Abstract
Purpose
The purpose of this study was to identify socioeconomic, physician-related, and rural-urban factors that may influence the presence of a Medicare-certified hospice in three rural-urban areas.
Design
This was secondary analysis of selected socioeconomic, physician-related, and rural-urban data from 3,140 counties using the 2005 Area Resource File, a county-level database. The county was the unit of analysis.
Methods
Descriptive statistics were calculated for selected socioeconomic, physician, and rural-urban variables for the data set of 3,140 counties. Logistic regression was used to identify variables that influenced the presence of a Medicare-certified hospice across three rural-urban areas.
Findings
As the rural-urban classification progressed from metropolitan (least rural) to rural-nonadjacent (most rural), the physician rate, racial-ethnic diversity, and number of counties with at least one Medicare-certified hospice decreased. However, in all three rural-urban areas only the physician rate was consistently significantly associated with the presence of a Medicare-certified hospice.
Conclusions
Given the increasing numbers of patients and families who will be facing end-of-life care issues across the globe, access to hospice care is a significant end-of-life outcome. The most rural communities are least likely to have a Medicare-certified hospice. The higher the physician rate, the more likely a county is to have a Medicare-certified hospice. The Medicare Hospice Benefit’s regulations requiring a physician’s certification of terminal illness may be creating a barrier to hospice care, especially in rural communities. In this study, racial-ethnic diversity decreased as the rural-urban classification progressed from metropolitan (least rural) to rural-adjacent to metro to rural-nonadjacent (the most rural). The availability of Medicare-certified hospices in the metro and rural nonadjacent counties was influenced by the minority composition of the county. More research is needed on how the interaction of rurality, race-ethnicity, and physician access may affect access to hospice in rural communities.
Clinical Relevance
Increasing numbers of patients and their families across the globe will be facing end-of-life care. One of the most common barriers to end-of-life care in rural communities all over the world is physician availability. People living in rural communities with few physicians may experience less access to the comprehensive services of hospice than people living in metropolitan communities and therefore not realize important end-of-life outcomes such as symptom management, improved quality of life, financial support, and bereavement support.
Keywords: terminal care/palliative care, health policy, health disparities, quantitative methodology
Hospice use significantly increased from 1992 to 2004 (Carlson, Morrison, Holford, & Bradley, 2007; Han, Remsburg, & Iwashyna, 2006; Lackan, Ostir, Freeman, Mahnken, & Goodwin, 2004; Virnig, Ma, Hartman, Moscovice, & Carlin, 2006; Virnig, Moscovice, Durham, & Casey, 2004). However, Medicare beneficiaries who live in rural communities and are members of ethnic or racial minority groups are less likely than other patients to die at home under the care of a hospice provider (Connor, Tecca, LundPerson, & Teno, 2004; Flory, Young-Xu, Gurol, Levinsky, Ash, & Emanuel, 2004; Virnig et al., 2004).
Background and Significance
Researchers have consistently reported rural-urban differences in hospice use (Lackan et al., 2004; Virnig et al., 2004, 2006). For example, Virnig and colleagues (2006) found that in the United State, hospice services were unavailable in 23% of the most rural zip codes, while only 1.3% of the metropolitan zip codes were unserved by hospice.
Historically, hospice programs in the United States have served primarily White patients with a cancer diagnosis and their families (Buck, 2007). While the most recent statistics indicate that patients who are enrolled in a hospice program are now more likely to have a non-cancer diagnosis (National Hospice and Palliative Care Organization [NHPCO], 2008), many hospice programs still have little ethnic or racial diversity in their average daily census, especially in rural communities. Nationally, the racial-ethnic description of people using hospice is as follows: White 81.3%, African American 9.0%, Asian/Hawaiian 1.6%, American Indian 0.3%, multiracial/ other races 7.8%, and Hispanic 5.1% (NHPCO).
While rural-urban and racial-ethnic differences in the use of hospice have been noted, the studies to date do not fully explain rural-urban and racial-ethnic disparities in hospice use (Virnig, 2007). County-level data have been the unit of analysis in studies that have examined geographic variation in hospice use. One limitation of using county-level data, however, is that many hospice programs provide services in multiple counties and across state lines; therefore, county-level data alone may not accurately explain the difference in hospice use between urban and rural communities (Virnig; Virnig et al., 2006). Virnig and colleagues, noting the limitations of using county-level data to describe differences in hospice use in different geographic areas, used zip code level data to identify regions in the United States that were not served by home-based hospice services. Using the zip code as the level of analysis improved the ability to describe hospice utilization by Medicare beneficiaries, especially for hospice agencies providing services in multiple counties or states. This validates that hospices located in one county may serve clients in other counties and across state lines (Virnig et al., 2006). While the use of zip code level data was effective in providing information about rural areas that lacked hospice coverage, no additional information was provided on community characteristics that might affect hospice coverage, such as physician availability, minority composition, median age, percentage of the population living below the poverty line, and household income (Crawley, 2005; Crawley, Payne, Bolden, Payne, Washington, & Williams, 2000; Lackan et al., 2004; Virnig et al., 2004).
