Abstract
Inflammatory diseases of mucosal organs are significantly influenced by the microenvironment in which they reside. Cytokines found within this microenvironment contribute significantly to endpoint functions of the mucosa. Studies dating back to the 1990s have revealed that epithelial cells are both a source as well as a target for numerous cytokines and that such signaling can substantially influence the outcome of mucosal disease, such as inflammatory bowel disease. Here, we will review literature regarding intestinal epithelial cells as sources and responders to cytokines found in the intestinal milieu. These studies highlight the dynamic nature of these pathways and lend insight into the complexity of treating mucosal inflammation.
Keywords: Inflammation, Mucosa, Colitis, Leukocyte, Epithelium, Murine model
Background
Epithelial cells that line mucosal organs are uniquely positioned to serve as a line of communication between the immune system and the external environment. In their normal state, mucosal surfaces of the alimentary tract are exposed on the luminal surface to high concentrations of foreign antigens, while at the same time, intimately associated with the immune system via subepithelial lymphoid tissue [1]. As a result, the epithelium forms an important barrier, preventing the free mixing of luminal microbiota/antigenic material with the lamina propria that houses the mucosal immune system [1]. This latter capability is attributable primarily to intercellular tight junctions, which function as selectively permeable gaskets that circumferentially join epithelial cells at their apices. Tight junctions regulate the passive permeation of hydrophilic solutes through the “paracellular” space. Tight junctions are dynamic structures, the permeability of which is a highly regulated process [2], whereby dysregulation can result in a multiplicity of disease states [3]. A second important function of the epithelium is the maintenance of mucosal hydration [4]. A plethora of epithelial stimuli (secretagogues) activate membrane ion channels and transporters that result in absorption or secretion of ions that provide the driving force for paracellular water transport. Like many aspects of cell biology and immunology, this view has changed dramatically in the past decade. The epithelium is now viewed as an active part of mucosal innate immunity and orchestrates mucosal responses in a variety of diseases [1, 5].
The observation that epithelial cells produce and respond to cytokines has contributed significantly to the burgeoning area of mucosal immunology. In the past, it was broadly accepted that mucosal immunity differed from other classical immune responses, and that the difference likely rested on the ability of mucosal tissues to separate and distinguish themselves from the outside world. The observations that epithelial cells respond to, and provide an available reservoir of cytokines, chemokines and growth factors have ushered in a new view of the epithelium as a functionally dynamic cell type critical for normal innate immune responses. It is important to consider that the surface area of the intestine covered by epithelial cells is orders of magnitude larger than that covered by immune cells, and thus, even with smaller amounts produced per epithelial cell, the total quantity of epithelial-derived cytokine can be quite large and physiologically important in this regard. Here, we will review the recent literature with regard to epithelial cytokine responses, with particular emphasis on functional consequences within the intestinal mucosa.
Intestinal epithelial cytokine receptors
The microenvironment surrounding intestinal epithelial cells (IEC) is particularly enriched with cytokine-liberating cell types. In close proximity, and even juxtaposed against the basolateral epithelial membrane, are intraepithelial lymphocytes, dendritic cells, and resident eosinophils [5]. During disease states, the number and composition of these cells can dramatically change, providing a new array of signals for which epithelial cells must adapt. As such, in both health and disease, cytokines can be delivered directly to the epithelial plasma membrane. Important in this regard, the cytokine receptors studied to date are expressed in a polarized fashion. With some exceptions (see later), cytokine receptors are expressed on the basolateral surface, in close physiologic proximity to cytokine sources.
One of the first cytokines studied with regard to paracrine activation of intestinal epithelia was IFNγ [6]. This was particularly interesting given that IFNγ production is readily detectable in the mucosa, and the mucosa is one of the more enriched sources of IFNγ [7]. During numerous disease states, the number of lymphocytes increases, and upon antigenic challenge of mucosal T-lymphocytes, these older studies revealed IFNγ signal is markedly enhanced in the mucosa [7]. The biological effects of IFNγ are pleiotropic and have been most extensively studied in its role as a modulator of the immune system. IFNγ-elicited immunomodulation may extend to cell types not classically associated with the immune system. For example, older studies showed compelling evidence that this lymphokine elicits MHC class II molecule expression on epithelial cells, and as a result, these cells may become primed with the ability to present antigen [8, 9].
Since these initial studies with IFNγ, functional receptors for a wide variety of cytokines (as well as those for growth factors and chemokines), have been described [1] (see Table 1). It is notable that the expression of these receptors can also be regulated by cytokines and inflammatory stimuli. For example, IFNγ has been shown to regulate the IEC IL-1 and IL-6R [10] and IFNγ induces IEC TNFγR II [11]. Some redundancy also exists among the expression and function of these cytokine receptors. For instance, functional IL-2 receptors are expressed on IEC [12], the signaling of which requires the dimerization of the IL-2 receptor beta chain and a common gamma chain that is shared with IL-7 and IL-9 [13]. Similarly, IL-4 and IL-13 receptors share a common heterodimeric IL-4 alpha chain [14].
Table 1.
Roles of cytokines in epithelial function
| Epithelial function | Regulatory cytokines | Target cells |
|---|---|---|
| Barrier | IFNγ, TNFα, IL-1β, IL-10, IL-6, IL-22, IL-4, IL-13 | IECs |
| Leukocyte recruitment | IL-8, MCP-1, CCL20 | Leukocytes |
| Antigen presentation | IFNγ, TSLP, APRIL | IECs, dendritic cells, B cells |
| Homeostasis | IL-10, TGFβ, TSLP, APRIL, IL-25, IL-22 | IECs, dendritic cells, macrophages, B cells |
| Proinflammatory response(s) | IFNγ, TNFα, IL-1β, IL-8 | IECs, leukocytes |
| Regulation of solute/water transport | IFNγ, IL-4, IL-13 | IECs |
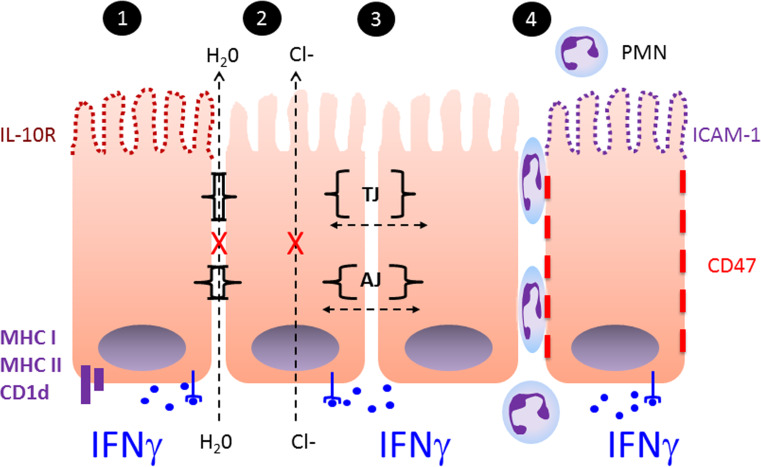
It was recently shown that intestinal epithelial cells express IL-10 receptors in response to IFNγ activation [15]. From initial microarray analysis, these studies revealed that IFN-γ selectively induced the expression of the alpha chain of the IL-10 receptor (IL-10R1, also called IL-10RA) on intestinal epithelia. This receptor complex shares a common IL-10R2 chain with five class 2 cytokines, namely IL-10, IL-22, IL-26, IL-28 and IL-29 [16]. The IL-10R2 chain was shown to be constitutively expressed in high levels in both cultured intestinal epithelia as well as epithelial cells in intact colonic tissue [17]. Notably, further analysis revealed that IL-10R1 was expressed predominantly on the apical membrane of polarized epithelial cells. Receptor activation functionally induced canonical IL-10 target gene expression in epithelia and resulted in enhanced barrier restitution following injury. Studies of colitis in intestinal epithelial-specific IL-10R1-null mice revealed a remarkable increase in disease susceptibility associated with increased intestinal permeability. These results provided important insight into an underappreciated role of epithelial IL-10 signaling in the maintenance and restitution of epithelial barrier and of the temporal regulation of these pathways by IFN-γ (Fig. 1). While such studies largely analyze single cytokine-elicited modulations on cell surfaces/secreted proteins, in aggregate, these results support the original idea of a global phenotypic switch from cells expressing classic epithelial function (e.g. barrier, ion transport) to those with significant immune function (regulated MHC function, chemokine and cytokine balance, coordination of leukocyte trafficking) [18].
