Abstract
Affective lability, or the instability of emotional states, is associated with heightened levels of trauma-related emotional responding and posttraumatic stress disorder (PTSD) symptoms. However, the impact of affective lability, specifically on habituation to idiographic trauma cues, has yet to be examined among trauma-exposed individuals. The current study examined differential response trajectories to trauma-related imaginal exposure as a function of affective lability. Specifically, 72 women with a history of sexual victimization participated in a laboratory-based study involving a single session of repeated imaginal exposures to idiographic traumatic event cues. As hypothesized, participants higher in affective lability reported less reduction in trauma-cue elicited posttraumatic stress symptoms across exposure trials. Given these results, it will be important to continue to extend these laboratory findings to better understand how elevated affective lability is related to response to trauma-focused exposure therapy among individuals with PTSD or other trauma-related psychopathology (e.g., borderline personality disorder).
Keywords: PTSD, affective lability, exposure, trauma, habituation
Exposure to a Diagnostic and Statistical Manual – Fourth Edition (DSM-IV)-defined traumatic event (American Psychological Association [APA], 1994) has been associated with an increase in emotional and physiological responding in the presence of trauma cues, even for those who do not meet full criteria for posttraumatic stress disorder (PTSD; Badour et al., 2011; Badour & Feldner, 2013; McDonagh-Coyle et al., 2001; Orr et al., 1998). Indeed, posttraumatic stress symptom (PTSS) level has been associated with emotion regulation difficulties in response to increased emotional or physiological responding (Badour & Feldner, 2013; Tull, Barett, McMillan, & Roemer, 2007). PTSS severity has also been associated with affect lability among a sample of individuals with borderline personality disorder who had experienced a traumatic event (Marshall-Berenz, Morrison, Schumacher, & Coffey, 2011). It is possible that these difficulties in emotion regulation and increased affect lability among individuals with PTSS may result in an interpretation of heightened emotional experiences as uncontrollable and unpredictable (Bouton, Mineka, & Barlow, 2001), and may lead to the avoidance of trauma cues that elicit emotional responding, thus maintaining PTSS and preventing exposure to trauma cues (Foa & Kozak, 1986; Tull et al., 2007).
Emotion processing theory posits that fear networks are formed following exposure to a traumatic event. These networks are comprised of information about, behavioral responses to, and interpretations of the meaning of the feared stimulus (Foa & Kozak, 1986). Importantly, following a trauma, this fear structure contains information that implies both danger and a need to escape from or avoid danger, and it is resistant to modification (Foa & Kozak, 1986). Exposure to trauma cues in a safe and planned manner allows for new information to be introduced into the fear network (Foa, Hembree, & Rothbaum, 2007), allowing individuals to experience information that is inconsistent with the maladaptive information included in the trauma-related fear network. Over time, this newly incorporated information results in a change or a reduction of the emotional response to the feared stimulus (Rauch & Foa, 2006). As emotion processing theory highlights the need to both activate and modify the fear network, it is possible that instability in emotional states may impact the success of exposure therapy among those with trauma exposure, including those with PTSD, as the rapid fluctuation between emotional states may not allow for sufficient engagement of the fear network during exposure. Indeed, Rauch and Foa (2006) highlight that both under-activation and over-activation of the fear structure can hinder the efficacy of exposure therapy for PTSD.
Ample research suggests that people experiencing elevated levels of PTSS evidence greater emotional reactivity in response to the presentation of a traumatic event cue (Badour et al., 2011; Lanius et al., 2003; Liberzon et al., 1999; Orr, Pitman, Lasko, & Herz, 1993; Orr & Roth, 2000; Pitman et al., 1990; Wolfe et al., 2000). Affect lability and emotion regulation are thought of as two separate processes within the emotion system, both of which are important as they have been linked with maladaptive outcomes, including internalizing symptoms (Kim-Spoon et al., 2013). Indeed, Kim-Spoon and colleagues (2013) found emotion regulation to be a mediator between emotion lability-negativity and internalizing symptomatology among children, with those higher in emotion lability evidencing a decrease in emotion regulation skills in the following year. The authors hypothesize that emotion lability-negativity may serve as a vulnerability factor that may negatively impact the development or use of emotion regulation strategies, and therefore lead to problematic symptomatology (Kim-Spoon et al., 2013). There remains a need to more clearly isolate the components of this emotion response and regulation system as it relates to the presentation of trauma cues.
