Abstract
Objectives. To compare blood lead levels (BLLs) among US children aged 1 to 5 years according to receipt of federal housing assistance.
Methods. In our analyses, we used 2005 to 2012 data for National Health and Nutrition Examination Survey (NHANES) respondents that were linked to 1999 to 2014 administrative records from the US Department of Housing and Urban Development (HUD). After we restricted the analysis to children with family income-to-poverty ratios below 200%, we compared geometric mean BLLs and the prevalence of BLLs of 3 micrograms per deciliter or higher among children who were living in assisted housing at the time of their NHANES blood draw (n = 151) with data for children who did not receive housing assistance (n = 1099).
Results. After adjustment, children living in assisted housing had a significantly lower geometric mean BLL (1.44 µg/dL; 95% confidence interval [CI] = 1.31, 1.57) than comparable children who did not receive housing assistance (1.79 µg/dL; 95% CI = 1.59, 2.01; P < .01). The prevalence ratio for BLLs of 3 micrograms per deciliter or higher was 0.51 (95% CI = 0.33, 0.81; P < .01).
Conclusions. Children aged 1 to 5 years during 2005 to 2012 who were living in HUD-assisted housing had lower BLLs than expected given their demographic, socioeconomic, and family characteristics.
Lead exposure among children is linked to many adverse effects on health and cognitive development, which can be irreversible.1 Blood lead levels (BLLs) in the United States have decreased substantially over the past 40 years as a result of the removal of lead from gasoline, residential paint, and solder used for water pipes and food and drink cans1–3; however, ingestion of lead-based paint, particularly prevalent in older housing, remains one of the most common sources of lead exposures among young children.4 Despite declining BLLs in the United States, children aged 1 to 5 years5 and children living in poverty3,6 remain more likely than older children and children not living in poverty, respectively, to have higher levels of lead in their blood.
The rental assistance programs of the US Department of Housing and Urban Development (HUD) provide affordable housing for low-income individuals and families, including nearly 4 million children.7 The National Center for Health Statistics (NCHS) has linked 1999 to 2012 National Health and Nutrition Examination Survey (NHANES) data to administrative data for HUD’s largest rental assistance programs (1999–2014),8,9 and these linked NHANES–HUD data allow calculation of the first-ever national BLL estimates among children living in HUD-assisted housing. Here we compare BLLs among children aged 1 to 5 years in 2005 to 2012 who received housing assistance during 1999 to 2014 with levels among children who did not receive housing assistance during that period.
METHODS
NHANES is a cross-sectional, multistage probability sampling survey conducted by NCHS; the survey is designed to assess the health and nutritional status of noninstitutionalized civilians living in the United States through interviews and physical examinations.10 Between 2005 and 2012, 5139 children aged 1 to 5 years were interviewed for NHANES (response rate: 88%), and 4908 (96%) participated in the examination component.10 Individuals aged 1 year and older who underwent physical examinations were eligible for blood lead measurements.
Data from linkage-eligible 2005 to 2012 NHANES respondents were linked with data for the same individuals in the 1999 to 2014 administrative records of HUD’s largest rental assistance programs, namely public housing, housing choice vouchers, and privately owned, subsidized multifamily housing.8 Linkage eligibility was based on the respondent (or adult proxy when the respondent was a child) providing sufficient identifying information and informed consent for future administrative linkage projects. Linkage-eligibility rates among respondents ranged from 60% to 71% for the survey cycles included in our analysis (2005–2012).11 Linked individuals were identified through exact matches on the following personal identifiers: 9-digit Social Security number, gender, and month and year of birth. Linked data were obtained from the NCHS–HUD data linkage program through a data-use agreement for restricted-use data.
Receipt of Housing Assistance
We defined receipt of housing assistance as linkage to the 1999 to 2014 HUD administrative records before but not during the time of the NHANES examination, at the time of the NHANES examination, or only after the NHANES examination. Respondents without a link to the HUD administrative records were considered to not have received housing assistance during 1999 to 2014. Recoded variables from the linked files were used to define assisted-housing status8; all other variables included in the analysis were derived from NHANES data.
Blood Lead Levels
Whole blood specimens were collected by phlebotomists at the NHANES mobile examination center (MEC) in an ethylenediaminetetraacetic acid–coated tube via venipuncture, after which they were processed on site and stored frozen before being shipped on dry ice to the National Center for Environmental Health, where heavy metal assays were performed. Blood specimens remained frozen until they were analyzed. Inductively coupled plasma mass spectrometry with a limit of detection of 0.25 micrograms per deciliter was used to measure lead concentrations.12
Demographic and Family Characteristics
Data collected in NHANES and examined in our analysis included child age at screening, gender, race/ethnicity (Mexican American, non-Hispanic Black, non-Hispanic White, other), nativity, health insurance coverage, proxy-reported health status (excellent/very good vs good/fair/poor), and mother’s age at child’s birth. Data were also collected on the gender, marital status, educational attainment, and interview language of the household reference person (an adult living with the child who served as the head of the household).
