Abstract
Introduction
The literature on community-based participatory research (CBPR) approaches for promoting healthy diet, nutrition, and preventing and controlling obesity in African American communities was systematically reviewed as part of the planning process for new research.
Methods
CBPR studies of diet, nutrition, and weight management among African Americans were identified from 1989 through October 31, 2015 using PubMed and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases and MeSH term and keyword searches.
Results
A total of 16 CBPR studies on healthy diet, nutrition, and weight management among African Americans were identified; outcome evaluation results were available for all but two. Of the remaining 14 studies, 11 focused on adults, 1 on children, and 2 on both children and adults. Eight studies employed CBPR methods to address diet, nutrition, and weight management in church settings. Four had a cluster randomized controlled design. Others had a pre-post test, quasi-experimental, or uncontrolled design. Only one study addressed four levels of the socioecological model; none addressed all five levels of the model. The studies identified in this review indicate that CBPR approaches can be effective for promoting healthy diet, nutrition, and weight management among African American adults but there is a need for additional studies with rigorous study designs that overcome methodologic limitations of many existing studies. There is only limited evidence for the effectiveness of CBPR approaches for promoting healthy eating and weight control among African American children and adolescents
Conclusion
To address health disparities, additional CBPR studies are needed to promote healthy diet, nutrition, and weight management in African American communities. Of particular interest are multilevel CBPR studies that include interventions aimed at multiple levels of the socioecological model.
Keywords: African Americans, community-based participatory research, diet, nutrition, obesity, weight management
Introduction
The obesity epidemic represents a serious threat to the health of Americans. Compared to whites of similar ages, African American children and adults have a higher prevalence of overweight and obesity (1, 2). In addition, evidence from randomized controlled trials has shown that African American men and women tend to lose less weight and have different trajectories for weight loss than their white peers who are exposed to the same interventions (3, 4). Perhaps accounting for these racial differences are a variety of factors, including attitudes and preferences related to eating; socioeconomic and cultural factors; targeted advertising of high-calorie foods and beverages to African Americans; and environmental factors that create barriers to limiting intake of foods high in fat and sugar (5, 6). Neighborhood deprivation, minority composition, and residential segregation have been linked to poor dietary patterns and obesity (7). In terms of residential proximity to supermarkets and other food outlets that provide nutritious foods such as fresh fruit and vegetables and whole grains, African Americans are less likely than whites to live in neighborhoods that support healthy eating (3, 7, 8). Many African Americans live in inner city areas where there is a high density of fast-food outlets and convenience stores that provide foods high in saturated fat, trans fats, and calories. The affordability of nutritious foods is also a concern as the costs of fruit and vegetables have increased compared to prices of sugar and refined grains (8). Members of African American families are more likely to have incomes below the poverty line (9). African Americans consume fewer servings of fruits and vegetables than U.S. whites and are more likely to have diets high in fat, calories, and sugar-sweetened beverages (10, 11). It is important to note that overweight and obesity are not solely a concern in low-income communities (1, 2). The epidemic of obesity among African Americans (and the U.S. population, in general) crosses the socioeconomic spectrum.
Socioecological models show how factors at the individual (attitudes, beliefs, health literacy, behaviors); interpersonal (friends, family, coworkers, church congregants); community (schools, workplaces, neighborhoods, faith communities, community-based organizations, community coalitions); institutional (academic institutions, health care organizations, state and local health departments); and societal levels influence diet, nutrition, and obesity in diverse communities (12). The socioecological model is a theory-based framework for understanding the multifaceted and interactive effects of individual-level and environmental factors that influence behaviors, and for identifying leverage points for promoting health within communities and organizations. At institutional and societal levels, healthy eating and weight control are influenced by state and federal laws and regulations and school policies relating to restrictions on trans fats and sugar-sweetened beverages. Requirements for restaurants to provide information about the caloric and nutritional content of food items are also relevant. At the community level, coalitions have addressed “food deserts” by establishing farmer's markets in disadvantaged minority neighborhoods and by reaching out to supermarket chains and grocery stores to increase the availability of affordable and nutritious foods such as fruits, vegetables, and whole grains. A concept derived from socioecological models, which must be tailored for specific behaviors, is that the most effective interventions should operate at multiple levels because behavior is influenced at multiple levels (13, 14).
Academic-community partnerships and community coalitions provide promising approaches for addressing obesity in local communities. In recent decades, a growing literature has developed on community-based participatory research (CBPR) approaches to promote healthy eating and weight control in African American communities. Many of these studies have used faith-based intervention approaches involving people identified through church congregations. The CBPR approach to promoting healthy behaviors and addressing obesity and grass-roots efforts led by community-based organizations and coalitions are in contrast to federal efforts to address obesity, which are generally considered to be top-down approaches (15).
As part of the planning process for CBPR studies addressing obesity among African Americans, we reviewed the published literature on this topic. The goal of this review was to determine if there is sufficient published evidence to determine whether CBPR is effective for promoting healthy diet, nutrition, and weight management among African Americans.