Fig. 1.
IFN-gamma as a model cytokine signaling hub in the intestinal mucosa: 1 IFN-gamma signaling through basolaterally localized receptors induces the expression of immune regulatory components including MHC class I and II, CD1d as well as the apical IL-10R. 2 Through the down-regulation of CFTR and multiple ion channels in the epithelial membrane, IFN-gamma abrogates electrogenic chloride secretion and associated water transport (see text for details). 3 IFN-gamma signaling increases epithelial permeability through the regulation of tight junction (TJ) and adherens junction (AJ) component expression. 4 IFN-gamma signaling induces the apical expression of ICAM-1 and the basolateral expression of CD47. Together this allows migration and apical localization of neutrophils (PMN)
Epithelial endpoint responses to cytokines
The intestinal mucosa is a particularly complicated tissue. The complex structure of the intact intestinal mucosa (many cell types including epithelia, endothelia, smooth muscle, nerves, etc.), as well as cells that traffic through the intestinal mucosa (monocytes, dendritic cells, lymphocytes, eosinophils and neutrophils), is organized in a three-dimensional fashion and contributes to the dynamic nature of this tissue. Each individual cell type can be a source of cytokines and each expresses its own array of cytokine responses. Studying this tissue has been complicated by the need for primary cultures of native epithelial cells. Only recently have we been able to culture primary cells in a reliable manner that allows for interpretation of tissue function [19]. The ability to culture complex 3D epithelial tissue, known as enteroids, colonoids or organoids, based on cellular sources and culture conditions, has the potential to significantly expand our understanding of epithelial responses and interactions [20–22]. Nonetheless, the majority of studies have relied on cultured epithelial cell lines, a number of which form polarized cell monolayers with high barrier and ion transport properties which recapitulate native epithelia in both structure and function. Here, we will discuss the direct consequences of cytokines on aspects of epithelial function (Table 1).
A. Epithelial barrier function The loss of epithelial barrier function, with concomitant increases in paracellular permeability, has been reported in a number of enteropathies, including the inflammatory bowel diseases (IBD) Crohn’s disease and ulcerative colitis [23]. Debates still exist as to whether decreased barrier function is associated with the etiology of IBD or rather, as a potentiating factor of ongoing disease [24]. Nonetheless, of particular interest is the observation that epithelial barrier function is markedly attenuated upon exposure to pro-inflammatory cytokines [25]. A number of elegant studies have addressed the molecular details of this response. For instance, Mankertz et al. originally demonstrated that TNFγ and IFNγ independently and synergistically down-regulate transcription of occludin [26], one of the transmembrane “sealing” proteins localized to the tight junction [27]. This transcriptional response mapped within the occludin promoter to a ~200 bp fragment upstream from the transcription start site, an area rich in binding sites for the transcription factors AP2 and NFIL6 (CEBPβ). It has also been reported that IFNγ regulates epithelial homeostasis through convergent beta-catenin signaling modules, involving increased Dkk1-mediated apoptosis with extended cytokine exposure and reduced proliferation through depletion of the Wnt coreceptor LRP6 [28]. Similarly to IFNγ and TNFγ, one of the critical proinflammatory cytokines in the intestine, IL-1β, has been demonstrated to increase epithelial tight junction permeability, also by down-regulation of occludin expression, in an NF-κB dependent manner [29]. Other cytokines, including both IL-4 and IL-13, attenuate epithelial barrier function in vitro [30], and compelling evidence exists that IL-4 significantly enhances transepithelial transport of lumenal antigens in vivo [31, 32]. Additionally, IL-6 has been demonstrated to attenuate IEC barrier function in vitro, mainly through a claudin-2 dependent increase in tight junction permeability [33, 34]. Conversely, IL-6, which is produced by several cell types including epithelial cells and intraepithelial lymphocytes, has been shown to protect epithelial cells from apoptosis and promote epithelial proliferation in the setting of injury [35, 36].
Anti-inflammatory cytokines mainly have a protective effect on intestinal epithelial barrier function. Mice lacking IL-10 (IL-10KO mice) develop spontaneous microbiota-dependent colitis and are a well-established model of Crohn’s colitis. Prior to the onset of colitis, it has been established that these mice develop a permeability defect in the ileum and colon associated with elevated levels of TNFα and IFNγ [37]. IECs are demonstrated sources of IL-10 [38] and significant evidence exists that IL-10 contributes to the development of mucosal tolerance of commensal bacteria and homeostasis as previously discussed in the case of IL-10KO mice. As noted earlier, IEC-specific IL-10R1 deletion leads to barrier defects which are associated with increased pro-inflammatory cytokine expression and increased susceptibility to experimental colitis which supports the importance of IL-10 signaling in maintenance of the epithelial barrier [15]. IL-10’s protective effects are likely related to inhibition of the effects of TNFα and IFNγ on the epithelial barrier, given that therapy targeted towards restoring the permeability defect alone, is sufficient to significantly attenuate development of colitis [39]. It was recently demonstrated that IL-10 specifically suppresses tyrosine phosphorylation of signal transducer and activator of transcription-1 (STAT-1), a component of the IFNγ-induced DNA complex [40].
Another cytokine in the IL-10 family, IL-22, has recently been identified as important in maintenance of the intestinal epithelial barrier. It has been demonstrated to be protective in models of experimental colitis in mice and increased expression has been noted in the colons of patients with ulcerative colitis and Crohn’s disease [41]. IL-22 is produced mainly by cells of the lymphoid lineage including T cells and innate lymphoid cells including natural killer cells and lymphoid tissue inducer cells [42–45]. IL-22 binds to its heterodimeric receptor consisting of IL-22R1 and IL-10R2 located on the basolateral surface of colonic epithelial cells [46–49]. IL-22 signaling in IECs is via STAT3 [50, 51] and acts to augment the production of antimicrobial peptides, mucin, and proinflammatory cytokines while increasing epithelial migration and proliferation [47, 49, 52]. In total, IL-22 signaling in the epithelium appears to play a primary role in reconstitution of the epithelial barrier in the setting of injury.