Physician availability is a major community characteristic that may be associated with rural-urban difference in hospice use (Casey, Moscovice, Virnig, & Durham, 2005; Friedman, Harwood, & Shields, 2002; Winston, Leshner, Kramer & Allen, 2005). Since under the Medicare Hospice Benefit (MHB) the physician is the only healthcare provider to certify that a person’s life expectancy is 6 months or less (Buck, 2007; Centers for Medicare and Medicaid Services [CMS], 2008; J. Kennedy, NHPCO, personal communication, September 23, 2008). People living in rural communities without access to a physician may have a difficult time accessing hospice services (Winston et al.).
Providing care to a person with a life-limiting illness can be stressful. Caregivers may experience their own psychological and physical issues that impact their ability to provide care and often are juggling responsibilities to care for others in the household (McMillan et al., 2006). The added financial costs of medications, equipment, and supplies can increase tension for families that are already living with high levels of poverty or on a seasonal or fixed income.
The MHB pays for medications, equipment, and supplies related to hospice diagnosis. Although the Medicare Conditions of Participation allow the hospice providers to charge a co-pay, it is generally less than the 20% co-pay for other services under Medicare (CMS, 2008). However, without the hospice financial benefits, people with a life-limiting illness without insurance benefits are often faced with problems in meeting monthly expenses, such as the mortgage payment, the cost of gas or utilities, and paying for medications to manage pain and other symptoms. Given the significant resources that hospice care can provide to people living in rural communities, it is important to explore community characteristics such as geographic variation, socioeconomic variables, and the physician rate in a rural community that could influence rural-urban and racial-ethnic disparities in hospice use. This study seeks to identify community characteristics that influence the presence of a Medicare-certified hospice.
Conceptual Framework
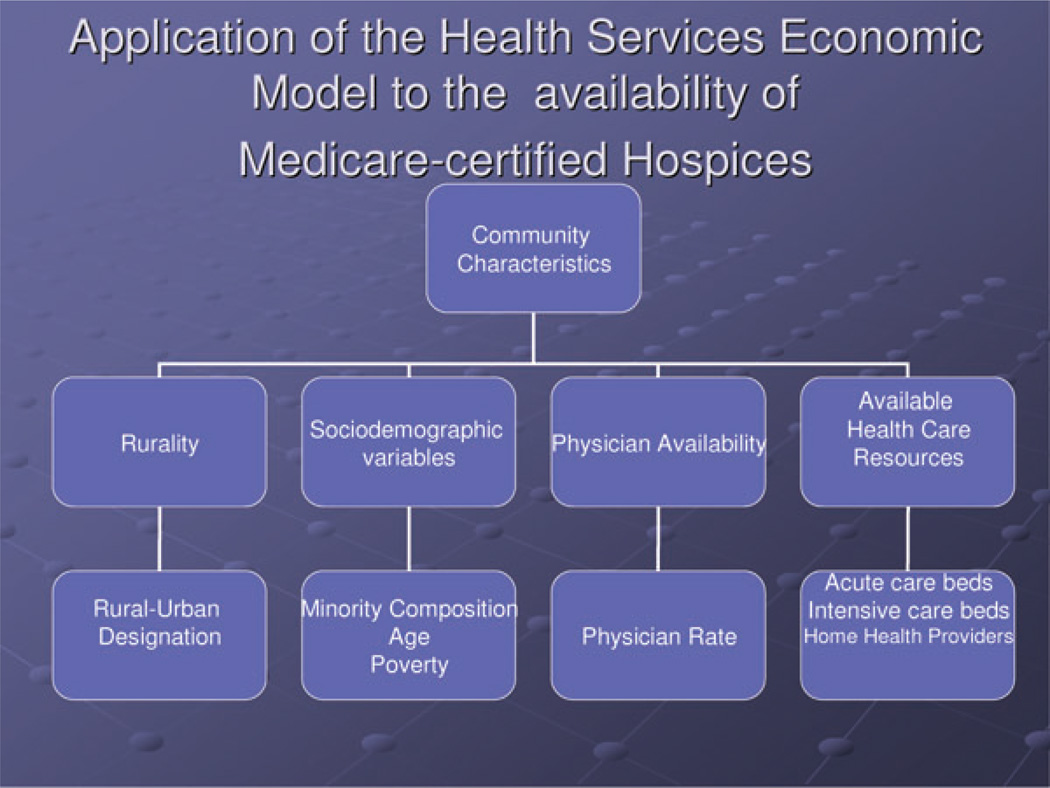
A model originally developed to study the supply of and demand for rural mental health providers (Merwin, Hinton, Dembling, & Stern, 2003) was used to guide the current study of community variables that may be associated with the presence of a Medicare-certified hospice. In this paper it will be referred to as the Health Services Economic Model (HSEM). According to the HSEM, the supply of mental health professionals is influenced by community characteristics and by the compensation available to healthcare professionals. The supply of healthcare professionals ultimately impacts community/patient mental health outcomes. Communities with higher degrees of rurality, higher levels of poverty, and higher percentage of minorities (Merwin et al., 2003) are more likely to be classified as underserved or designated healthcare shortage areas for mental health providers (physicians, advanced practice nurses [APNs], and other mental health services). In this study, we focused on physician rate, income, rurality, age, and minority composition. Figure 1 shows the community characteristics that may affect the presence of a Medicare-certified hospice.
