Abstract
Background/Objectives:
Indices predictive of central obesity include waist circumference (WC) and waist-to-height ratio (WHtR). These data are lacking for Colombian adults. This study aims at establishing smoothed centile charts and LMS tables for WC and WHtR; appropriate cutoffs were selected using receiver-operating characteristic analysis based on data from the representative sample.
Subjects/Methods:
We used data from the cross-sectional, national representative nutrition survey (ENSIN, 2010). A total of 83 220 participants (aged 20–64) were enroled. Weight, height, body mass index (BMI), WC and WHtR were measured and percentiles calculated using the LMS method (L (curve Box-Cox), M (curve median), and S (curve coefficient of variation)). Receiver operating characteristics curve analyses were used to evaluate the optimal cutoff point of WC and WHtR for overweight and obesity based on WHO definitions.
Results:
Reference values for WC and WHtR are presented. Mean WC and WHtR increased with age for both genders. We found a strong positive correlation between WC and BMI (r=0.847, P< 0.01) and WHtR and BMI (r=0.878, P<0.01). In obese men, the cutoff point value is 96.6 cm for the WC. In women, the cutoff point value is 91.0 cm for the WC. Receiver operating characteristic curve for WHtR was also obtained and the cutoff point value of 0.579 in men, and in women the cutoff point value was 0.587. A high sensitivity and specificity were obtained.
Conclusions:
This study presents first reference values of WC and WHtR for Colombians aged 20–64. Through LMS tables for adults, we hope to provide quantitative tools to study obesity and its complications.
Introduction
The prevalence of overweight and obesity has become a public health problem worldwide.1 Substantial evidence indicates that increased body weight (BW) and body fat distribution have been associated with a higher frequency of adverse health consequences including hypertension, cardiovascular disease, metabolic disorders, osteoarthritis, gallbladder stone disease, asthma, as well as multiple malignancies.2, 3, 4 International organisations and previous epidemiological cross-sectional studies have suggested that individuals with a large accumulation of body fat in the abdominal region are at greater risk of development of the metabolic syndrome.3, 5–9 To estimate the magnitude of this problem, direct indicators were used to assess various anthropometric indicators, such as body mass index (BMI), waist circumference (WC) and waist-to-height ratio (WHtR).8, 10, 11 All these indicators are simple, inexpensive, non-invasive and validated methods to apply in clinical practice and epidemiological studies.10, 12, 13
WC has been accepted by international organisations such as the International Diabetes Federation as a diagnostic criteria of metabolic complications.3, 14 In addition to the WC, the WHtR (waist (cm)/height (Ht, cm); also called the index of central obesity) has been suggested as a potentially useful index to determine abdominal fat deposition.3, 15, 16, 17 Recently, Ashwell's10 report in a robust meta-analysis, including data on more than 300 000 individuals from diverse populations across the world, confirms previous claims from smaller and less robust analyses that measures of abdominal obesity, especially WHtR, provide a superior tool for discriminating obesity-related cardiometabolic risk compared with BMI. In addition, in ‘within studies' comparison, these authors showed that WHtR was significantly superior to WC for diabetes, dyslipidaemia, hypertension and cardiovascular disease.
Given the risk of over nutrition in developing countries, it is necessary to measure its prevalence in vulnerable populations such as Latin-American people to identify high-risk groups and develop preventive interventions.18 Currently, there are few global reports on the prevalence of overweight and obesity, in particular for low-to-middle income countries (LMICs) experiencing rapid nutrition transitions such as Latin America or Africa.19, 20 Low-to-middle income countries including Colombia are an environment to assess body composition because the prevalence of both underweight and overweight individuals is relatively high; furthermore, an obesity gradient that includes developing countries from even the poorest households has been reported.19 In addition, it is likely that ethnicity and environmental differences influence body proportions, indicating the usefulness of national references to control for variations between populations. Cutoff values and percentiles for WC and WHtR are available for adults in several countries.21, 22, 23, 24, 25, 26 However, to the best of our knowledge, anthropometric indicators (WC and WHtR) that could help identify risk groups and offer information to better design interventions have not been investigated in a nationally representative sample in the Americas.
The aims of this study were to establish a Colombian smoothed centile chart and LMS tables for WC and WHtR based on data from the Colombian national nutrition survey.
Materials and methods
Design
The Colombian National Nutrition Survey (ENSIN, 2010) was carried out together with the National Demographic and Health Survey by Asociación Pro-bienestar de la Familia Colombiana (PROFAMILIA), a nonprofit organisation focusing on reproductive health.27 Details of the survey have been published elsewhere.27 In brief, participants were selected to represent 99% of the country's population using a multistage stratified sampling scheme. Subsamples were randomly drawn to estimate departmental, subregional, regional and/or national-level estimates of specific nutrition problems among individuals 0–64 years of age.28 All municipalities from the thirty-two departments in the country were grouped into a strata based on similar geographic and sociodemographic characteristics. The survey included 50 670 households, representing 4987 clusters from 258 strata.27 The first author applied to the PROFAMILIA-ENSIN and obtained permission to use the publicly available data for research and teaching learning purpose. Further details can be obtained from the website of PROFAMILIA-ENSIN (http://www.icbf.gov.co/portal/page/portal/PortalICBF/Bienestar/ENSIN1).
