Abstract
Context:
Glaucoma is the leading cause of global irreversible blindness. No recent study with adequate sample size has been carried out to estimate glaucoma prevalence in Eastern India.
Aims:
The aim of this study was to assess and compare the prevalence and types of glaucoma in a rural and urban East Indian population.
Settings and Design:
The Hooghly River Glaucoma Study (HRGS) is a population-based cross-sectional study from West Bengal. A tertiary hospital in Kolkata was our urban study center. Our rural study area included 28 contiguous villages from the district of Hooghly surrounding the rural base hospital located at Dhobapara in village Bakulia. Individuals aged 40 years and above were included in this study.
Subjects and Methods:
All subjects underwent a detailed ophthalmic examination at our base hospitals including applanation tonometry, ultrasound pachymetry, gonioscopy, and frequency doubling technology perimetry. Glaucoma was defined using modified International Society of Geographical and Epidemiological Ophthalmology criteria.
Statistical Analysis Used:
Analysis was performed using Chi-square test and multiple logistic regression using SPSS.
Results:
Totally, 14,092 individuals participated; 2.7% were detected to have glaucoma in rural arm and 3.23% in urban arm (P < 0.001). In urban population, 2.10% had primary open angle glaucoma (POAG), 0.97% had primary angle closure glaucoma (PACG), and 0.15% had secondary glaucoma. In rural population, 1.45% had POAG, 1.15% had ACG, and 0.10% had secondary glaucoma.
Conclusions:
HRGS is the largest population-based glaucoma study in India to date with glaucoma prevalence comparable to other landmark Indian studies. POAG was the most common form of glaucoma in our study population as well. PACG was more common in this region than previously thought.
Keywords: Frequency doubling perimetry, gonioscopy, intraocular pressure, primary angle closure glaucoma, primary open angle glaucoma
Glaucoma, the leading cause of global irreversible blindness, is estimated to have affected over 60.5 million persons worldwide.[1] The estimated prevalence for India was 11.9 million in a study conducted in the late 1990s; the number has only increased since.[2,3]
Urban and rural India differ in patient demographics, disease patterns, and access to ophthalmic care.[4,5,6] The only glaucoma prevalence study from Eastern India examined 1269 subjects from a rural population.[7] The purpose of the Hooghly River Glaucoma Study (HRGS) was to examine the prevalence of glaucoma in a larger rural and urban East Indian population to make the results comparable to other international landmark glaucoma prevalence studies.
Subjects and Methods
The HRGS was a population-based cross-sectional study. The Institutional Ethics Review Board approved the study that adhered to the tenets of the Declaration of Helsinki.
The sample size required for a precise estimate of the prevalence of glaucoma was calculated based on the methodology of other prominent prevalence studies. Assuming a 3.5% prevalence of glaucoma based on the Andhra Pradesh Eye Diseases Study (APEDS),[8] Vellore Eye Study,[9] and Chennai Glaucoma Study (CGS)[10] and a design effect of two, the required sample size (n) was calculated using Daniel's Formula.[11]
Kolkata city was our urban study area. The city is divided into 15 boroughs and 141 wards.[12,13,14] One division was randomly selected from each of these 15 boroughs and 8 divisions were randomly picked from those 15 divisions. The following areas of Kolkata constituted the eight randomly selected divisions: (i) Bidhan Sarani, (ii) C. R. Avenue, (iii) Rash Behari Avenue, (iv) Prince Anwar Shah Road, (v) Diamond Harbour Road, (vi) Circular Garden Reach Road, (vii) B. T. Road, and (viii) A. J. C. Bose Road. A simple random sample of 910 each from the above eight randomly selected divisions was enumerated to reach a sample size of 7248 for our urban population.
The rural study area consisted of 28 contiguous villages from 13 Gram Panchayats in Balagarh Police Station of Hooghly district in West Bengal, which was within a 20 km radius surrounding the rural base hospital located at Dhobapara, Balagarh Police Station, in the village Kuliapara of this district. The rural study area comprises a total population of 14,816 people residing in the 13 Gram Panchayats. Twenty-Five percent of the population was above the age of 40 years as per 2011 census of West Bengal, and hence, 3704 people were expected to fall in the age group of above 40 years in our rural study area. Applying a design effect of 2, our rural sample size came to 7408.