B. Epithelial ion and water transport A number of cytokines have also been shown to influence epithelial electrogenic chloride secretion, the transport event responsible for mucosal hydration. This aspect of epithelial function has been studied in detail utilizing IFNγ [18, 53–55]. For example, exposure to IFNγ elicits a marked attenuation in stimulated Cl− secretion and concomitant water transport. Importantly, the observed downregulation of Cl− secretion is not simply a reflection of altered barrier function of IFNγ treated monolayers. The IFNγ-mediated attenuation of Cl− secretion was demonstrated at times which predated any alteration in barrier function. The global nature of IFNγ-mediated downregulation of Cl− secretion is further highlighted by the fact that agonists acting through differing signaling pathways and exerting primary effects at differing membrane channels (Ca2+, receptor-mediated and non-receptor-mediated cAMP pathways) were all markedly downregulated. The influence of IFNγ on chloride secretion was documented using rate constant measurements of uptake/efflux experiments which delineate the specific transport proteins involved independent of monolayer confluency. Interestingly, these later studies demonstrated that the functionally defined surface expression of all transporters, pumps, and channels contributing to Cl− secretion were downregulated by IFNγ. Extensions of these studies revealed that IL-4 and IFNγ post-transcriptionally downregulate expression of the cystic fibrosis transmembrane regulator (CFTR) in intestinal cell lines [30, 53]. Interestingly, it was also found that post-colitis epithelial responses may be selectively impaired. Utilizing a rat model of colitis, Asfaha et al. demonstrated that at 6 weeks post-colitis induction, barrier function defects had resolved but colonic secretory dysfunction persisted [56]. These findings paralleled increased bacterial translocation and increased colonic aerobes, suggesting that prolonged secretory impairment may underlie the chronic nature of enteropathies such as IBD. An interesting exception with regard to cytokine influences on ion transport is that of IL-4 and IL-13. While these cytokines share common receptor subunits and in most cases display overlapping functions (e.g., attenuation of barrier function) [57], only IL-4 appears to influence electrogenic chloride secretion [30]. This finding was one of the first divergent functions ascribed to these apparently redundant cytokines, although some studies have suggested no differences between IL-4 and IL-13 with regard to proximal receptor activation [58]. Nonetheless, a number of discernible differences between IL-4 and IL-13 have now been documented. These differences lie in activity associated with two novel proteins, termed IL-13R alpha 1 and 2 [59, 60], which demonstrated that IL-13 signaling may be more complicated than first appreciated. More work is required to definitively define the relative role of IL-13 and IL-4 in epithelial responses. Some studies also indicate an interesting role for epidermal growth factor, a homolog of TGFα, in inhibition of Ca2+-mediated epithelial chloride secretion. For instance, Keely et al., reported that transactivation of the epithelial EGF receptor by the muscarinic agonist carbachol may mediate inhibitory influences on electrogenic chloride secretion [61], and as such, may provide an “off switch” for chloride secretion under some circumstances.
C. Interactions with the microbiota The alimentary tract is initially sterile in utero but soon after birth is subject to colonization by a complex variety of anaerobic and aerobic bacteria ranging in density from 103 organisms per ml in the upper digestive tract up to 1012 in the colon [62]. There is increasing evidence that the composition of the commensal microbiota influences disease susceptibility, responses to environmental antigens and challenge from pathogenic organisms. Intestinal epithelial cells play a significant role in regulating the response to the microbiota through multiple pattern recognition receptors that recognize microbial-associated molecular patterns (MAMPs) and facilitate crosstalk with luminal bacteria and their antigens. These include Toll-like receptors (TLR) which are expressed on apical, basolateral and endosomal membranes [63] as well as nucleotide oligomerization domain-like receptors (NLR) which are present in the cytosol. TLRs recruit adaptor proteins such as MyD88, or TRIF in the case of TLR3 and TLR4, which lead to activation of the MAPK pathway or NF-κB which translocates to the nucleus to initiate transcription of cytokines and chemokines. NLRs similarly activate the MAPK and NF-κB pathways but through alternative mechanisms [5].
Apical or basolateral stimulation of polarized intestinal epithelial TLRs appears to have different effects on cytokine production that may be important in maintaining intestinal homeostasis. It has been demonstrated that basolateral stimulation of TLR3, TLR5 and TLR9 leads to significant expression of the mainly neutrophil chemokine, IL-8/CXCL8, but not apical stimulation, while the opposite is the case for TLR2 [64, 65]. Interestingly, while TLR9 is expressed apically and basolaterally, IL-8 is only produced after basolateral stimulation while apical stimulation inhibits IL-8 production, even with subsequent basolateral stimulation. This signaling mechanism, termed the “polarizing-tolerizing” response [66], suggests a mechanism by which epithelial cell responses are dampened by luminal commensal bacteria in homeostasis while in the setting of epithelial barrier disruption, recruited leukocytes in close proximity to IECs may play a role in eliciting a proinflammatory IEC response to even commensal bacteria [67]. TLR5 expression isolated to the basolateral membrane appears to be an alternate mechanism for sensing mucosal bacterial invasion/translocation leading to a protective homeostatic response that includes IL-8 expression [65]. In the absence of TLR5, there is significant dysregulation of commensal bacterial populations, increased translocation of bacteria to extra-luminal sites and development of colitis associated with TLR4 mediated proinflammatory cytokine signaling [68]. Part of the reason for this development may be the loss of TLR5 mediated crosstalk between IECs and B cells which is epithelial thymic stromal lymphoprotein (TSLP) and a proliferation-inducing ligand (APRIL) dependent and promotes IgA antibodies active against commensal bacteria that help regulate their population [69].
D. Regulation of adaptive immunity Appropriate responses to non-pathogenic constituents of the commensal microbiota are regulated in part by crosstalk between IECs and resident/non-resident antigen presenting cells (APCs) such as macrophages and dendritic cells. In response to commensal bacteria, IEC derived cytokines, TSLP and transforming growth factor β (TGFβ), promote tolerant APCs which then traffic to secondary lymphoid sites and promote the development of regulatory T cells [70]. IECs constitutively express TSLP mRNA and protein at baseline which can be increased upon exposure to multiple stimuli including bacteria, viruses, parasites and proinflammatory cytokines like IL-1β and TNFα. NF-κB has been identified as a transcriptional activator of TSLP [71]. Both TSLP and TGFβ play a role in conditioning dendritic cells to downregulate inflammatory cytokines and skew naïve T cells towards a Th2 > Th1 phenotype as well as promote Foxp3+ Treg differentiation [72]. The absence of TSLP signaling worsens experimental colitis in mice associated with increased proinflammatory cytokine production and increased IFNγ+ CD4+ T cells in mesenteric lymph nodes as well as inadequate responses to helminth infection [73]. TSLP and APRIL from epithelial cells are important for triggering IgA class switching in effector B cells independently and with the assistance of mucosal dendritic cells [69]. APRIL is a member of the TNF ligand family and is induced in IECs through stimulation of TLRs by commensal bacteria while epithelial TSLP also stimulates dendritic cell production of APRIL [69]. TLR stimulation and pathogenic bacterial exposure has been demonstrated to promote recruitment of B cells, dendritic cells and T cells through IEC expression of the chemokine CCL20 [74–76]. Exposure to commensal bacteria, however, does inhibit epithelial inflammatory cytokine expression, including the chemokine CCL20 [77–79]. The commensal microbiota also stimulates production of IL-25 (IL-17E) by IECs which acts to limit colonic IL-23 production (which plays a role in IBD pathogenesis), and regulate the numbers of IL-17 producing CD4+ T cells (Th17), which may play a proinflammatory role under certain conditions [80–82].
