Abstract
This study evaluated the efficacy of the From Survivor to Thriver program, an interactive, online therapist-facilitated cognitive-behavioral program for rape-related PTSD. Eighty-seven college women with rape-related PTSD were randomized to complete the interactive program (n = 46) or a psycho-educational self-help website (n = 41). Both programs led to large reductions in interview-assessed PTSD at post-treatment (interactive d = 2.22, psycho-educational d = 1.10), which were maintained at three month follow-up. Both also led to medium- to large-sized reductions in self-reported depressive and general anxiety symptoms. Follow-up analyses supported that the therapist-facilitated interactive program led to superior outcomes among those with higher pre-treatment PTSD whereas the psycho-educational self-help website led to superior outcomes for individuals with lower pre-treatment PTSD. Future research should examine the efficacy and effectiveness of online interventions for rape-related PTSD including whether treatment intensity matching could be utilized to maximize outcomes and therapist resource efficiency.
Keywords: rape, posttraumatic stress disorder, online therapy, clinical trial
1. Introduction
The experience of rape is associated with high rates of posttraumatic stress disorder (PTSD; Boudreaux, Kilpatrick, Resnick, Best, & Saunders, 1998; Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Rizvi, Vogt, & Resick, 2009; Van Minnen, Arntz, & Keijsers, 2002; Zinzow et al., 2012). Although efficacious treatments for rape-related PTSD exist, help seeking among rape victims remains very low, with few victims accessing available services and many distressed victims delaying treatment for years (Ahrens, Campbell, Ternier-Thames, Wasco, & Sefl, 2007; Foa, Rothbaum, Riggs, & Murdock, 1991; Walsh, Banyard, Moynihan, Ward, & Cohn, 2010). For many rape victims, it is likely that stigma concerns serve as a key barrier to help-seeking. Indeed, a recent study of college rape victims found that only 3% accessed available campus services for victims and that privacy concerns (70%), shame and embarrassment (50%), and concerns about others finding out (39%) were among the reasons most often cited for not utilizing services (Walsh et al., 2010). Thus, there is a need to develop alternative interventions, such as online programs, in order to disseminate efficacious treatments to affected individuals while allaying potential privacy and stigma concerns.
Several online cognitive-behavioral treatments for PTSD have been developed and evaluated, including prolonged exposure based protocols (Lange et al., 2003; Lange et al., 2000; Litz, Engel, Bryant, & Papa, 2007), self-help cognitive-behavioral protocols (Hirai & Clum, 2005; Klein et al., 2010), a cognitive restructuring self-help based protocol with or without exposure components (Spence et al., 2014), and a protocol designed to increase adaptive trauma-related coping (Wang, Wang, & Maercker, 2013). These online programs have varied in their level of therapist involvement, including those that were primarily self-help (e.g., Hirai & Clum, 2005; Spence et al., 2014; Wang et al., 2013), those that involved email and/or telephone based therapist support (e.g., Klein et al., 2010; Knaevelsrud & Maercker, 2007; Lange et al., 2003), as well as one which included limited in-person and telephone therapy sessions (Litz et al., 2007). In general, clinical trials have supported the efficacy of these online cognitive-behavioral programs with them leading to large sized reduction in PTSD symptoms from pre- to post-treatment (ds = 0.8–1.9), as well as larger reductions in PTSD symptoms as compared to waitlist (ds = 0.4–1.4). In addition, Litz and colleagues (2007) found that their online program that included limited in-person and telephone based therapy sessions led to superior post-treatment PTSD symptom outcomes as compared to a psycho-educational website, d = 1.0, among a sample of 24 U.S. Department of Defense employees.
Despite the promising nature of these programs, the extant research regarding them suffers from a number of methodological limitations. First, many trials excluded individuals with elevated depressive symptoms and/or individuals with histories of childhood sexual abuse (Hirai & Clum, 2005; Klein et al., 2010; Lange et al., 2003; Lange et al., 2000). As a result, it is unclear whether findings from those studies would generalize to more distressed individuals (e.g., those with comorbid depression or childhood trauma histories). In addition, several trials included individuals with subclinical PTSD as well as those meeting full diagnostic criteria (Hirai & Clum, 2005; Knaevelsrud & Maercker, 2007; Lange et al., 2003; Lange et al., 2000; Wang et al., 2013), and thus it is not known if comparable results would have been obtained if participants were restricted only to those who met full diagnostic criteria. Additionally, with the exception of Litz and colleagues (2007), no others compared the efficacy of the online program to an active control condition. Also, many of these programs did not leverage the potential advantages of online interventions, such as integrating multimedia into the program (e.g., videos) or using secure online asynchronous communication within the program (as opposed to using email which is less secure). Finally, none of these programs were tailored to meet the needs of a particular population of trauma victims, such as women who have experienced rape.
The aim of the current study was to evaluate the efficacy of The From Survivor to Thriver program, a therapist-facilitated, online cognitive-behavioral program tailored to meet the needs of rape victims with PTSD. The From Survivor to Thriver program is a nine module, online, therapist-facilitated program that utilizes a variety of cognitive behavioral strategies (e.g., relaxation training, cognitive restructuring) to address issues commonly faced by rape victims (e.g., self-blame for the assault, difficulties with trust and intimacy). It includes written text, video content, and written examples of women modeling skills taught in the program. In addition, the program integrates individually tailored written and video feedback from a program therapist. A pilot study with five college women with rape-related PTSD who completed the program in a lab setting over the course of seven weeks supported that it led to large-sized reductions in PTSD symptoms (d = 2.4), anxiety symptoms (d = 1.1), and vulnerability fears (d = 2.7; Author Citation, 2012).
For the current study, a randomized clinical trial (RCT) was conducted comparing the efficacy of the From Survivor to Thriver program with a self-help psycho-educational website among a sample of college women who met full diagnostic criteria for rape-related PTSD. College women were chosen as participants as they report high rates of rape and current PTSD, as well as low rates of help seeking (e.g., Walsh et al., 2010; Zinzow et al., 2012). In addition, the vast majority of college students utilize the Internet on a regular basis and report comfort with using it for mental health information and support (e.g., Horgan & Sweeney, 2010; Smith, Rainie, & Zickuhr, 2011). Thus, college women seemed a population that might be particularly likely to utilize an online intervention for rape-related PTSD. Based on prior studies of therapist-facilitated and self-help based interventions for PTSD, it was predicted that both programs would be efficacious in reducing PTSD symptomology. Drawing on the findings from the treatment intensity matching literature (e.g., CATS Consortium, 2010; De Leon, Melnick, & Cleland, 2008; Hammond et al., 2012), it was hypothesized that the therapist-facilitated intervention would demonstrate superior efficacy among participants with higher levels of pre-treatment PTSD but not among individuals with lower levels of pre-treatment PTSD.
2. Methods
2.1 Participants
Participants were 87 women with a diagnosis of rape-related PTSD currently enrolled as a student at one of four universities/community colleges. Participants were recruited via posted advertisements on all four campuses (e.g., fliers, campus bus advertisements, advertisements in campus newspapers), postings on university psychology department participant management websites, as well as via social media (e.g., a study Facebook page, postings in student Facebook groups). Recruitment materials and the informed consent emphasized that the study was designed to evaluate the efficacy of online programs for women distressed about an unwanted sexual experience. All materials and study procedures were approved by the institutional review boards at the four participating universities/community colleges.
Diagnostic status and study eligibility was determined via a telephone interview conducted by study staff (either an advanced clinical psychology doctoral student or a postdoctoral fellow). Items from the Sexual Experiences Survey-Revised (SES-R) were administered to determine that participants had experienced a completed rape since the age of 14 (Koss et al., 2007). PTSD diagnosis was determined using the PTSD Symptom Scale Interview (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993). Participants were instructed to respond to the items on the PSS-I in reference to their experience of completed rape, or their self-assessed worst experience of completed rape if they had experienced multiple rapes. Information about the characteristics of participants’ rape experience (or worst rape experience) was assessed using an extant questionnaire (Littleton, Axsom, Breitkopf, & Berenson, 2006).
Exclusion criteria included currently receiving psychotherapy, lack of stability on psychotropic medication (individual has not been on current medication/dosage for at least three months), active suicidality as determined by interview utilizing the Scale for Suicidal Ideation (Beck, Kovacs, & Weissman, 1979), or meeting DSM-IV criteria for current substance dependence as assessed with the substance use disorder module of the SCID-IV (First, Spitzer, Gibbon, & Williams, 2002). In addition, all participants had to have regular access to a computer and a telephone number at which they could reliably be reached.