Affective lability has been linked to a variety of forms of psychopathology, including PTSD and borderline personality disorder (BPD), where trauma exposure is common (Koenigsberg, 2010; Marshall-Berenz, Morrison, Schumacher, & Coffey, 2011; Scheiderer, Wang, Tomko, Wood, & Trull, 2015). However, PTSD and BPD are highly comorbid disorders (Grant et al., 2008; Pagura et al., 2010), and recent research suggests that affective lability is also associated with heightened levels of PTSS (Carlson & Dalenberg, 2000). Indeed, among individuals with BPD who have experienced a traumatic event (meeting Criterion A for a traumatic event; American Psychiatric Association [APA], 1994), PTSS severity, but not BPD symptom severity, predicted affective lability (Marshall-Berenz et al., 2011). Similarly, Scheiderer and colleagues (2016) found that individuals diagnosed with both PTSD and BPD reported significantly greater negative affective instability (i.e., fear and sadness) than those diagnosed with only BPD, highlighting the potentially important impact of BPD and PTSD comorbidity on certain emotion regulation difficulties. Importantly, traumatic event exposure has been linked to emotion regulation difficulties even in the absence of PTSD or BPD (New et al., 2009). Indeed, Kashdan, Uswatte, Steger, and Julian (2006) found that Veterans with PTSD, compared to Veterans without a diagnosis of PTSD, reported greater fluctuations in affect, as well as self-esteem.
Research has only recently begun to explore the relation between affective lability and emotional reactivity to trauma-related cues, and no research has examined affective lability in the context of habituation to repeated presentations of idiographic trauma cues among individuals with trauma exposure. Accordingly, the current study provides an initial examination of how affective lability relates to affective responding in a laboratory model of trauma-focused imaginal exposure among sexually assaulted women. Specifically, it was hypothesized that greater affective lability would be associated with less PTSD symptom reduction across one session of repeated imaginal exposures.
2. Method
2.1 Participants
Participants for the present study were 72 community-recruited adult women (Mage = 31.15, SD = 13.17) who participated in a larger investigation examining specific emotional responses to sexual assault (Badour & Feldner, 2016). All participants endorsed an index trauma involving sexual victimization that satisfied the definition of a traumatic event as specified in Criterion A of the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition, Text Revision (DSM–IV–TR; APA, 2000) definition of PTSD. Participants endorsed one or more of the following acts: exposing of sexual organs (22.2%), touching/fondling of sexual organs (50.0%), vaginal intercourse (36.1%), oral intercourse (19.5%), anal intercourse (4.2%), and other sexual acts (8.3%). Participants’ relationship to the assailant included relative (38.9%), intimate partner/spouse (8.3%), date (6.9%), acquaintance (11.1%), friend (9.7%), stranger (12.5%), and other (12.5%). Sixty-one individuals (84.7%) reported a history of multiple sexual trauma experiences. The majority of participants (69.4%) reported that their index assault occurred prior to age 18 (Mage of assault = 14.00 years, SD = 9.20).
2.2 Measures
2.2.1 Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995)
The CAPS is a 30-item semi-structured interview designed to assess the frequency and severity of past-month posttraumatic stress symptoms, including 17 symptoms based on DSM-IV PTSD criteria (APA, 1994). The CAPS also allows for a determination of past-month PTSD diagnosis. Respondents rate the frequency and intensity of symptoms on separate 5-point scales. The CAPS has demonstrated excellent psychometric properties, with strong inter-rater reliability (Blake et al., 1990), test-retest reliability (Weathers et al., 1991, 1992), and convergent validity with other measures of PTSD (Keane, Caddell, & Taylor, 1988). As such, it is considered the gold standard in PTSD assessment (Weathers, Keane, & Davidson, 2001). The CAPS was used in the present study to record details about traumatic event exposure (e.g., most distressing event, time since exposure), severity of past-month posttraumatic stress symptoms, and past-month diagnosis of PTSD. The Frequency ≥1/Intensity ≥ 2 scoring rule described by Blake and colleagues (1990) as well as Weathers, Ruscio, and Keane (1999) was used to calculate PTSD. Using this rule, each symptom is considered present when a score of at least 1 is given for frequency and at least 2 for intensity. Participants must meet this criterion for at least one re-experiencing, three avoidance-numbing, and two hyperarousal symptoms. Symptoms need to have persisted for at least one month, and participants must endorse at least moderate distress or interference associated with these symptoms to receive a PTSD diagnosis.
2.2.2 Responses to Script-Driven Imagery Scale (RSDI; Hopper et al., 2007)
The RSDI measures symptomatic responses to a script-driven imagery procedure. This measure is comprised of 11 items (e.g., Did you feel as though the event was reoccurring, like you were reliving it? Were you distressed? Did you avoid experiencing images, sounds, or smells connected to the event?) and 3 subscales: Re-experiencing, Avoidance, and Dissociation. Respondents rate the degree to which they experienced each symptom on a 7-point scale from 0 (Not at all) to 6 (A great deal). The RSDI has good psychometric properties, with the subscales demonstrating strong internal consistencies (α = .76 to .91) as well as strong convergent and discriminant validity, as compared to physiological and self-report measures of re-experiencing (e.g., CAPS Re-experiencing subscale), avoidance (e.g., CAPS Effortful Avoidance subscale), and dissociation (e.g., Dissociative Experiences Scale; Hopper et al., 2007). The RSDI demonstrates strong test-retest reliability over a one-week interval, and change in RSDI ratings assessed weekly during treatment are correlated with pre-post change in PTSD symptoms as assessed by established measures (Sack, Hofmann, Wizelman, & Lempa, 2008). In the present study, participants completed the RSDI after each script presentation, and scores from each of the three subscales were summed to create a total symptom score for each exposure trial.
