Abstract
Every patient is embedded in a social network of interpersonal connections that influence health outcomes. Neurologists routinely need to engage with a patient’s family and friends due to the nature of the illness and its social sequelae. Social isolation is a potent determinant of poor health and neurobiological changes, and its effects can be comparable to those of traditional risk factors. It would seem reasonable, therefore, to map and follow the personal networks of neurology patients. This approach reveals influential people, their habits, and linkage patterns that could facilitate or limit health behaviours. Personal network information can be particularly valuable to enhance risk factor management, medication adherence, and functional recovery. Here, we propose an agenda for research and clinical practice that includes mapping the networks of patients with diverse neurological disorders, evaluating the impact of the networks on patient outcomes, and testing network interventions.
Sometimes, if you want to change a man’s mind, you have to change the mind of the man next to him first. Megan Whalen Turner, The King of Attolia1.
Focus on the individual is common in the clinic and in research studies. From the earliest stages of training, students are taught to see the patient as a solitary figure. Clinical practice, however, reveals that this is an inaccurate model, as every patient is embedded in a complex and diverse social system. A physician’s interaction with this social network is routine, implicit, and necessary. In neurology, an appreciation of patients’ social networks is especially important, as the nature of the injury or illness requires engagement with families and friends, sometimes to the exclusion of the patient. Systematic study of the social system’s constitution and natural evolution after disease, and its engagement for therapeutic purposes, is an important unmet need, particularly for neurological disorders.
Robust epidemiological studies conducted over three decades have shown that social structures influence health2–4. Social isolation and the perception of isolation, known commonly as loneliness, is as potent a determinant of poor health as smoking, elevated blood pressure, high cholesterol, and physical inactivity5–8. In cerebrovascular disease, social isolation has been linked to an increased risk of incident stroke9,10, and to poorer outcomes after stroke11–13. Conversely, an extensive social network is protective against dementia14,15, possibly by mitigating the effects of pathology on cognitive function16. In current practice, however, the social life of a patient is barely screened and rarely commented on in a neurologist’s final recommendations to the patient.
The interplay between social life and brain anatomy, physiology and biology is important. Neocortical volume co-varies with social group sizes in nonhuman primates and, possibly, humans17. This pattern suggests that social life is a primary evolutionary driver of neocortical enlargement across species17–20. Language itself might have evolved as a vehicle to facilitate social demands17. Pathologically, the socially isolated brain has been shown to have higher baseline vascular resistance, lower inflammatory control, and decreased neurogenesis after injury21–23. These effects of social isolation on the brain are accompanied by a host of systemic physiological changes, including an elevated stress response, inflammation, and hypertension24.
This article lays out a framework for understanding the local social structure around a patient. It explains the concepts and terms used in network research, outlines methods to elicit and analyse data, and proposes an agenda for research and clinical applications of network science.
Personal networks
Personal networks, also called egocentric networks, describe the relations of a set of individuals — the alters — around a focal individual — an ego. In accordance with the principles of graph theory, all individuals in the network are nodes, and their relations, which can be defined by emotional closeness, contact frequency or physical distance, are the ties that link the nodes (FIG. 1). Personal networks differ from whole networks, also known as sociocentric networks, which focus on patterns of relationships in a bounded group without a prespecified central node25. Personal networks are also distinct from social support studies, which focus on the quality and absolute number of a person’s social ties. By contrast, personal networks concentrate on a fuller view of the structure of the network, its components, and the types of ties26.
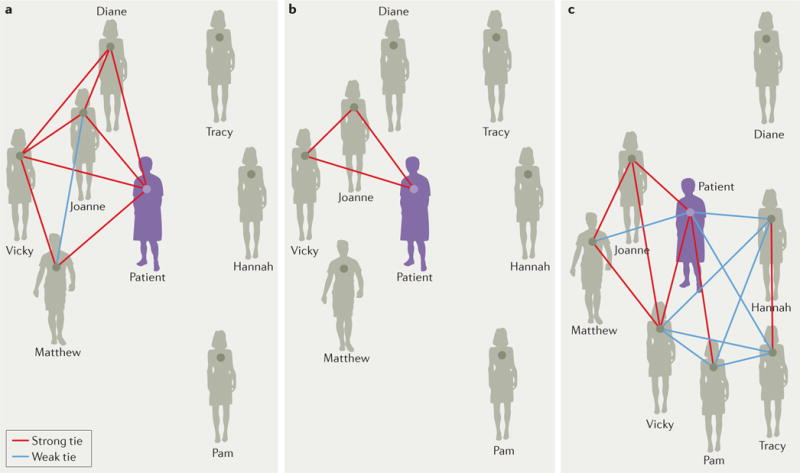
Figure 1. The personal network of a patient.