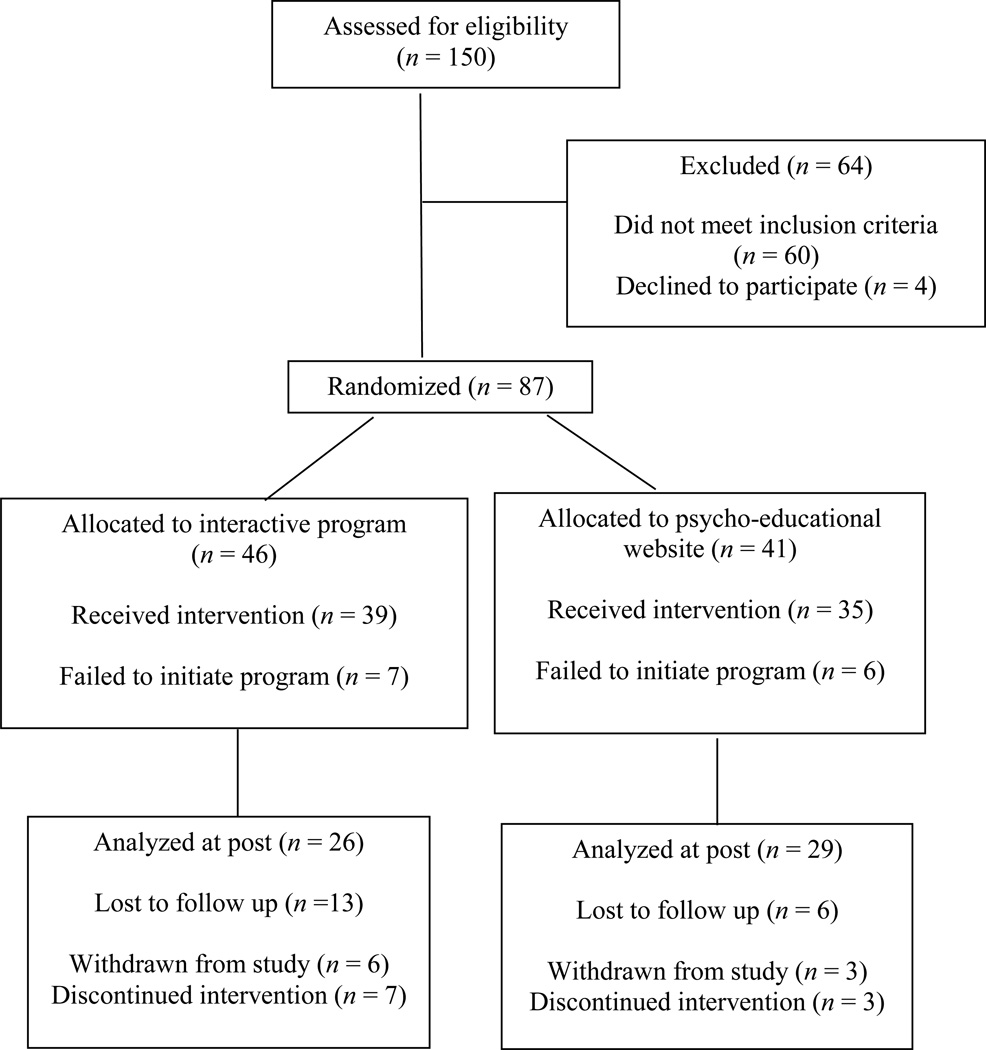
In total, 150 women were screened for eligibility via telephone. Of these, 87 women completed the screening and were determined to be eligible to participate. The most common reasons for ineligibility were reporting insufficient symptoms to meet diagnostic criteria for PTSD (31.3%, n = 20), currently receiving psychotherapy (26.6%, n = 17), or the individual had either experienced a completed rape that was a continuation of childhood sexual abuse committed by an authority figure/caregiver/relative or had not experienced a completed rape (15.6%, n = 10). Less frequent reasons for exclusion were current substance dependence (6.3%, n = 4), lack of stability on psychotropic medication (4.7%, n = 3), current suicidality (3.2%, n = 2), not currently enrolled as a student (3.2%, n = 2), and the potential participant appeared too acutely distressed to participate (3.2%, n = 2). In addition, four women (6.3%) decided during the screening that they no longer wished to participate.
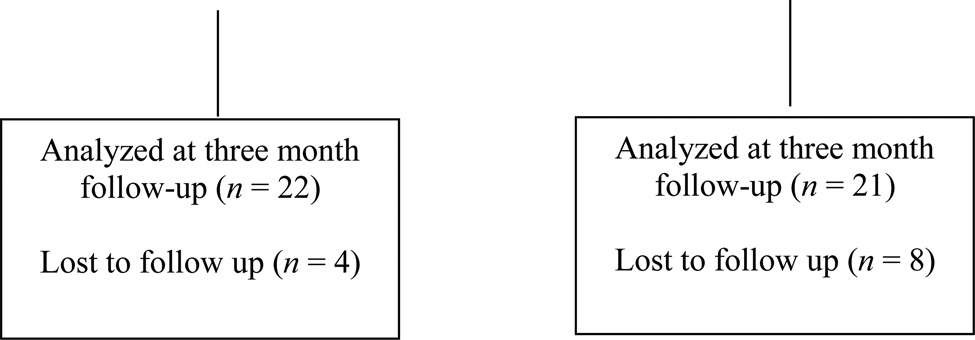
Of the 87 eligible and randomized women, 73 (83.9%) subsequently completed the baseline online questionnaires and logged in to their assigned program at least once (n = 39 interactive program, n = 35 psycho-educational website). There were no significant differences in pre-treatment PTSD symptoms or symptom interference ratings between women who initiated the program and those who did not. Among women assigned to the interactive program, 26 (66%) completed at least one post-treatment assessment (interview or online questionnaires), 22 (85%) of whom were retained for a three month follow-up assessment. Among women assigned to the psycho-educational website, 29 (83%) completed at least one post-treatment assessment, of whom 21 (72%) were retained for the three month follow-up. Women who did not log in to the interactive program for four weeks were considered drop-outs (15.2%, n = 7), of whom two (28.5%) completed at least one post-treatment assessment and one (14.3%) completed the three month follow-up assessment. There were no differences between drop-outs and completers on demographics, child abuse history, and pre-treatment PTSD, depression, or general anxiety.
2.2 Measures
2.21 Interview measures
Items from the Sexual Experiences Survey-Revised (SES-R) were administered during the initial telephone screening to determine if participants had experienced a completed rape in adolescence or adulthood (Koss et al., 2007). The SES-R consists of behaviorally specific questions designed to assess experiences of sexual victimization. Three items were administered to assess experiences of completed rape since the age of 14. These items queried regarding experiences of completed acts of oral, vaginal, or anal penetration perpetrated by 1. use of verbal threats to harm the individual or someone they care about, 2. use of physical force such as holding down or hitting the individual, and/or 3. taking advantage of the individual when she was not capable of consenting due to substance-induced impairment. To verify that an endorsed experience did not represent an ongoing experience of childhood sexual abuse, follow-up items queried whether the participant had an ongoing relationship with the person who assaulted her, and if so, the nature of that relationship, as well as how old the participant was when the experience began if she reported ongoing sexual abuse/rape.
To gather information about the characteristics of participants’ rape experience (or worst experience if she had experienced multiple rapes), a structured questionnaire (Littleton et al., 2006) was utilized that assessed the participant’s relationship with the perpetrator and forms of force used by the perpetrator during the rape: non-verbal intimidation, verbal threats, moderate force (holding her down, using body weight), and severe force (hitting, slapping, showing a weapon). Items also queried regarding the forms of resistance engaged in by the participant during the rape, classified as low (turning cold, crying), moderately (begging or pleading), or strongly (physically struggling, running away) assertive resistance. In addition, the number of standard alcoholic drinks consumed by the participant and impairment during the assault due to substance use (asleep, motor impairment, verbal impairment, unconscious) was assessed (Littleton et al., 2006).
To assess suicidality at pre-treatment, the Scale for Suicide Ideation (SSI) was administered (Beck et al., 1979). The SSI is a 21-item measure of current suicidal attitudes, behaviors, and plans. Initially, five screening items were administered, with the full measure administered if an individual endorsed any of these initial items (Beck & Steer, 1993). Previous studies have supported that a score of 3 or above is associated with elevated suicide risk and clinically significant suicidality (Brown, Beck, Steer, & Grisham, 2000; Holi et al., 2005). Therefore, an extensive interview to determine risk of suicidality was conducted with any individual who scored a 3 or above.