Methods
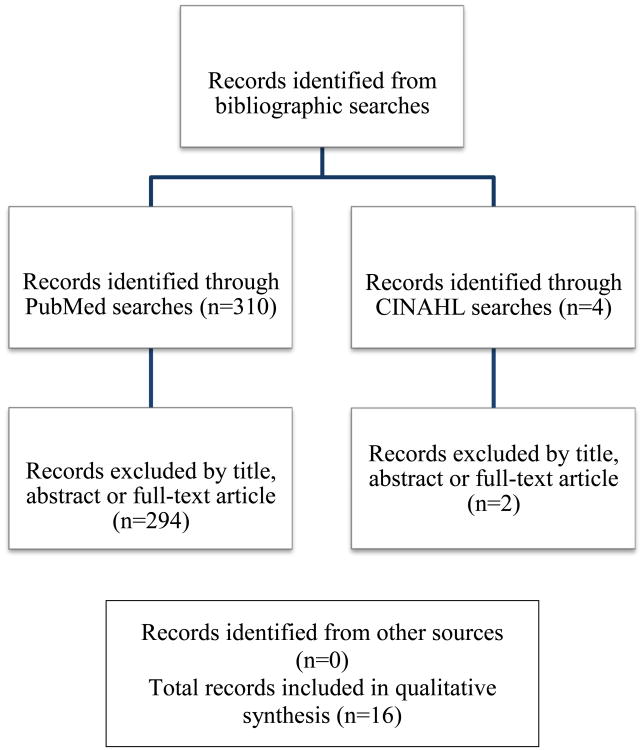
The present review is based upon bibliographic searches in PubMed and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) and relevant search terms. Articles published in English through October 31, 2015 were identified using the following MeSH search terms and Boolean algebra commands: (((((community-based participatory research) or (community-based study) or (community-based study) or (action research))) and (African Americans)) and (((weight) or (weight loss) or (weight management) or (diet weight) or (dietary) or (dietary intake) or (nutritional) or (health nutrition) or (diet weight loss))) and ((controlled before-after studies) or (comparative study) or (evaluation studies) or (intervention studies) or (randomized controlled trials) or (quasi-experimental)). Although the search criteria did not specify a begin date, the earliest article that met the search criteria was published in 1989. The searchers were not limited to words appearing in the title of an article. Studies that focused on patients with chronic diseases other than obesity were excluded, along with those that were limited to qualitative research (i.e., focus groups). Also excluded were studies in which <50% of the participants were African American. We used <50% African American as an exclusion criterion because health promotion studies that involve a heterogeneous target population (for example, non-Hispanic whites, Hispanics, and African Americans) are unlikely to have employed intervention materials that are culturally tailored for African Americans. Information obtained from bibliographic searches (title and topic of article, information in abstract, characteristics of study population, geographic locality of a study, and key words) was used to determine whether to retain each article identified in this way. In addition, reports included in Cohrane reviews (http://community.cochrane.org/cochrane-reviews) and reviewed the references of reports and published review articles were evaluated. A total of 321 citations were identified in the bibliographic searches (Figure 1). After screening the abstracts or full texts of these articles, 16 CBPR studies on promoting healthy diet, nutrition, and weight management among African Americans were identified. The two eligible studies identified in the CINAHL search overlapped with those identified in the PubMed search (Figure 1). The present review extends upon the work of earlier authors (16, 17) by including studies in the past few years and by focusing specifically on CBPR studies involving African Americans.
Figure 1.
Summary of search and exclusion process for identified studies.
Results
Outcome evaluation results were available from all but two of the studies (18). Of the 14 remaining studies, 11 focused only on adults, 1 on children, and 2 on both children and adults, as shown in Table 1. Four of the studies had a cluster randomized controlled design. Other studies had a pre-post, quasi-experimental, or uncontrolled design. Quasi-experimental studies share similarities with a randomized controlled trial or experimental design but they lack random assignment to intervention or control group; quasi-experimental designs allow the researcher to control assignment to the intervention condition using an approach other than random assignment. Eight studies employed CBPR methods to address diet, nutrition, and weight management in church settings. Only one study addressed four levels of the socioecological model. None of the studies addressed all five levels of the model.
Table 1.
CBPR studies on diet, nutrition, and weight management among African Americans.