E. Antigen processing and presentation The overwhelming majority of antigen encounters occurs at mucosal surfaces, particularly those associated with the intestine. Moreover, this surface is constitutively bathed in a heterogeneous population of microorganisms comprised of the commensal flora [62]. While IECs are important for the conditioning of tolerant APCs and T cells in response to the microbiota, IECs can also independently act as APCs and promote Foxp3+ Treg development utilizing MHC class II [83]. MHC class II is constitutively expressed by villus epithelial cells of the small intestine of rodents and humans and upregulated by inflammation, presumably in response to cytokines such as IFNγ. Receptor- and non-receptor-mediated processes of antigen uptake have the capability of delivering macromolecules into endosomal compartments in association with MHC class II antigen presentation. Upon exposure to IFNγ in vitro, MHC class II is distributed predominantly on the basolateral surface consistent with a presentation function to CD4+ intraepithelial and lamina propria lymphocytes [84]. Although little is known of the MHC class II associated antigen processing machinery in IECs, it is clear that IECs may express invariant chain, cathepsins and process soluble antigens for presentation to T cells [85]. In modeling MHC class II function, Hershberg, et al. originally provided strong evidence for epithelial uptake of soluble antigen either apically or basolaterally and presentation from the basolateral surface [86]. Interestingly, in this system, antigen presentation was more efficient as a consequence of receptor-mediated uptake when antigen was coupled to the cholera toxin B subunit which, targets uptake by GM-1 gangliosides. Since IECs take up antigen poorly, receptor-mediated uptake may be of major importance to such a process. In addition, basal processing, which models antigen delivered paracellularly, revealed T cell responses to neoepitopes not observed when processing proceeded from the apical surface. Taken together, these studies suggest antigen uptake under non-inflammatory (antigen uptake apical) and inflammatory (antigen uptake basal) conditions may have different outcomes. The consequences of MHC class II presentation are, however, unclear. Some evidence exists in support of MHC class II function in vivo [85], and other work revealed that the co-stimulatory molecule CD58, but not CD80 or CD86, was observed to be expressed constitutively on both native epithelia and in T84 and HT-29 cell lines [87]. Surface expression of CD58 was polarized to the basolateral surface of the cell, and antibodies directed against CD58, but not CD80 or CD86, inhibited the stimulation of CD4+ T cell proliferation mediated by epithelia.
In addition to MHC class I and II antigens, intestinal epithelia constitutively express the non-classical MHC molecule CD1d, a transmembrane molecule with a short cytoplasmic tail expressed as a β2-microglobulin-associated 48kD glycoprotein and novel β2-microglobulin-independent 37kD nonglycosylated protein on intestinal epithelia [88]. Like MHC class I and II, epithelial CD1d is induced by IFNγ [89]. Mouse CD1 and human CD1d have been shown to present a model glycolipid antigen α-galactosyl-ceramide (α-GalCer) to a specialized subset of T cells (NK-T cells) that expresses both the TCR/CD3 complex and CD161 [90]. NK-T cells utilize an invariant TCR-α chain paired with a limited set of TCR-β chains. In mice, this invariant TCR is composed of Vα14-Jα281 paired predominantly with Vβ8.2, while in humans, a homologous TCR is found that is comprised of Vα24-JαQ paired with Vβ1[91]. Cross-linking of the non-classical MHC molecule CD1d expressed by IECs leads to protective IL-10 production, which may dampen proinflammatory cytokine-mediated barrier disruption [38]. Studies using genetic mouse models have revealed that IEC-specific deletion of CD1d or IL-10 results in NKT cell mediated colitis [92]. NK-T cells appear to play an important role in regulating immune responses through their rapid production of large amounts of IL-4 and IFNγ upon stimulation. In support of this, they have been implied to be critical for tumor surveillance and the control of viral infections and certain autoimmune disorders [90].
F. Neutrophil trafficking and epithelial cytokine regulation Neutrophil (polymorphonuclear leukocyte, PMN) accumulation on the luminal side of intestinal epithelia, termed the crypt abscess, is one of the pathological hallmarks of inflammatory intestinal disease [93]. PMN migration into and across intestinal epithelia is a result of an orchestrated series of steps and the interplay of numerous cell types. In the late 1960s, it was observed that mice colonized with pathogenic bacterial strains resulted in the large scale accumulation of PMN at the epithelial surface [94]. Such morphologic observations lead to a burgeoning area of research into defining mechanism(s) of bacterial–epithelial–PMN interactions. A few highlighted studies provide important insight into basic mechanisms of inflammation. First, it is clear that pathogenic bacteria have evolved complex mechanisms to utilize host machinery to successfully invade and colonize the epithelium. The interaction of Shigella species with epithelial cells, for example, includes interactions of bacteria with the epithelial cell surface and release of Ipa proteins through a specialized type III secretion system. A complex signaling process involving activation of small GTPases of the Rho family and c-src results in dramatic rearrangements of the subcortical cytoskeleton. Actin-mediated motility promotes efficient colonization of the host cell cytoplasm and rapid cell-to-cell dissemination through protrusions that are engulfed by adjacent cells in a cadherin-dependent process [95]. Second, successful bacterial invasion transforms infected cells into strongly proinflammatory cells, not the least of which includes the liberation of numerous factors for recruitment of large numbers of PMN to the epithelial surface. These factors include chemokines, cytokines, cell adhesion molecules and lipid mediators [1]. Intracellular invasion of IECs by pathogenic bacteria in vitro has been demonstrated to elicit a strong leukocyte independent inflammatory cytokine response, typically involving expression of IL-8, MCP-1, TNFα, and GM-CSF [96]. Additionally, polarized IECs express receptors for TNFα and IL-1β on the basolateral surface and several types of mucosal immune cells elaborate these pro-inflammatory cytokines in the setting of infection which induce chemokine production by IECs [97]. Third, some pathogenic bacterial strains have developed mechanisms to defend against host inflammatory elements. For example, studies in the oral cavity have indicated that active bacterial infection (e.g. P. gingivalis) may “paralyze” chemokine generation and subvert a number of PMN functions [98].
The molecular details of PMN–epithelial interactions have evolved. It is now appreciated that adhesion-based interactions, involving specific cell adhesion epitopes, are the primary means by which PMNs interact with epithelial cells [93]. For example, initial adhesion events between PMN and epithelia are dependent on PMN β2 integrins [99]. These integrins, like others, are heterodimeric glycoproteins that exist in four forms on the PMN. Each displays a unique α-subunit (CD11a, b, c, or d) and an identical β-subunit (CD18) [100]. The epithelial counter-receptor for PMN β2 integrins remains elusive, and functional mapping studies of this β2 integrin-dependent pathway has suggested that the profile of inhibition is distinct from that of other known ligands of CD11b/CD18 [93]. Such data suggest novel pathways for PMN trafficking across the epithelium, and discovery of such pathways provides a potential therapeutic target.