In addition, information was collected on household size, family income-to-poverty ratio (IPR), and participation in federal nutrition assistance programs. IPR was based on reported family income and household composition relative to US Department of Health and Human Services poverty guidelines, set by year and state of residence. Data were also collected on household participation in the Supplemental Nutrition Assistance Program in the preceding 12 months and receipt of benefits from the Special Supplemental Nutrition Program for Women, Infants, and Children in the preceding 12 months.
Finally, data were collected on census region and division, calendar period of examination (to account for seasonal influences on lead exposure13), survey cycle (2005–2006, 2007–2008, 2009–2010, 2011–2012), urban–rural classification (ranging from noncore areas to large central metropolitan areas),14 home ownership status (owned vs rented), and number of rooms in the home. Also, we estimated the prevalence of anemia (identified as a hemoglobin level below 11 g/dL15) given that this condition can be caused by exposure to lead.1
Statistical Analysis
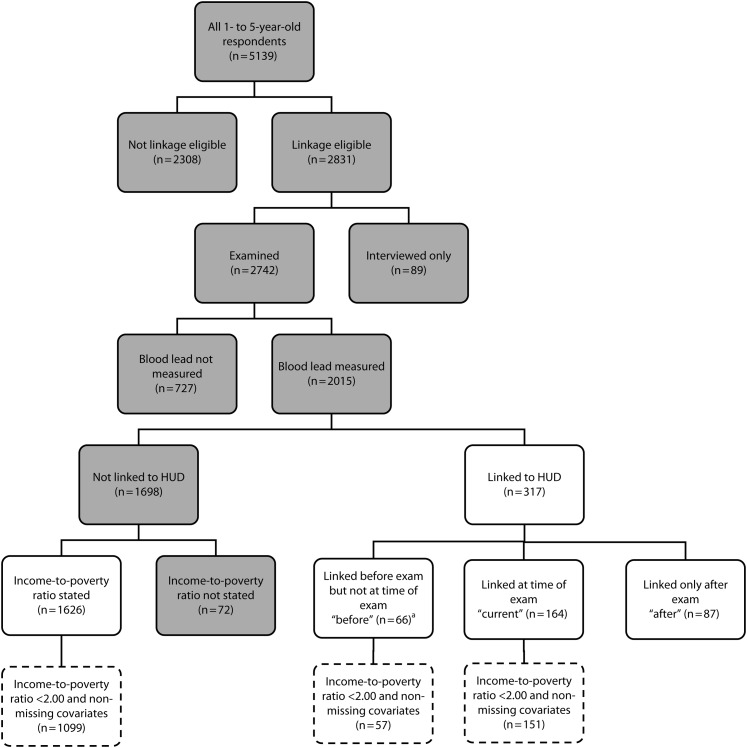
We limited our analysis to linkage-eligible children aged 1 to 5 years who participated in the 2005 to 2012 NHANES MEC component and had complete data on blood lead measurements. In addition, we excluded children without a linkage to the 1999 to 2014 HUD administrative records who had missing IPR data (Figure 1). These restrictions resulted in an analytic sample of 1943 children. All analyses accounted for the survey’s multistage, complex sampling design and employed linkage-eligible adjusted MEC weights (hereafter called “sample” weights); specifically, data on linkage-eligible respondents who underwent an examination were reweighted to reflect the age, gender, and race/ethnicity distributions of all noninstitutionalized civilians living in the United States during each survey cycle.8
FIGURE 1—
Flowchart of Analytic Sample Selection Criteria
Note. White boxes indicate respondents included in the analytic sample, and dashed boxes indicate respondents included in the propensity score analysis (2005–2012 National Health and Nutrition Examination Survey [NHANES] data linked to 1999–2014 Department of Housing and Urban Development [HUD] administrative records).
aIncludes 29 children linked to HUD after the NHANES examination.
We examined respondent characteristics by assisted-housing status, comparing children living in assisted housing at the time of the examination with children who did not receive housing assistance during 1999 to 2014. Income limits for eligibility to receive housing assistance are either 50% or 80% (depending on the locality) of the area median family income.16 To create low-income comparison groups, we stratified those who did not receive housing assistance (by IPR) into the following categories: IPR below 0.50, IPR between 0.50 and 0.99, IPR between 1.00 and 1.99, and IPR of 2.00 or above (with an IPR of 1.00 being equivalent to 100% of the poverty threshold).
In a secondary analysis, we created a collapsed category for children living in assisted housing before the time of their examination, at the time of their examination, or both (the “combined group” of children) because BLLs in children are a function of both current exposure to lead and accumulated body burden from birth17; thus, previous housing conditions may also be important with respect to current BLLs. All analyses of the association between housing assistance and BLLs excluded children who received housing assistance only after the NHANES examination.