| Study | Sample | Design | Results | Limitations |
|---|---|---|---|---|
| Ammerman et al. (18) | ≥1,300 members of 60 African American churches in 8 North Carolina counties | Cluster randomized controlled trial of a 12-month multilevel (individual, social, organizational, and community) nutrition intervention | Outcome evaluation results from this community-university partnership have not been published. | |
| Campbell et al. (19) | 2,519 adult members of 50 African American churches in 10 counties in North Carolina | 20-month cluster randomized trial of a multilevel (individual, social, community) intervention. The main outcome was consumption of 7 fruit and vegetable items according to National Cancer Institute 5-a-Day criteria. CBPR principles were followed. | At the 2-year follow-up, members of the intervention group consumed 0.85 (SE= 0.12) servings per day more than the delayed intervention group (P<0.0001). The largest increases were seen among people 66 years or older, those with education beyond high school, and those who attended church frequently. | Use of self-reported outcome measures assessed using a brief food frequency questionnaire |
| Choudhry et al. (20) | 40 African American children (24 girls and 16 boys, 54% overweight or obese) ages 5-12 yrs on Chicago's South Side | Pre-post test of a multicomponent intervention (environmental change, education on healthy eating and physical activity, and parent outreach) delivered during after-school care and at home | Post-intervention, BMI z scores decreased from 1.05 to 0.81 (p<0.001). Girls decreased their combined prevalence of overweight/obesity from 52% to 46%. The prevalence of overweight/obesity did not change among boys. | Small sample size, lack of a randomized controlled design, uncertain generalizability |
| Dodani & Fields (21) | 40 adult members (mean age 46 yrs, 85.3% female, 19.5% overweight, 48.8% obese, and 31.7% morbidly obese) of a church in Evans County, GA | Pre-post test of a spiritually based lifestyle modification program (diet, nutrition, physical activity, weight control) for diabetes prevention | Of the 35 participants who attended at least 10 sessions and provided information required for the study, 48% lost at least 5% of their baseline weight, 26% lost 7% or more, and 14% lost over 10% of their baseline weight. | Small sample size, lack of a comparison group, uncertain generalizability |
| Freedman et al. (22) | Predominantly low-income, urban, African American youth (n=65, average age 11 yrs), parents, guardians, and staff at four Boys and Girls Clubs in Nashville, TN. | Uncontrolled study of a multi-component environmental (farmers' market, Super Shopper voucher program, and Youth Leader Board) intervention designed to increase access to fresh fruits and vegetables | 34 farmers' markets occurred, resulting in 1,101 sales transactions of 5,750 units of fruits and vegetables. Financial vouchers were used to purchase 63% of the produce. All of the youth Super Shoppers came to a market at least once and made more purchase transactions than adults (P<0.05). | Lack of a comparison group, uncertain generalizability |
| Goldfinger et al. (23) | 26 overweight and obese African American adult (mean age 68 yrs) members of a church in Harlem, NY | Pre-post test of a peer-led, community-based course on healthy eating and active living. The main outcome was change in weight | Participants lost a mean of 4.4 pounds at 10 weeks, 8.4 pounds at 22 weeks, and 9.8 pounds at 1 year | Small sample size, lack of a randomized controlled design, uncertain generalizability |
| Harmon et al. (24) | 23 adult members of two African American churches in Columbia, SC; one intervention church (mean age of participants = 62 yrs, 60% female) and One comparison church (mean age 60 yrs,76.9% female) | Faith-based participatory study of a 12-week educational intervention designed to increase consumption of fruits and vegetables | At two months, a nonsignificant (P=0.07) increase in fruit and vegetable consumption was observed in the intervention group but this was not maintained at the conclusion of the study. | Small sample size, non-randomized design, use of self-reported outcome measures |
| Landry, et al. (25) | 269 adults (94% African American, 85% female, mean age 44 yrs) in Hattiesburg, Mississippi | 6-month, community-based, pre-post trial of an intervention consisting of motivational enhancement, social support, pedometer diary self-monitoring, and educational sessions. The outcome measures were steps per day, fitness, dietary intake, and psychosocial construct measures | For the dietary and physical activity outcome variables, temporal changes were observed only for sugar intake and steps per day. Sugar intake decreased by about 3 teaspoons and physical activity increased by about 2,010 steps per day | Lack of a randomized controlled design, uncertain generalizability, use of self-reported measures for dietary intake |
| Lasco et al. (26) | 70 obese African American residents (ages 18-59 yrs) of a neighborhood in Atlanta, GA | Pre-post evaluation of a multicomponent intervention (attitudes assessment, selection of a specific exercise class, and twice-weekly information on nutrition and community resources) | 42 (60%) of the participants lost weight and the weight of 8 (11%) of the participants remained the same (P=0.0009). | Lack of a randomized controlled design, uncertain generalizability |
| Scarinci et al. (27) | 565 African American women ages 45-65 yrs in rural Alabama counties | Cluster randomized trial comparing two interventions: promotion of healthy eating and physical activity (“healthy lifestyle” arm) vs. promotion of breast and cervical cancer screening. CBPR principles were followed. | At 12-month follow-up, participants in the “healthy lifestyle” arm showed significant positive changes (increased fruit/vegetable intake, decreased fried food consumption, increased physical activity). At 12 months, there was a 69% increase in the number of participants eating five or more servings of fruit and vegetables per day in the in the healthy lifestyle arm. At 24-months, these positive changes were maintained with healthy eating behaviors but not physical activity | Large differences in retention across intervention arms, use of self-reported outcome measures |
| Schulz et al. (28) | Residents of Detroit's East Side neighborhood | Case study description | Over a 2-year period, 18 community residents completed 2 eight-week project training sessions. After completion of the training, the community advocates implemented activities to prevent diabetes by promoting healthy diets and physical activity (walking club for seniors, community events focused on diabetes awareness for youth, older adults, residents of a shelter, and the community at large, healthy cooking demonstrations tailored to ensure cultural appropriateness). | Non-randomized design, lack of a comparison group, lack of a quantitative evaluation, uncertain generalizability |