Unlike endothelial cells, a number of studies have demonstrated that intercellular adhesion molecule-1 (ICAM-1) is not an epithelial ligand during transmigration. Rather in some conditions, ICAM-1 may function as an apical anchor for PMN. Original studies using either enteric bacterial strains or IFNγ as activating stimuli resulted in induction of ICAM-1 exclusively to the apical membrane domain [101, 102] (see Fig. 1). These studies were verified in tissue sections from IBD patients [101, 102]. Studies directed at defining the influence of cytokines on PMN transepithelial migration revealed that IFNγ significantly modulates PMN transmigration, and does so in a polarized manner [103]. In contrast to apical-to-basolateral directed migration (i.e., non-physiologic), both IFNγ and IL-4 markedly downregulated transepithelial migration of PMN in the physiologic direction [57, 103]. This cytokine influence on transmigration was not secondary to IFNγ influences on epithelial tight junction permeability. Moreover, this downregulation of PMN migration in the physiologic direction, however, was not due to failure of PMN to move across filters and into monolayers. Indeed, IFNγ exposure to epithelia increased the number of PMN which had moved into the basolateral space of the epithelium in naturally directed transmigration. Specifically, it appeared that in naturally directed migration, IFNγ may enhance the retention time of the recruited PMN in the paracellular space below tight junctions, and did so, at least in part, by inducing a basolateral ligand on the membrane of intestinal epithelia. Later studies identified a functionally inhibitory monoclonal antibody (mAb) which blocks PMN transmigration, but not PMN adhesion, to epithelia [104]. Subsequent experiments revealed that the antigen recognized by this mAb is CD47 (also termed integrin-associated protein), a previously cloned protein with homology to the immunoglobulin supergene family and with multiple ligands and a number of demonstrated leukocyte functions [105]. As predicted by the above-described experiments, epithelial CD47 surface expression was induced by IFNγ [104]. Thus, CD47 is critically important for successful mucosal inflammation provides a potential therapeutic target.
While exposure to commensal bacteria has been demonstrated to inhibit epithelial inflammatory cytokine expression, including the chemokine CCL20, [77–79] TLR stimulation and pathogenic bacterial exposure has been demonstrated to promote recruitment of B cells, dendritic cells and T cells through IEC expression of the chemokine CCL20 [74–76]. However, the particular environment at the time of IEC stimulation likely also dictates the cytokine response. In certain settings, a complex intercellular signaling network may be involved in regulation of epithelial cytokine responses, such as in the setting of acute inflammation. There is evidence that even commensal bacterial stimulation can lead to proinflammatory cytokine expression from IECs when there are leukocytes in close proximity which may reflect the need to clear even commensal bacteria when the epithelial barrier has been disrupted in the setting of acute colitis [67].
Conclusions
Epithelial cells are anatomically positioned to serve as a first line of communication between the immune system and the external environment. In this regard, epithelial cells are now appreciated to be a central component of innate immunity. Significant interest in epithelial cells as both a source and a responder to cytokines has revealed that epithelial phenotypes are plastic and moldable, depending on the particular demand of the tissue. Significant evidence is provided that epithelial cells contribute fundamentally to inflammatory resolution and that the dynamic interplay between pathogens and host epithelial cells may best exemplify the prominent role of epithelial cells in orchestration of inflammation.
Acknowledgments
This work was supported by the Veterans Administration and by Grants DK50189, DK095491 and DK104713 from the National Institutes of Health.
Compliance with ethical standards
Conflict of interest
The authors declare no financial interests in any of the work submitted here.
References
- 1.Kagnoff MF. The intestinal epithelium is an integral component of a communications network. J Clin Invest. 2014;124:2841–2843. doi: 10.1172/JCI75225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ivanov AI, Parkos CA, Nusrat A. Cytoskeletal regulation of epithelial barrier function during inflammation. Am J Pathol. 2010;177:512–524. doi: 10.2353/ajpath.2010.100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brandner JM, Schulzke JD. Hereditary barrier-related diseases involving the tight junction: lessons from skin and intestine. Cell Tissue Res. 2015;360:723–748. doi: 10.1007/s00441-014-2096-1. [DOI] [PubMed] [Google Scholar]
- 4.Thiagarajah JR, Verkman AS. Chloride channel-targeted therapy for secretory diarrheas. Curr Opin Pharmacol. 2013;13:888–894. doi: 10.1016/j.coph.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwasaki A, Medzhitov R. Control of adaptive immunity by the innate immune system. Nat Immunol. 2015;16:343–353. doi: 10.1038/ni.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madara JL, Stafford J. Interferon-gamma directly affects barrier function of cultured intestinal epithelial monolayers. J Clin Invest. 1989;83:724–727. doi: 10.1172/JCI113938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quiding M, Nordstrom I, Kilander A, et al. Intestinal immune responses in humans: oral cholera vaccination induces strong intestinal antibody responses and interferon-gamma production and evokes local immunological memory. J Clin Invest. 1991;88:143–148. doi: 10.1172/JCI115270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerf-Bensussan N, Quaroni A, Kurnick JT, et al. Intraepithelial lymphocytes modulate Ia expression by intestinal epithelial cells. J Immunol. 1984;132:2244–2252. [PubMed] [Google Scholar]
- 9.Mayer L, Shlien R. Evidence for function of Ia molecules on gut epithelial cells in man. J Exp Med. 1987;166:1471–1483. doi: 10.1084/jem.166.5.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panja A, Goldberg S, Eckmann L, et al. The regulation and functional consequence of proinflammatory cytokine binding on human intestinal epithelial cells. J Immunol. 1998;161:3675–3684. [PubMed] [Google Scholar]
- 11.Taylor CT, Dzus AL, Colgan SP. Autocrine regulation of intestinal epithelial permeability induced by hypoxia: role for basolateral release of tumor necrosis factor-a (TNF-a) Gastroenterology. 1998;114:657–668. doi: 10.1016/S0016-5085(98)70579-7. [DOI] [PubMed] [Google Scholar]
- 12.Ciacci C, Mahida YR, Dignass A, et al. Functional IL-2 receptors on intestinal epithelial cells. J Clin Invest. 1993;92:527–532. doi: 10.1172/JCI116598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demoulin JB, Renauld JC. Signalling by cytokines interacting with the interleukin-2 receptor gamma chain. Cytokines Cell Mol Ther. 1998;4:243–256. [PubMed] [Google Scholar]