BLL values were log-transformed to better approximate a normal distribution. We used an unadjusted linear regression of log(BLL) to estimate geometric mean BLLs for children receiving housing assistance at the time of their examination versus non-housing-assisted children. Analyses were repeated for the combined group of children versus non-housing-assisted children. A second set of unadjusted logistic regression models was used to estimate prevalence ratios (with predicted margins) for BLLs of 3 micrograms per deciliter or higher. Although 5 micrograms per deciliter is the current reference value for high BLLs among children,6 our preliminary investigation showed that prevalence estimates of 5 micrograms per deciliter or higher were too low to be reliably estimated by housing assistance status. Thus, to improve statistical reliability, we present results based on a prevalence of 3 micrograms per deciliter or higher. Recent evidence suggests that higher BLLs are associated with compromised neurodevelopment, even among children with low lead levels.18
Using propensity score (PS) weighting, we conducted adjusted analyses to assess whether BLLs among housing-assisted children were the same as those in a comparable group of non-housing-assisted children. The estimand of interest was the population average treatment effect on the treated, that is, the difference in BLLs when comparing a group of children in assisted housing with the same group of children had they not received housing assistance. We used PS methods because children in assisted housing might have different characteristics than children not in assisted housing and, in the case of insufficient overlap between the groups, multivariable regression models might not adequately control for confounding.19
Propensity Score Estimation
PSs were estimated via a logistic regression model for children receiving housing assistance at the time of their examination in comparison with children not in assisted housing (in a secondary analysis, this procedure was repeated for the combined group of children in comparison with children not in assisted housing). Factors that were related to both housing assistance20,21 and BLLs1,3,20,22 but were not considered intermediates along the causal pathway were selected as predictor variables (for all of the factors examined; Table A, available as a supplement to the online version of this article at http://www.ajph.org). PS models included child age at screening, gender, race/ethnicity, mother’s age at child’s birth, and health insurance coverage; the gender, marital status, and educational attainment of the household reference person; household size; family IPR; census division; calendar quarter of examination; survey cycle; and urban–rural classification.14
In addition, as recommended for PS analyses with complex survey designs, the sample weight (along with a squared term to account for nonlinearity20) was included as a predictor.23 Because the addition of stratum and primary sampling unit led to the models failing to converge, these sample design variables were consequently removed.
We examined PS distributions in the treatment and comparison groups with box plots to assess the overlap between the groups in the probability distribution for receiving housing assistance (i.e., common support; Figures A and B, available as supplements to the online version of this article at http://www.ajph.org). Initially, we defined all children who did not receive housing assistance during 1999 to 2014 as our comparison group. However, because HUD eligibility requirements are based on income, children living in families above 200% of the poverty threshold had close to zero probability of receiving housing assistance. To increase the overlap between the groups in terms of probability of receiving housing assistance, we restricted the analyses to children with family IPRs below 200%. The final sample sizes for the unadjusted and propensity-score-weighted comparisons were as follows: children receiving housing assistance at the time of their examination, 151; combined group of children, 208; and children without housing assistance, 1099 (Figure 1).
Propensity Score Application
PSs were applied through the strategy of weighting by the odds, with housing-assisted children receiving a weight of 1 and the comparison group of children without housing assistance receiving a weight of PS/(1 − PS). These weights were then multiplied by the sample weight to create a new composite weight, which was used along with strata and primary sampling units in the final model in a manner consistent with previous applications of PSs to complex survey designs.23–25
Covariate balance was assessed through inspection of standardized biases before and after PS weighting (Figures C and D, available as supplements to the online version of this article at http://www.ajph.org). Standardized biases were calculated as the difference in population-weighted proportions (or means in the case of continuous variables) between the treatment and comparison groups divided by the standard deviation in the treatment group.24,26 After PS weighting, all standardized biases were between −0.25 and 0.25, indicating adequate covariate balance.19 The variables included as predictors in the PS models were also included as covariates in the outcome models, consistent with recommendations.19 Additional PS estimation methods for complex survey designs were explored27; results are provided in the appendix, available as a supplement to the online version of this article at http://www.ajph.org.
Sensitivity Analyses
To determine erythrocyte lead levels, which may be a more accurate approximation of lead exposure status, we repeated our analysis and used hematocrit-corrected BLLs.28 Estimates and confidence intervals (CIs) for mean BLLs with and without this correction were similar. Therefore, for ease of understanding, we present non-hematocrit-corrected values.
Because of concerns about linkage-adjusted sample weights not adequately correcting for the approximately 27% (n = 727) of linkage-eligible examined children whose BLLs were not measured and the 3% (n = 72) of nonlinked children with missing IPR values (Figure 1), we used the Markov chain Monte Carlo method to impute log(BLL) and IPR (n = 10 imputations). This method assumes that missing data are multivariate normal and missing at random. The variables chosen for the imputation model were the same as those selected for the PS models. Estimates of mean BLLs by housing assistance status based on imputed data were similar to those based on observed data, providing evidence that linkage-adjusted sample weights adequately corrected for selection bias in this analysis (see Table B, available as a supplement to the online version of this article at http://www.ajph.org).
All of our analyses were conducted with SAS version 9.4 (SAS Institute Inc, Cary, NC) and SAS-callable SUDAAN version 11.0 (RTI International, Research Triangle Park, NC).