2.2.3 Affect Lability Scale-18 (ALS-18; Oliver & Simons, 2004)
The ALS-18 is an 18-item questionnaire, adapted from the original 54-item version, which assesses one's tendency to shift rapidly from a neutral to an affective state, as well as between different affective states (e.g., One minute I can be feeling OK and then the next minute I'm tense, jittery, and nervous; I frequently switch from being able to control my temper very well to not being able to control it very well at all). Participants rate their propensity to rapidly change between normal mood and four affective domains (i.e., anger, depression, elation, anxiety) as well as the tendency to shift between depression and elation and depression and anxiety. The items are categorized into six subscales, with each subscale based on a shift (e.g., euthymia to anger), and each item is rated on a 4-point Likert scale from 0 (Very uncharacteristic of me) to 3 (Very characteristic of me). Items are intended to capture both subjective and physiological experiences, as well as behaviors. The ALS-18 has demonstrated strong internal consistency (α = .87) and construct validity with individuals diagnosed with cluster B personality disorders reporting higher levels of affective lability than those with cluster A or C personality disorders (Look et al., 2010). The ALS-18 total score, used in the present study, has demonstrated strong internal consistency and correlates with the total score of the full measure (Oliver & Simons, 2004). It has demonstrated good psychometric properties in both clinical and non-clinical samples (Aas et al., 2015; Look et al., 2010).
2.3 Procedure
All procedures were first approved by the University of Arkansas Institutional Review Board. Participants were recruited from throughout the Northwest Arkansas community by way of paper and electronic flyers. After an initial phone screening, potentially eligible participants were invited to the laboratory to complete the experimental procedure (pending final eligibility). Participants were eligible to participate in the study if they reported an index trauma involving sexual victimization that satisfied the definition of a traumatic event as specified in Criterion A of the DSM-IV definition of PTSD and reported experiencing significant emotions of fear and disgust during their most distressing sexual trauma (as rated by a score of at least a 50 on a 0 [not at all afraid/disgusted] to 100 [extremely afraid/disgusted] scale during an initial screening). Participants were excluded from the study for current suicidal intent, unmanaged psychotic symptoms, experiencing a traumatic event within one month of the study, or having no or very limited memory of their index sexual assault due to factors such as acute intoxication or loss of consciousness during the assault, or due to the assault having occurred at a very young age. To prevent participant burden, participants were given the option to complete several questionnaires online (including the ALS-18) prior to their scheduled laboratory visit. Upon arrival to the lab, participants provided written informed consent and then completed the CAPS interview and several other questionnaires not relevant to the present study. Participants found ineligible after the lab screening received $10 in compensation and were debriefed.
2.3.1 Imagery development
All participants first underwent 15 minutes of imagery response training, a protocol adapted from Lang, Levin, Miller, and Kozak (1983), designed to train participants to focus on their responses during the script presentations. This training was conducted with standardized imagery scenes and cued the participant to focus on their active responses (e.g., Did your breathing or heart rate change?).
Participants then generated written narratives of one idiographic neutral experience and the index sexual trauma identified during the CAPS interview. Consistent with previous studies utilizing the script-driven imagery procedure (Pitman, Orr, Forgue, de Jong, & Claiborn, 1987), participants were instructed to include any sensory information, thoughts, feelings, and/or conversations that occurred and were given a checklist of physiological and behavioral responses and were asked to identify the degree to which they experienced any of the listed physiological sensations and wanted to (or did) engage in any of the listed behaviors during the event.
From the content included in written narratives, the experimenter then generated four audio-recorded scripts (two neutral, two trauma). As described in detail previously (Badour & Feldner, 2016), two separate trauma scripts were created in an attempt to manipulate the physiological and behavioral content within the scripts in order to repeatedly present two distinct scripts to all participants focusing on eliciting greater trauma-related disgust (Phase I) followed by greater trauma-related anxiety (Phase II; or vice versa). However, both trauma script types elicited similarly high levels of self-reported disgust and anxiety (Badour & Feldner, 2016). Script type was also unrelated to the outcomes in the present investigation; thus, both script types were combined together to constitute a general trauma-related content.