Figure 1.
Application of the Health Services Model to the availability of Medicare-certified Hospices.
This study was designed to answer these research questions: (a) What socioeconomic, physician, and rural-urban factors influence the presence of a Medicare-certified hospice? and (b) Does the importance of these factors vary across rural and urban areas?
Methods
Design and Procedures
We examined the association between the presence of a hospice in a county and county-level socioeconomic, physician, and rural-urban characteristics and assessed whether this association varied across three rural-urban areas. The study sample consisted of counties in the 2005 Area Resource File (ARF; U.S. Department of Health and Human Services, 2005). The ARF is a county-specific database containing more than 6,000 variables for each of the nation’s 3,225 counties, independent cities, the District of Columbia, Puerto Rico, Guam and the Virgin Islands. The ARF contains information on health facilities, health professionals, measures of resource scarcity, health status, economic activity, health training programs, and socioeconomic and environmental characteristics (U.S. Department of Health and Human Services, 2005). We analyzed the county-specific data from 3,140 counties in the United States, including the District of Columbia. The 82 counties in the U.S. territories of Puerto Rico, Guam, and the Virgin Islands and three counties in the United States were not included in the analysis (a record for the state of Alaska [considered one county]; Clifton-Forge City, Virginia; and Broomfield County, Colorado) because the ARF was missing key variables for these counties, such as rurality.
Study Variables
The rurality variable was categorized into three categories using rural-urban continuum areas, determined from the nine rural-urban areas in the U.S. Department of Agriculture’s classification based on population data from the 2000 Census: (a) metro (based on the census of the metropolitan area); (b) nonmetro, adjacent to metro; and (c) nonmetro, nonadjacent to metro (both based on their proximity to metro areas; U.S. Department of Agriculture, 2003). The demographic variables included the census of each county in 2004, the median age of people living in the county in 2000, the mean percentage of the county’s population that was older than 65 years, the percentage of people living in poverty, the percentage of the county considered rural, and the percentages of Hispanics, African Americans, Asians, and American Indians in the total population of the county. Because the distributions of these minority composition variables were highly skewed, we considered these variables as categorical rather than continuous in all the statistical models. Specifically, the variable of the African American percentage of the population was categorized into three groups using cutpoints roughly at the median and 90th percentile (2% and 30%, respectively); the variable of Hispanic population composition was also categorized into three groups using roughly the median and 90th percentile (2% and 15%, respectively); and the variables of Asian and Native American population composition were each categorized into two groups using the cutpoint of 2%, which is roughly the 90th percentile. We also included the physician rate (measured by the total number of MDs per 10,000 census in 2004). The dependent variable is defined as a binary indicator of whether a county has at least one Medicare-certified hospice or not.
Data Analysis
Logistic regression was the method chosen for data analysis. It is the regression technique customarily used for a binary dependent variable (Fleiss, Levin, & Paik, 2003). The data analysis was organized into three steps. In Step 1, logistic regression was used to obtain the overall association between the county predictors described above to the presence of at least one Medicare-certified hospice in a county as the dependent variable. In Step 2, we examined whether the association of county racial composition and the presence of a hospice differed with the degree of rurality. For this, we performed the tests for the interaction terms of rurality variable with the two racial variables, “African American population composition in a county” and “Hispanic population composition in a county.” In Step 3, since the results for these interaction terms were significant, separate logistic models were therefore performed to examine a different association for each of the three rural-urban areas. Odds ratios (ORs) were used to interpret the results, with a two-sided p value of .05.
Results
The characteristics of the 3,140 counties are summarized in Table 1 and shown in Figure 1. For the 3,140 counties in the data set, the average county census in 2004 was 93,507 (SD=304,790); the average of each county’s median age was 37.3 years (SD=4.01); and the mean percentage of each county’s population that was older than 65 years was 14.76% (SD=4.17). On average, 13.74% (SD=5.59) of the residents were living below the poverty line. Hispanics and African Americans were the minority groups with highest representation in the data set. The mean percentages of African Americans and Hispanics in the counties were 8.76% (SD=14.5) and 6.18% (SD=11.9), respectively. The mean physician rate was 12.61 (SD=14.89), and the mean number of Medicare-certified hospices was 0.83 (SD=1.84).
Table 1.