RESULTS
Between 2005 and 2012, approximately 11.8% (SE = 1.4) of children aged 1 to 5 years old lived in HUD-assisted housing at some point during the period assessed (1999–2014): 6.0% (SE = 0.7) were living in assisted housing at the time of the NHANES examination, 2.6% (SE = 0.6) lived in assisted housing before but not at the time of the examination, and 3.2% (SE = 0.4) lived in assisted housing only after the time of the examination. Of the children in assisted housing at the time of the examination, 53.0% (SE = 7.0) lived in households receiving a housing choice voucher, 25.5% (SE = 5.2) were in public housing, and 21.5% (SE = 5.9) were in multifamily housing programs (data not shown).
Characteristics of children living in assisted housing at the time of or before the examination and non-housing-assisted children are shown in Table 1. Children categorized as currently in assisted housing differed from non-housing-assisted children with respect to a number of characteristics; for example, they were more likely to live below the poverty threshold (80% vs 26%), to be of non-Hispanic Black race/ethnicity (50% vs 10%), to have a mother who was younger than 20 years at the time of their birth (16% vs 10%), to have nonprivate health insurance (88% vs 44%), to live in a household with 2 members (11% vs 3%), and to have a household reference person who was female (84% vs 47%), was unmarried (74% vs 26%), or did not have a high school diploma (43% vs 23%; χ2 P < .05 for each comparison; Table A).
TABLE 1—
Selected Demographic and Family Characteristics of US Children Aged 1–5 Years, by Housing Assistance Status: National Health and Nutrition Examination Survey (NHANES), United States, 2005–2012
| Resided in HUD-Assisted Housing During 1999–2014 |
Did Not Reside in HUD-Assisted Housing During 1999–2014 |
|||||
| Characteristic | Currenta (n = 164), % (SE) | Current+Beforeb (n = 230), % (SE) | IPR < 0.50 (n = 189), % (SE) | IPR 0.50–0.99 (n = 385), % (SE) | IPR 1.00–1.99 (n = 532), % (SE) | IPR ≥ 2.00 (n = 520), % (SE) |
| All | 6.0 (0.7) | 8.7 (1.1) | 7.9 (0.9) | 14.9 (1.1) | 27.3 (1.6) | 38.1 (2.2) |
| Race/ethnicityc,d | ||||||
| Mexican American | 9.4e (2.8) | 10.9 (2.9) | 36.6 (7.0) | 37.3 (4.2) | 19.9 (2.4) | 11.1 (1.3) |
| Non-Hispanic White | 17.6e (7.2) | 24.6e (8.7) | 22.8 (5.7) | 30.6 (3.9) | 53.2 (3.9) | 71.1 (2.5) |
| Non-Hispanic Black | 50.3 (7.0) | 46.1 (7.1) | 14.7 (3.5) | 12.5 (2.2) | 10.8 (1.3) | 7.5 (1.3) |
| Other | 22.6 (4.6) | 18.5 (4.0) | 25.9 (5.2) | 19.7 (3.0) | 16.1 (2.6) | 10.4 (1.5) |
| Gender of household reference personc,f | ||||||
| Male | 15.8e (6.0) | 21.4 (6.0) | 34.6 (4.7) | 43.1 (3.5) | 51.3 (4.2) | 62.6 (2.9) |
| Female | 84.2 (6.0) | 78.6 (6.0) | 65.4 (4.7) | 56.9 (3.5) | 48.7 (4.2) | 37.4 (2.9) |
| Marital status of household reference personc,f | ||||||
| Not married | 74.3 (5.4) | 69.2 (6.1) | 55.7 (4.2) | 40.0 (3.3) | 29.5 (3.5) | 11.4 (1.6) |
| Married | 20.7e (6.3) | 25.2 (7.2) | 39.6 (4.1) | 55.4 (3.4) | 67.7 (3.5) | 86.8 (1.6) |
| Not stated | 5.0e (2.1) | 5.7e (1.8) | 4.6e (1.5) | 4.6 (1.0) | 2.8e (1.1) | 1.7e (0.7) |
| Education of household reference personc,f | ||||||
| At least high school diploma | 57.5 (5.0) | 64.9 (3.5) | 43.1 (3.7) | 54.5 (3.8) | 74.2 (3.5) | 94.9 (0.9) |
| No high school diploma | 42.5 (5.0) | 35.1 (3.5) | 56.9 (3.7) | 45.5 (3.8) | 25.8 (3.5) | 5.1 (0.9) |
| Maternal age at birth, yc | ||||||
| < 20 | 16.4 (3.9) | 23.0 (3.5) | 22.9 (3.4) | 15.7 (2.4) | 11.7 (2.1) | 3.5 (0.7) |
| 20–29 | 64.0 (4.9) | 58.4 (3.9) | 57.4 (4.2) | 57.4 (3.1) | 60.6 (2.8) | 42.3 (3.3) |
| ≥ 30 | 19.7 (4.0) | 18.6 (3.6) | 19.7 (3.5) | 26.9 (3.0) | 27.8 (3.0) | 54.2 (3.3) |
| Health insurance coveragec | ||||||
| Private insurance | 8.3e (2.8) | 9.0e (2.9) | 2.8e (1.2) | 7.4 (1.3) | 34.2 (3.7) | 78.9 (2.1) |
| Other insurance | 88.2 (3.2) | 85.2 (3.3) | 90.3 (2.7) | 81.3 (2.1) | 51.5 (3.1) | 13.6 (1.7) |
| Uninsured | 3.5e (1.6) | 5.9e (1.8) | 7.0e (2.6) | 11.3 (1.8) | 14.3 (2.6) | 7.5 (1.4) |
| Household sizec | ||||||
| 2 | 11.1 (2.4) | 9.0 (1.9) | 4.1e (1.6) | 2.0e (0.7) | 4.0 (1.1) | 1.7e (0.7) |
| 3 | 25.1 (4.1) | 22.5 (3.6) | 18.2 (3.3) | 12.3 (2.1) | 15.9 (2.4) | 22.8 (2.5) |
| ≥ 4 | 63.9 (4.8) | 68.5 (4.2) | 77.8 (3.4) | 85.7 (2.1) | 80.1 (2.7) | 75.6 (2.6) |
Note. HUD = Department of Housing and Urban Development; IPR = income-to-poverty ratio. In some cases, information was missing or not stated for education of the household reference person (n = 43) and health insurance coverage (n = 1). The table excludes children linked to the HUD 1999–2014 administrative records only after the NHANES examination (n = 87); these children represented 3.2% (SE = 0.4) of our analytic sample (n = 1943).