2.3.2 Imagery exposure procedure
For purposes of the larger study from which these data were drawn (Badour & Feldner, 2016), dose of trials involving traumatic versus neutral content was systematically varied across the 10 exposure trials in order to examine possible dose effects of repeated imagery exposure. The trials were delivered in two phases: Phase I (Trials 1-1, 1-2, 1-3, 1-4, 1-5) and Phase II (Trials 2-1, 2-2, 2-3, 2-4, 2-5). Half of the participants were assigned to the experimental condition where they received a total of 8 trauma-focused trials (Trials 1-1, 1-2, 1-4, 1-5; 2-1, 2-2, 2-4, 2-5) and 2 neutral trials (Trials 1-3, 2-3). The remaining participants were assigned to a control condition, where they received half the dose of trauma-focused trials (Trials 1-1, 1-5, 2-1, 2-5), with the remaining 6 trials involving neutral content. The total number of trials was standardized to keep the length and number of trials consistent across condition. No dose effects were found in the primary study. Given the focus of the present investigation, only responding to trauma-focused trials (c.f. neutral trials) was examined in the present study.
Each exposure phase included 30-min of exposure (5-min baseline where participants were asked to sit quietly and relax in preparation for the exposure procedure, plus 5, 5-min exposure trials). Based on published script-driven imagery procedures (e.g., Orr et al., 1998; Pitman et al., 1987), each exposure trial consisted of six sections: 1) 1-min pre-script VAS ratings; 2) 30-sec baseline period; 3) 30-sec script presentation; 4) 30-sec imaginal rehearsal (participants were asked to sit quietly and continue to imagine the script just heard); 5) 30-sec recovery; and 6) 2-min inter-trial-interval where participants completed post-script VAS and RSDI ratings. Phase II was identical to Phase I with the exception of script content.
2.3.3 Debriefing and compensation
After participating in the final phase, participants were debriefed, given referrals to local health care providers, informed about common reactions to traumatic events, and compensated $40. There were no adverse reactions reported.
2.4 Data Analytic Approach
Linear mixed models with maximum-likelihood estimation (MLE) were used for hypothesis testing. Unstructured covariance matrices were employed in all models. Consistent with the approach outlined by Badour and Feldner (2016), time was modeled as follows: Trial 1-1 (0), Trial 1-2 (1), Trial 1-4 (3), Trial 1-5 (4), Trial 2-1 (5), Trial 2-2 (6), Trial 2-4 (8), Trial 2-5 (9). Trial 1-1 was coded as 0 to allow for interpretation of the intercept as an index of responding to the initial presentation of sexual trauma cues. Data for Trials 1-3 and 2-3 were not included in any models, as these trials involved presentation of neutral content for all participants. For Trials 1-2, 1-4, 2-2, and 2-4, data were only analyzed for participants in the experimental condition. A follow up analysis was conducted to ensure that the pattern of results remained consistent when accounting for the potential dose effect associated with the experimental versus control condition. Post-hoc probing of significant interactions was conducted in accordance with the recommendations of Holmbeck (2002).
3. Results
Demographic data for the sample are presented in Table 1. Eighteen percent of the sample met criteria for past-month PTSD on the CAPS (n = 13). Mean PTSD symptom severity on the CAPS was 32.52 (SD = 20.28; Range = 5 – 91). Mean ALS-18 scores were significantly higher among participants with PTSD (M = 35.00, SD = 10.45) as compared to those without PTSD (M = 16.32, SD = 11.28; t = −5.47, p < .001). To test the primary hypotheses, data were first submitted to an unconditional random intercept and slope model. Mean RSDI scores following the first exposure trial were significantly greater than zero (B0 = 33.92, t = 23.61, p < .001), and symptom ratings decreased significantly across exposure trials (B = −0.59, t = −3.5, p = .001).
Table 1.
Sample Demographic Information.
| Mean or n | SD or % | Range | |
|---|---|---|---|
| Age (years) | 31.15 | 13.17 | 18 – 59 |
| Race | -- | ||
| Caucasian | 57 | 79.2% | |
| African American | 7 | 9.7% | |
| Asian | 3 | 4.2% | |
| Bi-racial/Multi-racial | 3 | 4.2% | |
| Other | 2 | 2.8% | |
| Hispanic ethnicity | 5 | 6.9% | -- |
| Education | -- | ||
| High school or equivalent | 41 | 56.9% | |
| Some college | 8 | 11.1% | |
| Completed 2- or 4-year college | 7 | 9.7% | |
| Some graduate/professional school | 9 | 12.5% | |
| Completed graduate/professional school | 7 | 9.7% | |
| Annual Income (in dollars) | 20,681 | 22,630 | 0 – 119,000 |
Note. N = 72
There was a significant main effect of past-month CAPS scores in predicting RSDI ratings following trial 1-1 (B = .26, t = 3.83, p < .001), such that CAPS scores significantly positively correlated with RSDI ratings following the initial presentation of trauma cues. In contrast, the CAPS by trial interaction was not significant (B = .01, t = 1.17, p = .25), suggesting that past-month CAPS scores were not significantly related to change in RSDI scores across exposure trials.
