Abstract
Background
Migraine limb pain may be under-recognized in adults and children. There is little information about familial forms of this disorder.
Objectives
To describe the clinical and inheritance patterns of familial migraine limb pain over four generations and to review the evidence for limb pain as a manifestation of migraine.
Methods
Prospective clinical and pedigree analysis with an 8-year follow-up of 27 family members.
Results
Eight members of the family had benign recurrent limb pain associated with headache in a dominant inheritance pattern. Limb pain occurred before, during or after the headache, with probable or definite migraine with aura, migraine without aura and lower-half headache. The limb pain fulfilled the International Headache Society criteria for aura in six patients and also occurred without headache in three. Four members of the family had recurrent abdominal pain and/or motion sickness in childhood.
Conclusions
This is the first report of dominant familial limb pain temporally associated with migraine headache, starting in adulthood or starting in childhood and continuing into adulthood. A search for a genetic marker is indicated. Limb pain should be included as a childhood periodic syndrome linked to migraine and recognized as part of the migraine spectrum in adults.
Keywords: Migraine, limb pain, aura, familial, headache, periodic syndrome
Introduction
Sporadic reports of migraine limb pain date back to 1873 (see 1), with subsequent reports of recurrent limb pain temporally related to migraine, cluster headache or cluster migraine episodes (2–6). The estimated frequency of such limb pain in adult migraineurs is 2–4.4% (2,4). Two-thirds of children with migraine have one or more periodic syndromes (7,8), most commonly limb pain (44%), abdominal migraine (48%) and motion sickness (41%) (7–9). The disorder may be mistaken for joint or bone pathology, ‘growing pains’ or a psychological disturbance.
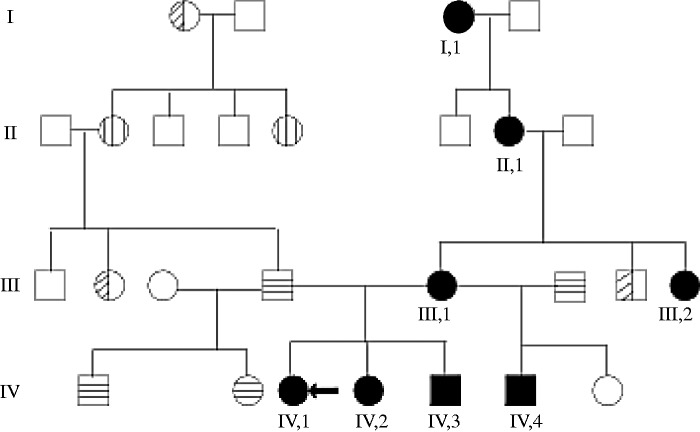
There is one previous report (10) of a family with childhood limb pain and migraine, usually in adulthood, with an autosomal dominant inheritance pattern, including male to male transmission (see II2 to III3 in their figure 1), but there was no temporal association between the limb pain and headache. We report here a four-generation family with recurrent limb pain in close temporal association with headache and review the evidence for limb pain as part of the migraine spectrum.
Figure 1.
Pedigree of family with migraine limb pain. Circle: female patient; square: male patient; black: migraine limb pain; vertical lines: migraine with aura; horizontal lines: migraine without aura; diagonal lines: migraine unspecified; arrow: index case.
Methods
International Headache Society (IHS) definitions (ICHD-3 beta) were used (11). Migraine headache was defined as in IHS code 1.1. Typical aura was defined as in code 1.2.1. Atypical aura was used when either the symptom did not accord with code 1.2.1.B or did not fulfil two criteria in 1.2.1.C, but fulfilled at least criteria 1.2.1.C2 or 1.2.1.C4. For headaches that did not fulfil the IHS criteria for migraine or other headaches, and were located below the eye, we used the term lower-half headache (LHH) as first described by Sluder et al. (see 1) and Alvarez et al. (12) According to IHS criteria, patients with migraine headache and atypical aura should be coded to 1.5.2 ‘Probable migraine with aura’, specifying the atypical feature of the aura. For clarity, we have retained the basic descriptive terms of migraine headache with typical (MA) or atypical (MA*) aura and without aura (MO).