To assess current substance dependence at pre-treatment, the SCID-I/P Substance Use Disorders (SUD) module was administered (First et al., 2002). The SCID-I/P is a highly reliable structured interview that assesses whether an individual meets DSM-IV criteria for alcohol or other substance dependence (Martin, Pollock, Bukstein, & Lynch, 2000; Zanarini et al., 2000).
The PTSD Symptom Scale-Interview (PSS-I; Foa et al., 1993) was administered at each assessment to evaluate whether participants met criteria for rape-related PTSD. The PSS-I is a reliable interview measure that consists of 17 items designed to map on to the DSM-IV criteria for the diagnosis of PTSD (Foa et al., 1993). For each item, participants were asked to indicate how much they had been bothered by each symptom in the past month in connection to their rape experience (or worst rape experience). Scores can range from 0 to 51 and a cutoff score of 14 is recommended (Coffey, Gudmundsdottir, Beck, Palyo, & Miller, 2006). Cronbach’s alpha in the current study ranged from .70 to .83 across the three assessments. In addition, participants were asked to indicate how much their PTSD symptoms currently interfered with their: 1. academic performance, 2. relationships with others, 3. job/volunteer work, and 4. life overall on a 0 (does not interfere at all) to 3 (interferes very much) scale for each item.
2.22 Self-report measures
The Center for Epidemiological Studies-Depression Scale was administered to assess current depressive symptoms (CES-D; Radloff, 1977). The CES-D is a 20 item, self-report measure of past week depressive symptoms, primarily tapping the affective dimension of depression. Scores can range from 0 to 60 with scores of 21 or above suggesting clinically significant depressive symptoms among college student samples (Shean & Baldwin, 2008). Prior research supports the measure’s test-retest reliability, convergent validity as compared to other self-report and interviewer administered measures of depression, and sensitivity to changes in symptomology following treatment (Radloff, 1977; Weissman, Sholomskas, Pottenger, Prusoff, & Locke, 1977). Cronbach’s alpha in the current study ranged from .87 to .91 across the three assessments.
To assess symptoms of general anxiety, the Four Dimensional Anxiety Scale was administered (FDAS; Bystritsky, Linn, & Ware, 1990). The FDAS is a 35 item measure of past week physiological, cognitive, emotional, and behavioral anxiety symptoms with a possible range of 35 to 175. Research supports the measure’s internal consistency, convergent validity with other self-report anxiety symptom measures, and ability to discriminate individuals seeking anxiety treatment from a general medical sample (Bystritsky et al., 1990; Stoessel, Bystritsky, & Pasnau, 1995). Cronbach’s alpha in the current study ranged from .91 to .94 across the three assessments.
To assess history of other forms of interpersonal violence, items from the Stressful Life Events Screening Questionnaire were administered at pre-treatment (SLESQ; Goodman, Corcoran, Turner, Yuan, & Green, 1998). Prior research supports the measure’s test-retest reliability as well as convergence with an interviewer-administered measure of traumatic event history (Goodman et al., 1998). To assess interpersonal trauma history, an initial yes-no behaviorally specific screening item was administered. If an individual endorsed the initial screening item, follow-up items were administered that assessed the participant’s age when the abuse/violence occurred, the duration/frequency of the abuse/violence, the participant’s relationship with the perpetrator or perpetrators, and the type of abuse/violence experienced or witnessed. In the current study, five screening items from the measure were administered to assess experiences of childhood/adolescent physical abuse, childhood sexual abuse, and childhood/adolescent witnessing domestic violence. A sixth screening item assessing experiences of physical violence from a dating partner was also administered. Participants’ responses to these items were reviewed by the first author who classified participants as having experienced childhood sexual abuse (experienced some type of sexual touching/contact before age 14), childhood/adolescent physical abuse by a parent/caregiver (experienced hitting/slapping/beating with a fist or other object that left marks by a parent/caregiver before age 18), witnessed domestic violence in childhood/adolescence (witnessed parents/caregivers hitting, slapping, or beating each other before age 18), and/or experienced domestic violence (experienced hitting/slapping, beating with a fist or object that left marks by a dating partner).
2.23 Assessment of therapist competence, satisfaction, and working alliance
To assess the competence of the online written and video feedback provided by therapists in the interactive program, an 18-item therapist competence rating form was developed for the study. Items evaluated therapist competence in a number of areas including establishing and maintaining the therapeutic relationship (e.g., conveying empathy, establishing a collaborative relationship), assisting the client with problems/goal setting (e.g., encouraging healthy coping, assisting with goal setting), and facilitating use of cognitive-behavioral strategies (e.g., providing socialization to the cognitive model, assisting the client with developing alternative views of distorted cognitions). For each item, raters evaluated the competence of the therapist’s feedback to a participant on a specific interactive program module on a scale ranging from 1 (did not display competence or displayed minimal competence) to 3 (displayed strong competence), providing ratings on the feedback provided in two to three modules for each participant. The competence ratings were conducted by three licensed psychologists unaffiliated with the project, each of whom had over a decade of training and experience providing cognitive behavioral therapy to individuals with PTSD.
The Working Alliance Inventory-Short Form (WAI-S) was administered at post-treatment to assess therapeutic alliance among interactive program participants (Horvath & Greenberg, 1989; Tracey & Kokotovic, 1989). The WAI-S is a 12 item measure of working alliance in three areas: agreement on therapeutic tasks (My therapist and I agree about the things I needed to do to help improve my situation), mutual endorsement of therapeutic goals (My therapist and I are working toward mutually agreed upon goals), and bond between therapist and client (I feel that my therapist appreciates me). For each item, individuals rated the extent to which the statement was true regarding their experience working with their therapist on a scale bounded by 1 (Never) and 7 (Always). Prior research supports the measure’s reliability and factor structure, including among individuals completing online treatment (Busseri & Tyler, 2003; Leibert, Archer, Munson, & York, 2006; Tracey & Kokotovic, 1989). In addition, scores have been found to predict improvement in therapy (Busseri & Tyler, 2003; Tracey & Kokotovic, 1989). Cronbach’s alpha in the current sample was acceptable: task α = .91, bond α = .96, and goals α = .72.
To assess participant satisfaction with the interactive program and their program therapist, the Satisfaction with Therapy and Therapist Scale-Revised (STTS-R) was administered at post-treatment (Oei & Green, 2008). The STTS-R is a 12 item measure which provides scores on two scales- satisfaction with one’s therapist and satisfaction with the treatment received. Individuals rate their agreement with each item on a Likert scale bounded by 1 (Strongly disagree) and 5 (Strongly agree). Research supports the measure’s reliability and factor structure, and scores discriminated low and high improvement groups following treatment for mood and anxiety disorders (Oei & Green, 2008). In the current study, Cronbach’s alpha of the satisfaction with treatment received scale was .95 and the satisfaction with therapist scale was .92.
2.3 Online programs
2.31 Interactive program
The From Survivor to Thriver Program consisted of nine program modules (see Table 1). The program was designed to be completed sequentially, with participants completing one module at a time. Once a participant completed a module, she was given access to the next program module by her therapist. The program had three phases. The first phase (modules 1–3) was designed to provide psycho-education about PTSD and the impact of unwanted sex, as well as introduce general distress management strategies (i.e., relaxation, grounding) and healthy coping (e.g., asking others for help, setting an action plan) skills. The second phase (modules 4–5) introduced the cognitive model and taught participants to identify distorted and unhelpful automatic thoughts and utilize the challenging questions technique to respond to these thoughts. The third phase (modules 6–9) focused on using a number of cognitive-behavioral techniques (e.g., the challenging questions technique, the pros and cons technique, behavioral experiments) to address specific concerns common among women following sexual assault (e.g., difficulties with trust, self-blame for the assault).
Table 1.