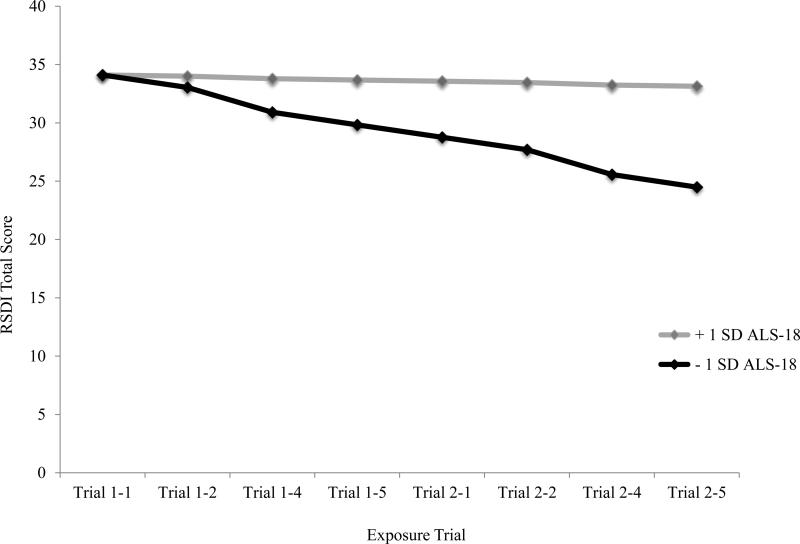
To test the primary hypothesis, ALS-18 scores and the ALS-18 by trial interaction were entered into the model while accounting for variance associated with CAPS scores. ALS-18 scores were not significantly related to RSDI scores following the initial presentation of trauma cues (B = .02, t = .17, p = .87). However, the interaction of ALS-18 scores by trial was significant (B = .03, t = 2.30, p = .03). Post-hoc probing of the interaction demonstrated that RSDI scores declined significantly across exposure trials for participants scoring relatively lower on the ALS-18 (B = −.97, t = −4.17, p < .001); however, RSDI did not decline significantly among participants scoring relatively higher on the ALS-18 (B = −.21, t = −.88, p = .38). This interaction is displayed graphically in Figure 1. This pattern of results did not change when dose (experimental vs. control) and the dose by trial interaction were added as covariates into the model.
Figure 1.
Growth model predicting change in script-elicited PTSD symptoms as a function of affective lability.
4. Discussion
Given the negative outcomes associated with PTSD and the significant portion of people who either drop out of treatment or do not experience a resolution of symptoms (Schottenbauer et al., 2008), it is important to better understand potential mechanisms that may benefit from targeted treatment prior to engaging in exposure therapy. Conducting controlled, laboratory-based research to understand such mechanisms is a critical aspect of treatment development research (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014). Given that affective lability has been associated with increased levels of PTSD (Carlson & Dalenberg, 2000), but had yet to be examined in the context of such controlled research, the current laboratory-based study conducted an initial test of how affective lability relates to affective responding to exposure-based techniques.
Past month CAPS score significantly predicted responses to the first trauma script presentation. This is consistent with research linking elevated levels of PTSD symptoms to greater emotional reactivity to trauma cue exposure (Badour et al., 2011; Orr & Roth, 2000; Orr et al., 1993; Pitman et al., 1990). Results also suggested that symptomatic responding to the script procedure decreased across repeated exposure trials. This pattern is consistent with models of fear habituation in that we would expect those with relatively elevated levels of PTSS to initially evidence greater emotional responding, followed by a reduction in these responses across repeated exposures to the feared stimulus. Interestingly, past month CAPS scores were not predictive of the degree to which symptomatic responding decreased across exposure trials. Taken together, these results suggest that this type of exposure paradigm may be a valuable model for further evaluating predictors and consequences of exposure techniques. Additional evaluation of the convergent and divergent validity as well as the predictive utility of this laboratory model will continue to inform use of the method in the future.
Results were consistent with the hypothesis that people with relatively elevated affective lability would evidence decreased habituation of responding to idiographic trauma cues. One possible explanation for these findings in the context of emotion processing theory is that those reporting higher affective lability may be unable to activate the fear network and allow the network to remain activated for a long enough period of time to incorporate new information and habituate to the feared stimulus. Alternatively, it is possible that high affective lability may interact with either a lack of emotion regulation strategies or poor regulation strategies, resulting in an elevated state of reactivity when exposed to trauma-related cues in the laboratory rather than habituating to the cues, therefore potentially requiring additional exposure trials to habituate to the trauma cues. Future research is now positioned to evaluate this more refined question by monitoring and evaluating indirect effects of state affect and use of regulation strategies during exposure trials in the relation between affective lability and exposure outcomes.