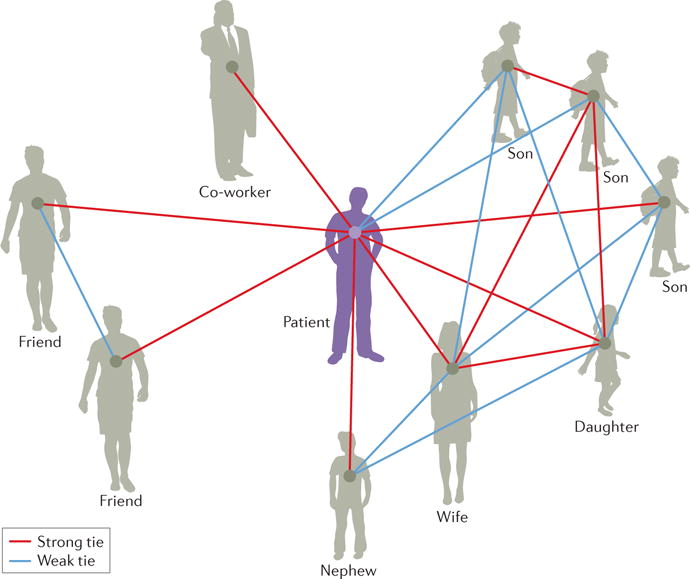
The ego (that is, the patient) is connected to members of his personal network, known as alters, by either a strong or a weak tie. In this figure, the personal network of the patient includes subgroups of family members, friends and a co-worker. By evaluating the architecture and composition of relationships among network members, neurologists might be able to identify patients who are at risk of poor outcomes.
Personal networks operationalize the social context into quantitative variables, thereby enabling evaluation of the social capital available to the individual in the form of social resources, cohesion, and brokering opportunities27,28. Examples of personal networks include individuals consulted when a person seeks a new job, or the social circle around a new immigrant. Research shows that the characteristics of alters and their relationships with each other influence the ego’s behaviour, performance, and adaptation to life events27. For example, perhaps counter-intuitively, an ego with weaker ties to alters who are strangers to one another is more likely to get a job, probably because unconnected alters provide novel information and contact to useful parties outside the ego’s typical social circle29. Similarly, individuals who assimilate into society after immigration have a tendency to maintain friendship groups of varying demographics earlier in life30. Delineation of the characteristics of such networks, in terms of face-to-face interaction versus contact mediated through technology and social media, is an active area of research20.
In terms of health, connected individuals often display interdependent well-being, which has been attributed to a variety of mechanisms31 (FIG. 2). This principle is best demonstrated in the context of marriage, where the illness and death of a spouse can shorten the lifespan of a caregiving partner — the so-called bereavement effect32. The illness and, ultimately, death of the spouse is thought to impose stress and deprive the caregiver of a supportive tie33 The bereavement effect is particularly pronounced when the spouse has a condition such as stroke, dementia or critical illness that can compromise physical or mental abilities. Caregiving partners in this scenario have among the highest hazard ratios for depression and mortality32,34. For the patient, having more friends beyond the caregiver is associated with health improvements and, complementarily, healthiness is associated with closer relationships among all people in the network35. As mentioned earlier, a deficient personal network for the patient portends poorer recovery from stroke, worse trajectories after dementia, and a higher risk of mortality and morbidity in general9–16. Therefore, personal network mapping could identify at-risk patients and caregivers, while also providing a means for potential intervention.
Figure 2. Social network mechanisms that influence health behaviour.
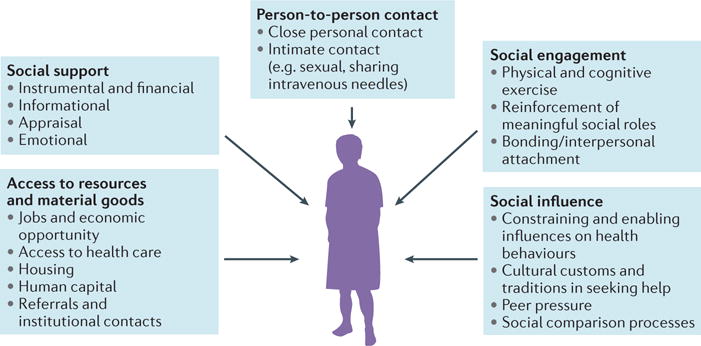
Networks affect behaviour through at least five pathways; person to person contact, social engagement, social influence, access to resources and material goods, and social support31. Social support comes in four forms; instrumental and financial support, informational support, appraisal support and emotional support. Appraisal support relates to how an alter can provide an ego with appropriate feedback or help with decision making. The influence of a pathway on the ego–alter relationship can change over time. Some ties operate through several pathways, while others are more specialized. The ego is the patient at the centre of the network, an alter is an individual in a network, and a tie is the connection between individuals in a network.