Summary of Socioeconomic, Rural-Urban, and Physician Variables
| Variables | Mean | SD |
|---|---|---|
| Census in 2004 | 93,507 | 304,790 |
| County median age in 2000 (yr) | 37.3 | 4.01 |
| Percentage of county living below poverty line in 2003 | 13.74 | 5.59 |
| Percentage of population residing in a rural area | 59.9 | 30.98 |
| Percentage of Whites in county | 84.4 | 16.60 |
| Percentage of African Americans | 8.76 | 14.5 |
| Percentage of Hispanics in population | 6.18 | 11.99 |
| Percentage of Asians | 0.84 | 2.13 |
| Percentage of Native Americans | 1.9 | 7.6 |
| MDs per 10,000 census in 2004 | 12.61 | 14.89 |
| Number of Medicare-certified hospices in 2004 | 0.83 | 1.84 |
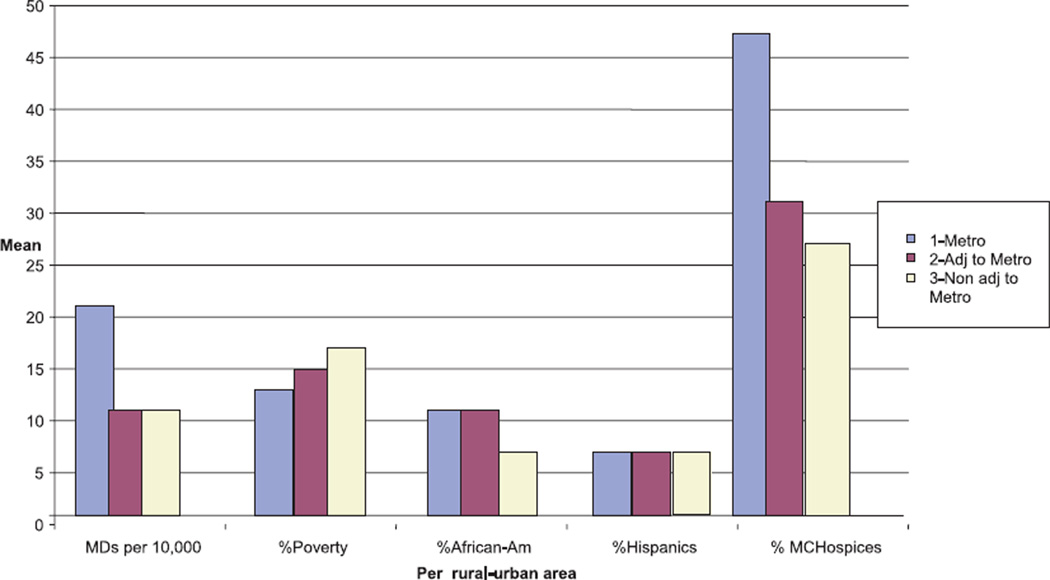
Some community characteristics varied substantially in rural and urban areas. The physician rate in metropolitan areas was much higher than that of adjacent to metro and rural areas (18.99, 8.98, and 9.48, respectively); the percentage of residents living below the poverty line was much lower in metro areas than the other two areas; the percentage of African Americans was higher in metro and the rural, adjacent to metro areas, while the percentage of Hispanics did not vary depending on the areas. The percentage of counties with at least one Medicare-certified hospice was much higher in the metro area than the other two areas, as might be expected (Figure 2).
Figure 2.
A comparison of MDs per 10,000 census, mean percentage of poverty, of African Americans, of Hispanics, and counties with at least one Medicare-certified hospice across three rural-urban areas.
The majority of the counties did not have a Medicare-certified hospice. The percentages of counties with at least one Medicare-certified hospice varied substantially across urban and rural areas: 59%, 39% and 36% in metro, adjacent to metro, and rural, nonadjacent to metro areas, respectively. The most rural counties were least likely to have a Medicare-certified hospice, while the metro counties were most likely to have one, as one would expect.
The results of logistic regression models that examined the associations between the presence of a Medicare-certified hospice and county characteristics are shown in Table 2 as ORs. In the full model, African American composition and Hispanic composition, age, percentage of people living in poverty, and physician rate were significantly associated with the presence of a hospice in a county. The odds of a county having at least one Medicare-certified hospice increased 10% for every 1-unit increase in the county physician rate (OR=1.105, p<.0001). A higher percentage of people living in poverty and a higher county median age were associated with decreased likelihood of having a Medicare-certified hospice. The odds of having a hospice in counties where the African American population ranged from 2% to 30% was 29% greater than counties with less than 2% African Americans (OR=1.286, p=.0087). Counties with a Hispanic population ranging from 2% to 15% were 23% more likely to have a hospice provider than counties whose population was less than 2% Hispanic (OR=1.232, p=.0211). Although the percentage of counties having a hospice was highest in metro areas and lowest in the most rural areas, this difference disappeared after controlling for community characteristics. This suggested that the differences between urban and rural areas might be partially attributable to the differences in county median age, county physician rate, poverty level, and racial-ethnic composition.
Table 2.