| Parker et al. (29) | 35 African American women (ages 25-64 yrs) at churches in 3 rural counties of South Carolina | Pre-post test | Two different 10-week interventions (spiritually-based and nonspiritually-based) were pilot tested using a pre-post design. Both interventions led to significant reductions in BMI but the spiritually-based intervention (z = -1.97, P<0.01) led to greater reductions in BMI. | Non-randomized design, small sample size, uncertain generalizability |
| Ries et al. (30) | 485 low-income, predominately minority women (63% African American) in rural North Carolina (mean age 47.5 yrs) | Quasi-experimental design. CBPR principles were followed to address obesity, poverty, and low levels of education | For both African Americans (P<0.05) and whites (P<0.0001), intervention participants were more likely than comparison participants to move from contemplation to action/maintenance for the goal of increasing physical activity. For all participants, progression in stages of change mediated the intervention effect on physical activity, but not fruit and vegetable intake. Intervention group participants engaged in significantly more minutes of physical activity per week (138 minutes) than comparison participants (86 minutes, P<0.05). No difference was observed between study groups in fruit and vegetable intake (P=0.33). | Use of self-reported information about diet and physical activity |
| Wilcox et al. (31) | 1,257 participants (mean ages 54.1 yrs, 99.4% African American, 27.1% overweight, 61.8% obese) who attended 74 African Methodist Episcopal churches in North Carolina | Cluster randomized controlled trial of a CBPR intervention (full-day committee training, full-day cook training, and 15 months of mailings and technical assistance calls) targeting healthy eating and physical activity | In intention-to-treat analyses conducted using analysis of variance, there was a significant intervention effect in self-reported leisure-time moderate-to-vigorous intensity physical activity (P=0.02) but no effect for dietary outcomes. Analysis of covariance analyses for participants who completed both pre- and post-measurements showed an intervention effect for moderate-to-vigorous intensity physical activity (P=0.03) and self-reported fruit and vegetable consumption (P=0.03). | High attrition, use of self-reported information about physical activity and diet |
| Woods et al. (32) | 106 adults (73% female, 90% African American, 80% some college or above) from five churches (3 intervention, 2 control) in Colorado | Cluster randomized trial of diet, nutrition, an physical activity intervention (small group educational sessions, demonstrations of healthy food preparation, physical activities) developed using CBPR principles | At 2-months follow-up, the intervention group showed greater decreases in weight (P<0.02), BMI (P<0.05), and % body fat (P<0.03) than the control groups. An increase in physical fitness (P<0.10) was also observed. | Limited number of male participants, uncertain generalizability |
| Kim et al. (33) | 73 participants (71% female, mean age 54.1 yrs, 100% African American) from rural churches in North Carolina | Quasi-experimental design with an intervention group and a delayed intervention control group | Small groups led by trained community members met weekly for 8 weeks and emphasized healthy nutrition, physical activity, and faith's connection to health. The mean weight loss in the intervention group was 3.60 lbs., compared to 0.59 lbs. in the control group (P<0.001). The intervention was also associated with an increase in recreational physical activity (P<0.01). No significant difference was observed in fruit and vegetable consumption. | Non-randomized design, small sample size, use of self-reported information about fruit and vegetable consumption and recreational physical activity, uncertain generalizability |
BMI - body mass index, CBPR - community-based participatory research, lbs – pounds, SE – standard error, WIC – Women, Infants, and Children Program
Campbell et al. (19) conducted a CBPR study involving 2,519 adult members of 50 African American churches in ten counties in North Carolina. The counties were pair matched and randomly assigned to either intervention or delayed intervention conditions. A multicomponent intervention was delivered over a 20 month period. At the 2-year follow-up, members of the intervention group consumed 0.85 (standard error = 0.12) servings of fruits and vegetables more than the delayed intervention group (P < 0.0001). Self-reported information about fruit and vegetable consumption was not validated. The support of the pastors and statewide ministerial alliances contributed to the success of the study.
Choudhry et al. (20) conducted a pilot study involving 40 African American children ages 5-12 years who were attending after-school care on Chicago's South Side. The nutrition and physical activity intervention followed CBPR principles and had multiple components (environmental change, nutrition and physical activity education, and outreach by parents). Post-intervention, mean body mass index (BMI) z scores decreased from 1.05 to 0.81 (P<0.001). Girls decreased their combined prevalence of overweight/obesity from 52% to 46%.
Dodani and Fields (21) conducted a feasibility study of a spiritually based lifestyle modification program (diet, nutrition, physical activity, and weight control) for diabetes prevention. The participants included 40 adult members of a church in Evans County, Georgia who were overweight, obese, or morbidly obese. CBPR principles were followed to deliver a spiritually based lifestyle modification program (diet, nutrition, physical activity, and weight control) for diabetes prevention. Of the 35 participants who attended at least 10 sessions and provided information required for the study, 48% lost at least 5% of their baseline weight, 26% lost 7% or more, and 14% lost over 10% of their baseline weight. The study was limited by the lack of a comparison group.
Freedman et al. (22) conducted an uncontrolled study of a multi-component environmental (farmer's market, Super Shopper voucher program, and Youth Leader Board) intervention designed to increase access to fresh fruits and vegetables. The participants were predominantly low-income, urban, African American youth (n=65, average age 11 years) and parents, guardians, and staff at four Boys and Girls Clubs in Nashville, TN. About two-thirds of the youth reported the receipt of food assistance (e.g., food stamps, WIC, free or reduced-price school lunches) during the past year. A total of 34 farmers' markets occurred, resulting in 1,101 sales transactions of 5,750 units of fruits and vegetables. Financial vouchers were used to purchase 63% of the produce. All of the youth Super Shoppers came to a market at least once and made more purchase transactions than adults (P<0.05). Like the feasibility study by Dodani and Fields (21), the study was limited by the lack of a comparison group (22).