A survey is the standard instrument for the generation of data regarding personal networks, although derivation of nodes and ties from existing phone, email or Internet sources is also possible36. Typically, the survey has three components: name generator, name inter-relater, and name interpreter (TABLE 1). The name generator is a set of questions designed to identify the nodes in the network. The example questions listed in TABLE 1 are adapted from validated questions that are used in the General Social Survey, a population-based sociological survey conducted annually in the USA37. For sample sizes of up to 250, we recommend not capping the total number of individuals named. By following this protocol, researchers can avoid a ceiling effect in data gathering. The name inter-relater questions aim to elicit the tie pattern and strength among the named individuals. These are the critical data that distinguish network structure studies from social support surveys, which typically stop at the quantity and quality of relationships rather than the structure26,27. Finally, name interpreter questions generate data on the individual characteristics of each alter. Here, questions about health behaviour are asked with a view to understanding the local health environment and possible social influences acting on the ego. To avoid survey fatigue in patients, we only collect name inter-relater and name interpreter data for the first ten individuals named by the ego.
Table 1.
| Survey section | Example questions |
|---|---|
| Name generator | 1. From time to time, most people discuss important personal matters with other people. Looking back over the past 3 months, who are the adults with whom you discussed an important personal matter? 2. From time to time, people socialize with other people. For instance, they visit each other, go together on a trip or to dinner. In the past 3 months, who are the adults with whom you usually do these things? 3. In the past 3 months, who supported you most often? |
| Name inter-relater | 1. Compared with the others you mentioned, do you feel especially close to[Name 1]? 2. I will now focus on the relationships between each pair of people you mentioned. For example, I will ask about [Name 1] and [Name 2]. For each pair, I will ask whether they are total strangers, especially close, or in between. By total strangers, I mean that they wouldn’t recognize one another if they met on the street. By especially close, I mean as close to each other as they are to you. By in between, I mean all other relationships. Is [Name 1] a total stranger, especially close, or in between with [Name 2]? (Repeat for each name pairing) |
| Name interpreter | 1. Is [Name 1] a man or woman? 2. Does [Name 1] have a negative influence on your health? For example does he or she passively or actively encourage you to smoke, not eat well, or not exercise? 3. How is [Name 1] connected to you? Options include spouse, parent, sibling, child, other family, co-worker, co-member in organization, neighbour, friend, advisor, or other. You can choose more than one. 4. Has [Name 1] done any of the following to try and improve his or her health in the past 3 months?
|
Analysis of personal networks
The analysis of personal networks is divided into composition analysis, which examines the range of characteristics of people around the patient, and structure analysis, which examines the organization of ties and their patterns in graph theoretical terms.
For composition analysis, consider two people who have experienced a stroke (FIG. 3). They are of similar age and stroke severity — the two strongest predictors of functional outcome38. However, the make-up of their social networks differs. Patient 1 (FIG. 3a) has a network composed totally of kin who are the same race and differing gender, and have similar non-healthy behaviours. Patient 2 (FIG. 3b) has a network composed of a mixture of kin and non-kin who are the same gender and race, and have similar healthy behaviours. An open question is whether these two patients will have different outcomes at 6 months that might be partly explained by the differences in their networks. Measures of composition include the standard deviation of the alters’ ages, the proportion of kin, the diversity of gender index, the diversity of race index, and the proportions of individuals who engage in healthy and unhealthy behaviours. In these measures, the amount of variation — or heterogeneity — in the variables is important to understand the range of diversity around the patient39.
Figure 3. Personal network composition for two patients with stroke.