Includes children in households receiving housing assistance at the time of the NHANES examination.
Includes children in households receiving housing assistance before the NHANES examination, at the time of the NHANES examination, or both.
χ2 P < .01 for comparison between children living in assisted housing at the time of the examination and children who did not receive housing assistance during 1999–2014 (see Table A for other characteristics examined).
“Other” includes Hispanic or Latino other than Mexican American and non-Hispanic of races other than Black and White, including multiracial.
Relative standard error > 0.30.
The household reference person for NHANES was an adult living with the child who served as the head of the household.
Blood Lead Levels
Between 2005 and 2012, the overall mean BLL of children aged 1 to 5 years was 1.27 micrograms per deciliter (95% CI = 1.21, 1.33). The overall percentages of children with BLLs of 3 micrograms per deciliter or higher, 5 micrograms per deciliter or higher, and 10 micrograms per deciliter or higher were, respectively, 8.4% (95% CI = 6.7, 10.1), 2.7% (95% CI = 1.9, 3.5), and 0.7% (95% CI = 0.3, 1.2; data not shown).
Among children living in assisted housing at the time of their examination or not receiving housing assistance during 1999 to 2014, those with BLLs of 3 micrograms per deciliter or higher were more likely than those with lower BLLs to live below the poverty threshold (48% vs 28%), be non-Hispanic Black (26% vs 11%), have nonprivate health insurance (67% vs 45%), reside in the Northeast (29% vs 10%), and have a household reference person who was female (58% vs 48%), was unmarried (40% vs 28%), or did not have a high school diploma (43% vs 23%; χ2 P < .05 for each comparison; Table A).
Housing Assistance and Blood Lead Levels
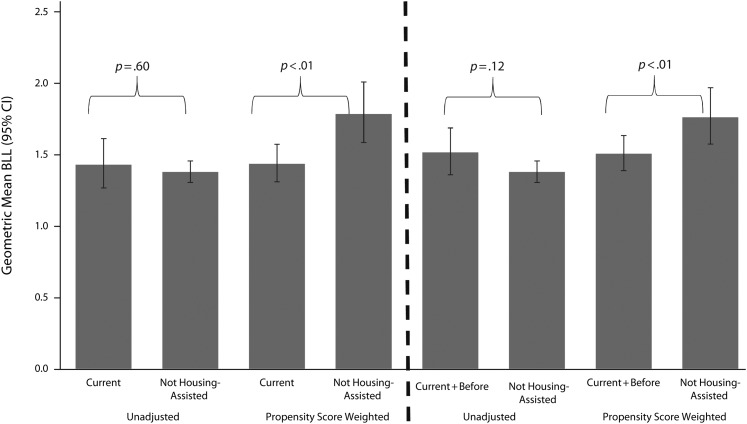
In the group of children with family incomes below 200% of the poverty threshold, the unadjusted mean BLL among those living in assisted housing at the time of their examination (1.43 µg/dL; 95% CI = 1.27, 1.61) was not significantly different from that among non–housing-assisted children (1.38 µg/dL; 95% CI = 1.31, 1.4; P = .60; Figure 2). After adjustment by PS weighting, children in assisted housing had a significantly lower mean BLL (1.44 µg/dL; 95% CI = 1.31, 1.57) than non-housing-assisted children (1.79 µg/dL; 95% CI = 1.59, 2.01; P < .01).
FIGURE 2—
Geometric Mean Blood Lead Levels Among US Children Aged 1–5 Years With Income-to-Poverty Ratios < 2.00, by Housing Assistance Status: National Health and Nutrition Examination Survey (NHANES), United States, 2005–2012
Note. BLL = blood lead level; CI = confidence interval. “Current” includes children in households receiving housing assistance at the time of the NHANES examination (n = 151). “Current+before” includes children in households receiving housing assistance before the NHANES examination, at the time of the NHANES examination, or both (n = 208). Not housing assisted includes children in households that did not receive housing assistance during 1999 to 2014 (n = 1099).
