siegler IC et al. Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosom Med. 2001;63(2):267–272. doi: 10.1097/00006842-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Patterson AC, Veenstra G. Loneliness and risk of mortality: a longitudinal investigation in Alameda County, California. Soc Sci Med. 2010;71(1):181–186. doi: 10.1016/j.socscimed.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 17.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golden J, Conroy RM, Bruce I et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int J Geriatr Psychiatry. 2009;24(7):694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- 21.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51(suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 23.Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(3, suppl):S39–S52. [PubMed] [Google Scholar]
- 24.Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–1111. doi: 10.1200/JCO.2005.04.2846. [DOI] [PubMed] [Google Scholar]
- 25.House JS. Social isolation kills, but how and why? Psychosom Med. 2001;63(2):273–274. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 27.Vonneilich N, Jöckel K-H, Erbel R et al. Does socioeconomic status affect the association of social relationships and health? A moderator analysis. Int J Equity Health. 2011;10:43. doi: 10.1186/1475-9276-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: changes in core discussion networks over two decades. Am Sociol Rev. 2006;71(3):353–375. [Google Scholar]
- 29.Taylor SE, Seeman TE. Psychosocial resources and the SES–health relationship. Ann N Y Acad Sci. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- 30.Stringhini S, Berkman L, Dugravot A et al. Socioeconomic status, structural and functional measures of social support, and mortality: The British Whitehall II Cohort Study, 1985–2009. Am J Epidemiol. 2012;175(12):1275–1283. doi: 10.1093/aje/kwr461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ahola A, Djerf K, Heiskanen M, Vikki K. Survey of Living Conditions 1994. Data Collection [in Finnish]. Helsinki, Finland: Living Conditions 2; 1995.
- 32.Wood SN. Generalized Additive Models: An Introduction with R. Boca Raton, FL: Chapman and Hall/CRC; 2006. [Google Scholar]
- 33.Cacioppo JT, Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation. Soc Personal Psychol Compass. 2014;8(2):58–72. doi: 10.1111/spc3.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin Psychol Rev. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]