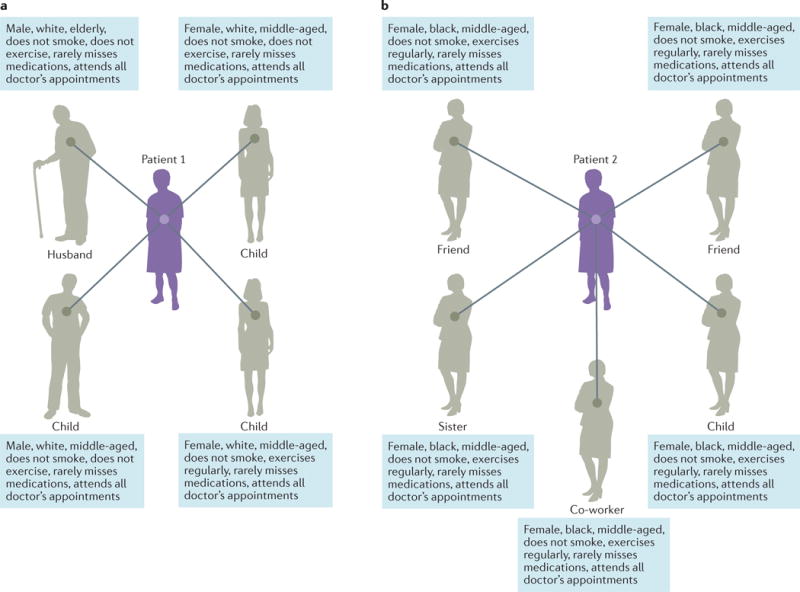
The composition of a network includes information about alters and their habits, such as diet and the frequency of exercise. a | Patient 1 has a kin-based network with pervasive unhealthy habits. b | Patient 2’s network is mixed with kin and non-kin who are the same gender and race with healthy habits.
The structural analysis of personal networks involves graph theoretical measurements. The researcher usually begins by measuring network size, which is the total number of nodes excluding the ego. The second step is to calculate network density. The density of personal networks is the extent to which alters are connected, and is calculated as the sum of ties divided by all possible ties excluding the ego:
where L is the number of observed ties, and N is the number of nodes40.
Certain network structural motifs offer constraints as well as opportunities for the ego. Both of these possibilities can be addressed by conducting a series of measurements under the theory of structural holes41. A structural hole is the absence of a connection between two alters. Although the hole can seem to be a weakness, it empirically affords an advantage to the ego, who is provided with an opportunity to connect or bridge the gap between the two parties. Bridging affords advantages such as diversity of information, non-overlapping resources and knowledge, and the opportunity to broker between the strangers42. In terms of health, bridging has been associated with increased wellness and longer life43. However, it also creates cognitive demands that might not be sustainable during illness43.
To measure structural holes and bridging, constraint and effective size can be calculated. Constraint is a measure of the extent to which the ego’s alters have ties to each other. It is highest in a close-knit network of individuals who are familiar to each other, such as in a nuclear family. Mathematically, it is the sum of direct and indirect paths from the ego to every alter:
where i is the ego, q and j are alters, pij is the proportional strength of i’s relationship with j, piq is the proportional strength of i’s relationship with q, and pqj is the proportional strength of q’s relationship with j (REF. 44). In this calculation, ties can be weighted to account for strong and weak relationships as evaluated by the patient. In such cases, we set strong ties as 2, weak ties as 1, and no tie as 0 (REF. 44).
Effective size is the inverse of constraint and denotes the number of nonredundant nodes in the network:
where i is the ego, q and j are alters, and
measures the portion of i’s relationship with j that is redundant to i’s relationships with other primary contacts44. High effective size, which is usually accompanied by low constraint, indicates a network of unconnected individuals that has structural holes. Examples include networks centred on individuals who have located a new job quickly, or individuals engaged with groups in varying places such as work, church and school.
FIG. 4 shows the same patients presented in FIG. 3, but with tie information included. Both have relatively small networks. However, Patient 1’s (FIG. 4a) network is full of strong ties, creating a dense network with high constraint and low effective size, whereas Patient 2’s (FIG. 4b) network has more weak ties and individuals unknown to each other, resulting in a less dense network with lower constraint and higher effective size. This latter network structure might afford Patient 2 with opportunities to access differing social resources, engage in various social contexts, and receive novel advice.
Figure 4. Personal network structure for two patients with stroke.
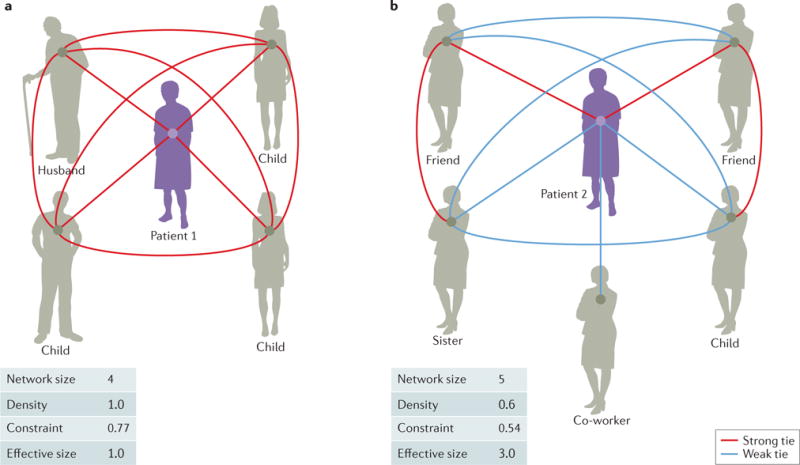
The structure of a network is the organization of ties and their patterns in quantitative terms. Patients who are at risk of poor outcomes are typically surrounded by a small number of close-knit alters. a | Patient 1 has a high-constraint network in which all members are closely knit together. b | Patient 2 has a low-constraint network that includes unconnected individuals and structural holes.