Limb and/or body pain associated with migraine headache in adults and periodic limb pain in children are not included in the IHS definitions. The working definitions used here for adult limb pain in migraine are upper or lower limb or body pain in close temporal relationship (immediately before, during, after or in continuation) with migraine or cluster headache (2,4,6). For children, periodic limb pain is defined as two or more episodes of limb pain over a one-year period, lasting less than 72 hours, with no clinical sign or other explanation (9). The presence of allodynia was determined by asking the living patients in this study whether they experienced pain with a light touch in the painful area of the limb/body during and between attacks.
Information from family members was obtained from interviews using a standardized survey of headache and limb pain based on the above definitions and from examination and symptom diaries. The history in deceased family members was obtained from other family members and medical records. Patients were followed for eight years. Data handling was in accord with the Data Protection Act 1998. Informed consent for publication was obtained from the patient or guardian for the living patients, or the next of kin for the deceased patient.
Results
Four adults, one adolescent and three children with migraine limb pain were identified in 27 members of a four-generation family The inheritance pattern was dominant (Figure 1). A number of clinical details are lacking for member I1 (deceased) and she is excluded from some of the analyses.
The mean age of onset of migraine limb pain was 13 years (range 6–30 years). Onset was during childhood in four patients, adolescence in one and adulthood in two. Neurological examination during and between attacks was normal in all living patients. Blood and imaging investigations were normal in patients III1, III2 and II1. Table 1 summarizes the main clinical features of the limb/body pain and all types of headache in each patient, their site, laterality, aura and the types of headache that were associated with limb pain.
Table 1.
Clinical features of limb/body pain and headache.
| Limb ± body pain |
Headache |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Sex | Age at onset (years) | Age at presentation (years) | Duration from onset to latest follow-up (years) | Site | Length of episodes (minutes) | All types of headache | Side | Site | Aura | With LP | Timing |
| IV, 1 | F | 7 | 7 | 8 | L or R foot | 15 | MO, MA | Unilateral | Frontal | Paraesthesiae | MO, MA | C or post |
| IV, 2 | F | 6 | 6 | 7 | L or R foot, L or R hand, abdomen | 10 | MA* | Unilateral | Fronto-orbital | Vestibular* | MA* | Post |
| IV, 3 | M | 7 | 7 | 5 | L or R arm, back | <30 | MA* | Bilateral | Frontal, vertex | Macrosomatognosia* | MA* | Post |
| IV, 4 | M | 13 | 16 | 11 | L or R arm, R shoulder | <300 | MA* | Unilateral | Frontal | Visual + vestibular* | MA* | C |
| III, 1 | F | 20 | 46 | 34 | L or R hip, R toe | <30 | MO, MA* LHH | Unilateral/ bilateral | Fronto-orbital, jaw | Macrosomatognosia* | MO | C or post |
| III, 2 | F | 10 | 38 | 37 | L shoulder, L hip, L knee, L neck | 120 | LHH | Unilateral | L jaw | Visual* | LHH | Pre, C |
| II, 1 | F | 30 | 75 | 52 | L or R arm, L or R shoulder, R chest, neck | 30 | MO, MA LHH | Bilateral | Temporal, jaw | Visual + hemiparesis | MO, LHH | Post |
| I, 1 | F | NS | NS | NS | Shoulder, arm | NS | MA* | NS | NS | Visual | MA* | C |
F: female; M: male; NS: not specified; R: right; L: left; with LP: headache types associated with limb pain; LP: limb pain; M: migraine headache; A: aura; *: atypical; O: without aura; C: concurrent with limb pain; Pre: before limb; Post: after limb pain.
Headache and aura
All patients except patient III2 fulfilled the IHS criteria for migraine headache. The headache of patient III2 did not fulfil any IHS definition and is described as LHH. Two patients had MA (sensory in patient IV1 and visual in patient II1 when adolescent), but in patient II1 the limb pain episodes occurred in association with MO and LHH (Table 1). Four patients (IV2, IV3, IV4 and III1) had MA* (Table 1) with or without limb pain. One patient (III1) had MA*, MO and LHH, but limb pain only with MO. One patient (III2) had LHH and atypical aura.