Module content of the intervention program
| Module | Name | Content |
|---|---|---|
| 1 | Welcome to the From Survivor to Thriver program |
Introduces the From Survivor to Thriver program, as well as provides psycho-education about frequent issues encountered following unwanted sex. Individuals are encouraged to think of ways their experience of unwanted sex has affected them, as well as to identify personal and social strengths. |
| 2 | Introduction to relaxation and grounding |
Discusses individuals’ emotional and physiological responses to stressful situations and introduces relaxation techniques to help individuals manage stress and reduce physiological arousal level. Grounding is also introduced as a technique to respond to strong emotions and dissociative responses. |
| 3 | Introduction to adaptive and maladaptive coping |
Introduces adaptive and maladaptive coping strategies. Individuals are encouraged to evaluate their coping approaches and more consistently select adaptive coping strategies. Examples include asking for help, practicing good self-care, and setting an action plan. |
| 4 | Introduction to automatic thoughts |
Introduces the cognitive model and discusses the relationships among situations, thoughts, and feelings. Individuals are taught to begin identifying their own maladaptive automatic thoughts. |
| 5 | Introduction to the challenging questions technique |
Introduces the challenging questions technique as a useful tool to challenge maladaptive automatic thoughts and modify maladaptive thought patterns. |
| 6 | Coping with stigma, thoughts of low self- worth, and shame |
Provides education regarding stigma, self-worth, and shame, as well as helps individual identify the role that these cognitions (and subsequent emotions) may be playing in their own lives. Challenging questions and pros/cons techniques are used to evaluate shame and stigma concerns. |
| 7 | Coping with trust and intimacy concerns |
Discusses difficulties with trusting others as well as physical intimacy with a partner. Challenging questions, pros/cons technique, and behavioral experiment are used to respond to trust and intimacy concerns. |
| 8 | Coping with self- blame |
Helps individuals identify ways in which they may be blaming themselves for their experience. Introduces the re-attribution technique to address self-blame. |
| 9 | Coping with safety concerns |
Discusses safety concerns and how this concern could cause individuals to avoid situations perceived as dangerous, or, alternatively, miss cues that a situation is potentially unsafe. Challenging questions and pros/cons technique are used to evaluate safety concerns. |
Each module contained several components, including: a video clip of the program developers discussing the topic covered in the module, a written description of the skills or techniques being introduced or utilized in the module, and, for modules 4 through 9, written examples of women modeling using the skills and techniques utilized in the module. The final program component included in all modules was the interactive exercises. These interactive exercises were designed either to help women think about the extent to which the particular issue raised in the module was a concern for them (e.g., the extent to which they blame themselves for the sexual assault) or to enable them to practice a described cognitive-behavioral skill or technique and receive feedback on their practice. The interactive exercises were completed asynchronously, and were designed in a question and answer format, e.g., “What were your automatic thoughts in this situation?” “How do you know if you can trust someone?” After a participant completed the interactive exercise, her program therapist then provided written feedback to each answer provided, as well as embedded a video message containing more extensive feedback on the interactive exercise page in the program. Therapist feedback focused on encouraging and praising participants for their effort, expressing empathy, encouraging continued program progress, socializing participants to the cognitive model, and providing assistance in challenging automatic thoughts, such as through further use of Socratic questioning. Thus, the interactive exercises served to establish and maintain a therapeutic alliance, increase women’s efficacy to use the program skills, and assist them in successfully utilizing the cognitive-behavioral skills introduced in the program.
2.32 Psycho-educational website
The psycho-educational website contained the written informational content of the first three modules of the interactive program including the symptoms of PTSD, information about relaxation and grounding, and information about healthy coping strategies. The website did not contain any of the multimedia content (videos from the program developers, audio recorded relaxation exercises) or any interactive exercises. Women assigned to the psycho-educational website condition were given access to all the website content and instructed to log in to the program and utilize the content in whatever manner and however frequently they desired to do so over the course of the study.
2.4 Procedure
A telephone screening interview was scheduled with interested potential participants who signed up to be contacted on a website created for the study or on one of the psychology department participant management websites, or who directly contacted the study office via telephone or text message. During this screening, women were informed about the study procedures and gave verbal consent after review of the consent form with study staff. They then completed a 30 to 60 minute telephone interview to determine eligibility. Eligible women then created a program username and password, were given instructions on how to log in to the online program, and were sent a copy of the consent form via email. Before initiating the program, they were required to complete a battery of self-report online questionnaires. Participants were randomized to the interactive program or psycho-educational website based on a computerized coin flip. Once participants completed the online questionnaires, they were given access to the online program content and were sent a program welcome message via email.
Participants had 14 weeks to view content in the online program to which they were assigned. While participating in the online program, they received scheduled check-in phone calls from study staff (doctoral students in clinical psychology) approximately once every two weeks. During these brief check-in calls (approximately 5 minutes), seven queries were conducted: 1. Participants’ recent mood and any changes in mood (e.g., increased depression); 2. Recent substance use; 3. Any suicidal or self-harming urges or behaviors; 4. Time spent in enjoyable activities; 5. Frequency of logging into the program; 6. Technical problems or distress related to completing the program; and 7. Any upcoming events that would prevent program participation. Participants varied in their completion of these check-in calls, completing 3.8 check-ins on average (range 0 to 7; SD = 1.87).
After approximately 14 weeks, participants were contacted via email and telephone to complete a post-treatment interview regarding their current rape-related PTSD symptoms and impressions of the program, as well as provided information about how to complete the post-treatment online questionnaires. Participants who completed at least one post-treatment assessment (phone interview or online questionnaires) were contacted via email and telephone three months after completing the program to complete a follow-up telephone interview regarding their current rape-related PTSD symptoms, as well as to complete follow-up online questionnaires. Participants received a $25 gift card for completing each interview and each set of online questionnaires (total possible compensation of $150). The study was approved by the Institutional Review Boards at each participating community college/university and a data safety monitoring board, consisting of three faculty members at the first author’s institution unaffiliated with the project, reviewed study progress/human subjects issues at six month intervals during the RCT.
2.5 Statistical analysis
Analyses were conducted on individuals who initiated the assigned programs and provided data at post-test assessments. The use of “initiators” in our analysis allowed us to investigate the effect of the program for both groups of participants. In addition, estimates of change from pre-test to post-test and follow-up were estimated for all participants assigned to a program, an Intent-to-Treat (ITT) model. For the ITT analyses, post-test and follow-up data for participants who left the study was imputed using the R package mice (van Buuren & Groothuis-Oudshoorn, 2011). Twenty imputations were used with all outcome variables.
To evaluate whether participants in both programs experienced clinically significant change on study measures from pre- to post-and follow-up assessments, the reliable change index (RCI) was utilized (Jacobson & Truax, 1991). The RCI is a measure of statistically and clinically significant improvement following treatment that takes into account both the measure’s reliability and variability in participants’ scores at pre-treatment. RCI values are converted into standardized Z scores, and thus scores above 1.96 represent significant change (Jacobson & Truax, 1991). Prior research supports that the RCI is a more conservative estimate of clinically significant change than other extant measures (Hays, Brodsky, Johnston, Spritzer, & Hui, 2005).
To evaluate the comparative efficacy of the two programs, a residual difference score model was used to assess change from pre- to post-treatment. In the residual difference score model, post-treatment scores are predicted by pre-treatment scores and provide an estimate of change from pre-treatment (Little, 2013). Treatment effects were estimated by regressing outcomes (PTSD symptoms, depressive symptoms, anxiety symptoms) on a binary predictor representing treatment condition (0 = psycho-educational website, 1 = interactive program). The effect of treatment condition is a test of differential change from pre-treatment across conditions. Additional analyses investigated if treatment effects differed as a function of level of pre-treatment symptomology. These moderation analyses investigated the interaction of treatment condition (the focal predictor) and pre-treatment scores (the moderator) on the dependent variable at post-treatment. If a significant interaction was present, simple slope analyses were conducted at one standard deviation above and below the mean of pre-treatment scores.
3. Results
3.1 Pre-treatment characteristics
Demographic information, information about prior trauma history, and characteristics of participants’ index rape experience among the 87 women assigned to one of the online programs is summarized in Table 2. Participants were 22 years old on average (range 18–42 years) and most were ethnic minorities, with representation across multiple ethnic groups. The ethnic representation of participants was consistent with the demographic profiles of the universities from which they were recruited. Over half of participants had experienced some other form of interpersonal violence, with childhood/adolescent physical and/or sexual abuse being most commonly reported, followed by physical abuse by a romantic partner.
Table 2.