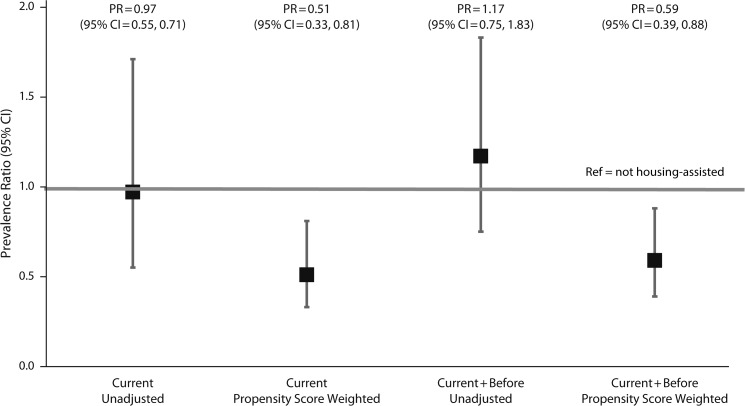
Prevalence estimates of BLLs of 3 micrograms per deciliter or higher among children living in assisted housing at the time of their examination and non-housing-assisted children were 10.6% and 10.9%, respectively, yielding an unadjusted prevalence ratio of 0.97 (95% CI = 0.55, 1.71; P = .92; Figure 3; Figure E, available as a supplement to the online version of this article at http://www.ajph.org). After adjustment by PS weighting, the prevalence of BLLs of 3 micrograms per deciliter or higher among children in assisted housing was 11.0%, which was approximately half the prevalence estimate for non-housing-assisted children (21.5%; adjusted prevalence ratio = 0.51; 95% CI = 0.33, 0.81; P < .01).
FIGURE 3—
Prevalence Ratios for Blood Lead Levels of ≥ 3 µg/dL Among US Children Aged 1–5 Years With Income-to-Poverty Ratios Below 2.00, by Housing Assistance Status: National Health and Nutrition Examination Survey (NHANES), United States, 2005–2012
Note. CI = confidence interval; PR = prevalence ratio. “Current” includes children in households receiving housing assistance at the time of the NHANES examination (n = 151). “Current+before” includes children in households receiving housing assistance before the NHANES examination, at the time of the NHANES examination, or both (n = 208). Not housing assisted includes children in households that did not receive housing assistance during 1999 to 2014 (n = 1099).
Findings were similar when children living in assisted housing before the time of their examination, at the time of their examination, or both were compared with non-housing-assisted children (Figures 2 and 3).
DISCUSSION
In our analysis of US children aged 1 to 5 years with family incomes below 200% of the poverty threshold, our unadjusted results showed that BLLs among children living in federally assisted housing were not significantly different from BLLs among those who did not receive housing assistance. However, after adjustment for potential confounders, children living in federally assisted housing had lower BLLs than would be expected given their demographic, socioeconomic, and family characteristics. The interpretation of findings was similar when we examined the prevalence of children with BLLs of 3 micrograms per deciliter or higher and when we included children who lived in assisted housing before the time of their blood draw, at the time of their blood draw, or both.
The literature on BLLs among residents of federally assisted housing is sparse. To our knowledge, the only previous study evaluating BLLs among children according to housing assistance status was conducted by Rabito et al. in New Orleans in 1998 and involved children 6 to 71 months of age who received blood lead screening from a public health clinic.20 The results of that study showed a higher proportion of children with BLLs of 10 micrograms per deciliter or above among those residing in public housing developments than among those not residing in such developments (32% vs 28%). However, that study was conducted almost 20 years ago, when BLLs were much higher than they are today; in addition, it was conducted in one US city, among only children screened in public health clinics, and with public housing defined as residence in a public housing development. Therefore, the Rabito et al. findings may not reflect associations at a national level with more recent data and with housing assistance more broadly defined.
Furthermore, although that study’s final adjusted model revealed no significant differences in childhood BLLs of 10 micrograms per deciliter or higher by public housing residence, the model adjusted for age of housing, a potential causal intermediate, which could have introduced overadjustment bias.29 Also, the findings could have been residually confounded by many of the demographic, socioeconomic, and family characteristics included in our analysis but not included by Rabito et al.
There have been several legislative efforts to protect children from lead paint exposure. For example, the Lead-Paint Poisoning Prevention Act (42 US Code Chap. 63), passed in 1971, sought to protect children in public housing developments from exposure. The Residential Lead-Based Paint Hazard Reduction Act of 1992 (Title X) mandated, among many policies, lead-based paint inspections and hazard control plans for those living in most housing units built before 1978 that receive financial assistance from HUD, including units occupied by tenants with housing vouchers.30 The Lead-Safe Housing Rule (24 CFR 35), which took effect in 2000, implemented the new requirements, concepts, and terminologies established by Title X.31
Although non-assisted housing has also benefited from the lead disclosure legislation enacted as part of Title X, efforts to prevent lead exposure in non-assisted housing primarily rely on voluntary rather than mandatory compliance.20 A recent nationwide survey revealed a lower prevalence of lead-based hazards associated with receipt of government housing assistance than with no receipt of assistance4; however, children can also be exposed to lead through sources other than the home, and these categories fall outside the scope of Title X and its lead paint regulations.