Limb pain
Limb pain was described by patients as throbbing, stabbing or as a dull, heavy pain or ache in the limb. No patient had allodynia. Limb pain remained lateralized during a single episode, but in five of seven patients it varied in laterality between episodes. Severity ranged from Visual Analogue Scale 2–8/10. There was no relationship between the severity nor laterality of the limb pain and the headache. All patients had episodes of limb pain in close temporal relationship with headache, occurring before (3/8), during (2/8), before or during (2/8) or after or during (1/8) headache. Limb pain episodes always occurred with headache in three patients (IV2, III2 and II1). Half of the episodes of limb pain were accompanied by headache in another three patients (IV1, IV3 and III1) and in one patient (IV4) 20% of episodes of limb pain occurred with headache. The proportion of headache attacks with limb pain varied throughout the period of observation. Overall it was estimated to be mostly without limb pain in four patients (IV3, IV4, III1 and II1), mostly with limb pain in two patients (IV1, IV2) and always with limb pain in one patient (III2).
Limb pain and aura
Limb pain occurred concurrently with aura in four patients, before the headache in three patients (IV2, IV3 and IV4) and during the headache in one patient (III2). Limb pain followed the aura and preceded the headache in one patient (IV1). There was no aura with limb pain in two patients (III1 and II1). Limb pain was ipsilateral to lateralized aura (IV1 and III2). Limb pain was accompanied by aura in all attacks in three patients (IV2, IV4 and III2), in about 35% of attacks in one patient (IV1) and only sometimes in one patient (IV3). Limb pain satisfied IHS criteria 1.2.1 for sensory aura in six patients (IV1, IV2, IV3, IV4, III1 and II1), Part C 2.3.4 in five patients and 3 and 4 in one patient. One patient (III2) did not have migraine headache. Patient I1 was classified as MA* as there was limited information about the aura.
Limb pain without headache
In three patients (IV1, IV3 and III1) limb pain also occurred on occasion without headache, when it was similar to that occurring with headache, but sometimes associated with abdominal pain for 30 minutes (patient IV1), back pain (patient IV3) and stabbing pains (patient III1).
Periodic syndrome and limb pain
Four of our patients had abdominal pain (patient IV1) or motion sickness (patient IV4) or both (patients IV2 and III1) during childhood. One patient (IV1) had both abdominal and limb pain during childhood, but only the recurrent limb pain continued into adolescence was associated with migraine headache. Another patient had abdominal and limb pain concurrently with MA* (IV2) and one patient (III1) had recurrent abdominal pain and motion sickness during childhood, but MO with limb pain and LHH starting in adulthood.
Response to treatment
Headaches and limb pain responded well to analgesia during episodes. In one patient (III1) prophylaxis was indicated and the frequency of headaches and limb pain was reduced by propranolol.
Case descriptions
Index case (IV1)
A 7-year-old schoolgirl awoke at 02:00, crying, pale and distressed with a diffuse, severe ache in her left foot lasting for 15 minutes. She was afebrile, lucid and the foot was normal with no tenderness or allodynia. She could walk during the pain. A similar episode occurred a few days later. Before investigations for a focal cause of left foot pain took place, she awoke twice with right foot pain, nausea and abdominal pain. On a fifth occasion, she awoke with a right-sided severe throbbing frontal headache, photophobia, nausea, pallor and right foot pain.
This patient reported over 30 episodes involving the left or right foot over the next 2 years. The foot pain occurred prior to the headache or concurrently. Sometimes the foot pain or headache occurred independently. The headache was frontal, unilateral, moderate to severe, pounding, with marked photophobia and lasted up to 5 hours. The initial episodes were nocturnal, but five episodes subsequently occurred during the day. On 12 occasions she had malaise and tingling in her foot for 30–60 minutes before the onset of limb pain. At follow-up at 15 years of age, the episodes of limb pain usually occurred when awake, often starting in the evening, and were coupled with ipsilateral or contralateral headache in 50% of occurrences.