Procedure
The study procedures were divided into two segments: (i) Epidemiological fieldwork and (ii) hospital-based clinical examination and diagnostic procedures. Epidemiological fieldwork commenced in April 2011 and was completed in December 2013. The clinical examinations commenced in June 2011 and were completed in January 2014. People aged 40 years and above or those turning 40 in the current calendar year who were residents at the target addresses for a minimum period of 6 months were eligible for inclusion.
Epidemiological fieldwork
Field operations and enumeration
Social workers and volunteers belonging to the study area carried out the field operations, with the cooperation of local community leaders. The social workers conducted a door-to-door survey of all the households in the study area to collect details regarding the number of families in the area, the total number of members, and eligible members in each family. Multistage random cluster sampling was used. On the day of the examination, the social worker accompanied the eligible subjects in the project vehicle to the base examination center.
Awareness programs
Awareness programs, the main essence of HRGS, were periodically organized and conducted by the project staff in various nongovernment organizations, local party offices, and community centers of the above-defined rural and urban study areas to promote participation. The importance of glaucoma as a public health problem and the need to undergo eye examinations for early diagnosis were stressed during these meetings.
Hospital-based clinical examination and diagnostic procedures
Overview
On arrival at the examination center, the subjects were requested to sign an informed consent. In the case of illiterate subjects, the consent form was read out to them in their vernacular language in the presence of either a relative or a community volunteer. The left thumb impression was used as a signature for illiterate patients. They then proceeded through various ophthalmic examinations and diagnostic procedures in the following order:
Ocular and medical history
Lensometry was performed where necessary
Refraction and recording of best-corrected visual acuity
Pupillary evaluation
Frequency doubling technology perimetry (FDT): Visual field evaluation was done with the FDT (Zeiss Humphrey Systems, Dublin, CA, USA) which was calibrated 3 monthly. All subjects underwent the screening C-20-1 test twice and the N-30 threshold test once. Subjects with unreliable performance were recalled 2 weeks later to repeat the test, and the repeat test results were included in the analysis
Corneal pachymetry: The central corneal thickness was measured using the ultrasonic pachymeter (OcuscanRxP, Alcon Inc., USA) which was calibrated by the manufacturer every 6 months
Slit lamp biomicroscopy, including van Herick grading of the angle of the anterior chamber angle, was performed
Applanation tonometry: Intraocular pressure (IOP) recording with the Goldmann applanation tonometer (Haag-Streit International, AT 900) was done. Calibration was done by three trained senior glaucoma surgeons on a weekly basis. These three surgeons were responsible for performing all clinical examinations and interpreting the results
Gonioscopy: A Sussman-type 4-mirror hand-held gonioscope (Volk Optical Inc, Mentor, Ohio, USA) was used, and the angle was graded according to the Shaffer system. Gonioscopy was performed in dim ambient illumination with a shortened slit that did not fall on the pupil. An angle was considered occludable if the pigmented trabecular meshwork was not visible in >270° of the angle in dim illumination. All subjects with occludable angles in one or both the eyes were deemed to have primary angle closure disease (PACD). If the angle was occludable, indentation gonioscopy was performed, and the presence or absence of peripheral anterior synechia was recorded. Laser iridotomy was performed in subjects with occludable angles after obtaining their consent. The rest of the examination was deferred to another convenient date following laser iridotomy
Ocular biometry
Grading of lens opacities (Lens Opacities Classification System II)
Fundus examination
Optic disc evaluation was done using + 78D lens. The vertical cup-disc ratio (VCDR) was recorded, and a special note was made of peripapillary atrophy and optic disc/peripapillary hemorrhage, bayoneting sign, baring of circumlinear vessels, and laminar dot sign
Blood pressure recording.
Diagnostic definition of glaucoma for the HRGS was based on the International Society of Geographical and Epidemiological Ophthalmology (ISGEO) recommendations[15] with some study specific modifications. A diagnosis of glaucoma was made in the HRGS when the subjects fulfilled two or more of the following criteria:
IOP by Goldman applanation tonometry ≥22 mmHg
VCDR ≥0.6 in either eye or VCDR asymmetry of ≥0.2
Shaffer grading of 2 or less for more than 270° in either eye by gonioscopy
FDT results suggestive of glaucomatous damage as interpreted by three senior trained glaucoma specialists. Based on ISGEO guidelines,[15] the presence of a cluster of three contiguous points at the 5% level or less on the pattern deviation plot of the N-30 threshold test was taken to be indicative of glaucomatous damage.