Demographic characteristics, prior trauma history, and index rape characteristics of participants stratified by program condition
| Interactive program (n = 46) % (n) |
Psycho-educational website (n = 41) % (n) |
|
|---|---|---|
| Race | ||
| White/European American | 41.3% (19) | 51.2% (21) |
| Black/African American | 21.7% (10) | 29.3% (12) |
| Asian American/Pacific Islander | 8.7% (4) | 4.9% (2) |
| Native American | 0.0% (0) | 2.4% (1) |
| Multi-ethnic | 19.6% (9) | 7.3% (3) |
| Not reported | 8.7% (4) | 4.9% (2) |
| Ethnicity | ||
| Hispanic/Latina | 6.5% (3) | 9.8% (4) |
| Not Hispanic/Latina | 87.0% (40) | 90.2% (37) |
| Not reported | 6.5% (3) | 0.0% (0) |
| Prior trauma history | ||
| Childhood sexual abuse | 32.6% (15) | 24.4% (10) |
| Childhood/adolescent physical abuse | 23.9% (11) | 24.4% (10) |
| Witnessed domestic violence | 2.2% (1) | 2.4% (1) |
| Physical abuse by romantic partner | 15.2% (7) | 19.5% (8) |
| Relationship with perpetrator | ||
| Stranger/just met | 19.6% (9) | 7.3% (3) |
| Acquaintance | 26.1% (12) | 22.0% (9) |
| Friend | 13.0% (6) | 41.5% (17) |
| Romantic partner | 32.6% (15) | 29.3% (12) |
| Relative/guardian | 8.7% (4) | 0.0% (0) |
| Force by perpetrator | ||
| Non-verbal intimidation | 65.2% (30) | 51.2% (21) |
| Verbal threats | 37.0% (17) | 26.8% (11) |
| Moderate physical force | 89.1% (41) | 82.9% (34) |
| Severe physical force | 43.5% (20) | 19.5% (8) |
| Resistance during assault | ||
| Low assertive resistance | 93.5% (43) | 87.8% (36) |
| Moderately assertive resistance | 91.3% (42) | 80.5% (33) |
| Strongly assertive resistance | 87.0% (40) | 70.7% (29) |
| Binge drinking during assault | 23.9% (11) | 41.5% (17) |
| Substance-related impairment during assault | ||
| Asleep | 13.0% (6) | 17.1% (7) |
| Verbal impairment | 34.8% (16) | 48.8% (20) |
| Motor impairment | 37.0% (17) | 58.5% (24) |
| Unconscious | 15.2% (7) | 17.1% (7) |
| Participant scores on psychological distress measures at pre-treatment, post-treatment, and three month follow-up stratified by online program condition. | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Interactive program | Psycho-educational website | ||||||||||
| M (SD) | Range | n | dcompleter | dITT | % RCI | M (SD) | Range | n | dcompleter | dITT | % RCI | |
| PSS-I | ||||||||||||
| Pre | 23.7 (6.5) | 11–35 | 38 | 23.0 (7.3) | 11–43 | 35 | ||||||
| Post | 11.2 (5.8) | 0–22 | 23 | 2.22 | 0.88 | 73.9 | 10.4 (8.5) | 0–39 | 28 | 1.10 | 0.86 | 75.0 |
| Follow-up | 7.9 (6.3) | 0–23 | 20 | 2.60 | 1.80 | 80.0 | 6.8 (5.7) | 0–21 | 21 | 2.26 | 1.80 | 70.0 |
| Interference (school) | ||||||||||||
| Pre | 1.2 (0.9) | 0–3 | 38 | 1.3 (1.0) | 0–3 | 35 | ||||||
| Post | 0.7 (0.8) | 0–2 | 23 | 0.71 | 0.28 | — | 0.8 (1.0) | 0–3 | 28 | 0.54 | 0.32 | — |
| Interference (work) | ||||||||||||
| Pre | 0.8 (0.9) | 0–3 | 38 | 0.7 (0.9) | 0–3 | 35 | ||||||
| Post | 0.3 (0.7) | 0–3 | 23 | 1.69 | 0.05 | — | 0.4 (0.8) | 0–3 | 28 | 0.39 | 0.13 | — |
| Interference (relationships) | ||||||||||||
| Pre | 2.5 (0.6) | 1–3 | 38 | 2.2 (0.7) | 0–3 | 35 | ||||||
| Post | 1.3 (1.0) | 0–3 | 23 | 1.53 | 0.51 | — | 1.6 (0.9) | 0–3 | 28 | 0.76 | 0.79 | — |
| Interference (overall) | ||||||||||||
| Pre | 2.1 (0.6) | 1–3 | 38 | 2.1 (0.6) | 1–3 | 35 | ||||||
| Post | 1.5 (0.8) | 0–3 | 23 | 0.99 | 0.60 | — | 1.3 (0.7) | 0–3 | 28 | 1.08 | 0.50 | — |
| CES-D | ||||||||||||
| Pre | 22.0 (9.7) | 7–42 | 38 | 22.6 (9.1) | 5–40 | 35 | ||||||
| Post | 14.7 (9.6) | 4–36 | 18 | 0.76 | 0.68 | 40.0 | 13.2 (7.5) | 3–34 | 24 | 0.86 | 0.39 | 37.5 |
| Follow-up | 14.4 (10.7) | 0–39 | 20 | 0.95 | 0.84 | 40.0 | 10.8 (7.2) | 0–24 | 17 | 1.03 | 0.62 | 52.9 |
| FDAS | ||||||||||||
| Pre | 78.7 (18.4) | 48–114 | 37 | 81.5 (23.4) | 38–136 | 33 | ||||||
| Post | 68.9 (23.3) | 38–117 | 20 | 0.70 | 0.75 | 55.0 | 58.7 (16.4) | 37–96 | 23 | 0.87 | 0.63 | 52.2 |
| Follow-up | 60.7 (16.0) | 35–101 | 19 | 1.50 | 0.78 | 68.4 | 59.7 (17.2) | 37–96 | 17 | 1.05 | 0.68 | 52.9 |
Note: PSS-I: PTSD Symptom Scale-Interview, possible range 0–51; CES-D: Center for Epidemiological Studies- Depression Scale, possible range 0–60; FDAS: Four Dimensional Anxiety Scale, possible range 35–175; % RCI: Percentage of participants with statistically significant Reliable Change Index scores at post-treatment. Interference ratings were made on a 0–3 scale. Effect size (d) is reported for participants who completed the program (dcompleters) and all participants assigned to condition (dITT)
Participants’ index rape had occurred on average just under four years ago, although this ranged from 1.5 months to 21 years ago. Participants reported being 18 years old on average when the rape occurred, with this ranging from ages 14 to 33. The majority of participants reported a prior relationship with their assailant. The assailants included strangers, friends, acquaintances (family friend, friend of a friend, neighbor), relatives (stepfather, cousin), and romantic partners (boyfriend, husband, ex-boyfriend). In general, participants reported that the perpetrator used a variety of coercive and physically violent tactics during the rape and they reported engaging in multiple resistance behaviors. Finally, a substantial minority reported engaging in binge drinking prior to the assault as well as some type of impairment due to substance use during the assault.
Participants’ scores on the measures of psychological distress at pre-treatment are summarized in Table 2. Participants reported fairly similar levels of PTSD symptomology as participants in other clinical trials involving rape victims with PTSD (Ms = 25.5–35.5; Devilly & Spence, 1999; Foa et al., 2005; Foa, Molnar & Cashman, 1995; Foa, Riggs, Massie, & Yarczower, 1995; Ironson, Freund, Strauss, & Williams, 2002; Leiner, Kearns, Jackson, Astin, & Rothbaum, 2012; Rothbaum, Astin, & Marsteller, 2005; Van Minnen & Foa, 2006; Zoellner, Feeny, Fitzgibbons, & Foa, 1999) although there was substantial variability in PTSD scores. Participants reported moderately high levels of interference in their relationships and life overall on average due to PTSD symptoms (Ms > 2.0), but on average reported minimal to moderate interference in their job and academic performance (Ms < 1.2) due to symptoms. On average, participants reported moderate levels of depression (Ms > 22), with 56.2% scoring above the clinical cutoff, although scores covered nearly the entire possible range. Finally, participants on average reported mild to moderate symptoms of general anxiety (Ms < 82), although again, there was substantial variability in reported levels of general anxiety.
Chi square analyses were conducted comparing women assigned to the two programs on demographic characteristics, prior trauma history, and index rape characteristics. Results of the chi square analyses revealed no significant differences between women assigned to the two programs with the exception that women assigned to the interactive program were more likely to report that the perpetrator used severe force, χ2 (1, N = 87) = 5.71, p = .017. Independent samples t-tests were conducted comparing women assigned to the two programs on the distress (PSS-I, FDAS, CES-D) and interference measures. None of these analyses revealed any statistically significant differences.