- 14.Zurawski SM, Vega FJ, Huyghe B, et al. Receptors for interleukin-13 and interleukin-4 are complex and share a novel component that functions in signal transduction. EMBO J. 1993;12:2663–2670. doi: 10.1002/j.1460-2075.1993.tb05927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kominsky DJ, Campbell EL, Ehrentraut SF, et al. IFN-gamma-mediated induction of an apical IL-10 receptor on polarized intestinal epithelia. J Immunol. 2014;192:1267–1276. doi: 10.4049/jimmunol.1301757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Commins S, Steinke JW, Borish L. The extended IL-10 superfamily: IL-10, IL-19, IL-20, IL-22, IL-24, IL-26, IL-28, and IL-29. J Allergy Clin Immunol. 2008;121:1108–1111. doi: 10.1016/j.jaci.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 17.Denning TL, Campbell NA, Song F, et al. Expression of IL-10 receptors on epithelial cells from the murine small and large intestine. Int Immunol. 2000;12:133–139. doi: 10.1093/intimm/12.2.133. [DOI] [PubMed] [Google Scholar]
- 18.Colgan SP, Parkos CA, Matthews JB, et al. Interferon-γ induces a surface phenotype switch in intestinal epithelia: downregulation of ion transport and upregulation of immune accessory ligands. Am J Physiol. 1994;267:C402–C410. doi: 10.1152/ajpcell.1994.267.2.C402. [DOI] [PubMed] [Google Scholar]
- 19.Clevers H. The intestinal crypt, a prototype stem cell compartment. Cell. 2013;154:274–284. doi: 10.1016/j.cell.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 21.Spence JR, Mayhew CN, Rankin SA, et al. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro. Nature. 2011;470:105–109. doi: 10.1038/nature09691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sato T, Stange DE, Ferrante M, et al. Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology. 2011;141:1762–1772. doi: 10.1053/j.gastro.2011.07.050. [DOI] [PubMed] [Google Scholar]
- 23.Abraham C, Cho JH. Inflammatory Bowel Disease. N Eng J Med. 2009;361:2066–2076. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mankertz J, Schulzke JD. Altered permeability in inflammatory bowel disease: pathophysiology and clinical implications. Curr Opin Gastroenterol. 2007;23:379–383. doi: 10.1097/MOG.0b013e32816aa392. [DOI] [PubMed] [Google Scholar]
- 25.Koch S, Nusrat A. The life and death of epithelia during inflammation: lessons learned from the gut. Annu Rev Pathol. 2012;7:35–60. doi: 10.1146/annurev-pathol-011811-120905. [DOI] [PubMed] [Google Scholar]
- 26.Mankertz J, Tavalali S, Schmitz H, et al. Expression from the human occludin promoter is affected by tumor necrosis factor alpha and interferon gamma. J Cell Sci. 2000;113:2085–2090. doi: 10.1242/jcs.113.11.2085. [DOI] [PubMed] [Google Scholar]
- 27.Furuse M, Hirase T, Itoh M, et al. Occludin: a novel integral membrane protein localizing at tight junctions. J Cell Biol. 1993;123:1777–1788. doi: 10.1083/jcb.123.6.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nava P, Koch S, Laukoetter MG, et al. Interferon-gamma regulates intestinal epithelial homeostasis through converging beta-catenin signaling pathways. Immunity. 2010;32:392–402. doi: 10.1016/j.immuni.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Sadi RM, Ma TY. IL-1beta causes an increase in intestinal epithelial tight junction permeability. J Immunol. 2007;178:4641–4649. doi: 10.4049/jimmunol.178.7.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zund G, Madara JL, Dzus AL, et al. Interleukin-4 and interleukin-13 differentially regulate epithelial chloride secretion. J Biol Chem. 1996;271:7460–7464. doi: 10.1074/jbc.271.13.7460. [DOI] [PubMed] [Google Scholar]
- 31.Berin MC, Yang P-C, Ciok L, et al. Role of IL-4 in macromolecular transport across human intestinal epithelium. Am J Physiol (Cell Physiol) 1999;276:C1046–C1052. doi: 10.1152/ajpcell.1999.276.5.C1046. [DOI] [PubMed] [Google Scholar]
- 32.Yu LC, Yang PC, Berin MC, et al. Enhanced transepithelial antigen transport in intestine of allergic mice is mediated by IgE/CD23 and regulated by interleukin-4. Gastroenterology. 2001;121:370–381. doi: 10.1053/gast.2001.26470. [DOI] [PubMed] [Google Scholar]
- 33.Al-Sadi R, Ye D, Boivin M, et al. Interleukin-6 modulation of intestinal epithelial tight junction permeability is mediated by JNK pathway activation of claudin-2 gene. PLoS One. 2014;9:e85345. doi: 10.1371/journal.pone.0085345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suzuki T, Yoshinaga N, Tanabe S. Interleukin-6 (IL-6) regulates claudin-2 expression and tight junction permeability in intestinal epithelium. J Biol Chem. 2011;286:31263–31271. doi: 10.1074/jbc.M111.238147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grivennikov S, Karin E, Terzic J, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009;15:103–113. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuhn KA, Manieri NA, Liu TC, et al. IL-6 stimulates intestinal epithelial proliferation and repair after injury. PLoS One. 2014;9:e114195. doi: 10.1371/journal.pone.0114195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Madsen KL, Malfair D, Gray D, et al. Interleukin-10 gene-deficient mice develop a primary intestinal permeability defect in response to enteric microflora. Inflamm Bowel Dis. 1999;5:262–270. doi: 10.1097/00054725-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Colgan SP, Hershberg RM, Furuta GT, et al. Ligation of intestinal epithelial CD1d induces bioactive IL-10: critical role of the cytoplasmic tail in autocrine signaling. Proc Natl Acad Sci USA. 1999;96:13938–13943. doi: 10.1073/pnas.96.24.13938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arrieta MC, Madsen K, Doyle J, et al. Reducing small intestinal permeability attenuates colitis in the IL10 gene-deficient mouse. Gut. 2009;58:41–48. doi: 10.1136/gut.2008.150888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ito S, Ansari P, Sakatsume M, et al. Interleukin-10 inhibits expression of both interferon alpha- and interferon gamma-induced genes by suppressing tyrosine phosphorylation of STAT1. Blood. 1999;93:1456–1463. [PubMed] [Google Scholar]
- 41.Li LJ, Gong C, Zhao MH, et al. Role of interleukin-22 in inflammatory bowel disease. World J Gastroenterol. 2014;20:18177–18188. doi: 10.3748/wjg.v20.i48.18177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liang SC, Tan XY, Luxenberg DP, et al. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J Exp Med. 2006;203:2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Satoh-Takayama N, Vosshenrich CA, Lesjean-Pottier S, et al. Microbial flora drives interleukin 22 production in intestinal NKp46+ cells that provide innate mucosal immune defense. Immunity. 2008;29:958–970. doi: 10.1016/j.immuni.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 44.Takatori H, Kanno Y, Watford WT, et al. Lymphoid tissue inducer-like cells are an innate source of IL-17 and IL-22. J Exp Med. 2009;206:35–41. doi: 10.1084/jem.20072713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cella M, Fuchs A, Vermi W, et al. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature. 2009;457:722–725. doi: 10.1038/nature07537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kotenko SV, Izotova LS, Mirochnitchenko OV, et al. Identification, cloning, and characterization of a novel soluble receptor that binds IL-22 and neutralizes its activity. J Immunol. 2001;166:7096–7103. doi: 10.4049/jimmunol.166.12.7096. [DOI] [PubMed] [Google Scholar]