Among the subjects diagnosed with glaucoma, patients with a history of use of topical steroids in the last 6 months, a history of trauma or ocular surgery (excluding squint or oculoplastic surgeries), a history of chronic uveitis, evidence of pseudoexfoliation or pigment dispersion on slit lamp examination, and those with hypermature or intumescent cataract were grouped under secondary glaucomas. Manifest primary angle closure glaucoma (PACG) was defined as IOP of 22 mmHg or more by applanation tonometry or glaucomatous optic disc damage with visual field loss in the presence of an occludable angle. An IOP of 22 mmHg or more by applanation tonometry in the presence of an occludable angle secondary to an obvious cause was defined as secondary angle closure glaucoma. All the other subjects diagnosed with glaucoma were classified as primary open angle glaucoma (POAG).
Statistical analysis
The data collected from both rural and urban cohorts were analyzed using SPSS Statistics software package version 13 (SPSS Inc., Chicago, IL, USA). Statistical significance was defined as P < 0.05 and P < 0.001 was taken to be statistically highly significant. Multiple logistic regressions were used to examine the association between the risk factors such as age, sex, IOP, and CCT with POAG and PACG.
Results
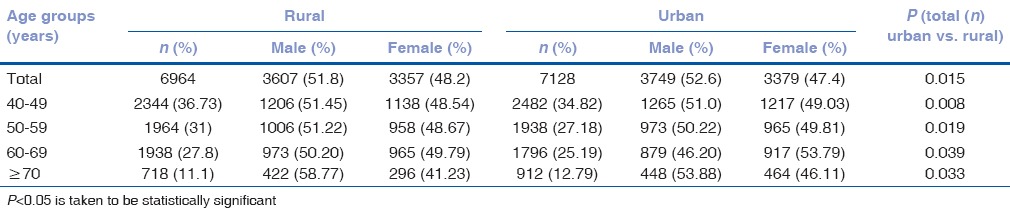
A total of 7248 subjects aged 40 years or older were enumerated from Kolkata city whereas 7408 subjects were enumerated in the rural area. Data from 7128 subjects were analyzed in the urban phase (response rate – 98%) and 6964 subjects were analyzed in the rural phase (response rate – 94%) of this largest Indian epidemiological study on glaucoma prevalence. Table 1 shows that 52.6% of the subjects analyzed were male in the urban group, and 51.8% were male in the rural group. The average age of the subjects in our study was 59.34 (±12.63) years in the urban group and 59.25 (±9.28) years in the rural group (P > 0.05; no significant difference).
Table 1.
Age and sex distribution of subjects in the Hooghly River Glaucoma Study
Totally, 230 subjects (3.23%; 95% confidence interval [CI]: 2.93–3.53%) were detected to have glaucoma in our urban population using the modified ISGEO criteria with 53.42% being male whereas 188 subjects (2.70%; 95% CI: 1.09–4.31%) were suffering from glaucoma in the rural group with 55.31% being male as is detailed in Table 2. The prevalence of glaucoma increased with age in both our urban and rural study populations.
Table 2.
Age and sex distribution of subjects detected with glaucoma in the Hooghly River Glaucoma Study

The average age of the subjects with glaucoma was 64.03 (±2.56) years in the urban group and 63.62 (±2.22) years in the rural group. The average IOP in our urban study population was 19.4 mmHg for the right eye (range: 8–52 mmHg) and 18.7 mmHg for the left eye (range: 8–50 mmHg). The average IOP in our rural study population was 18.3 mmHg for the right eye (range: 8–52 mmHg) and 17.9 mmHg for the left eye (range: 8–50 mmHg). The mean VCDR in both our urban and rural study populations was 0.4 with 0.6 being the 97.5th percentile.