Patient IV2
This female patient had severe motion sickness aged 2–4 years and daytime episodes of foot pain at 6 years of age, starting with dizziness and a deep aching in the left or right foot or hand for about 10 minutes. One limb was involved at a time, followed by a unilateral, fronto-orbital, throbbing headache, ipsilateral or contralateral to the limb pain, sometimes with abdominal pain. She was quiet, pale, nauseated and photophobic during the episodes and wanted to sleep in a dark room, awakening pain-free a few hours later. Episodes occurred at a maximum every 2 months. On some occasions the headaches were preceded by dizziness, but not by limb pain.
Patient IV3
At 7 years of age this boy developed episodic back pain with nausea, lethargy, pallor and marked photophobia, sometimes with a bilateral frontal or vertex headache. The episodes started with a deep throbbing pain between the shoulder blades, going down the centre of his back, and sometimes followed by a throbbing pain in the top half of his right arm, occasionally in his left arm, but never in both. As he was lying down in a quiet dark room, he would often get a severe, pounding headache on the top of his head and in both eyes, with a feeling that his eyes were swollen. He said ‘the head felt big and weighed down on my body’. The backache would get better while the headache was getting worse, then the arm would get better, then finally the headache. Episodes lasted about 30 minutes in total. On a few occasions the backache was present for several hours.
Patient IV4
This male patient had motion sickness from the age of 4 until 12 years and intermittent headaches from before the age of 10 years. In his teenage years these were unilateral, frontal, aching or throbbing, mild (2/10), lasting for hours and associated with dizziness preceding and during the headache. On a few occasions he had persistent blurred vision with the headache or visual bright spots lasting seconds and severe headaches (9/10) with nausea, vomiting and photophobia. With a few headaches he had a moderate (3/10) ache or throb in the right scapula and right upper arm, ipsilateral or contralateral to the headache, and on one occasion in the left arm. Episodes lasted up to 5 hours with a maximum frequency of every 2 months.
Patient III1
Aged 46 years at the index time, this patient had episodic abdominal pain and motion sickness as a child. In her 20s and 30s she had episodes of a moderately severe deep ache in her right hip, lasting half an hour at a time, with normal examination during and between the pain. She could not recall the frequency of these episodes. At other times she had a sharp, severe, stabbing pain in her right or left hip, behind either eye, or in her right third toe. These pains came for a period of a day or two, occurred up to 20 times per day, and then abated for weeks or months. She had mild unilateral throbbing fronto-orbital headaches at other times, but never with the hip or stabbing pain. From her early 40s she had episodes of severe pain in the lower left half of her face, awakening her at night and localized to the lower molars, together with watering of both eyes. The pain lasted 20–40 minutes and was relieved by aspirin within 20–30 minutes. Sometimes she had the unilateral sensation that part of her face or her hand was enlarged for about 30 minutes just before the head pain started. From her early 40s she noted episodes of limb pain in her right or left hip, independently or associated in 50% of episodes with unilateral throbbing headache of moderate severity, nausea, photophobia and malaise. The limb pain occurred before and/or during the headache and lasted for about 30 minutes. The headache lasted longer than the limb pain (up to 60 minutes).
Patient III2
As a child, this patient had recurrent hip pain that was never diagnosed or investigated. As an adult, she had monthly (usually premenstrual) heavy, severe pain in her left jaw starting in the morning and accompanied later by pain in her left shoulder and left neck. During these pains she had blurring of her vision for 5–10 minutes and, at the same time, pain in her left hip and knee. The pains stopped her from doing her usual activities. The episodes lasted 2 hours.
Patient II1
Aged 75 years at presentation, this patient had migraine with aura from her teenage years (visual aura for about 20 minutes, hemiparesis once lasting for a few hours and leading to hospital admission). Since her 30s, she had had pulsating headaches in the temples, usually both, with nausea and photophobia, or unilateral jaw pain lasting for 2 hours. Both pains were often preceded by left or right shoulder or arm ache and neck pain for 30 minutes. In her 70s she sometimes had short, 10–30 minute episodes of dizziness. Magnetic resonance imaging of her brain and cardiac investigations were normal for her age. She did not have any symptoms to suggest transient ischaemic attacks or stroke over the follow-up period.