The analysis of personal networks is facilitated by computer software in statistical packages such as R, UCINET, Pajek, and E-Net (REF. 25). Important additional study includes qualitative and longitudinal analyses, which allow investigation of mechanisms and explanations for the patterns observed. Posing open-ended questions to the patient about his or her relationships and their evolution during illness often elicits rich information. These types of questions can inform mechanistic hypotheses about social influence, access to resources and goods, and social support. For example, friendship ties for young adults might be a source of multidimensional support or no support at all. To fully elucidate the meaning of ties, and to understand the consequences of their changes on an ego, qualitative data are needed45. Furthermore, structural assessments over time reveal important information on network dynamics and adaptation to disease states46. For instance, research in older adults suggests that individuals who gain confidants over time report better functional and psychological health, whereas loss of network ties is associated with functional — but not psychological — decline47. In the context of neurological illness, assessing the development of a patient’s personal network over time can provide insight into which patients are at risk of poor health outcomes. One such example from the clinic is presented in BOX 1 and Supplementary information S1 (video), which depict the evolving social network of a patient with stroke, from onset to 6 months.
Box 1. Network dynamics during stroke recovery.
A 48-year-old married woman, who worked as a chef, had a brainstem stroke with moderate deficits (NIH Stroke Scale score = 5). Her personal network at the time of stroke is shown in panel a, and included four individuals, most of whom knew each other. Three of the four were family members. At 3 months (panel b), her network had shrunk to two family members. She scored poorly on patient-reported recovery outcomes, and showed increased levels of depression. At 6 months (panel c), her network had increased to six individuals, including three reacquainted friends. Her patient-reported recovery outcomes improved. She reported purposely seeking new friends to avoid being “stuck at home.” She and Vicky also simultaneously gave up smoking. Supplementary information S1 (video) shows the evolution of the network dynamics over time. Written consent for publication was obtained from the patient described in this case report.
Applications in neurology
Core issues of medical care, including but not limited to risk factor management, medication adherence, health education, and physical and cognitive rehabilitation, involve social networks. Engagement — or, at least, awareness — of the behaviours of key members in a network enhances counselling conversations about everyday activities such as diet, smoking habits, and exercise.
To advance network science in neurology, at least four research priorities need to be addressed. The first step is to establish baseline network characteristics and their longitudinal changes in patients with common neurological disorders such as stroke, headache, seizure disorders, dementia, or movement disorders. This step requires establishment of a set of network instruments that are applicable to neurological patients. The second step is to determine which aspects of network structure and composition are associated with neurological outcomes. Outcomes can be in the form of patient-reported measures, such as the Patient Reported Outcomes Measurement Information System (PROMIS), and traditional functional outcome measures, such as the modified Rankin Scale. The third step is to identify the most important social and biological mechanisms through which social networks act. These mechanisms could include social influence, information spread, social support, and neurophysiological, neuroanatomical and inflammatory changes. The fourth and final step is to test promising network interventions against usual care in prospective and randomized studies.
An example of social network research in neurology is our work on the impact of patients’ social networks on timing of hospital arrival after acute ischaemic stroke48. We examined the personal social networks of fast (<6 h) and slow (>6 h) responders, building on prior literature which showed that being unmarried and living alone were risk factors for delay49,50. Our preliminary analysis revealed that patients who arrived later had close-knit networks, that is, smaller networks with higher constraint. The underlying mechanisms included over-reliance on strong ties, such as those between family members, who might downplay symptoms, and lack of contact with weak ties, for example, a friend who is a nurse, who can advise on the appropriate course of action. The finding is consistent with extensive literature on the strength of weak ties29. Further work in this area could lead to stroke education that is tailored to patients’ personal network characteristics.