Totally, 110 subjects (1.54%) in the urban arm of the HRGS had PACD. Sixty were male and fifty were female. PACD in both the eyes was detected in 62 subjects and PACG was detected in 69 subjects. No cases of secondary angle closure glaucoma were detected in our urban cohort. One hundred and sixty-one subjects had OAG, out of which 11 subjects had secondary OAG. In the secondary glaucoma subgroup, five subjects had pigmentary glaucoma, three had pseudoexfoliation syndrome, two had uveitic glaucoma, and a single eye had neovascular glaucoma secondary to uncontrolled diabetes mellitus. Hence, in our urban population, 2.10% (95% CI: 1.99–2.21%) had POAG, 0.97% (95% CI: 0.90–1.04%) had ACG, and 0.15% (95% CI: 0.13–0.17%) had secondary OAG.
Totally, 132 subjects (1.9%) in the rural arm of HRGS had PACD. Among the subjects diagnosed with glaucoma in the rural arm, 72 subjects had PACG. Eight subjects had secondary angle closure glaucoma due to hypermature/intumescent cataract. Of the eighty subjects with angle closure glaucoma, 47 (59%) were male and 33(41%) were female. Angle closure in both the eyes was detected in fifty subjects. The rest of the 108 subjects had OAG, out of which 7 subjects had secondary glaucoma. In the secondary OAG subgroup, one subject had pigmentary glaucoma, three had pseudoexfoliation syndrome, two had uveitic glaucoma, and a single eye had neovascular glaucoma secondary to central retinal venous obstruction. In our rural population, 1.45% (95% CI: 0.59–2.31%) had POAG, 1.15% (95% CI: 0.88–1.42%) had ACG, and 0.10 ± 0.03% (95% CI: 0.07–0.13%) had secondary OAG.
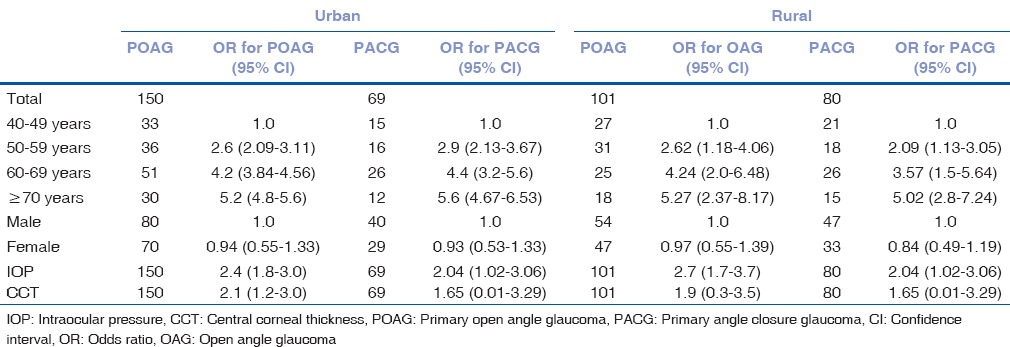
Table 3 shows the multiple logistic regressions for POAG and PACG in our rural and urban study populations. Increasing age, lower CCT, and a higher IOP were detected as risk factors for glaucoma.
Table 3.
Multiple logistic regressions for risk factors for primary open angle glaucoma and primary angle closure glaucoma in the urban and rural phases of the Hooghly River Glaucoma Study
Frequency doubling technology (FDT) results of 322 subjects (4.62%) in the rural cohort and 182 subjects (2.55%) in the urban cohort could not be analyzed due to poor/unreliable performance. Table 4 shows the decadal age distribution of subjects who had FDT positive for glaucomatous damage. In the urban population, FDT was positive in both the eyes in 177 (2.48%) subjects. In the rural arm, FDT was positive in both the eyes in 122 (1.75%) subjects. FDT positivity increased with age in both the rural and urban groups. FDT positivity was found to be significantly higher in the urban group (P < 0.05).
Table 4.