- 47.Sugimoto K, Ogawa A, Mizoguchi E, et al. IL-22 ameliorates intestinal inflammation in a mouse model of ulcerative colitis. J Clin Invest. 2008;118:534–544. doi: 10.1172/JCI33194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xie MH, Aggarwal S, Ho WH, et al. Interleukin (IL)-22, a novel human cytokine that signals through the interferon receptor-related proteins CRF2-4 and IL-22R. J Biol Chem. 2000;275:31335–31339. doi: 10.1074/jbc.M005304200. [DOI] [PubMed] [Google Scholar]
- 49.Zheng Y, Valdez PA, Danilenko DM, et al. Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat Med. 2008;14:282–289. doi: 10.1038/nm1720. [DOI] [PubMed] [Google Scholar]
- 50.Nagalakshmi ML, Rascle A, Zurawski S, et al. Interleukin-22 activates STAT3 and induces IL-10 by colon epithelial cells. Int Immunopharmacol. 2004;4:679–691. doi: 10.1016/j.intimp.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 51.Sugimoto K. Role of STAT3 in inflammatory bowel disease. World J Gastroenterol. 2008;14:5110–5114. doi: 10.3748/wjg.14.5110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brand S, Beigel F, Olszak T, et al. IL-22 is increased in active Crohn’s disease and promotes proinflammatory gene expression and intestinal epithelial cell migration. Am J Physiol Gastrointest Liver Physiol. 2006;290:G827–G838. doi: 10.1152/ajpgi.00513.2005. [DOI] [PubMed] [Google Scholar]
- 53.Bensancon F, Przewlocki G, Baro I, et al. Interferon-g downregulates CFTR gene expression in epithelial cells. Am J Physiol. 1994;267:C1398–C1404. doi: 10.1152/ajpcell.1994.267.5.C1398. [DOI] [PubMed] [Google Scholar]
- 54.Rocha F, Musch MW, Lishanskiy L, et al. IFN-gamma downregulates expression of Na(+)/H(+) exchangers NHE2 and NHE3 in rat intestine and human Caco-2/bbe cells. Am J Physiol Cell Physiol. 2001;280:C1224–C1232. doi: 10.1152/ajpcell.2001.280.5.C1224. [DOI] [PubMed] [Google Scholar]
- 55.Sugi K, Musch MW, Field M, et al. Inhibition of Na+, K+-ATPase by interferon gamma down-regulates intestinal epithelial transport and barrier function. Gastroenterology. 2001;120:1393–1403. doi: 10.1053/gast.2001.24045. [DOI] [PubMed] [Google Scholar]
- 56.Asfaha S, MacNaughton WK, Appleyard CB, et al. Persistent epithelial dysfunction and bacterial translocation after resolution of intestinal inflammation. Am J Physiol Gastrointest Liver Physiol. 2001;281:G635–G644. doi: 10.1152/ajpgi.2001.281.3.G635. [DOI] [PubMed] [Google Scholar]
- 57.Colgan SP, Resnick MB, Parkos CA, et al. IL-4 directly modulates function of a model human intestinal epithelium. J Immunol. 1994;153:2122–2129. [PubMed] [Google Scholar]
- 58.Ceponis PJ, Botelho F, Richards CD, et al. Interleukins 4 and 13 increase intestinal epithelial permeability by a phosphatidylinositol 3-kinase pathway. Lack of evidence for STAT 6 involvement. J Biol Chem. 2000;275:29132–29137. doi: 10.1074/jbc.M003516200. [DOI] [PubMed] [Google Scholar]
- 59.Gauchat JF, Schlagenhauf E, Feng NP, et al. A novel 4-kb interleukin-13 receptor alpha mRNA expressed in human B, T, and endothelial cells encoding an alternate type-II interleukin- 4/interleukin-13 receptor. Eur J Immunol. 1997;27:971–978. doi: 10.1002/eji.1830270425. [DOI] [PubMed] [Google Scholar]
- 60.Miloux B, Laurent P, Bonnin O, et al. Cloning of the human IL-13R alpha1 chain and reconstitution with the IL4R alpha of a functional IL-4/IL-13 receptor complex. FEBS Lett. 1997;401:163–166. doi: 10.1016/S0014-5793(96)01462-7. [DOI] [PubMed] [Google Scholar]
- 61.Keely SJ, Uribe JM, Barrett KE. Carbachol stimulates transactivation of epidermal growth factor receptor and mitogen-activated protein kinase in T84 cells. Implications for carbachol-stimulated chloride secretion. J Biol Chem. 1998;273:27111–27117. doi: 10.1074/jbc.273.42.27111. [DOI] [PubMed] [Google Scholar]
- 62.Lozupone CA, Stombaugh JI, Gordon JI, et al. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489:220–230. doi: 10.1038/nature11550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marques R, Boneca IG. Expression and functional importance of innate immune receptors by intestinal epithelial cells. Cell Mol Life Sci. 2011;68:3661–3673. doi: 10.1007/s00018-011-0829-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee J, Mo JH, Katakura K, et al. Maintenance of colonic homeostasis by distinctive apical TLR9 signalling in intestinal epithelial cells. Nat Cell Biol. 2006;8:1327–1336. doi: 10.1038/ncb1500. [DOI] [PubMed] [Google Scholar]
- 65.Gewirtz AT, Navas TA, Lyons S, et al. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol. 2001;167:1882–1885. doi: 10.4049/jimmunol.167.4.1882. [DOI] [PubMed] [Google Scholar]
- 66.Lee J, Gonzales-Navajas JM, Raz E. The, “polarizing-tolerizing” mechanism of intestinal epithelium: its relevance to colonic homeostasis. Semin Immunopathol. 2008;30:3–9. doi: 10.1007/s00281-007-0099-7. [DOI] [PubMed] [Google Scholar]
- 67.Haller D, Bode C, Hammes WP, et al. Non-pathogenic bacteria elicit a differential cytokine response by intestinal epithelial cell/leucocyte co-cultures. Gut. 2000;47:79–87. doi: 10.1136/gut.47.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vijay-Kumar M, Sanders CJ, Taylor RT, et al. Deletion of TLR5 results in spontaneous colitis in mice. J Clin Invest. 2007;117:3909–3921. doi: 10.1172/JCI33084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.He B, Xu W, Santini PA, et al. Intestinal bacteria trigger T cell-independent immunoglobulin A(2) class switching by inducing epithelial-cell secretion of the cytokine APRIL. Immunity. 2007;26:812–826. doi: 10.1016/j.immuni.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 70.Rochman Y, Spolski R, Leonard WJ. New insights into the regulation of T cells by gamma(c) family cytokines. Nat Rev Immunol. 2009;9:480–490. doi: 10.1038/nri2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee HC, Ziegler SF. Inducible expression of the proallergic cytokine thymic stromal lymphopoietin in airway epithelial cells is controlled by NFkappaB. Proc Natl Acad Sci USA. 2007;104:914–919. doi: 10.1073/pnas.0607305104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zeuthen LH, Fink LN, Frokiaer H. Epithelial cells prime the immune response to an array of gut-derived commensals towards a tolerogenic phenotype through distinct actions of thymic stromal lymphopoietin and transforming growth factor-beta. Immunology. 2008;123:197–208. doi: 10.1111/j.1365-2567.2007.02687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Taylor BC, Zaph C, Troy AE, et al. TSLP regulates intestinal immunity and inflammation in mouse models of helminth infection and colitis. J Exp Med. 2009;206:655–667. doi: 10.1084/jem.20081499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shang L, Fukata M, Thirunarayanan N, et al. Toll-like receptor signaling in small intestinal epithelium promotes B-cell recruitment and IgA production in lamina propria. Gastroenterology. 2008;135:529–538. doi: 10.1053/j.gastro.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Izadpanah A, Dwinell MB, Eckmann L, et al. Regulated MIP-3alpha/CCL20 production by human intestinal epithelium: mechanism for modulating mucosal immunity. Am J Physiol Gastrointest Liver Physiol. 2001;280:G710–G719. doi: 10.1152/ajpgi.2001.280.4.G710. [DOI] [PubMed] [Google Scholar]