Limitations
This analysis involves limitations. For instance, our referent group for the analysis was children aged 1 to 5 years between 2005 and 2012 who did not link to 1999 to 2014 administrative records from HUD’s largest rental assistance programs (and whose family incomes were below 200% of the poverty threshold). Although we considered this group of children as having not received housing assistance, this might not have been true. Children could have been erroneously classified as not receiving housing assistance as a result of inconsistent identifying information required for the linkage algorithm or incorrect specifications of the dates defining entry into or exit from HUD-assisted housing, which were used in the HUD–NCHS linkage protocol to categorize respondents’ assisted-housing status.8
Furthermore, the HUD administrative records were available only up until 2014; therefore, some children may have entered into assisted housing at some point after 2014 but were considered to not have received housing assistance in our analysis. In addition, approximately one third of the children (31.4%; SE = 8.0) identified as receiving housing assistance before but not at the time of their examination were linked to HUD after the examination, raising concerns about misclassification of current assisted-housing status. However, in our secondary analysis, we collapsed children in HUD-assisted housing before the examination with those in HUD-assisted housing at the time of the examination, which would have partially corrected for this misclassification. Also, a separate tabulation of 2011 American Housing Survey data confirmed our estimate that 6.0% of US children aged 1 to 5 years (approximately 880 000 children) were living in assisted housing on any given day (B. A. Haley, unpublished data, 2016).
In addition, the small sample size of children currently receiving housing assistance precluded stratifying the analysis according to type of housing assistance. As a result of reliability concerns, we were also not able to present prevalence estimates associated with BLLs of 5 micrograms per deciliter or higher, currently considered the reference value for high BLLs among children.6
Strengths
In terms of study strengths, our investigation is the first to our knowledge to examine BLLs in a nationally representative sample of US children receiving housing assistance and to compare these children with comparable children not receiving housing assistance. The HUD–NHANES linkage algorithm required a stringent match of personal identifiers, minimizing the number of false positives, which was especially important for identifying a relatively low-prevalence characteristic such as receipt of housing assistance.
We used PS weighting methods to adjust for potential confounders, excluding potential causal intermediates in the PS models (e.g., current health conditions and housing information), which could have led to an underestimation of the total effect of housing assistance on BLLs.20,29 In sensitivity analyses, we used multiple imputation to estimate the magnitude of potential selection bias introduced by excluding children who were examined in NHANES but did not have their blood lead measured; the findings indicated that the linkage-adjusted sample weights appeared to adequately correct for this potential selection bias. Also, in line with studies that suggest there is no clear threshold for lead’s effect on cognitive development, we modeled BLLs as a continuous outcome.18
Public Health Implications
In conclusion, in a nationally representative sample of US children aged 1 to 5 years in 2005 to 2012, children receiving federal housing assistance had lower blood lead levels than expected given their demographic, socioeconomic, and family characteristics. Our study adds to the literature describing how factors related to housing conditions and stability are associated with health among US children and can help inform future research.32,33
ACKNOWLEDGMENTS
This work was performed under employment of the US federal government; the authors did not receive any outside funding.
Findings from our analysis were presented at the Epidemiology Congress of the Americas in Miami, FL, in June 2016.
We thank Jon Sperling, senior policy analyst, Geographic Information and Analysis, Department of Housing and Urban Development (HUD), for facilitating the HUD data linkage collaboration with the National Center for Health Statistics (NCHS); Makram Talih, associate director for science, Office of Analysis and Epidemiology, NCHS, for providing a critical review of the article; and Warren Friedman, senior advisor to the director, Office of Lead Hazard Control and Healthy Homes, HUD, for his review of the text describing lead hazard control legislation.
Note. The findings and conclusions presented in this article are those of the authors and do not necessarily represent the official positions of the National Center for Health Statistics, the Centers for Disease Control and Prevention, or the Department of Housing and Urban Development.
HUMAN PARTICIPANT PROTECTION
No institutional review board protocol approval was needed for this study because secondary data were used.
Footnotes
See also Galea and Vaughan, p. 1901.
REFERENCES
- 1.Environmental Protection Agency. Integrated science assessment for lead. Available at: https://cfpub.epa.gov/ncea/isa/recordisplay.cfm?deid=255721. Accessed August 30, 2016.
- 2.Pirkle JL, Brody DJ, Gunter EW et al. The decline in blood lead levels in the United States: the National Health and Nutrition Examination Surveys (NHANES) JAMA. 1994;272(4):284–291. [PubMed] [Google Scholar]
- 3.America’s Children: Key National Indicators of Well-Being. Washington, DC: Federal Interagency Forum on Child and Family Statistics; 2015. [Google Scholar]
- 4.Dewalt FG, Cox DC, O’Haver R et al. Prevalence of lead hazards and soil arsenic in U.S. housing. J Environ Health. 2015;78(5):22–29. [PubMed] [Google Scholar]
- 5.Wheeler W, Brown MJ. Blood lead levels in children aged 1-5 years—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(13):245–248. [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Update on blood lead levels in children. Available at: http://www.cdc.gov/nceh/lead/ACCLPP/blood_lead_levels.htm. Accessed August 30, 2016.