3.2 Working alliance, satisfaction with therapy, and therapist competence
Women assigned to the interactive program overall reported a strong working alliance with their therapist: task, M = 5.90, SD = 0.98; bond, M = 5.79, SD = 1.12; goals, M = 5.57, SD = 1.23. A total of five participants (23.8%) reported the maximum possible score of seven on the task and bond subscales, as did seven participants (33.3%) on the goals subscale. In addition, only one participant (4.8%) obtained a mean working alliance rating lower than the midpoint of 4, with this participant obtaining a mean score of 3.75 on the goals subscale. Similarly, participants reported high levels of satisfaction with the online program, M = 4.33, SD = 0.64, and their online therapist, M = 4.43, SD = 0.62. A total of seven participants (33.3%) reported the maximum possible satisfaction rating of five with the online program, and nine participants (42.9%) reported the maximum possible satisfaction rating of five with their online therapist. No participants reported a mean satisfaction rating on either scale below the midpoint, and only one participant (4.8%) reported mean satisfaction ratings at the scale midpoint.
External raters reviewed the therapeutic feedback provided by program therapists for a total of 57 program modules reviewed. Of the modules reviewed, 49% were from phase one of the program (modules 1–3), 23% from phase two (modules 4–5), and 28% from phase three (modules 6–9). External ratings of the competence of the feedback provided by therapists were uniformly high. Mean competence ratings across the 17 items ranged from 2.85 (assisted the participant with coming up with alternative views of her distorted cognitions) to 2.98 (provided encouragement, praise, or reinforcement to the participant) out of a maximum possible score of 3.0. In addition, the external raters only gave a total of three ratings of 1 (the therapist displayed no or minimal competence) across the 1026 total ratings.
3.3 Treatment outcomes at post-treatment
Among the 38 participants who initiated the interactive program, 11 (28.9%) completed at least part of phase one (modules 1–3) of the program, 13 (34.2%) completed at least part of phase 2 (modules 4–5), 11 (28.9%) completed at least part of phase 3 (modules 6–9), and two (5.3%) did not complete any program modules. Six participants (15.8%) completed the entire program. As detailed in Table 2, results supported that both online interventions were efficacious at reducing PTSD symptoms from pre- to post-treatment: interactive program, t (22) = 7.02, p < .001, d = 2.22; psycho-educational website, t (27) = 8.06, p < .001, d = 1.10. Approximately three-fourths of participants who initiated both interventions also experienced a clinically significant reduction in PTSD symptoms as assessed by the RCI and no participants reported a clinically significant increase in PTSD symptoms. Additionally, women initiating the interactive program reported significantly lower interference in their life in all areas due to PTSD symptoms at post-treatment: school, t (22) = 3.21, p = .004; work, t (22) = 2.19, p = .039; relationships, t (22) = 5.18, p < .001; overall, t (22) = 3.51, p = .002. Similarly, women assigned to the psycho-educational website reported significantly lower interference in their school/academic performance, relationships, and life overall due to PTSD symptoms at post-treatment: school, t (27) = 2.30, p = .029; relationships, t (27) = 3.32, p = .003; overall, t (27) = 4.67, p < .001. However, they did not report significantly lower interference in their job/volunteer work due to symptoms, (27) = 1.56, p = .130. Similarly, intent-to-treat (ITT) analyses supported that both programs led to large-sized reductions in PTSD symptoms at post-testing: interactive program, dITT = 0.88, psycho-educational website, dITT = 0.86. Additionally ITT analyses supported that both programs led to medium-sized reductions in PTSD symptom interference in both their relationships (interactive program, dITT = 0.51, psycho-educational website, dITT = 0.79) and life overall (interactive program, dITT = 0.60, psycho-educational website, dITT = 0.50).
As summarized in Table 2, women in both programs experienced significant reductions in symptoms of depression from pre- to post-treatment (interactive program, t [17] = 2.27, p = .037, d = 0.76; psycho-educational website, t [24] = 4.07, p < .001, d = 0.86) and general anxiety (interactive program, t [19] = 2.30, p = .033, d = 0.77; psycho-educational website, t [22] = 5.63, p < .001, d = 0.87). Over one-third of women in both programs experienced clinically significant reductions in depression symptoms and over half reported clinically significant reductions in anxiety symptoms. None of the women assigned to the psycho-educational website reported clinically significant increases in either type of symptoms. Two women who completed the interactive program reported clinically significant increases in depression at post-treatment, one of whom also reported a clinically significant increase in anxiety. Notably, both of these women experienced the death of an immediate family member (mother, grandfather) while completing the intervention, so it is possible that these losses led to their increased symptomology. Three additional women also reported clinically significant increases in anxiety, although two of these women reported clinically significant decreases in PTSD symptomology. ITT analyses supported that both programs led to small- to medium-sized reductions in depression (interactive program, dITT = 0.68, psycho-educational website, dITT = 0.39) and anxiety symptoms (interactive program, dITT = 0.70, psycho-educational website, dITT = 0.63).
To directly compare the efficacy of the two programs at reducing PTSD symptomology and general distress, residual difference scores were compared across groups in a regression framework. As shown in Table 3, there were no significance differences between the interventions in change from pre- to post-treatment, although all three values were positive indicating more change in symptomology among individuals assigned to the interactive program as compared to the psycho-educational website.
Table 3.
Differences between interventions at post-treatment controlling for pre-treatment scores
| Measure | b | SE | p | d |
|---|---|---|---|---|
| PSS-I | 0.43 | 2.03 | .834 | 0.06 |
| CES-D | 1.27 | 2.62 | .632 | 0.15 |
| FDAS | 8.62 | 5.71 | .139 | 0.46 |
Note: PSS-I: PTSD Symptom Scale-Interview; CES-D: Center for Epidemiological Studies-Depression Scale; FDAS: Four Dimensional Anxiety Scale
Next, regression analyses were conducted to investigate if level of symptomology at pre-treatment moderated the relationship between intervention condition and symptomology at post-treatment. As shown in Table 4, there were no significant moderation effects for depression or general anxiety. In contrast, PTSD symptomology at pre-treatment significantly moderated the relationship between treatment condition and post-treatment PTSD symptomology.
Table 4.
Interaction between pre-treatment scores and intervention condition predicting post-treatment scores
| Measure | b | SE | p |
|---|---|---|---|
| PSS-I | −0.66 | 0.30 | .032 |
| CES-D | −0.32 | 0.27 | .245 |
| FDAS | −0.39 | 0.25 | .135 |
Note: PSS-I: PTSD Symptom Scale-Interview; CES-D: Center for Epidemiological Studies-Depression Scale; FDAS: Four Dimensional Anxiety Scale.
Examining the simple slopes revealed that for women with low PTSD symptomology at pre-treatment, women assigned to the interactive program had higher post-treatment PTSD symptom scores than those assigned to the psycho-educational website, b = 5.12, SE = 2.89, p = .082. In contrast, for women high in PTSD symptomology at pre-treatment, the interactive program resulted in lower post-treatment levels of PTSD symptomology than the psycho-educational website, b = −3.93, SE = 2.77, p = .164.
3.4 Maintenance of gains at follow-up
As summarized in Table 2, participants in both programs either maintained or increased reductions in symptoms at the follow-up assessment. Among women who initiated the interactive program, 80.0% reported a reliable reduction in PTSD symptoms from pre-treatment to follow-up as assessed by the RCI, t (19) = 7.55, p < .001, d = 2.60. In addition, 40.0% reported a reliable reduction in symptoms of depression, t (19) = 2.96, p < .01, d = 0.95, and 68.4% reported a reliable reduction in general symptoms of anxiety, t (18) = 4.10, p < .001, d = 1.50. ITT analyses supported that women assigned to the interactive program had large reductions in PTSD symptoms, dITT = 1.80, depression symptoms, dITT = 0.84, and anxiety symptoms, dITT = 0.78, from pre- testing to follow-up. Similarly, among women assigned to the psycho-educational website, 70.0% reported a reliable reduction in PTSD symptoms from pre-treatment to follow-up as assessed by the RCI, t (20) = 8.54, p < .001, d = 2.26. In addition, 52.9% reported a reliable reduction in symptoms of depression, t (16) = 3.39, p < .005, d = 1.03, and 52.9% reported a reliable reduction in general symptoms of anxiety, t (16) = 5.33, p < .001, d = 1.05. ITT analyses supported that women assigned to the psycho-educational website had large reductions in PTSD symptoms, dITT = 1.80, and medium-sized reductions in depression, dITT = 0.62, and anxiety symptoms, dITT = 0.68, from pre- testing to follow-up.
No participants reported a clinically significant increase in PTSD symptoms from pre-treatment to follow-up. Two participants in the interactive program reported continued clinically significant increases in depression symptoms from pre-treatment to follow-up (the same participants who reported elevated levels of depressive symptoms at post-treatment). One participant assigned to the psycho-educational website also experienced a clinically significant increase in depressive symptoms from pre-treatment to follow-up. Finally, one additional participant in the interactive program reported a clinically significant increase in anxiety at follow-up.