Patient I1
This female patient, now deceased, had weekly unilateral severe migraine headache with visual aura. The migraine usually occurred when relaxing after a busy time. She would then withdraw to lie in a dark, quiet room. On occasions the headaches were accompanied by pain in her shoulder and upper arm. Further clinical details were not available.
Discussion
Our four-generation family adds further weight to the documented temporal link between recurrent limb pain and migraine (Table 2) (1–6). This is the first description of this association in both children and adults with an autosomal or X-linked dominant inheritance. The former is consistent with the previously reported family of Saito et al. (10). The long uncomplicated follow-up period in our family reinforces the benign nature of the disorder, as previously reported (1,2,4).
Table 2.
Recurrent limb pain and associated headache. Summary of the literaturea.
| Headache typeb |
Limb ± body pain |
Family history |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference number | No. of patients | Mean (range) age (years) | Age group | Sex (F,M) | With limb pain | Without limb pain | Localization | Laterality | Allodynia | Isolatedc | Migraine | Limb pain |
| 2 | 22 | 33 (13–79) | C 1, A 21 | 19, 3 | MO 2, MA 4 CH 7, CM 9 | None 4, CH 3, MO 5, MA 2 CM 2, Multiple 6** | UL 2 UL plus 20*** | unil | NS | 11 | 10 | NS |
| 4 | 11 | 39 (11–57) | C 1, A 10 | 8, 3 | MO 9, MA 1, LHH 1 | Same 9; none 2 | UL 8, UL + LL 2 UL or LL 1 | unil 9, bil 2 | NS | 0 | NS | 1 |
| 10 | 13 | NS | C 4, A 9 | 5, 8 | None | MO, MA | UL, LL | unil or bil | NS | 13 | 8 AD | 13 AD |
| 5 | 3 | 37 (30–41) | A 3 | 3, 0 | Migraine NS 3 | NS | UL 1, UL + B 1, LHH + UL 1 | unil 2 bil 1 | 3 | NS | NS | NS |
| 3 | 1 | 47 | A 1 | 0, 1 | CH 1 | NS | UL + LL | unil | 1 | 0 | NS | NS |
| 6 | 6 | 23 (12–36) | C 1, A 5 | 6, 0 | MO 6 | MO 5; none 1 | UL 1, UL + LL 5 | NS | 1 | 5 | 6 | 1 |
| This paper | 8 | 28 (6–75) | C 3, A 5 | 6, 2 | MA 4, MO 1, LHH 1 MO + LHH 1, MO + MA 1 | MA 4, MA + MO 1, LHH + MA + Mo 2, LHH 1 | UL + LL + N 1, UL + LL + B 1 UL 1,UL + LL 1, LL 2 UL + B 1, UL + B + N 1 | unil 8 | 0 | 3 | 8 AD | 8 AD? |
Data are presented as number of patients for each feature.
For reports before 1988, see reference (1) (Liveing, Gowers, Sluder, Cushing, Harris, Vail, Glaser, Montgomery, Wolff, Sacks, Sutherland, Wakefield, Sjaastadt, Olesen).
Headache type: with limb pain means temporally associated with limb pain; without limb pain means without associated limb pain in the same patient.
Isolated limb pain means patients in whom limb pain also occurred without associated headache.
F: female; M: male; NS: not specified; AD: autosomal dominant; C: children; A: adult; MA: migraine with aura or atypical aura; MO: migraine without aura; CH: cluster headache; CM: cluster migraine; LHH: facial pain/lower half headache; ISH: intermittent stabbing headache; UL: upper limb; LL: lower limb; N: neck; B: body (chest/abdomen/back); Unil: unilateral within one episode (may change sides between episodes); Bil: bilateral within one episode (may vary between episodes).
Multiple: MA/CH 1, MA/MO 3, MO/CH 1, MO/CM 1.