- 76.Sierro F, Dubois B, Coste A, et al. Flagellin stimulation of intestinal epithelial cells triggers CCL20-mediated migration of dendritic cells. Proc Natl Acad Sci USA. 2001;98:13722–13727. doi: 10.1073/pnas.241308598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sibartie S, O’Hara AM, Ryan J, et al. Modulation of pathogen-induced CCL20 secretion from HT-29 human intestinal epithelial cells by commensal bacteria. BMC Immunol. 2009;10:54. doi: 10.1186/1471-2172-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bahrami B, Macfarlane S, Macfarlane GT. Induction of cytokine formation by human intestinal bacteria in gut epithelial cell lines. J Appl Microbiol. 2011;110:353–363. doi: 10.1111/j.1365-2672.2010.04889.x. [DOI] [PubMed] [Google Scholar]
- 79.Neish AS, Gewirtz AT, Zeng H, et al. Prokaryotic regulation of epithelial responses by inhibition of IkappaB-alpha ubiquitination. Science. 2000;289:1560–1563. doi: 10.1126/science.289.5484.1560. [DOI] [PubMed] [Google Scholar]
- 80.Duerr RH, Taylor KD, Brant SR, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science. 2006;314:1461–1463. doi: 10.1126/science.1135245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zaph C, Du Y, Saenz SA, et al. Commensal-dependent expression of IL-25 regulates the IL-23-IL-17 axis in the intestine. J Exp Med. 2008;205:2191–2198. doi: 10.1084/jem.20080720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wedebye Schmidt EG, Larsen HL, Kristensen NN, et al. TH17 cell induction and effects of IL-17A and IL-17F blockade in experimental colitis. Inflamm Bowel Dis. 2013;19:1567–1576. doi: 10.1097/MIB.0b013e318286fa1c. [DOI] [PubMed] [Google Scholar]
- 83.Westendorf AM, Fleissner D, Groebe L, et al. CD4+ Foxp3+ regulatory T cell expansion induced by antigen-driven interaction with intestinal epithelial cells independent of local dendritic cells. Gut. 2009;58:211–219. doi: 10.1136/gut.2008.151720. [DOI] [PubMed] [Google Scholar]
- 84.Hershberg RM, Cho DH, Youakim A, et al. Highly polarized HLA class II antigen processing and presentation by human intestinal epithelial cells. J Clin Invest. 1998;102:792–803. doi: 10.1172/JCI3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hershberg RM, Mayer LF. Antigen processing and presentation by intestinal epithelial cells—polarity and complexity. Immunol Today. 2000;21:123–128. doi: 10.1016/S0167-5699(99)01575-3. [DOI] [PubMed] [Google Scholar]
- 86.Hershberg RM, Framson PE, Cho DH, et al. Intestinal epithelial cells use two distinct pathways for HLA class II antigen processing. J Clin Invest. 1997;100:204–215. doi: 10.1172/JCI119514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Framson PE, Cho DH, Lee LY, et al. Polarized expression and function of the costimulatory molecule CD58 on human intestinal epithelial cells. Gastroenterology. 1999;116:1054–1062. doi: 10.1016/S0016-5085(99)70008-9. [DOI] [PubMed] [Google Scholar]
- 88.Balk SP, Burke S, Polischuk JE, et al. b2-microglobulin-independent MHC class Ib molecule expressed by human intestinal epithelium. Science. 1994;265:259–262. doi: 10.1126/science.7517575. [DOI] [PubMed] [Google Scholar]
- 89.Colgan SP, Morales VM, Madara JL, et al. IFN-g modulates CD1d expression on intestinal epithelia. Am J Physiol. 1996;271:C276–C283. doi: 10.1152/ajpcell.1996.271.1.C276. [DOI] [PubMed] [Google Scholar]
- 90.Zeissig S, Blumberg RS. Commensal microbiota and NKT cells in the control of inflammatory diseases at mucosal surfaces. Curr Opin Immunol. 2013;25:690–696. doi: 10.1016/j.coi.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Elewaut D, Kronenberg M. Molecular biology of NK T cell specificity and development. Semin Immunol. 2000;12:561–568. doi: 10.1006/smim.2000.0275. [DOI] [PubMed] [Google Scholar]
- 92.Olszak T, Neves JF, Dowds CM, et al. Protective mucosal immunity mediated by epithelial CD1d and IL-10. Nature. 2014;509:497–502. doi: 10.1038/nature13150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sumagin R, Parkos CA. Epithelial adhesion molecules and the regulation of intestinal homeostasis during neutrophil transepithelial migration. Tissue Barriers. 2015;3:e969100. doi: 10.4161/21688362.2014.969100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Takeuchi A. Electron microscope studies of experimental Salmonella infection . Am J Pathol. 1967;50:109–119. [PMC free article] [PubMed] [Google Scholar]
- 95.Phalipon A, Sansonetti PJ. Shigella’s ways of manipulating the host intestinal innate and adaptive immune system: a tool box for survival? Immunol Cell Biol. 2007;85:119–129. doi: 10.1038/sj.icb7100025. [DOI] [PubMed] [Google Scholar]
- 96.Jung HC, Eckmann L, Yang SK, et al. A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Invest. 1995;95:55–65. doi: 10.1172/JCI117676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vallee S, Laforest S, Fouchier F, et al. Cytokine-induced upregulation of NF-kappaB, IL-8, and ICAM-1 is dependent on colonic cell polarity: implication for PKCdelta. Exp Cell Res. 2004;297:165–185. doi: 10.1016/j.yexcr.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 98.Olsen I, Hajishengallis G. Major neutrophil functions subverted by Porphyromonas gingivalis . J Oral Microbiol. 2015 doi: 10.3402/jom.v8.30936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Parkos CA, Delp C, Arnaout MA, et al. Neutrophil migration across a cultured intestinal epithelium: dependence on a CD11b/CD18—mediated event and enhanced efficiency in the physiologic direction. J Clin Invest. 1991;88:1605–1612. doi: 10.1172/JCI115473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fan Z, Ley K. Leukocyte arrest: biomechanics and molecular mechanisms of beta2 integrin activation. Biorheology. 2015;52:353–377. doi: 10.3233/BIR-15085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Huang GT, Eckmann L, Savidge TC, et al. Infection of human intestinal epithelial cells with invasive bacteria upregulates apical intercellular adhesion molecule-1 (ICAM)-1) expression and neutrophil adhesion. J Clin Invest. 1996;98:572–583. doi: 10.1172/JCI118825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Parkos CA, Colgan SP, Diamond MS, et al. Expression and polarization of intercellular adhesion molecule-1 on human intestinal epithelia: consequences for CD11b/18-mediated interactions with neutrophils. Mol Med. 1996;2:489–505. [PMC free article] [PubMed] [Google Scholar]
- 103.Colgan SP, Parkos CA, Delp C, et al. Neutrophil migration across cultured intestinal epithelial monolayers is modulated by epithelial exposure to interferon-gamma in a highly polarized fashion. J Cell Biol. 1993;120:785–795. doi: 10.1083/jcb.120.3.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Parkos CA, Colgan SP, Liang A, et al. CD 47 mediates post-adhesive events required for neutrophil migration across polarized intestinal epithelia. J Cell Biol. 1996;132:437–450. doi: 10.1083/jcb.132.3.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Murata Y, Kotani T, Ohnishi H, et al. The CD47-SIRPalpha signalling system: its physiological roles and therapeutic application. J Biochem. 2014;155:335–344. doi: 10.1093/jb/mvu017. [DOI] [PubMed] [Google Scholar]