4. Discussion
The aim of this study was to evaluate the efficacy and acceptability of an online therapist-facilitated cognitive behavioral program tailored to meet the needs of women with rape-related PTSD. Completer analyses strongly supported the efficacy of this program with a large pre- to post-treatment effect size for PTSD symptoms (d = 2.2), which was somewhat larger than the majority of prior trials of online interventions for PTSD (ds = 0.8–1.9), and comparable to trials of several in person cognitive behavioral interventions for PTSD utilizing the same measure of PTSD symptomology (ds = 1.3–2.4; Foa, Molnar et al., 1995; Foa et al., 2005; Ironson et al., 2002; Jaycox, Foa, & Morral, 1998; Rothbaum et al., 2005; Van Minnen & Foa, 2006; Zoellner et al., 1999). Notably, ITT analyses supported similar sized reductions in PTSD symptoms (d = 0.9) as prior studies of online interventions for PTSD utilizing ITT analyses (ds = 0.8 to 1.3; Klein et al., 2010; Wang et al., 2013) as well as ITT analyses of the efficacy in person cognitive behavioral interventions for PTSD (ds = 1.1–1.4; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick et al., 2008; van Minnen & Foa, 2006).
In addition, participants reported maintenance or further improvement in PTSD symptomology at a three month follow-up assessment. Both completer and ITT analyses also supported that the interactive program led to medium to large-sized improvements in symptoms of depression and anxiety symptoms at post-testing and follow-up (ds = 0.7–1.5), which is comparable to analyses of other online interventions for PTSD (ds = 0.5–1.2; Hirai & Clum, 2005; Knaevelsrud & Maercker, 2007; Litz et al., 2007; Spence et al., 2014; Wang et al., 2013) as well as several in-person intervention trials for PTSD (ds = 0.5–1.5; Blanchard et al., 2003; Foa et al., 1999; Jaycox et al., 1998; Resick et al., 2002; Resick et al., 2008; van Minnen & Foa, 2006). Finally, women completing the interactive program reported high levels of satisfaction with the program and their therapist, as well as a strong working alliance. Thus, the interactive program was efficacious at reducing PTSD symptomology and overall well-received by participants. Notably, this strong therapeutic working alliance was formed despite the asynchronous nature of therapeutic communication. However, it should be noted that information on satisfaction and working alliance were not obtained from participants who did not complete the post-test assessment.
Results also supported the efficacy of the psycho-educational website, with completer analyses supporting that individuals assigned to this program experienced large reductions in PTSD symptoms from pre- to post-treatment (d = 1.1) and large reductions in symptoms of depression and anxiety (ds = 0.9). ITT analyses supported that this intervention led to large-sized reductions in PTSD symptoms (d = 0.9), and small to medium-sized reductions in symptoms of depression and anxiety (ds = 0.4–0.6). These findings are consistent with prior studies of primarily self-help based online interventions for PTSD (e.g., Hirai & Clum, 2005; Spence et al., 2014; Wang et al., 2013). Thus, these findings provide further support for the efficacy of online self-help for many individuals with PTSD, particularly when combined with some form of therapist support as in the current trial, where participants received regular check in calls from a graduate student clinician. Overall, results suggest that the combination of brief regular support from a trained clinician combined with psycho-education about the impact of rape and PTSD along with provision of information about adaptive coping and distress management strategies may be an efficacious treatment option for many individuals.
Initial comparisons of the efficacy of these two interventions supported that the programs were equally efficacious at reducing symptoms of PTSD, depression, and general anxiety. Moderator analyses suggested superiority of the psycho-educational website at reducing symptoms of PTSD among individuals with lower levels of pre-treatment PTSD symptomology and superiority of the interactive program for individuals with higher levels of pre-treatment PTSD symptomology. If replicated, this finding has implications for treatment intensity matching for PTSD. For individuals with low to moderate levels of PTSD symptomology, online self-help interventions combined with therapist support may be most likely to lead to positive outcomes, whereas individuals with more severe symptomology may require more intensive therapist-facilitated interventions. Indeed, supporting the feasibility and efficacy of such a treatment matching protocol, while not involving randomization, a prior study matched youth with low levels of PTSD symptoms after the September 11th terrorist attacks to a brief CBT skills intervention and youth with more significant symptomology to a trauma-specific CBT intervention, and achieved comparable outcomes for both groups (CATS Consortium, 2010).
Findings of the present study must be placed within the context of the study’s strengths and limitations. First, participants consisted of college women who overall had high levels of computer literacy as well as comfort with the asynchronous communication format utilized in the current trial. Future trials with populations that vary in their level of computer literacy and comfort with asynchronous communication is necessary to determine if these aspects of the intervention may represent barriers for some individuals. An additional limitation involves the format of the psycho-educational website, which consisted of identical content (without multimedia or interactive features) of phase one of the interactive program. As approximately one third of women assigned to the interactive program only completed phase one of the intervention, differences between the two intervention conditions were less marked for many participants, perhaps in part explaining the fairly equivalent outcomes across the two programs. Also, as previously mentioned, like in many other trials of online intervention, the majority of participants did not complete the entire interactive online program. While in many cases this may have been because they were already experiencing clinical benefit (indeed, number of program modules completed was uncorrelated with post-treatment PTSD, r = −.09), the extent to which completing additional program modules may have further improved outcomes is not known. Additionally, given the nature of the trial, individuals completing pre-, post- and follow-up assessments were not blind to participants’ intervention condition. Finally, while attempts were made to obtain data from individuals who dropped out of the interactive program, only two of seven treatment drop-outs completed the post-treatment assessment. It also should be noted that overall only 72.6% of individuals who initiated one of the two programs completed the post-treatment assessment, and thus it is not known whether these individuals who did not complete the assessment experienced clinical benefit.
Bearing these limitations in mind, results provide support for the efficacy of tailored cognitive-behaviorally oriented online interventions for rape-related PTSD presented in either a self-help or therapist-facilitated format. Future trials are necessary to evaluate the efficacy and effectiveness of such interventions when delivered to more diverse populations and when delivered in multiple practice settings (e.g., college counseling centers, VA outpatient clinics, sexual assault resource centers). Additionally, future research is necessary to determine which individuals are most likely to benefit from a self-help or therapist-facilitated format, including utilizing a treatment matching protocol. Finally, future research should focus on strategies to increase engagement in online treatments, as well as to determine the necessary effective treatment dose for different groups of individuals. Work in these areas is necessary in order to develop beneficial, therapist-resource efficient online interventions for PTSD.
Figure 1.
Participant flow
Highlights.
The From Survivor to Thriver program is an online program for rape-related PTSD
The efficacy of the program was compared to online self-help for rape-related PTSD
Both programs led to large, maintained reductions in PTSD, depression, and anxiety
The interactive program led to superior outcomes for those with more severe PTSD
Acknowledgments
Redacted for review.
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
This research was supported by funding from the National Institute of Mental Health, under grant number 1R34MH085118.
Research data derived from an approved East Carolina University IRB protocol # UMCIRB 09-0553.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Heather Littleton, Email: littletonh@ecu.edu.
Amie E. Grills, Email: agrills@bu.edu.
Katherine D. Kline, Email: katherine.d.kline2.mil@mail.mil.
Alexander M. Schoemann, Email: schoemanna@ecu.edu.
Julia C. Dodd, Email: fondrenj10@students.ecu.edu.