One of ultimate goals for network science in neurology is to build and deploy evidence-based network interventions for neurological patients in clinical settings. A network intervention is the use of social network data to accelerate behavioural change51. Though not deliberately monitoring personal networks, Alcoholics Anonymous is one example of an intervention that changes personal networks by adding nodes and rewiring existing ties52. Also in the addiction context, ‘network therapy’ is a form of cognitive behavioural therapy that aims to employ the core network of family members and friends to support adherence to treatment53. Such strategies have been shown to improve the effectiveness of maintenance therapy for heroin addiction54. The Treatment and Prevention Study (TAPS) is a promising randomized controlled trial currently recruiting intravenous drug users. It tests the effectiveness of a ‘bring your friends’ personal network approach to reduce the incidence of hepatitis C infection55,56. Prior studies show that treating all members of the personal network is the most effective way to clear a communicable infection in the population. The personal network approach outperformed selective targeting of nodes with the most ties56.
In the neurology office, we hope that the promising data presented by network studies will compel clinicians to incorporate a network lens when recording the social history of a patient. By reimagining the patient as a social being embedded in an interpersonal web of relations that constrain and facilitate health-related behaviours, we can obtain valuable information. For example, by asking the ego a set of questions aimed at unravelling relationships in the network, we might identify patients who are at risk of poor outcomes. Questions could include: who do you discuss important matters with? Who do you socialize with regularly? Who supports you on a regular basis? Are these individuals as close to each other as they are to you? Patients who are at risk are typically surrounded by a small number of close-knit alters. Identifying at-risk individuals is the first step to implementing an effective behavioural change intervention.
Once patients with at-risk networks are identified, therapeutic network interventions can be tried. Initial strategies include recruitment of driver nodes, that is, individuals who hold particular sway regarding dietary and lifestyle behaviours in the network. Such an individual might not be the spouse, but, rather, a close friend or family member who holds a structurally pivotal position. Influential people in a network can be recruited to champion important and difficult behavioural changes. Secondly, network components that are, for example, tightly bound clusters in the networks can be targeted for team interventions, such as full-group smoking cessation or exercise programmes. Additionally, social expansion — a deliberate attempt to increase personal network size — can be tried for patients with small networks. Increasing the size of an individual’s personal network can extend the typical support group model and improve patient outcomes in both psychosocial domains — such as the severity of depression — and biological domains — such as the level of hypertension or the degree of inflammation.
Limitations of network models
As a middle-level theory, personal network approaches have limitations in both the individual and broader social–historical dimensions57. By definition, the network perspective reduces the emphasis on individual agency, defined as the view that an individual decides and acts independently regardless of context. Social networks are also an insufficient model for broader social and historical forces, such as poverty or racism. To address such factors, a combination of quantitative (epidemiological) and qualitative (ethnographic) analysis at the community and population level is needed. Networks also privilege human actors over technologies, animals and inanimate objects that can also have an impact on health. Realistically, some of these forces are beyond the purview and influence of an individual neurologist, and are probably more relevant to psychological, public health and policy strategies. Finally, more research is needed on the creation and execution of network interventions in clinical populations. Due to these blind spots in personal network approaches, we advise that a network lens should be used in combination with traditional clinical and epidemiological approaches.
Conclusions
Rethinking the patient as a person embedded in a social web is important in neurological contexts. Social networks influence health, they can be mapped in research and clinical contexts, and they can be utilized for therapeutic purposes. The network approach shows promise to improve understanding of health behaviours and create sustainable change in patients’ lives. Future research to foster this vision includes robust measurement of networks in neurological patients, association of networks to patient outcomes, establishing the role of social mechanisms in disease and recovery, and building evidence-based network interventions.
Supplementary Material
Acknowledgments
We thank Selena Lee for producing the network video supplement. We also gratefully acknowledge all the patients who contributed to the research contained within the manuscript.
Glossary
- Diversity of gender index
The amount of gender variation in the network, ranging from zero, where all members are the same gender, to one, where there are equal numbers across all gender categories
- Diversity of race index
The amount of racial variation in the network, ranging from zero, where all members are the same race, to one, where there are equal numbers across all racial categories
Footnotes
Author contributions
All authors researched data for the article and contributed equally to discussions of the content. All authors wrote the article and reviewed and/or edited the manuscript before submission.
Competing interests
The authors declare no competing interests.
Contributor Information
Amar Dhand, Department of Neurology, Brigham and Women’s Hospital, Harvard Medical School, 45 Francis Street and at the Network Science Institute, Northeastern University, 177 Huntington Avenue, 11th Floor, Boston, Massachusetts 02115, USA.