Influence of Rurality, Socioeconomic Characteristics, and Availability of Physicians on the Presence of a Medicare-certified Hospice in a County
| Full model |
Metro |
Nonmetro, adjacent to metro |
Rural, nonadjacent |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | Odds ratio |
p | Odds ratio |
P | Odds ratio |
P | Odds ratio |
p |
| County African American (AA) population (counties with < 2% AA are the reference group) | ||||||||
| Counties with 2%–30% AA | 1.286 | .0087* | 1.559 | .0053* | 0.989 | 0.9427 | 1.414 | .0795 |
| Counties with > 30% AA | 0.983 | .9196 | 0.769 | .3998 | 0.656 | 0.1249 | 2.196 | .0108* |
| County Hispanic population (counties with < 2% Hispanic are the reference group) | ||||||||
| Counties with 2%–15% Hispanic | 1.232 | .0211* | 1.887 | <.0001* | 1.085 | .5857 | 0.976 | .8884 |
| Counties with > 15% Hispanic | 0.989 | .9438 | 1.308 | .3399 | 0.753 | .3221 | 0.928 | .7713 |
| County Native American (NA) population (counties with < 2% NA are the reference group) | ||||||||
| Counties with > 2% NA | 1.087 | .5265 | 1.434 | 0.2487 | 1.274 | .2792 | 0.886 | .5548 |
| County Asian population (counties with < 2% Asian are the reference group) | ||||||||
| Counties with > 2% Asian | 1.106 | .6020 | 1.848 | .0143* | 0.560 | .3277 | 0.320 | .0159* |
| County median age | 0.922 | <.0001* | 0.961 | .0864 | 0.916 | <.0001* | 0.890 | <.0001* |
| Percentage living in poverty | 0.972 | .0028* | 1.026 | .1954 | 0.951 | .0040* | 0.952 | .0018* |
| MDs per 10,000 census | 1.105 | <.0001* | 1.077 | <.0001* | 1.156 | <.0001* | 1.118 | <.0001* |
| Rural adjacent vs Metro | 1.093 | 0.4164 | ||||||
| Rural nonadjacent vs. metro | 1.003 | 0.9825 | ||||||
p < .05.
In the metro model, counties with an African American population ranging from 2% to 30%, Hispanic population ranging from 2% to 15%, a greater percentage of Asians in the population, and a larger physician rate are associated with increased likelihoods of having a hospice. In the adjacent to metro model, county median age (OR=0.916, p<.0001), percentage of people living in poverty (OR=0.951, p=.0040), and physician rate were significantly associated with the presence of a Medicare-certified hospice. African American composition, age, and physician rate were significantly associated with the presence of a Medicare-certified hospice in counties categorized as rural nonadjacent, the most rural counties.
When the association of the presence of a hospice and community characteristics was examined across the three rural-urban areas, the physician rate remained as a significant variable that influenced the presence of a Medicare-certified hospice. Counties with higher rates of physicians were more likely to have hospice in metro areas as well as both types of rural areas. Counties with higher levels of poverty are less likely to have a hospice in all but the metro areas. Median age is a significant variable in both rural models. Counties with a higher median age were less likely to have a hospice in all but the metro areas.
Discussion
The purpose of this study was to answer the following research questions: (a) What are the socioeconomic, physician, and rural-urban factors that influence the presence of a Medicare-certified hospice? (b) Are there differences across three rural-urban areas? The proportion of counties that had at least one Medicare-certified hospice varied substantially across urban and rural areas from 59% in metro to 39% in adjacent to metro (p<.001 compared to metro) and 36% in rural, nonadjacent to metro areas, respectively (p<.001 when compared to metro). The finding that the most rural counties (nonadjacent to metro) are least likely to have a Medicare-certified hospice provider is consistent with other studies that have reported rural-urban differences in hospice use (Lackan et al., 2004; Virnig et al., 2004, 2006). Bushy (2008) suggested that people living in a rural community could be identified as a vulnerable population because their place of residence negatively impacts access to health care.
In the 3,140 counties examined in this analysis, the physician rate varied substantially across rural and urban areas and was the only significant variable that influenced the presence of a Medicare-certified hospice in all three rural-urban areas. The Medicare Hospice Conditions of Participation mandate that a physician’s certification of a life expectancy of 6 months or less is an admission criterion for hospice services (CMS, 2008; Kvale, Williams, Bolden, Padgett, & Bailey, 2004; Winston et al., 2005).
The physician is not only the gatekeeper for access to hospice services, but also holds the key for payment. That is, if a hospice provider does not have the certification statement, the organization cannot be paid for services (CMS, 2008; Virnig et al., 2004). Although the Conditions of Participation require that hospice agencies have their own medical director who can certify a patient as hospice eligible and take on the role as primary physician for those who do not have a primary provider, the physician-as-gatekeeper model may negatively affect hospice access for rural residents in counties with few physicians.
A community hospice is a significant resource that can help families living in rural communities achieve significant outcomes such as symptom management for the patient and emotional support for the family and caregivers. In Jordan’s National Palliative Care Initiative (Stjernsward et al., 2007), it was estimated that for every person who may receive palliative care services, including hospice, at least two family members are providing direct patient care.