This study addresses an important gap in the literature by providing a controlled laboratory-based study of how individual differences in affective lability relate to responses to repeated trauma-focused exposure trials over time. The use of the script-driven imagery procedure (Orr et al., 1990) in this study allowed for a controlled presentation of idiographic traumatic event cues, as well as real time assessment of cue-elicited posttraumatic stress symptoms following cue presentation. However, the fact that this study was conducted as a single session in the laboratory with a sample that included both clinical and subclinical levels of posttraumatic stress symptoms limits generalizability of the results to treatment settings. It is plausible to hypothesize that these findings would replicate in a treatment study, given Cloitre and colleagues (2002, 2010) work demonstrating positive effects of providing affect regulation training to individuals prior to exposure therapy. The generalizability of this study is also limited by the sample being comprised exclusively of women who have experienced a sexual assault. Given that PTSD symptom severity varied in this sample, with a portion of the sample meeting criteria for PTSD, it will be important to examine whether these results replicate among a sample of participants with current PTSD. Moreover, BPD, a disorder commonly associated with emotion regulation difficulties and trauma exposure, was not formally assessed during this study. Future research in this area will benefit from broadening the sample to include both sexes and different trauma types, as well as conducting a more comprehensive interview battery that includes an assessment of personality disorders. Finally, the measurement of trauma exposure and PTSS was assessed using DSM-IV criteria, and the affective lability and response to traumatic event cue presentation were both self-report measures. As such, future research should examine these phenomena with the new DSM 5 criteria among those who meet criteria for PTSD and begin to address the issue of self-report measures by supplementing these measures with additional assessment methods (e.g., behavioral observation of trauma-cue elicited affective reactions, physiological responding, ecological momentary assessment). Using assessment tools like physiological responding in the laboratory or ecological momentary assessment would allow for both a more thorough analysis of trauma-related emotional responding and reduce reliance on retrospective reporting of general affect patterns; nevertheless, other areas of study have demonstrated that while state measures provide additional, rich information, self-report data on affective lability are also able to significantly predict the outcome of interest (Anestis et al., 2010).
These limitations notwithstanding, the current study significantly contributes to the extant literature examining mechanisms that may impact exposure treatment for PTSD. Indeed, these findings suggest that individuals who endorse relatively elevated affective lability may benefit from interventions designed to address these difficulties prior to engaging in exposure therapy for PTSD. Additional laboratory-based research is now needed to both replicate these findings and extend this research to better understand the influence of affective lability on habituation during repeated traumatic event cue presentation among individuals with PTSD. Indeed, this study allows for more specific hypothesis testing in the future, including how affective lability may relate to responses of specific posttraumatic stress symptom clusters. Existing treatment-oriented research with individuals who are diagnosed with BPD and PTSD (Harned, Korslund, Foa, & Linehan, 2012; Harned, Korslund, Linehan, 2013; Harned & Linehan, 2008), as well as research looking at exposure therapy in high-risk individuals (Cloitre et al., 2010), has demonstrated that the combination of treatment targeting skills, including emotion regulation and distress tolerance prior to exposure therapy, can be effective with these populations. Future research may benefit from examining how changes in affective lability across treatment impacts habituation and treatment engagement during exposure therapy for PTSD.
Highlights.
Affective lability is associated with increased levels of PTSD symptoms, but its impact on habituation to idiographic trauma cues has not been examined.
The impact of affective lability was examined during a single laboratory-based session of imaginal exposure to idiographic trauma cues.
Higher levels of affective lability were associated with less reduction in PTSS across exposure trials.
Acknowledgments
This research was supported by a National Research Service Award (F31 MH092994) from the National Institute of Mental Health (NIMH) awarded to Dr. Badour. The expressed views do not necessarily represent those of NIMH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aas M, Pederson G, Henry C, Bjella T, Bellivier F, Leboyer M, Kahn J, Etain B. Psychometric properties of the Affective Lability Scale (54 and 18-item version) in patients with bipolar disorder, first-degree relatives, and healthy controls. Journal of Affective Disorders. 2015;172:375–380. doi: 10.1016/j.jad.2014.10.028. doi: 10.1016/j.jad.2014.10.028. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Author; Washington, DC: 2000. [Google Scholar]