Goldfinger et al. (23) and a coalition of community and academic leaders conducted a pre-post design, pilot study of a peer-led, community-based course on healthy eating and active living (23). The participants were 26 overweight and obese African American adult members of a church in Harlem, NY. Participants lost a mean of 4.4 pounds at 10 weeks, 8.4 pounds at 22 weeks, and 9.8 pounds at 1 year.
Harmon et al. (24) conducted a faith-based participatory research study of a 12-week educational intervention designed to increase consumption of fruits and vegetables. The 23 participants were members of two African American churches (one intervention and one comparison) in Columbia, SC. At two months, a non-significant (P=0.07) increase in fruit and vegetable consumption was observed in the intervention group.
Landry et al. (25) conducted a 6-month, community-based, pre-post trial of an intervention consisting of motivational enhancement, social support, pedometer diary self-monitoring, and educational sessions. The participants were 269 adults in Hattiesburg, Mississippi. The outcome measures were steps per day, fitness, dietary intake, and psychosocial construct measures. For the dietary and physical activity outcome variables, temporal changes were observed only for sugar intake and steps per day. Sugar intake decreased by about 3 teaspoons and physical activity increased by approximately 2,010 steps per day. Self-reported information about dietary intake was not validated.
Using a pre-post design, Lasco et al. (26) evaluated a community-led multicomponent intervention that consisted of an attitudes assessment, selection of a specific exercise class, and twice-weekly information on nutrition and community resources). The participants were 70 obese African American residents of a neighborhood in Atlanta, GA, between the ages of 18 and 59 years. During the course of the intervention, 42 (60%) of the participants lost weight; the weight of 8 (11%) remained the same (P=0.0009).
Scarinci et al. (27) conducted a community-based, cluster randomized trial comparing two interventions: 1) promotion of healthy eating and physical activity (“healthy lifestyle” arm), and 2) promotion of breast and cervical cancer screening. The participants were 565 African American in rural counties in Alabama. At 12-month follow-up, participants in the “healthy lifestyle” arm showed significant positive changes (increased fruit/vegetable intake, decreased fried food consumption, increased physical activity). There was a 69% increase in the number of participants eating five or more servings of fruit and vegetables per day in the in the healthy lifestyle arm. In addition to the use of unvalidated information about the outcomes of interest, the study was limited by large differences in retention across intervention arms.
Schulz et al. (28) conducted an uncontrolled CBPR project on diabetes prevention among residents of Detroit's East Side neighborhood. Over a 2-year period, 18 community residents completed 2 eight-week project training sessions. After completion of the training, the community advocates implemented activities to prevent diabetes by promoting healthy diets and physical activity (a walking club for seniors; community events focused on diabetes awareness for youth, older adults, residents of a shelter, and the community at large; healthy cooking demonstrations tailored to ensure cultural appropriateness). A monthly fruit and vegetable minimarket was established at a community site to increase access to fresh fruits and vegetables in an area with few retail outlets carrying high-quality produce (28). An attempt was made to track participation and sales volume at minimarkets, but the evaluation was not fully implemented due to limited funding.
In 3 rural counties in South Carolina, Parker et al. (29) conducted a church-based weight loss intervention among 35 African American women. The study was developed with community input. Two different 10-week interventions (spiritually-based and nonspiritually-based) were pilot tested using a pre-post design. Both interventions led to significant reductions in BMI but the spiritually-based intervention (z = -1.97, P<0.01) led to greater reductions in BMI.
In rural North Carolina counties, Ries et al. (30) conducted a quasi-experimental study involving 485 low-income, predominately minority women (63% African American). The curriculum for the bi-weekly group meetings held over a 6-month period addressed healthy eating, physical activity, weight control, stress management, education, and job skills. For both African Americans (P<0.05) and whites (P<0.0001), intervention participants were more likely than comparison participants to move from contemplation to action/maintenance for the goal of increasing physical activity. Intervention group participants engaged in significantly more minutes of physical activity per week (138 minutes) than comparison participants (86 minutes, P<0.05). There was no difference between study groups in fruit and vegetable intake (P=0.33).
Wilcox et al. (31) conducted a cluster randomized controlled trial of an intervention (full-day committee training, full-day cook training, and 15 months of mailings and technical assistance calls) targeting healthy eating and physical activity in 74 African Methodist Episcopal churches in North Carolina. The churches were randomized to immediate or delayed intervention. The 1,257 participants had a high attrition. In intention-to-treat analyses conducted by use of analysis of variance, there was a significant intervention effect in self-reported, leisure-time moderate-to-vigorous intensity physical activity (MVPA) (P=0.02) but no effect for dietary outcomes. The study was limited by the use of self-reported information about the outcomes of interest.