The quality of life of family members can also be improved by the services provided by hospice (Stjernsward et al., 2007). Decreasing the financial burden of a life-limiting illness is also an important outcome in rural communities. In the current study, as the designation of a county became more rural, the percentage of the population living below the poverty level increased. Haven Hospice, one of the largest rural hospice providers in the country, estimated that the median household income for their 17-county service in north central Florida is 24% below the state average and 32% below the national average, and that 17% of the population is living below the national poverty level (Haven Hospice, 2007). Without the financial support of hospice, families do not have additional income to pay for medications, equipment, and supplies to manage an illness.
African Americans and Hispanics were the largest ethnic and racial groups living in the counties studied here. The percentage of African Americans in the population was higher in areas classified as metro and adjacent to metro, while the percentage of Hispanics did not vary. The majority of the counties had a population that was less than 2% Hispanic and African American, and in the most rural counties, ethnic and racial diversity was particularly limited. Racial-ethnic composition was not consistently a significant variable influencing the presence of Medicare-certified hospice across three rural-urban areas.
African Americans and Hispanics comprise 12.2% and 15.1%, respectively, of the U.S. population (U.S. Department of the Census, 2007). The southern states have the greatest concentration of African Americans, and the western states have a higher proportion of Hispanics living in rural communities (Pathman, Konrad, & Schwartz, 2002; U.S. Census Bureau, 2000).Virnig et al. (2004) found that minority and rural beneficiaries were less likely to receive hospice care. In the current study, the most rural counties were less likely to have a hospice, but race and ethnicity were not consistently associated with the presence of a hospice in the three rural-urban areas. Individuals who live in rural communities and are members of racial-ethnic minorities are extremely vulnerable to certain health conditions (Bushy, 2008) and are more likely to experience disparities in access to health care.
Limitations
The source of the data for this analysis was the 2005 ARF (U.S. Department of Health and Human Services, 2005), which provided data only at the county level. We did not have information about individual utilization of hospice services. This study did not examine other community or organization characteristics that might be associated with availability and access to hospice services, such as staffing availability, physician referral patterns, administrative decisions made to provide services in a given area, or challenges faced by the staff in accessing homes, for example, impassible terrain and large distances between patients (Casey et al., 2005; Friedman et al., 2002). Although it is recognized that physicians and hospices serve populations residing in counties and states other than where they are located, this study considered only resources and characteristics within each county. It is recognized that people travel across county and state lines to access physician and hospice services.
The conceptual model used in this study also included a variable on available healthcare resources. We chose to focus on the impact of the socioeconomic, physician, and rural-urban factors. Future studies will look at the impact of available healthcare resources on the availability of a Medicare-certified hospice and multilevel models including smaller geographic units of analysis and individual level data. Additional research should be done on the interactive effects of rurality and race/ethnicity on hospice access by minorities living in rural communities, and on whether the physician-driven hospice model is a barrier to hospice services in rural communities, nationally and internationally.
Nursing Implications
The physician remains the only healthcare provider in the United States who can certify eligibility for hospice services provided under the MHB. This regulation may negatively affect hospice access for rural residents in counties with few physicians. Although the study was conducted in the United States, it highlights one of the most common barriers to end-of-life care in rural communities across the globe: physician availability. In many parts of the world, physician availability is severely limited because people are widely distributed across large geographic regions, and palliative care and hospice services, including written prescriptions for symptom management medications, must be initiated by a physician’s order (Ens, Gwyther, Chochinov, Moses, Jackson, & Harding, 2008; Jagwe & Merriman, 2007).
HIV/AIDS and its related cancers are decimating many countries in sub-Saharan Africa, and the need for palliative care and hospice is more urgent than ever before. The World Health Organization (WHO) has declared the provision of palliative care as “an urgent, humanitarian responsibility” (Stjernsward, Foley, & Ferris, 2007; WHO, 2005); therefore, it has become important for nurses to identify and to explore factors that may impact access to palliative care and hospice in their countries. Other barriers to end-of-life care around the world are the lack of knowledge of symptom management principles and pharmacology (Stjernswald et al., 2007), migration of trained health workers (Logie & Leng, 2007), restricted access to opioids for pain management (Jagwe & Merriman, 2007), and the lack of regional or national health policies that endorse and provide funding for palliative care and hospice services (Reb, 2003; Stjernsward, Foley, & Ferris, 2007).
The lack of physicians to provide hospice and palliative care is an opportunity for nurses across the globe to demonstrate that we have the skills to help our communities fill this gap. The MHB is a physician-directed, nurse-coordinated model of hospice care delivery in the United States (Buck, 2007). APNs in the United States believe that the lack of physician access in rural communities is an opportunity to demonstrate to policy makers that APNs have the knowledge, skills, and clinical judgment to determine when a person meets hospice eligibility criteria and to initiate an order for hospice services, including prescribing medications, equipment, and supplies.