UL plus: UL + N 8, UL + LL + LHH 4, UL + LHH 3; UL + B 2; UL + LL + B 1; UL + LL + B + LHH = 1; UL + LL + N = 1.
The limb pain met the current IHS criteria of a typical sensory aura in six of our patients. The limb pain was associated with migraine headache. In three patients with MA* and two patients with MO, the diagnosis would change to MA if their limb pain was considered for their headache classification. Although the limb pain did not have a gradual onset in our patients, such a migrainous march or spread has been described previously (1,2,4), further supporting limb pain as a migrainous aura. Limb or body pain in this family did not have features of an extracranial site of migraine pain, although this has been described previously (1,2,4).
In this family there was phenotypic variation, as often described in genetic conditions. The age of onset of limb pain varied and it occurred in patients with MA or MO, or with both in the same patient, and with LHH. LHH is not currently included in the IHS classification (11). It is uncertain whether some cases of LHH with no underlying cause and with certain associated features may indicate a relation with migraine or some other primary headache. Migraine involves the lower half of the face in 8.9% of patients and isolated facial pain has been suggested as a migraine variant (12,13). Limb pain has also been described in cluster headache (1–3).
Six children and 44 adults with limb or body pain in close temporal relation to headache have now been described (41 with migraine, eight with cluster headaches and 12 with facial pain or LHH) in addition to the sporadic reports going back to 1873 (Table 2). This temporal relationship is similar to that in symptoms accepted as migrainous.
Approximately 70% of children with migraine have periodic symptoms (most commonly abdominal migraine, motion sickness and limb pain) (7). Limb pain occurs in more than one-third of children with migraine (7,8). Periodic symptoms may be part of the migraine syndrome and not migraine precursors (7). Recurrent limb pain is reported in 2.6% of children (9) and 43% of childhood migraineurs (7). Abdominal migraine – present in 4% of schoolchildren, a quarter of whom also have migrainous headaches (14) – is included in the IHS classification of periodic syndromes (11), as are spasmodic torticollis (0.4% of childhood migraineurs) (7), benign paroxysmal vertigo (6.1%) (7) and motion sickness (40%) (7). Periodic limb pain, a childhood symptom also linked with migraine (7–10), is not mentioned. Our family adds to other evidence (1,2,4,6,7,9) suggesting that limb pain and other periodic syndromes are part of the migrainous syndrome, as an aura analogous to paraesthesia, weakness or visual phenomena, or as an extracranial site of migraine pain (acephalic migraine) (7,15).
Familial migraine limb pain shares some clinical similarities with familial hemiplegic migraine. Both are dominant with a reversible neurological picture associated with migraine, although familial hemiplegic migraine may be associated with permanent deficits such as hemiplegia, cerebellar ataxia, epilepsy or intellectual deficit (16). In one patient (patient II1) with migraine headache and typical visual aura, one episode during adolescence was associated with a short-lived reversible hemiparesis.
Migraine limb pain may involve the up-regulation of central convergent pathways (17) in the brainstem, cervical cord, thalamus and cortex (18,19). The central modulation of responses and sensitization (17–19) may be relevant to projected pain, allodynia, variable pain sites and the pattern of involvement.
Swelling and bluish patches in the skin of the painful limb (2) and clinical and thermographic confirmation of cold limbs at the onset of pain, which became warmer (10), have been described in some patients with migraine limb pain. Regional or central reflex triggers are more likely than a local ischaemic phenomenon, as evidenced by systemic increases in substance P and CGRP in three patients during an episode of limb pain (10).
Conclusions
Dominant limb pain with temporally related migraine and other primary headaches and with phenotypic variability can start in adulthood or childhood. In this family, the limb pain has the same temporal profile as other periodic syndromes in children and a close temporal association with headache. It may fulfil the IHS criteria for aura and be an extracranial site for migraine. Central convergence of nociceptive pathways may be relevant to its pathogenesis. A genetic marker should be sought. Limb pain should be considered for inclusion as one of the periodic syndromes in childhood linked to migraine and recognized in adulthood as part of the migraine spectrum.