- Anestis MD, Selby EA, Crosby RD, Wonderlich SA, Engel SG, Joiner TE. A comparison of retrospective self-report versus ecological momentary assessment measures of affective lability in the examination of its relationship with bulimic symptomatology. Behaviour Research and Therapy. 2010;48:607–613. doi: 10.1016/j.brat.2010.03.012. doi: 10.1016/j.brat.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badour CL, Feldner M. Trauma-related reactivity and regulation of emotion: Associations with posttraumatic stress symptoms. Journal of Behavior Therapy and Experimental Psychiatry. 2013;44:69–76. doi: 10.1016/j.jbtep.2012.07.007. doi: 10.1016/j.jbtep.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badour CL, Feldner M. Disgust and imaginal exposure to memories of sexual trauma: Implications for the treatment of posttraumatic stress. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8:267–275. doi: 10.1037/tra0000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badour CL, Feldner MT, Babson KA, Smith RC, Blumenthal H, Trainor CD, Olantunji BO. Differential emotional responding to ideographic cues of traumatic interpersonal violence compared to non-interpersonal traumatic experiences. Journal of Experimental Psychology. 2011;2:400–417. doi: 10.5127/jep.014711. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;13:187–188. [Google Scholar]
- Blake DD, Weather FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi:10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037/0033-295x.108.1.4. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Dalenberg CJ. A conceptual framework for the impact of traumatic experiences. Trauma, Violence, & Abuse. 2000;1:4–28. doi: 10.1177/1524838000001001002. [Google Scholar]
- Cloitre M, Koenen K, Cohen L, Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70:1067–1074. doi: 10.1037//0022-006x.70.5.1067. doi: 10.1037//0022-006X.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough C, Nooner K, Zorbas P, Cherry S, Jackson C, Petkova E. Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry. 2010;167:915–924. doi: 10.1176/appi.ajp.2010.09081247. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree E, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide (treatments that work) Oxford University Press; New York: 2007. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear. Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from wave 2 National Epidemiological Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. doi: 10.4088/JCP.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned M, Korslund K, Foa E, Linehan M. Treating PTSD in suicidal and self-injuring women with borderline personality disorder: Development and preliminary evaluation of a Dialectical Behavior Therapy Prolonged Exposure Protocol. Behaviour Research and Therapy. 2012;50:381–386. doi: 10.1016/j.brat.2012.02.011. doi: 10.1016/j.brat.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned M, Korslund K, Linehan M. A pilot randomization controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. doi: 10.1016/j.brat.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned MS, Linehan MM. Integrating Dialectical Behavior Therapy and Prolonged Exposure to treat co-occurring borderline personality disorder and PTSD: Two case studies. Cognitive and Behavioral Practice. 2008;15(3):263–276. [Google Scholar]
- Holmbeck G. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Frewen PA, Sack M, Lanius RA, Van der Kolk BA. The Responses to Script-Driven Imagery Scale (RSDI): assessment of state posttraumatic symptoms for psychobiological and treatment research. Journal of Psychopathology and Behavioral Assessment. 2007;29(4):249–268. doi: 10.1007/s10862-007-9046-0. [Google Scholar]
- Kashdan TB, Uswatte G, Steger MF, Julian T. Fragile self-esteem and affective instability in posttraumatic stress disorder. Behaviour Research and Therapy. 2006;44:1609–1619. doi: 10.1016/j.brat.2005.12.003. doi: 10.1016/j.brat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Kim-Spoon J, Cicchetti D, Rogosch F. A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development. 2013;84:512–527. doi: 10.1111/j.1467-8624.2012.01857.x. doi:10.1111/j.1467-8624.2012.01857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenigsberg HW. Affective instability: Toward an integration of neuroscience and psychological perspectives. Journal of Personality Disorders. 2010;24:60–82. doi: 10.1521/pedi.2010.24.1.60. doi: 10.1521/pedi.2010.24.1.60. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Levin DN, Miller GA, Kozak MJ. Fear behavior, fear imagery, and the psychophysiology of emotion: the problem of affective response integration. Journal of Abnormal Psychology. 1983;92(3):276–306. doi: 10.1037//0021-843x.92.3.276. doi: 10.1037/0021-843X.92.3.276. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Williamson PC, Hopper J, Densmore M, Boksman K, Gupta MA, Menon RS. Recall of emotional states in posttraumatic stress disorder: an fMRI investigation. Biological Psychiatry. 2003;53:204–210. doi: 10.1016/s0006-3223(02)01466-x. doi: 10.1016/S0006-3223(02)01466-X. [DOI] [PubMed] [Google Scholar]
- Liberzon I, Taylor SF, Amdur R, Jung TD, Chamberain KR, Minoshima S, Fig LM. Brain activation in PTSD in response to trauma-related stimuli. Biological Psychiatry. 1999;45:817–826. doi: 10.1016/s0006-3223(98)00246-7. doi: 10.1016/S0006-3223(98)00246-7. [DOI] [PubMed] [Google Scholar]