- 7.Center on Budget and Policy Priorities. Policy basics: federal rental assistance. Available at: http://www.cbpp.org/research/housing/policy-basics-federal-rental-assistance. Accessed August 30, 2016.
- 8.Lloyd P, Helms V. NCHS-HUD linked data: analytic considerations and guidelines. Available at: http://www.cdc.gov/nchs/data/datalinkage/nchs_hud_analytic_considerations.pdf. Accessed August 30, 2016.
- 9.National Center for Health Statistics. NCHS data linked to HUD Housing Assistance Program files. Available at: http://www.cdc.gov/nchs/data_access/data_linkage/hud.htm. Accessed August 30, 2016.
- 10.National Center for Health Statistics. NHANES response rates and population totals. Available at: http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed August 30, 2016.
- 11.National Center for Health Statistics. NCHS-HUD linked file sample sizes and percentages linked, by survey and age at interview. Available at: http://www.cdc.gov/nchs/data/datalinkage/nchs_hud_linked_file.pdf. Accessed August 30, 2016.
- 12.National Center for Health Statistics. National Health and Nutrition Examination Survey 2005–2006 data documentation, codebook, and frequencies: cadmium, lead, and total mercury. Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/PBCD_D.htm. Accessed August 30, 2016.
- 13.Kaufmann RB, Clouse TL, Olson DR, Matte TD. Elevated blood lead levels and blood lead screening among US children aged one to five years: 1988–1994. Pediatrics. 2000;106(6):e79. doi: 10.1542/peds.106.6.e79. [DOI] [PubMed] [Google Scholar]
- 14.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Available at: http://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf. Accessed August 30, 2016. [PubMed]
- 15.World Health Organization. Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. Available at: http://www.who.int/vmnis/indicators/haemoglobin.pdf. Accessed August 30, 2016.
- 16.US Department of Housing and Urban Development. FY 2015 income limits. Available at: http://www.huduser.gov/portal/datasets/il/il15/index.html. Accessed August 30, 2016.
- 17.National Research Council. Measuring Lead Exposure in Infants, Children, and Other Sensitive Populations. Washington, DC: National Academies Press; 1993. [PubMed] [Google Scholar]
- 18.Lucchini RG, Zoni S, Guazzetti S et al. Inverse association of intellectual function with very low blood lead but not with manganese exposure in Italian adolescents. Environ Res. 2012;118:65–71. doi: 10.1016/j.envres.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods. 2010;15(3):234–249. doi: 10.1037/a0019623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rabito FA, Shorter C, White LE. Lead levels among children who live in public housing. Epidemiology. 2003;14(3):263–268. [PubMed] [Google Scholar]
- 21.Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, Horsburgh CR. Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health. 2008;98(1):85–91. doi: 10.2105/AJPH.2006.094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahaffey KR, Annest JL, Roberts J, Murphy RS. National estimates of blood lead levels: United States, 1976–1980: association with selected demographic and socioeconomic factors. N Engl J Med. 1982;307(10):573–579. doi: 10.1056/NEJM198209023071001. [DOI] [PubMed] [Google Scholar]
- 23.Cook BL, McGuire TG, Meara E, Zaslavsky AM. Adjusting for health status in non-linear models of health care disparities. Health Serv Outcomes Res Methodol. 2009;9(1):1–21. doi: 10.1007/s10742-008-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossen LM, Kobernik EK. Food insecurity and dietary intake among US youth, 2007–2010. Pediatr Obes. 2016;11(3):187–193. doi: 10.1111/ijpo.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference. 2015;3(2):237–249. doi: 10.1515/jci-2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.deSilva PE. Blood lead levels and the haematocrit correction. Ann Occup Hyg. 1984;28(4):417–428. doi: 10.1093/annhyg/28.4.417. [DOI] [PubMed] [Google Scholar]
- 29.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4):488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Residential Lead-Based Paint Hazard Reduction Act of 1992 (Public Law 102-550), as amended through April 21, 2005. Available at: http://www.hud.gov/offices/lead/library/lead/Title_X.pdf. Accessed August 30, 2016.
- 31.US Department of Housing and Urban Development. Interpretive guidance on HUD’s lead safe housing rule. Available at: http://portal.hud.gov/hudportal/documents/huddoc?id=DOC_25476.pdf. Accessed August 30, 2016.
- 32.Bostic RW, Thornton RL, Rudd EC, Sternthal MJ. Health in all policies: the role of the US Department of Housing and Urban Development and present and future challenges. Health Aff (Millwood) 2012;31(9):2130–2137. doi: 10.1377/hlthaff.2011.1014. [DOI] [PubMed] [Google Scholar]
- 33.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]