Subjects with frequency doubling technology perimetry changes positive for glaucomatous damage in the rural and urban arms of the Hooghly River Glaucoma Study
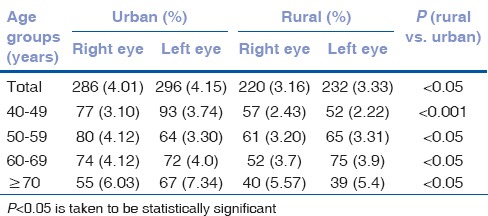
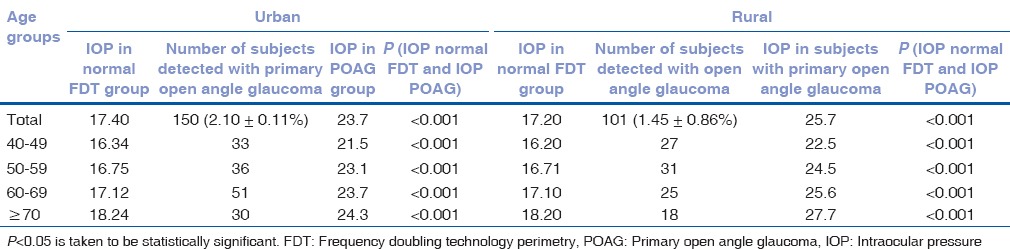
Table 5 shows the distribution of IOP across various age groups in persons with normal FDT in both eyes and subjects with POAG. The IOP in the POAG group was significantly higher than in the group with normal FDT (P < 0.001) in both the rural and urban arms.
Table 5.
Distribution of intraocular pressure across age groups in persons with normal visual field in both eyes by frequency doubling perimetry and subjects with primary open angle glaucoma
Discussion and Conclusions
The estimated global prevalence of glaucoma was found to be 3.54% in a systematic meta-analysis in 2014, with the highest prevalence in Africa.[3] The number of people with glaucoma worldwide (ages 40–80 years) was projected to increase from 64.3 million in 2013 to 111.8 million in 2040, disproportionately affecting people residing in Asia and Africa.[3]
The HRGS is the largest glaucoma prevalence study from India and the first glaucoma prevalence study from Eastern India to examine an urban population and compare the findings with a rural population. The sample size was comparable with other landmark glaucoma prevalence studies worldwide.[2,3,7,8,9,10,16,17,18] The high response rate of 94% for the rural arm and 98% for the urban arm was probably the biggest triumph for the study team.
Our study shows a higher prevalence of glaucoma in men in both urban and rural areas. The Aravind Comprehensive Eye Survey,[16] Barbados Eye Study,[17] Rotterdam Study,[18] and Framingham Eye Study[19] also showed a higher prevalence of glaucoma in men whereas the Beaver Dam Eye Study[20] showed no gender difference in glaucoma prevalence. The CGS and Central India Eye and Medical Study (CIEMS) also showed no difference in age-adjusted glaucoma prevalence rates between genders.[21,22] The Blue Mountains Eye Study[23] reported a higher prevalence of glaucoma in women.
Several studies have shown that the prevalence of glaucoma increases with age.[16] Our study also showed a similar trend with the prevalence being more than 4% in those aged ≥70 years in both the rural and urban areas. CGS also found similar results with subjects over 70 years being five times more likely to have POAG than those younger than 50 years.[21] The average VCDR of the subjects in both the groups was 0.4 (±0.1) with 97.5% of the examined population having a VCDR of ≤0.6. Both rural and urban arms of the CGS also found a VCDR of 0.4.[7]
The HRGS used modified ISGEO criteria to diagnose glaucoma. The CGS, West Bengal Glaucoma Study (WBGS), and CIEMS also used the ISGEO recommendations.[15] The overall prevalence of glaucoma in the urban arm of HRGS was 3.23% (95% CI: 2.93–3.53%) and 2.70% (95% CI: 1.09–4.31%) in the rural arm. As has been seen in other studies,[2,8,10] here also the prevalence of glaucoma increased with age. In the CGS, the prevalence of OAG in subjects above 40 years was 3.51% (95% CI: 3.04–4.0%), and the prevalence of angle-closure glaucoma was 0.88% (95% CI: 0.60–1.16%).[10,24] In the South Indian Aravind Eye Survey, the prevalence of glaucoma in the population aged 40+ years was 2.6% (95% CI: 2.2–3.0%).[4] In the WBGS, the prevalence of glaucoma in the rural population aged 50+ years was 2.7% (95% CI: 1.7–3.7%).[7]
The prevalence of POAG has been found to be higher in the urban population in the HRGS as well as the CGS[24] and the APEDS.[8] Since the age and sex compositions of the rural and urban populations in the HRGS were similar, the significant differences between the two populations in glaucoma prevalence could be attributed to genetic differences between the two groups.