With CPBR principles, Woods et al. (32) conducted a cluster randomized trial of diet, nutrition, and physical activity interventions (small group educational sessions, demonstrations of healthy food preparation, physical activities). The 106 adult were from five churches (3 intervention, 2 control) in Colorado. At 2-months follow-up, the intervention group showed greater decreases in weight (P<0.02), BMI (P<0.05), and % body fat (P<0.03) than the control groups. There was an increase in physical fitness (P<0.10).
Kim et al. (33) conducted a quasi-experimental study of a faith-based weight loss intervention; a delayed-intervention control group was used. The 73 participants were from rural churches in North Carolina. Small groups led by trained community members met weekly for 8 weeks and emphasized healthy nutrition, physical activity, and the connection of faith to health. The mean weight loss in the intervention group was 3.60 lbs. relative to 0.59 lbs. in the control group. The study was limited by the use of self-reported information about fruit and vegetable consumption and physical activity.
Discussion
The studies identified in this review indicate that CBPR approaches can be effective for promoting healthy diet, nutrition, and weight management among African American adults, but there is a need for additional studies with adequate sample sizes and rigorous study designs that overcome methodologic limitations of most existing studies. Of the CBPR studies identified in this review, the study by Campbell et al. (19) had the largest sample size. The multilevel (individual, social, community) intervention significantly increased consumption of fruits and vegetables in adults (19). The cluster randomized controlled trial by Wilcox et al. (31), which had the second largest sample size, found a significant intervention effect in adults for leisure-time physical activity but not for dietary outcomes. Because of the small number and methodological limitations of reported studies, there is only limited evidence for the effectiveness of CBPR approaches for promoting healthy eating and weight control among African American children and adolescents. Common study limitations include small sample sizes, the lack of a comparison group, and the use of self-reported information about the outcomes of interest. Self-reported information about height and weight can be validated through direct measurements. Self-reported information about physical activity can be validated using accelerometers. Self-reported information about vegetable consumption has been validated in epidemiologic studies using measurements of vitamin B-6 and carotenoids in plasma (34).
As a collaborative approach to research, CBPR equitably involves all partners in the research process (35, 36). The CBPR approach often involves partnerships between academic and community organizations with the goal of increasing the value of the research product for all partners (36) and has a goal of acknowledging and implementing the participants' needs, behaviors, and beliefs concerning their well-being. CBPR takes into account the strengths and insights that community and academic partners bring to framing health problems and developing solutions (36). Many of the studies identified in this review show that community members are often quite interested in being involved in CBPR and helping to ensure that the educational interventions that are developed are tailored to the needs of their community.
At the local level, numerous faith organizations and institutions are addressing the obesity epidemic and encouraging healthy eating. The black church in the United States has long addressed social and economic injustices. Poverty, discrimination, and other injustices are part of the contextual factors that contribute to high obesity rates in the African American community (37). As noted by Derose et al. (38), “congregations are often the last to leave distressed neighborhoods, thereby shouldering much of the burden of meeting community needs, and they can raise awareness about community problems and resources.” The collective efforts of faith organizations at the local, regional, and national level are helping to address pronounced health disparities, such as high rates of overweight, obesity, and obesity-associated chronic diseases (e.g., cancer, cardiovascular disease, and diabetes) among African Americans (39).
Frameworks that have been proposed for translating evidence into action highlight the desirability of identifying factors that contribute to obesity and points of intervention, defining opportunities for action, evaluating potential interventions, and working towards a portfolio of policies, programs, and actions (40). Action includes research-tested interventions that have been identified as part of the Guide to Community Preventive Services (www.thecommunityguide.org). To address obesity in children or adults, the Community Guide currently recommends behavioral interventions that aim to reduce recreational sedentary screen time among children; technology-supported multicomponent coaching or counseling interventions to reduce weight and maintain weight loss; and worksite programs to prevent and control obesity. For other interventions of potential interest (e.g., school-based programs), the Community Guide found insufficient evidence for a recommendation. There is a need for additional research to fill in these gaps in the evidence base, particularly studies of high-risk and under-studied populations (41).
Socioecological model provides a theory-based framework for understanding the multifaceted and interactive effects of individual-level and environmental factors that influence behaviors, and for identifying leverage points for promoting health within social networks (i.e., families, friends, coworkers), communities, and organizations (12). Included in the model are policy-level interventions (e.g., state and federal laws and regulations and school policies relating to restrictions on trans fats and sugar-sweetened beverages). Health interventions that address multiple levels of the socioecological model have been shown to be more effective that interventions aimed at a single level (12-14). Of all the CBPR studies identified in this review, the cluster randomized controlled trial by Campbell et al. (18) had the largest sample size by far. In addition, it employed a multilevel (individual, social, community) intervention. The results of this review suggest that researchers are challenged to address all five levels of the model in a single CBPR study.
Studies that involve partnerships between academic institutions and community partners (i.e., CBPR and community-engaged research) contribute to the evidence base of what is effective in addressing obesity in African American communities. This includes a) research-tested interventions that encourage healthy behaviors through individual-level interventions or by increasing social support for healthy eating and physical activity and b) community-level interventions that involve small group education, environmental changes, and other collective efforts to address obesity in African American communities. Additional research in this area is needed to fill in gaps in the evidence base about what works to address obesity among African American children, adolescents, and adults. Of particular interest are multicomponent CBPR studies that include interventions aimed at multiple levels of the socioecological model (13, 14).