- Look AE, Flory JD, Harvey PD, Siever LJ. Psychometric properties of a short form of the Affective Lability Scale (ALS-18). Personality and Individual Differences. 2010;49(3):187–191. doi: 10.1016/j.paid.2010.03.030. doi:10.1016/j.paid.2010.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Morrison JA, Schumacher JA, Coffey SF. Affect intensity and lability: The role of posttraumatic stress disorder symptoms in boderline personality disorder. Depression and Anxiety. 2011;28:393–399. doi: 10.1002/da.20798. doi: 10.1002/da.20798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonagh-Coyle A, McHugo G, Friedman M, Schnurr P, Zayfert C, Descamps M. Psychophysiological reactivity in female sexual abuse survivors. Journal of Traumatic Stress. 2001;14:667–683. doi: 10.1023/A:1013081803429. doi: 10.1023/A:1013081803429. [DOI] [PubMed] [Google Scholar]
- New A, Fan J, Murrough J, Liu X, Liebman R, Guise K, Charney D. A functional magnetic resonance imaging study of deliberate emotion regulation in resilience and posttraumatic stress disorder. Biological Psychiatry. 2009;66:656–664. doi: 10.1016/j.biopsych.2009.05.020. doi: 10.1016/j.biopsych.2009.06.020. [DOI] [PubMed] [Google Scholar]
- Oliver MNI, Simons JS. The affective lability scales: Development of a short-form measure. Personality and Individual Differences. 2004;37:1279–1288. doi: 10.1016/j.paid.2003.12.013. [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science. 2014;2:22–34. doi: 10.1177/2167702613497932. doi:10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr SP, Claiborn JM, Altman B, Forgue DF, de Jong JB, Pitman RK, Herz LR. Psychometric profile of posttraumatic stress disorder, anxious, and healthy Vietnam veterans: correlations with psychophysiologic responses. Journal of Consulting and Clinical Psychology. 1990;58:329–335. doi: 10.1037//0022-006x.58.3.329. doi: 10.1037/0022-006X.58.3.329. [DOI] [PubMed] [Google Scholar]
- Orr SP, Lasko NB, Metzger LJ, Berry NJ, Ahern CE, Pitman RK. Psychophysiologic assessment of women with posttraumatic stress disorder resulting from childhood sexual abuse. Journal of Consulting and Clinical Psychology. 1998;66(6):906–913. doi: 10.1037//0022-006x.66.6.906. doi:10.1037/0022-006X.66.6.906. [DOI] [PubMed] [Google Scholar]
- Orr SP, Pitman RK, Lasko NB, Herz LR. Psychophysiological assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. Journal of Abnormal Psychology. 1993;102:152–159. doi: 10.1037//0021-843x.102.1.152. doi: 10.1037/0021-843X.102.152. [DOI] [PubMed] [Google Scholar]
- Orr SP, Roth WT. Psychophysiological assessment: clinical applications for PTSD. Journal for Affective Disorders. 2000;61:225–240. doi: 10.1016/s0165-0327(00)00340-2. doi: 10.1016/S0165-0327(00)00340-2. [DOI] [PubMed] [Google Scholar]
- Pagura J, Stein MB, Bolton JM, Cox BJ, Grant B, Sareen J. Comorbidity of personality disorder and posttraumatic stress disorder in the U. S. population. Journal of Psychiatric Research. 2010;44:1190–1198. doi: 10.1016/j.jpsychires.2010.04.016. doi: 10.1016/j.jpsychires.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, Altman B, Je Jong JB, Herz LR. Psychophysiologic responses to combat imagery of Vietnam veterans with posttraumatic stress disorder versus other anxiety disorders. Journal of Abnormal Psychology. 1990;99:49–54. doi: 10.1037//0021-843x.99.1.49. doi:10.1037/0021-843X.99.1.49. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Archives of General Psychiatry. 1987;44(11):970–975. doi: 10.1001/archpsyc.1987.01800230050009. doi:10.1001/archpsyc.1987.01800230050009. [DOI] [PubMed] [Google Scholar]
- Rauch S, Foa E. Emotional processing theory (EPT) and exposure therapy for PTSD. Journal of Contemporary Psychotherapy. 2006;36:61–65. doi: 10.1007/s10879-006-9008-y. [Google Scholar]
- Scheiderer EM, Wang T, Tomko RL, Wood PK, Trull TJ. Negative affect instability among individuals with comorbid borderline personality disorder and posttraumatic stress disorder. Clinical Psychological Science. 2015:1–15. doi: 10.1177/2167702615573214. doi: 10.1177/2167702615573214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: Review and Methodological Considerations. Psychiatry. 2008;71:134–168. doi: 10.1521/psyc.2008.71.2.134. doi:10.1521/psyc.2008.71.2.134. [DOI] [PubMed] [Google Scholar]
- Sack M, Hofmann A, Wizelman L, Lempa W. Psychophysiological changes during EMDR and treatment outcome. Journal of EMDR Practice and Research. 2008;2(4):239–246. doi:10.1891/1933-3196.2.4.239. [Google Scholar]
- Tull M, Barrett H, McMillan E, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. Doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Krinsley KE, Haddad W, Huska JA, Keane TM. The Clinician-Administered PTSD Scale: reliability and construct validity.. annual meeting of the Association for the Advancement of Behavior Therapy; Boston. Nov, 1992. [Google Scholar]
- Weathers FW, Blake DD, Litz BT. Reliability and validity of a new structured interview for PTSD.. In: Keane TM, editor. Advances in psychometric assessment of combat related post-traumatic stress disorder; Symposium presented at the meeting of the American Psychological Association; San Francisco, CA. 1991. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. doi:10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. [Google Scholar]
- Wolfe J, Chrestman KR, Ouimette PC, Kaloupek D, Harley M, Bucsela M. Trauma-related psychophysiological reactivity in women exposed to war-zone stress. Journal of Clinical Psychology. 2000;56:1371–1379. doi: 10.1002/1097-4679(200010)56:10<1371::AID-JCLP8>3.0.CO;2-X. doi: 10.1002/1097-4679(200010)56:10<1371::AID-JCLP8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]