There seems to be wide variation in the reported prevalence of PACG within India. The prevalence of PACG in Southern India ranges from 0.5% to 4.3%[9,16,25,26] whereas the reported prevalence of PACG in Eastern India was only 0.23%.[7] In the HRGS, 1.54% (95% CI: 1.46–1.62%) of subjects had PACD in the urban group and 1.9% (95% CI: 1.76–2.04%) had PACD in the rural group. 0.97% (95% CI: 0.9–1.04%) were diagnosed with ACG in the urban group whereas 1.15% in the rural group had ACG. The rural ACG prevalence was, therefore, higher than the urban one and was significantly higher than that found in the only other rural glaucoma prevalence studies in this part of the country, the WBGS.[7]
Ninety-five percent of the subjects in the urban population and 98% in the rural population were unaware of the fact that they had glaucoma. The CGS also found that 94.1% of those with POAG were unaware of their disease.[25] Very low case detection rates in our population are a major health concern.[24] This underlines the inadequacy of glaucoma awareness and screening programs in India. It is worth noting that in the HRGS, about 75% subjects with POAG and 57% subjects with PACG (in both cohorts) had IOP ≤97.5th percentile of normal IOP of the respective cohorts. This suggests that screening for glaucoma based merely on IOP measurement cannot be fully effective. Furthermore, the diurnal variation of IOP should be given its due importance in subjects with a single normal IOP reading and apparent disc damage.
The strengths of HRGS include a large sample size, a high response rate, and use of established standardized protocols for glaucoma diagnosis including FDT. The main limitations of our study are the lack of objective documentation of the optic nerve head (ONH) and IOP measurements for a particular subject at only a single-time-point. However, the data set is exhaustive and the results provide important new information. POAG, as seen in all other glaucoma prevalence studies,[8,23] is indeed the most common type of glaucoma. However, PACG is more common in this region than previously thought, and the current study strongly recommends that gonioscopy should be made an integral part of the routine ophthalmological evaluation. Further, the findings of this large epidemiological study involving both a rural and urban populations can be used to help design cost-effective glaucoma screening, treatment, and rehabilitation programs, and to develop public health strategies on early detection and management of glaucoma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quigley HA. Number of people with glaucoma worldwide. Br J Ophthalmol. 1996;80:389–93. doi: 10.1136/bjo.80.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Ramachandran A, Snehalatha C, Dharmaraj D, Viswanathan M. Prevalence of glucose intolerance in Asian Indians. Urban-rural difference and significance of upper body adiposity. Diabetes Care. 1992;15:1348–55. doi: 10.2337/diacare.15.10.1348. [DOI] [PubMed] [Google Scholar]
- 5.Reddy KS, Prabhakaran D, Shah P, Shah B. Differences in body mass index and waist: Hip ratios in North Indian rural and urban populations. Obes Rev. 2002;3:197–202. doi: 10.1046/j.1467-789x.2002.00075.x. [DOI] [PubMed] [Google Scholar]
- 6.Rao GN. Ophthalmology in India. Arch Ophthalmol. 2000;118:1431–2. doi: 10.1001/archopht.118.10.1431. [DOI] [PubMed] [Google Scholar]
- 7.Raychaudhuri A, Lahiri SK, Bandyopadhyay M, Foster PJ, Reeves BC, Johnson GJ. A population based survey of the prevalence and types of glaucoma in rural West Bengal: The West Bengal Glaucoma Study. Br J Ophthalmol. 2005;89:1559–64. doi: 10.1136/bjo.2005.074948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dandona L, Dandona R, Srinivas M, Mandal P, John RK, McCarty CA, et al. Open-angle glaucoma in an urban population in Southern India: The Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1702–9. doi: 10.1016/s0161-6420(00)00275-x. [DOI] [PubMed] [Google Scholar]
- 9.Jacob A, Thomas R, Koshi SP, Braganza A, Muliyil J. Prevalence of primary glaucoma in an urban South Indian population. Indian J Ophthalmol. 1998;46:81–6. [PubMed] [Google Scholar]
- 10.Vijaya L, George R, Arvind H, Baskaran M, Ve Ramesh S, Raju P, et al. Prevalence of primary angle-closure disease in an urban South Indian population and comparison with a rural population. The Chennai Glaucoma Study. Ophthalmology. 2008;115:655–60. doi: 10.1016/j.ophtha.2007.05.034. e1. [DOI] [PubMed] [Google Scholar]
- 11.Daniel WW. Biostatistics: A Foundation for Analysis in the Health Sciences. 7th ed. New York: John Wiley and Sons; 1999. [Google Scholar]
- 12. [Last accessed on 2015 Nov 10]. Available from: http://www.westbengal.gov.in/BanglarMukh/Download?FilePath=/alfresco/d/d/workspace/SpacesStore/329ba5f1-5753-4c45-af30-a191c289fb92/Chap-p_03_08_15.pdf .