Douglas A. Luke, Center for Public Health Systems Science, George Warren Brown School of Social Work, Washington University in St. Louis, Campus BOX 1196, One Brookings Drive, St. Louis, Missouri 63130, USA
Catherine E. Lang, Program in Physical Therapy, Washington University School of Medicine, Campus Box 8502, 4444 Forest Park Avenue, Suite 1101, St. Louis, Missouri 63110, USA
Jin-Moo Lee, Department of Neurology, Washington University School of Medicine, Campus Box 8111, 660 South Euclid Avenue, St. Louis, Missouri 63110, USA.
References
- 1.Turner MW. The King of Attolia. Harper Collins; 2009. [Google Scholar]
- 2.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 3.Seeman TE, Kaplan GA, Knudsen L, Cohen R, Guralnik J. Social network ties and mortality among the elderly in the Alameda County Study. Am J Epidemiol. 1987;126:714–723. doi: 10.1093/oxfordjournals.aje.a114711. [DOI] [PubMed] [Google Scholar]
- 4.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pantell M, et al. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103:2056–2062. doi: 10.2105/AJPH.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rico-Uribe LA, et al. Loneliness, social networks, and health: a cross-sectional study in three countries. PLoS ONE. 2016;11:e0145264. doi: 10.1371/journal.pone.0145264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nagayoshi M, et al. Social network, social support, and risk of incident stroke: atherosclerosis risk in communities study. Stroke. 2014;45:2868–2873. doi: 10.1161/STROKEAHA.114.005815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rutledge T, et al. Social networks and incident stroke among women with suspected myocardial ischemia. Psychosom Med. 2008;70:282–287. doi: 10.1097/PSY.0b013e3181656e09. [DOI] [PubMed] [Google Scholar]
- 11.Boden-Albala B, Litwak E, Elkind MS, Rundek T, Sacco RL. Social isolation and outcomes post stroke. Neurology. 2005;64:1888–1892. doi: 10.1212/01.WNL.0000163510.79351.AF. [DOI] [PubMed] [Google Scholar]
- 12.Kotila M, Waltimo O, Niemi ML, Laaksonen R, Lempinen M. The profile of recovery from stroke and factors influencing outcome. Stroke. 1984;15:1039–1044. doi: 10.1161/01.str.15.6.1039. [DOI] [PubMed] [Google Scholar]
- 13.Glymour MM, Weuve J, Fay ME, Glass TA, Berkman LF. Social ties and cognitive recovery after stroke: does social integration promote cognitive resilience? Neuroepidemiology. 2008;31:10–20. doi: 10.1159/000136646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355:1315–1319. doi: 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]
- 15.Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–353. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- 16.Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS. The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol. 2006;5:406–412. doi: 10.1016/S1474-4422(06)70417-3. [DOI] [PubMed] [Google Scholar]
- 17.Dunbar RI. Coevolution of neocortical size, group size and language in humans. Behav Brain Sci. 1993;16:681–694. [Google Scholar]
- 18.Dunbar RI, Spoors M. Social networks, support cliques, and kinship. Hum Nat. 1995;6:273–290. doi: 10.1007/BF02734142. [DOI] [PubMed] [Google Scholar]
- 19.Heide Von, Der R, Vyas G, Olson IR. The social network-network: size is predicted by brain structure and function in the amygdala and paralimbic regions. Soc Cogn Affect Neurosci. 2014;9:1962–1972. doi: 10.1093/scan/nsu009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunbar R. Do online social media cut through the constraints that limit the size of offline social networks? R Soc Open Sci. 2016;3:150292. doi: 10.1098/rsos.150292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychol Bull. 2014;140:1464–1504. doi: 10.1037/a0037618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Venna VR, Xu Y, Doran SJ, Patrizz A, McCullough LD. Social interaction plays a critical role in neurogenesis and recovery after stroke. Transl Psychiatry. 2014;4:e351. doi: 10.1038/tp.2013.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Venna VR, McCullough LD. Role of social factors on cell death, cerebral plasticity and recovery after stroke. Metab Brain Dis. 2015;30:497–506. doi: 10.1007/s11011-014-9544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang YC, et al. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci USA. 2016;19:578–583. doi: 10.1073/pnas.1511085112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borgatti SP, Everett MG, Johnson JC. Analyzing Social Networks. SAGE; 2013. [Google Scholar]
- 26.Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol. 2008;34:405–429. [Google Scholar]
- 27.Crossley N, et al. Social Network Analysis for Ego-Nets. SAGE; 2015. [Google Scholar]
- 28.Nin N. Social capital A Theory Of Social Structure And Actions. Cambridge Univ. Press; 2001. [Google Scholar]