Clinical implications
Migraine limb pain in adults and children is an important under-recognized migraine variant with a benign prognosis.
Familial migraine limb pain is one form of this disorder.
Limb pain should be included as a childhood periodic syndrome linked to migraine and as a migrainous symptom in adults.
Limb pain responds to analgesia and migraine prophylaxis.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Fondecyt (Chile) Grant 1120339.
References
- 1.Guiloff RJ, Fruns M. Migrainous limb pain. A historical note. Headache 1990; 30: 138–141. [DOI] [PubMed] [Google Scholar]
- 2.Guiloff RJ, Fruns M. Limb pain in migraine and cluster headache. JNNP 1988; 51: 1022–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riederer F, Selekler H, Sándor PS, et al. Cutaneous allodynia during cluster headache attacks. Cephalalgia 2009; 29: 796–798. [DOI] [PubMed] [Google Scholar]
- 4.Raudino F. Limb pain and headache. Headache 1994; 34: 169–171. [DOI] [PubMed] [Google Scholar]
- 5.Cuadrado ML, Young WB, Fernández-de-las-Peñas C, et al. Migrainous corpalgia: body pain and allodynia associated with migraine attacks. Cephalalgia 2008; 28: 87–91. [DOI] [PubMed] [Google Scholar]
- 6.Prakash S, Shah ND, Dholakia SY. Recurrent limb pain and migraine: case reports and a clinical review. Cephalalgia 2009; 29: 898–905. [DOI] [PubMed] [Google Scholar]
- 7.Tarantino S, Capuano A, Torriero R, et al. Migraine equivalents as part of migraine syndrome in childhood. Pediatr Neurol 2014; 51: 645–649. [DOI] [PubMed] [Google Scholar]
- 8.Lanzi G, Zambrino CA, Balottin U, et al. Periodic syndrome and migraine in children and adolescents. Ital J Neurol Sci 1997; 18: 283–288. [DOI] [PubMed] [Google Scholar]
- 9.Abu-Arafeh I, Russell G. Recurrent limb pain in schoolchildren. Arch Dis Child 1996; 74: 336–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saito Y, Fusayasu E, Iitsuka T, et al. Familial limb pain in childhood: Unusual manifestation of migraine? Brain Dev 2006; 28: 660–662. [DOI] [PubMed] [Google Scholar]
- 11.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013; 33: 629–808. [DOI] [PubMed] [Google Scholar]
- 12.Alvarez M, Montojo T, de la Casa B, et al. Unilateral nasal pain with migraine features. Cephalalgia 2013; 33: 1055–1058. [DOI] [PubMed] [Google Scholar]
- 13.Yoon MS, Mueller D, Hansen N, et al. Prevalence of facial pain in migraine: a population-based study. Cephalalgia 2010; 30: 92–96. [DOI] [PubMed] [Google Scholar]
- 14.Abu-Arafeh I, Russell G. Prevalence and clinical features of abdominal migraine compared with those of migraine headache. Arch Dis Child 1995; 72: 413–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunkel RS. Acephalgic migraine. Headache 1986; 26: 198–201. [DOI] [PubMed] [Google Scholar]
- 16.Tolner EA, Houben T, Terwindt GM, et al. From migraine genes to mechanisms. Pain 2015; 156(Suppl 1): S64–S74. [DOI] [PubMed] [Google Scholar]
- 17.Bernstein C, Burstein R. Sensitization of the trigeminovascular pathway: perspective and implications to migraine pathophysiology. J Clin Neurol 2012; 8: 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angus-Leppan H, Lambert GA, Boers P, et al. Craniovascular nociceptive pathways relay in the upper cervical spinal cord in the cat. Neurosci Lett 1992; 137: 203–206. [DOI] [PubMed] [Google Scholar]
- 19.Angus-Leppan H, Olausson B, Boers P, et al. Convergence of afferents from superior sagittal sinus and tooth pulp on cells in the thalamus of the cat. Cephalalgia 1995; 15: 191–199. [DOI] [PubMed] [Google Scholar]