- 13. [Last accessed on 2013 Dec 06]. Available from: http://www.censusindia.gov.in/PopulationFinder/District_Master.aspx?state_code=19 .
- 14.Hugli (Hooghly) District Population Census 2011, West Bengal Literacy, Sex Ratio and Density. [Last accessed on 2014 Nov 20]. Available from: http://www.census2011.co.in/census/district/12-Hooghly.html .
- 15.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–42. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramakrishnan R, Nirmalan PK, Krishnadas R, Thulasiraj RD, Tielsch JM, Katz J, et al. Glaucoma in a rural population of Southern India: The Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–90. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 17.Leske MC, Connell AM, Schachat AP, Hyman L. The Barbados Eye Study. Prevalence of open angle glaucoma. Arch Ophthalmol. 1994;112:821–9. doi: 10.1001/archopht.1994.01090180121046. [DOI] [PubMed] [Google Scholar]
- 18.Dielemans I, Vingerling JR, Wolfs RC, Hofman A, Grobbee DE, de Jong PT. The prevalence of primary open-angle glaucoma in a population-based study in The Netherlands. The Rotterdam Study. Ophthalmology. 1994;101:1851–5. doi: 10.1016/s0161-6420(94)31090-6. [DOI] [PubMed] [Google Scholar]
- 19.Kahn HA, Leibowitz HM, Ganley JP, Kini MM, Colton T, Nickerson RS, et al. The Framingham Eye Study. I. Outline and major prevalence findings. Am J Epidemiol. 1977;106:17–32. doi: 10.1093/oxfordjournals.aje.a112428. [DOI] [PubMed] [Google Scholar]
- 20.Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1992;99:1499–504. doi: 10.1016/s0161-6420(92)31774-9. [DOI] [PubMed] [Google Scholar]
- 21.Vijaya L, George R, Paul PG, Baskaran M, Arvind H, Raju P, et al. Prevalence of open-angle glaucoma in a rural South Indian population. Invest Ophthalmol Vis Sci. 2005;46:4461–7. doi: 10.1167/iovs.04-1529. [DOI] [PubMed] [Google Scholar]
- 22.George R, Vijaya L. Prevalence of glaucoma in India: A review. J Curr Glaucoma Pract. 2007;1:7–11. [Google Scholar]
- 23.Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology. 1996;103:1661–9. doi: 10.1016/s0161-6420(96)30449-1. [DOI] [PubMed] [Google Scholar]
- 24.Vijaya L, George R, Baskaran M, Arvind H, Raju P, Ramesh SV, et al. Prevalence of primary open-angle glaucoma in an urban South Indian population and comparison with a rural population. The Chennai Glaucoma Study. Ophthalmology. 2008;115:648–54.e1. doi: 10.1016/j.ophtha.2007.04.062. [DOI] [PubMed] [Google Scholar]
- 25.Vijaya L, George R, Arvind H, Baskaran M, Paul PG, Ramesh SV, et al. Prevalence of angle-closure disease in a rural Southern Indian population. Arch Ophthalmol. 2006;124:403–9. doi: 10.1001/archopht.124.3.403. [DOI] [PubMed] [Google Scholar]
- 26.Dandona L, Dandona R, Mandal P, Srinivas M, John RK, McCarty CA, et al. Angle-closure glaucoma in an urban population in Southern India. The Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1710–6. doi: 10.1016/s0161-6420(00)00274-8. [DOI] [PubMed] [Google Scholar]