Legislation was introduced during the 107th Congress that would have permitted nurse practitioners to admit a patient to hospice, but the bill did not see legislative action by close of the 107th congress (Reb, 2003). Nurse practitioners are very active in palliative care and hospice as direct care providers, educators, and administrators. Many states have granted APNs narcotic prescriptive authority independently or under the collaboration or supervision of a physician; however, the physician remains the only healthcare provider in the United States who can provide an order to initiate hospice services provided under the MHB (CMS, 2008; Reb, 2003).
Nurses in countries such as Australia, Sweden, and Uganda are addressing the lack of physician availability by lobbying their policy makers and regulatory bodies for the authority to prescribe narcotics for symptom management (Colleau, 2001). In 2004, Uganda was one of the first African nations to allow specially trained nurses to prescribe morphine. Families are able to care for their loved ones at home rather than traveling great distances to a hospital or having to care for a person at home who is suffering with unrelenting pain. This change in practice revolutionized hospice care at home in Uganda and affirmed that nurses can safely manage patients on narcotics in the community and improve the quality of life for people with a life-limiting illness (Jagwe & Merriman, 2007).
Conclusions
Given the increasing numbers of patients and families who will be facing end-of-life care issues, nurses from all over the globe will continue to be involved in new initiatives to increase access to hospice and palliative care services. (Reb, 2003; Stjernsward, Foley, & Ferris, 2007).
Clinical Resources.
End-life Life Nursing Education Consortium (EL-NEC). A national educational initiative to improve end-of-life care: www.aacn.nche.edu/elnec
Growth House. An Internet portal to resources for life-threatening illness and end-of-life care: www.growthhouse.org
National Hospice and Palliative Care Organization. Facts and figures on hospice. http://www.nhpco.org/files/public/Statistics Research/NHPCO facts-and-figures 2008.pdf
Acknowledgements
This paper was supported in part by Grant No. P20 NR009009, Rural Health Care Research Center, from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
References
- Buck J. Netting the hospice butterfly: Politics, policy and translation of an ideal. Home Health Care Nurse. 2007;25(9):566–571. doi: 10.1097/01.NHH.0000296113.56567.fd. [DOI] [PubMed] [Google Scholar]
- Bushy A. Conducting culturally competent nursing research. Annual Review of Nursing Research. 2008;26:221–236. [PubMed] [Google Scholar]
- Carlson MD, Morrison RD, Holford TR, Bradley EH. Hospice care: What services do patients and families receive? Health Services Research. 2007;42(4):1672–1690. doi: 10.1111/j.1475-6773.2006.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey M, Moscovice IS, Virnig B, Durham S. Providing hospice care in rural areas: Challenges and strategies. American Journal of Hospice and Palliative Care. 2005;22(5):363–368. doi: 10.1177/104990910502200509. [DOI] [PubMed] [Google Scholar]
- Centers for Medicaid and Medicare Services, U.S. Department of Health and Human Services. Conditions of participation: Hospice care. 2008 Retrieved September 23, 2008, from http://www.access.gpo.gov/nara/cfr/waisidx 04/ 42cfr418 04.html.
- Colleau S. Expanding the nurses’ role in pain management. International news on nurse prescribing. Cancer Pain Relief. 2001;14(4) Retrieved May 5, 2009, from https://whocancerpain.bcg.wisc.edu/?q=node/180. [Google Scholar]
- Connor SR, Tecca M, LundPerson J, Teno J. Measuring hospice care: The national hospice and palliative care organization national data set. Journal of Pain and Symptom Management. 2004;28(4):316–328. doi: 10.1016/j.jpainsymman.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Crawley L. Racial, cultural, and ethnic factors influencing end of life care. Journal of Palliative Medicine. 2005;8(Suppl. 1):58–69. doi: 10.1089/jpm.2005.8.s-58. [DOI] [PubMed] [Google Scholar]
- Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. Journal of the American Medical Association. 2000;284(19):2518–2521. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- Ens CD, Gwyther L, Chochinov H, Moses S, Jackson C, Harding R. Access to hospice care: Multi-professional specialist perspectives in South Africa. International Journal of Palliative Nursing. 2008;14(4):169–174. doi: 10.12968/ijpn.2008.14.4.29227. [DOI] [PubMed] [Google Scholar]
- Fleiss JL, Levin B, Paik MC. Statistical methods for rates & proportions. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- Flory J, Young-Xu, Gurol I, Levinsky N, Ash A, Emanuel E. Place of death: U.S. trends since 1980. Health Affairs. 2004;23(3):194–200. doi: 10.1377/hlthaff.23.3.194. [DOI] [PubMed] [Google Scholar]
- Friedman B, Harwood MK, Shields M. Barriers and enablers to hospice referrals: An expert review. Journal of Palliative Medicine. 2002;5:73–81. doi: 10.1089/10966210252785033. [DOI] [PubMed] [Google Scholar]
- Han B, Remsburg RE, Iwashyna TJ. Differences in hospice use between black and white patients during the period 1992–2000. Medical Care. 2006;44(8):731–737. doi: 10.1097/01.mlr.0000215858.37118.65. [DOI] [PubMed] [Google Scholar]
- Haven Hospice. Annual report. 2007 Retrieved April 10, 2009, from http://www.havenhospice.org/about_publications.html.