Acknowledgments
This work was funded by the National Cancer Institute (R01CA166785).
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.An R. Prevalence and trends of adult obesity in the US, 1999-2012. [Accessed November 17, 2015];Obesity. 2014 doi: 10.1155/2014/185132. http://www.hindawi.com/journals/isrn/2014/185132/ [DOI] [PMC free article] [PubMed]
- 3.Kumanyika SK, Whitt-Glover MC, Haire-Joshu D. What works for obesity prevention and treatment in black Americans? Research directions. Obesity Reviews. 2014;15(Suppl 4):204–12. doi: 10.1111/obr.12213. [DOI] [PubMed] [Google Scholar]
- 4.Svetkey LP, Ard JD, Stevens VJ, Loria CM, Young DY, Hollis JF, et al. Predictors of long-term weight loss in adults with modest initial weight loss, by sex and race. Obesity (Silver Spring) 2012;20:1820–8. doi: 10.1038/oby.2011.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grier SA, Kumanyika SK. The context for choice: health implications of targeted food and beverage marketing to African Americans. Am J Public Health. 2008;98:1616–29. doi: 10.2105/AJPH.2007.115626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell LM, Szcypka G, Chaloupka FJ. Trends in exposure to television food advertisements among children and adolescents in the United States. Arch Pediatr Adolesc Med. 2010;164:794–802. doi: 10.1001/archpediatrics.2010.139. [DOI] [PubMed] [Google Scholar]
- 7.Larson NI, Story MT, Nelson MC. Neighborhood environments. Disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 8.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–24. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 9.Macartney S, Bishaw A, Fontenot K. U.S. Department of Commerce, Economics and Statistics Amininistration, U.S. Census Bureau; 2013. [Accessed November 17, 2015]. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007-2011. http://www.census.gov/prod/2013pubs/acsbr11-17.pdf. [Google Scholar]
- 10.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988-1994 to 1999-2004. Am J Clin Nutr. 2009;89:372–81. doi: 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 11.James DC. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African-Americans: application of a culturally sensitive model. Ethn Health. 2004;9:349–67. doi: 10.1080/1355785042000285375. [DOI] [PubMed] [Google Scholar]
- 12.Blocker DE, Fruedenberg N. Developing comprehensive approaches for the prevention and control of obesity among low-income, urban, African-American women. J Am Med Womens Assoc. 2001;56:59–64. [PubMed] [Google Scholar]
- 13.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Quarterly. 2009;87:123–54. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 15.Dietz WH. The response of the US Centers for Disease Control and Prevention to the obesity epidemic. Annu Rev Public Health. 2015;36:575–96. doi: 10.1146/annurev-publhealth-031914-122415. [DOI] [PubMed] [Google Scholar]
- 16.Lemacks J, Wells BA, Ilich JZ, Ralston PA. Interventions for improving nutrition and physical activity behaviors in adults African American populations: a systematic review, January 2000 through December 2011. [Accessed November 17, 2015];Prev Chronic Dis. 2013 10:E99. doi: 10.5888/pcd10.120256. http://www.cdc.gov/pcd/issues/2013/12_0256.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newton RL, Jr, Griffith DM, Kearney WB, Bennett GG. A systematic review of weight loss, physical activity and dietary interventions involving African American men. Obesity Reviews. 2014;15(Suppl 4):93–106. doi: 10.1111/obr.12209. [DOI] [PubMed] [Google Scholar]
- 18.Ammerman A, Washington C, Jackson B, Weathers B, Campbell M, Davis G, et al. A church-based nutrition intervention designed for cultural appropriateness, sustainability, and diffusion. Health Promotion Practice. 2002;3:286–301. [Google Scholar]
- 19.Campbell MK, Demark-Wahnefried W, Symons C, Kasbeek WD, Dodds J, Cowan A, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health Project. Am J Public Health. 1999;89:1390–6. doi: 10.2105/ajph.89.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choudhry S, McClinton-Powell L, Solomon M, Davis D, Lipton R, Darukhanavala A, Steenes A, et al. Power-up: a collaborative after-school program to prevent obesity in African American children. Prog Community Health Partnersh. 2011;5:363–73. [PMC free article] [PubMed] [Google Scholar]
- 21.Dodani S, Fields JZ. Implementation of the Fit Body and Soul, a church-based life style program for diabetes prevention in high-risk African Americans. A feasibility study. Diabetes Educator. 2010;36:465–72. doi: 10.1177/0145721710366756. [DOI] [PubMed] [Google Scholar]
- 22.Freedman DA, Bell BA, Collins LV. The Veggie Project: a case study of a multi-component farmers' market intervention. J Primary Prevent. 2011;32:213–24. doi: 10.1007/s10935-011-0245-9. [DOI] [PubMed] [Google Scholar]