References
- Ahrens CE, Campbell R, Ternier-Thames NK, Wasco SM, Sefl T. Deciding whom to tell: Expectations and outcomes of rape survivors’ first disclosures. Psychology of Women Quarterly. 2007;31:38–49. [Google Scholar]
- Author Citation. 2012 [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal ideation: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Scale for Suicide Ideation Manual. San Antonio: Harcourt Brace; 1993. [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, Buckley TC. A controlled evaluation of cognitive behavioral therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Boudreaux E, Kilpatrick DG, Resnick HS, Best CL, Saunders B. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. Journal of Traumatic Stress. 1998;11:665–678. doi: 10.1023/A:1024437215004. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Busseri MA, Tyler JD. Interchangeability of the Working Alliance Inventory and Working Alliance Inventory, Short Form. Psychological Assessment. 2003;15:193–197. doi: 10.1037/1040-3590.15.2.193. [DOI] [PubMed] [Google Scholar]
- Bystritsky A, Linn LS, Ware JE. Development of a multidimensional scale of anxiety. Journal of Anxiety Disorders. 1990;4:99–115. [Google Scholar]
- CATS Consortium. Implementation of CBT for youth affected by the World Trade Center disaster: Matching need treatment intensity and reducing trauma symptoms. Journal of Traumatic Stress. 2010;23:699–707. doi: 10.1002/jts.20594. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Gudmundsdottir B, Beck JG, Palyo SA, Miller L. Screening for PTSD in motor vehicle accident survivors using the PSS-SR and IES. Journal of Traumatic Stress. 2006;19:119–128. doi: 10.1002/jts.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeon G, Melnick G, Cleland C. Client matching: A severity-treatment intensity paradigm. Journal of Addictive Diseases. 2008;27:99–113. doi: 10.1080/10550880802122703. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Spence SH. The relative efficacy and treatment distress of EMDR and a cognitive-behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders. 1999;13:131–157. doi: 10.1016/s0887-6185(98)00044-9. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID I/P) New York: Biometrics Research; 2002. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Molnar C, Cashman L. Change in rape narratives during exposure therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 1995;8:675–690. doi: 10.1007/BF02102894. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M. The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behavior Therapy. 1995;26:487–499. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: General issues and preliminary findings for the Stressful Life Events Screening Questionnaire. Journal of Traumatic Stress. 1998;11:521–542. doi: 10.1023/A:1024456713321. [DOI] [PubMed] [Google Scholar]
- Hammond GC, Croudace TJ, Radhakrishnan M, Lafortune L, Watson A, McMillan-Shields F, Jones PB. Comparative effectiveness of cognitive therapies delivered face-to-face or over the telephone: An observational study using propensity methods. PLoS ONE. 2012;7:e42916. doi: 10.1371/journal.pone.0042916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Brodsky R, Johnston MF, Spritzer KL, Hui K-K. Evaluating the statistical significance of health-related quality-of-life change in individual patients. Evaluation & the Health Professions. 2005;28:160–171. doi: 10.1177/0163278705275339. [DOI] [PubMed] [Google Scholar]
- Hirai M, Clum GA. An internet-based self-change program for traumatic event related fear, distress, and maladaptive coping. Journal of Traumatic Stress. 2005;18:631–636. doi: 10.1002/jts.20071. [DOI] [PubMed] [Google Scholar]
- Holi MM, Pelkonen M, Karlsson L, Kiviruusu O, Ruuttu T, Heilä H, Marttunen M. Psychometric properties and clinical utility of the Scale for Suicidal Ideation (SSI) in adolescents. BMC Psychiatry. 2005;5:8. doi: 10.1186/1471-244X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horgan A, Sweeney J. Young students’ use of the Internet for mental health information and support. Journal of Psychiatric and Mental Health Nursing. 2010;17:117–123. doi: 10.1111/j.1365-2850.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Ironson G, Freund B, Strauss JL, Williams J. Comparison of two treatments for traumatic stress: A community-based study of EMDR and prolonged exposure. Journal of Clinical Psychology. 2002;58:113–128. doi: 10.1002/jclp.1132. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Foa EB, Morral AR. Influence of emotional engagement and habituation on exposure therapy for PTSD. Journal of Consulting and Clinical Psychology. 1998;66:185–192. doi: 10.1037//0022-006x.66.1.185. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Study. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klein B, Mitchell J, Abbott J, Shandley K, Austin D, Gilson G, Redman T. A therapist-assisted cognitive behavior therapy internet intervention for posttraumatic stress disorder: Pre-, post-, and 3-month follow-up results from an open trial. Journal of Anxiety Disorders. 2010;24:635–644. doi: 10.1016/j.janxdis.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates development of a strong therapeutic alliance: A randomized controlled clinical trial. BMC Psychiatry. 2007;7:13. doi: 10.1186/1471-244X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Abbey A, Campbell R, Cook S, Norris J, Testa M, White J. Revising the SES: A collaborative process to improve assessment of sexual aggression and victimization. Psychology of Women Quarterly. 2007;31:357–370. [Google Scholar]
- Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PMG. Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the Internet. Journal of Consulting and Clinical Psychology. 2003;71:901–909. doi: 10.1037/0022-006X.71.5.901. [DOI] [PubMed] [Google Scholar]
- Lange A, Schrieken B, van de Ven JP, Bredeweg B, Emmelkamp PMG, van der Kolk J, Reuvers A. “Interapy”: The effects of a short protocolled treatment of posttraumatic stress and pathological grief through the Internet. Behavioral and Cognitive Psychotherapy. 2000;28:175–192. [Google Scholar]
- Leibert T, Archer J, Jr, Munson J, York G. An exploratory study of client perceptions of Internet counseling and the therapeutic alliance. Journal of Mental Health Counseling. 2006;28:69–83. [Google Scholar]
- Leiner AS, Kearns MC, Jackson JL, Astin MC, Rothbaum BO. Avoidant coping and treatment outcome in rape-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2012;80:317–321. doi: 10.1037/a0026814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD. Longitudinal Structural Equation Modeling. New York, NY: Guilford; 2013. [Google Scholar]
- Littleton HL, Axsom D, Breitkopf CR, Berenson AB. Rape acknowledgment and post assault behaviors: How acknowledgment status relates to disclosure, coping, worldview, and reactions received from others. Violence and Victims. 2006;21:765–782. [PubMed] [Google Scholar]
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry. 2007;164:1676–1683. doi: 10.1176/appi.ajp.2007.06122057. [DOI] [PubMed] [Google Scholar]
- Martin CS, Pollock NK, Bukstein OG, Lynch KG. Inter-rater reliability of the SCID alcohol and substance use disorders section among adolescents. Drug and Alcohol Dependence. 2000;59:173–176. doi: 10.1016/s0376-8716(99)00119-2. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Green AL. The Satisfaction with Therapy and Therapist Scale- Revised (STTS-R) for group psychotherapy: Psychometric properties and confirmatory factor analysis. Professional Psychology: Research and Practice. 2008;39:435–442. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47:737–743. doi: 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress. 2005;18:607–616. doi: 10.1002/jts.20069. [DOI] [PubMed] [Google Scholar]
- Shean G, Baldwin G. Sensitivity and specificity of depression questionnaires in a college-age sample. Journal of Genetic Psychology. 2008;169:281–288. doi: 10.3200/GNTP.169.3.281-292. [DOI] [PubMed] [Google Scholar]
- Smith A, Rainie L, Zickuhr K. College students and technology. 2011 Jul 19; Retrieved from http://www.pewinternet.org/2011/07/19/college-students-and-technology/
- Spence J, Titov N, Johnson L, Jones MP, Dear BF, Solley K. Internet-based trauma-focused cognitive behavioural therapy for PTSD with and without exposure components: A randomised controlled trial. Journal of Affective Disorders. 2014;162:73–80. doi: 10.1016/j.jad.2014.03.009. [DOI] [PubMed] [Google Scholar]
- Stoessel PW, Bystritsky A, Pasnau RO. Screening for anxiety disorders in the primary care setting. Family Practice. 1995;12:448–451. doi: 10.1093/fampra/12.4.448. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment. 1989;1:207–210. [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations. Journal of Statistical Software. 2011;45:1–67. [Google Scholar]
- Van Minnen A, Arntz A, Keijsers G. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy. 2002;40:439–457. doi: 10.1016/s0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Van Minnen A, Foa EB. The effect of imaginal exposure length on outcome of treatment for PTSD. Journal of Traumatic Stress. 2006;19:427–438. doi: 10.1002/jts.20146. [DOI] [PubMed] [Google Scholar]
- Walsh W, Banyard VL, Moynihan MM, Ward S, Cohn ES. Disclosure and service use on a college campus after an unwanted sexual experience. Journal of Trauma & Dissociation. 2010;11:134–151. doi: 10.1080/15299730903502912. [DOI] [PubMed] [Google Scholar]
- Wang Z, Wang J, Maercker A. Chinese My Trauma Recovery, a Web-based intervention for traumatized persons in two parallel samples: Randomized controlled trial. Journal of Medical Internet Research. 2013;15:e213. doi: 10.2196/jmir.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Shalomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Gunderson JG. The Collaborative Longitudinal Personality Disorders Study: Reliability of Axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley J, Amstadter AB, Ruggerio KJ, Kilpatrick DG. Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a national survey of women. Social Psychiatry and Psychiatric Epidemiology. 2012;47:893–902. doi: 10.1007/s00127-011-0397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Fitzgibbons LA, Foa EB. Response of African American and Caucasian women to cognitive behavioral therapy for PTSD. Behavior Therapy. 1999;30:581–595. [Google Scholar]