- Jagwe J, Merriman A. Uganda: Delivering analgesia in rural Africa. Opioid availability and nurse prescribing. Journal of Pain and Symptom Management. 2007;33(5):547–551. doi: 10.1016/j.jpainsymman.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Kvale EA, Williams BR, Bolden JL, Padgett CG, Bailey FA. The Balm of Gilead project: A demonstration project on end-of-life-care for safety-net populations. Journal of Palliative Medicine. 2004;7(3):486–493. doi: 10.1089/1096621041349428. [DOI] [PubMed] [Google Scholar]
- Lackan NA, Ostir GV, Freeman JL, Mahnken JD, Goodwin JS. Decreasing variation in the use of hospice among older adults with breast, colorectal, lung and prostate cancer. Medical Care. 2004;42:116–122. doi: 10.1097/01.mlr.0000108765.86294.1b. [DOI] [PubMed] [Google Scholar]
- Logie D, Leng M. Africans die in pain because of fears of opiate addiction. British Medical Journal. 2007;335(7622):68–69. doi: 10.1136/bmj.39353.715359.DB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan S, Small BJ, Weitzner [O17] M, Schonwetter R, Tittle M, Moody H, et al. Impact of coping skills intervention with family members of caregivers of hospice patients with cancer. Cancer. 2006;106(1):214–222. doi: 10.1002/cncr.21567. [DOI] [PubMed] [Google Scholar]
- Merwin E, Hinton I, Dembling B, Stern S. Shortages of rural mental health professionals. Archives of Psychiatric Nursing. 2003;17(1):42–51. doi: 10.1053/apnu.2003.1. [DOI] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization. Facts and figures on hospice. 2008 Retrieved November 6, 2008, from http://www.nhpco.org/files/public/Statistics_Research/NHPCO facts-and-figures 2008.pdf.
- Pathman DE, Konrad TR, Schwartz R. The proximity of predominantly African American and Hispanic rural communities to physicians and hospital services. Journal of Rural Health. 2002;18(3):416–427. doi: 10.1111/j.1748-0361.2002.tb00906.x. [DOI] [PubMed] [Google Scholar]
- Reb AM. Palliative and end-of-life care: Policy analysis. Oncology Nursing Forum. 2003;30(1):35–49. doi: 10.1188/03.ONF.35-50. [DOI] [PubMed] [Google Scholar]
- Stjernsward J, Ferris F, Khleif S, Jamous W, Treish I, Milhelm M, et al. Jordan Palliative Care Initiative: A WHO demonstration project. Journal of Pain and Symptom Management. 2007;33(5):628–633. doi: 10.1016/j.jpainsymman.2007.02.032. [DOI] [PubMed] [Google Scholar]
- Stjernsward J, Foley KM, Ferris FD. Integrating palliative care into national policies. Journal of Pain and Symptom Management. 2007;33(5):514–520. doi: 10.1016/j.jpainsymman.2007.02.031. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. State and county quick facts. 2000 Retrieved April 11, 2008, from http://quick facts.census.gov/gfd/states/51000.html.
- U.S. Department of Agriculture. Rural-urban continuum codes for metro and nonmetro counties. 2003 Retrieved July 13, 2007, from http://www.ers.usda.gov/Briefing/Rurality/RuralUrbCon/
- U.S. Department of the Census. American community survey demographic and housing estimates 2007. 2007 Retrieved September 23, 2008, from http://factfinder.census.gov/servlet/ADPTable? bm=y&-geo id=01000US&-qr name=ACS 2007 1YR G00 DP5&-ds name=&- lang=en&-redoLog=false&-format=
- U.S. Department of Health and Human Services. Area resource file. Health Resources and Services Administration, Bureau of Health Professions. Rockville, MD: Author; 2005. [Google Scholar]
- Virnig BA. Toward a better understanding of the role of geography in intensity of end-of-life care. Medical Care. 2007;45(5):374–376. doi: 10.1097/01.mlr.0000263474.23170.c2. [DOI] [PubMed] [Google Scholar]
- Virnig BA, Ma H, Hartman LK, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. Journal of Palliative Medicine. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]
- Virnig BA, Moscovice IS, Durham S, Casey M. Do rural elders have limited access to Medicare hospice services? Journal of the American Geriatrics Society. 2004;52:731–735. doi: 10.1111/j.1532-5415.2004.52213.x. [DOI] [PubMed] [Google Scholar]
- Winston CA, Leshner P, Kramer J, Allen G. Overcoming barriers to access and utilization of hospice and palliative care services in African American Communities. Omega. 2005;50(2):151–163. doi: 10.2190/qqkg-epfa-a2fn-ghvl. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Cancer prevention and control resolution (WHA58.22). World Health Assembly 58 Official Records. Geneva, Switzerland: Author; 2005. [Google Scholar]