- 23.Goldfinger JZ, Arniella G, Wylie-Rosett J, Horowitz CR. Project HEAL: peer education leads to weight loss in Harlem. J Health Care Poor Underserved. 2008;19:180–92. doi: 10.1353/hpu.2008.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harmon BE, Adams SA, Scott D, Gladman YS, Ezell B, Hebert JR. Dash of Faith: a faith-based participatory research study. J Relig Health. 2014;53:747–59. doi: 10.1007/s10943-012-9664-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landry AS, Thomson JL, Madson MB, Zoellner JM, Mohn RS, Noble J, et al. Psychosocial constructs and postintervention changes in physical activity and dietary outcomes in a lifestyle intervnention, Hub City Steps, 2010. [Accessed November 17, 20115];Prev Chronic Dis. 2015 12:140525. doi: 10.5888/pcd12.140525. www.cdc.gov/pcd/issues/2015;/14_o525.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lasco RA, Curry RH, Dickson VJ, Powers J, Menes S, Merritt RK. Participation rates, weight loss, and blood pressure changes among obese women in a nutrition-exercise program. Public Health Rep. 1989;104:640–6. [PMC free article] [PubMed] [Google Scholar]
- 27.Scarinci IC, Moore A, Wynn-Wallace T, Cherrington A, Fouad M, Li Y. A community-based, culturally relevant intervention to promote healthy eating and physical activity among middle-aged African American women in rural Alabama: findings from a group randomized controlled trial. Prev Med. 2014;69:13–20. doi: 10.1016/j.ypmed.2014.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, Ridella W, et al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am J Public Health. 2005;95:645–51. doi: 10.2105/AJPH.2004.048256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parker VG, Coles C, Logan BN, Davis L. The LIFE Project: a community-based weight loss intervention program for rural African American women. Fam Comm Health. 2010;33:133–43. doi: 10.1097/FCH.0b013e3181d594d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ries AV, Blackman LT, Page RA, Gizlice Z, Benedict S, Barnes K, et al. Goal setting for health behavior change: evidence from an obesity intervention for low-income women. [Accessed November 17, 2016];Rural and Remote Health. 2014 14:2682. http://www.rrh.org.au. [PubMed] [Google Scholar]
- 31.Wilcox S, Parrot A, Baruth M, Laken M, Condrasky M, Saunders R, et al. The Faith, Activity, and Nutrition Program. A randomized controlled trial in African-American churches. Am J Prev Med. 2013;44:122–31. doi: 10.1016/j.amepre.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woods G, Levinson AH, Jones G, Kennedy RL, Johnson LC, Tran ZV, et al. The Living Well By Faith Health and Wellness Program for African Americans: an exemplar of community-based participatory research. Ethn Dis. 2013;23:223–9. [PMC free article] [PubMed] [Google Scholar]
- 33.Kim KH, Linnan L, Campbell MK, Brooks C, Koenig HG, Wiesen C. The WORD (Wholeness, Oneness, Righteousness, Deliverance): a faith-based weight-loss program utilizing a community-based participatory research approach. Health Educ Behav. 2008;35:634–50. doi: 10.1177/1090198106291985. [DOI] [PubMed] [Google Scholar]
- 34.Merete C, Falcon LM, Tucker KL. Vitamin B6 is associated with depressive symptomatology in Massachusetts elders. J Am Coll Nutr. 2008;27:421–7. doi: 10.1080/07315724.2008.10719720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berkley-Patton JY, Moore E, Berman M, Thompson CB, Schleicher T, Hawes SM. Assessment of HIV-related stigma in a US faith-based HIV education and testing intervention. J Int AIDS Soc. 2013;16(Suppl 2):18644. doi: 10.7448/IAS.16.3.18644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith SA, Whitehead MS, Sheats JQ, Ansa BE, Coughlin SS, Blumenthal DS. Community-based participatory research principles for the African American community. J Georgia Public Health Assoc. 2015;5:52–6. [PMC free article] [PubMed] [Google Scholar]
- 37.Corbie-Smith G, Adimora AA, Youmans S, Muhammad M, Blumenthal C, Ellison A, et al. Project GRACE: a staged approach to development of a community-academic partnership to address HIV in rural African American communities. Health Promot Pract. 2011;12:293–302. doi: 10.1177/1524839909348766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Derose KP, Mendel PJ, Kanouse DE, Blumenthal RN, Castenada LW, Hawes-Dawson J, et al. Learning about urban congregations and HIV/AIDS: community-based foundations for developing congregational health interventions. J Urban Health. 2010;87:617–30. doi: 10.1007/s11524-010-9444-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peterson J, Atwood JR, Yates B. Key elements for church-based health promotion programs: outcome-based literature review. Public Health Nurs. 2002;19:401–11. doi: 10.1046/j.1525-1446.2002.19602.x. [DOI] [PubMed] [Google Scholar]
- 40.Swinburn B, Gill T, Kumanyika S. Obesity prevention: a proposed framework for translating evidence into action. Obesity Reviews. 2005;6:23–33. doi: 10.1111/j.1467-789X.2005.00184.x. [DOI] [PubMed] [Google Scholar]
- 41.Kumanyika SK, Obarzanek E, Stevens VJ, Hebert PR, Whelton PK. Weight loss experience of black and white participants in NHLBI-sponsored clinical trials. Am J Clin Nutr. 1991;53:1631S–38S. doi: 10.1093/ajcn/53.6.1631S. [DOI] [PubMed] [Google Scholar]