- 29.Granovetter MS. The strength of weak ties. AJS. 1973;78:1360–1380. [Google Scholar]
- 30.Lubbers MJ, Molina JL, McCarty C. Personal networks and ethnic identifications: the case of migrants in Spain. Int Sociol. 2007;22:721–741. [Google Scholar]
- 31.Berkman LF, Glass TA, Brissette I, Seeman TE. From social integration to health: durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 32.Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med. 2006;354:719–730. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- 33.Martikainen P, Valkonen T. Mortality after the death of a spouse: rates and causes of death in a large Finnish cohort. Am J Public Health. 1996;86:1087–1093. doi: 10.2105/ajph.86.8_pt_1.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cameron JI, et al. One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374:1831–1841. doi: 10.1056/NEJMoa1511160. [DOI] [PubMed] [Google Scholar]
- 35.O’Malley AJ, Arbesman S, Steiger DM, Fowler JH, Christakis NA. Egocentric social network structure, health, and pro-social behaviors in a national panel study of Americans. PLoS ONE. 2012;7:e36250. doi: 10.1371/journal.pone.0036250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eagle N, Pentland AS, Lazer D. Inferring friendship network structure by using mobile phone data. Proc Natl Acad Sci USA. 2009;106:15274–15278. doi: 10.1073/pnas.0900282106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burt RS. Network items and the general social survey. Soc Networks. 1984;6:293–339. [Google Scholar]
- 38.Rost NS, et al. Stroke severity is a crucial predictor of outcome: an international prospective validation study. J Am Heart Assoc. 2016;5:e002433. doi: 10.1161/JAHA.115.002433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agresti A, Agresti BF. Statistical analysis of qualitative variation. Sociol Methodol. 1978;9:204–237. [Google Scholar]
- 40.Wasserman S, Faust K. Social Network Analysis. Cambridge Univ. Press; 2009. [Google Scholar]
- 41.Burt RS. Structural holes and good ideas. AJS. 2004;110:349–399. [Google Scholar]
- 42.Stovel K, Shaw L. Brokerage. Annu Rev Sociol. 2012;38:139–158. [Google Scholar]
- 43.Cornwell B. Good health and the bridging of structural holes. Soc Networks. 2009;31:92–103. doi: 10.1016/j.socnet.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burt RS. Structural Holes. Harvard Univ. Press; 2009. [Google Scholar]
- 45.Bellotti E. What are friends for? Elective communities of single people. Soc Networks. 2008;30:318–329. [Google Scholar]
- 46.Barabási AL. The architecture of complexity. IEEE Control Syst Mag N Y. 2007;27:33–42. [Google Scholar]
- 47.Cornwell B, Laumann EO. The health benefits of network growth: new evidence from a national survey of older adults. Soc Sci Med. 2015;125:94–106. doi: 10.1016/j.socscimed.2013.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhand A, Luke D, Tsiaklides M, Lang C, Lee JM. S209. Social network characteristics influence timing of hospital arrival after acute ischemic stroke. Ann Neurol. 2016;78:S2. [Google Scholar]
- 49.Reeves MJ, Prager M, Fang J, Stamplecoski M, Kapral MK. Impact of living alone on the care and outcomes of patients with acute stroke. Stroke. 2014;45:3083–3085. doi: 10.1161/STROKEAHA.114.006520. [DOI] [PubMed] [Google Scholar]
- 50.Addo J, et al. Delay in presentation after an acute stroke in a multiethnic population in South London: the South London stroke register. J Am Heart Assoc. 2012;1:e001685. doi: 10.1161/JAHA.112.001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Valente TW. Network interventions. Science. 2012;337:49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 52.Galanter M. Alcoholics anonymous and twelve-step recovery: a model based on social and cognitive neuroscience. Am J Addict. 2014;23:300–307. doi: 10.1111/j.1521-0391.2014.12106.x. [DOI] [PubMed] [Google Scholar]
- 53.Galanter M. Network therapy for addiction: a model for office practice. Am J Psychiatry. 1993;150:28–36. doi: 10.1176/ajp.150.1.28. [DOI] [PubMed] [Google Scholar]
- 54.Galanter M, et al. Network therapy: decreased secondary opioid use during buprenorphine maintenance. J Subst Abuse Treat. 2004;26:313–318. doi: 10.1016/j.jsat.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 55.Hellard M, et al. Hepatitis C transmission and treatment as prevention - the role of the injecting network. Int J Drug Policy. 2015;26:958–962. doi: 10.1016/j.drugpo.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 56.Rolls DA, et al. Hepatitis C transmission and treatment in contact networks of people who inject drugs. PLoS ONE. 2013;8:e78286. doi: 10.1371/journal.pone.0078286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Emirbayer M, Goodwin J. Network analysis, culture, and the problem of agency. AJS. 1994;99:1411–1454. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