Participants
The present cross-sectional study included 83 220 participants 20–64 years of age (mean age 40.9±16.7). A total of 108 916 of 25 696 (76.9%) subjects were omitted, because of missing values for WC and/or Ht (36 264 men/46 956 (56.4%) women). The study was conducted according to the guidelines laid down in the Declaration of Helsinki. All participants provided written informed consent and the Research Ethics Review Board at the Colombian Institute of Family Welfare approved the survey protocol. A comprehensive verbal description of the nature and purpose of the study and its experimental risks was given to all participants and provided written informed consent before entering the study. The Ethical Committee of the PROFAMILIA provided ethical approval before data collection. To conduct the present analysis using the ENSIN 2010 database, the Manuela Beltrán University Research Ethics exempted the project (Resolución 8430 de 1993; Ministerio de Salud de Colombia).
Data sources
Anthropometric measurements were obtained in all household members with the use of standardised techniques and calibrated instruments. Ht was measured with the use of a stadiometer (Diseños Flores S.R. Ltda, Bogotá, Colombia) to the nearest millimetre. BW was measured on SECA 872 scales to the nearest 100 g. BMI was calculated as weight (kg)/height2 (m2). WC was measured twice using inextensible anthropometric tape with the subjects standing erect and relaxed with arms at the sides and feet positioned close together. WC was measured midway between the lowest border of rib cage and the upper border of iliac crest, at the end of normal expiration. WHtR was expressed as the ratio of WC (in cm) to Ht (in cm). For all measurements, the tape was positioned at a level parallel to the floor. Overweight and obesity were defined as having a BMI above the age- and sex-specific thresholds of the WHO.6 According to this definition, the group of subjects with overweight (the equivalent of BMI >25 kg/m2) also contains those who are obese (the equivalent of BMI >30 kg/m2).
Data analysis
Anthropometric characteristics from the study sample are presented as the mean with standard deviation (s.d.). Normality for selected variables was verified using histograms and Q–Q plots. Data were then split by sex and a one-way ANOVA with post hoc tests (Tukey) was used to identify differences between age groups within sexes. Smoothed age- and gender-specific table and graph percentiles were constructed for WC and WHtR via a penalised maximum likelihood with the following abbreviations: (1) M (median), (2) L (Box–Cox transformation) and (3) S (coefficient of variation).29 The appropriate number of degrees of freedom was selected on the basis of the deviance, Q-tests and worm plots, following the suggestions of Royston and Wright.30 The 3rd, 10th, 25th, 50th, 75th, 90th and 97th smoothing centiles were chosen as age- and gender-specific reference values. The associations between WC, WHtR and BMI were tested by means of Pearson's correlation coefficients. The relation between WC, WHtR and overweight/obesity as defined by the WHO was investigated with Receiver operating characteristic curves (ROC). Cutoff values were derived mathematically from the ROC curves, using the point on the ROC curve with the lowest value for the formula: (1-sensitivity)2+(1-specificity).2 The positive likelihood ratio LR (+) and the negative likelihood ratio LR (−) were also determined. Reference curves were fitted using LMS Chartmaker version 2.3 (Medical Research Council, London, UK). Descriptive statistics were calculated with SPSS Rel.21.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at P<0.05.
Results
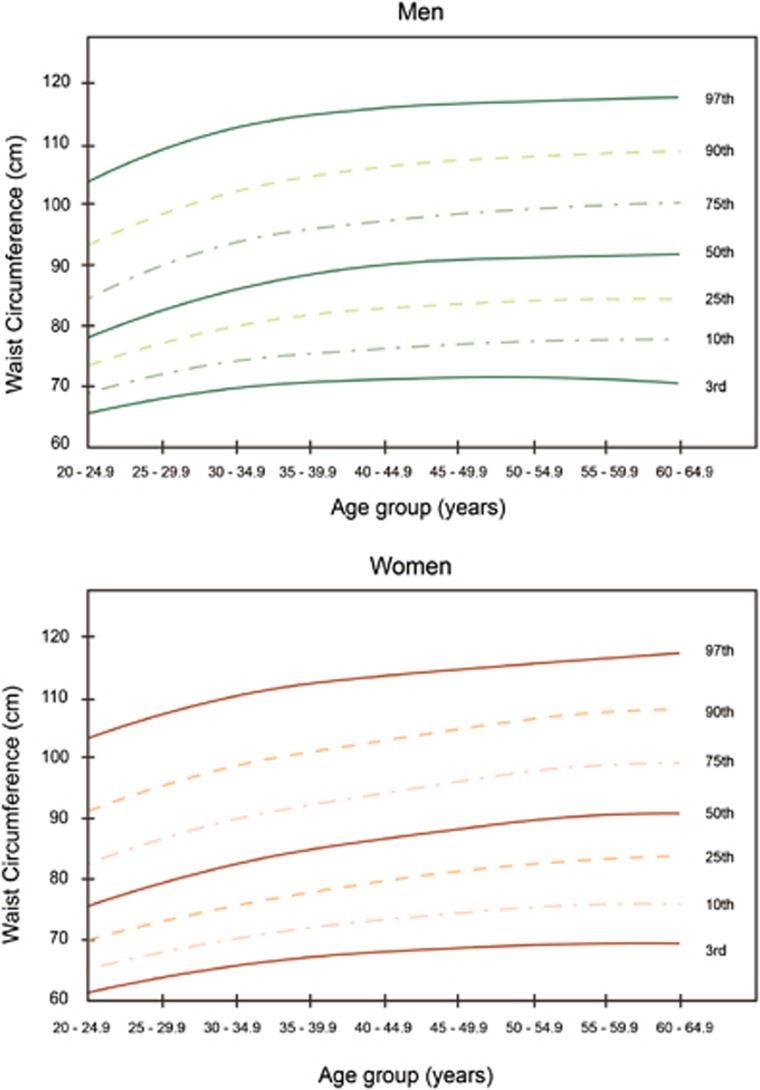
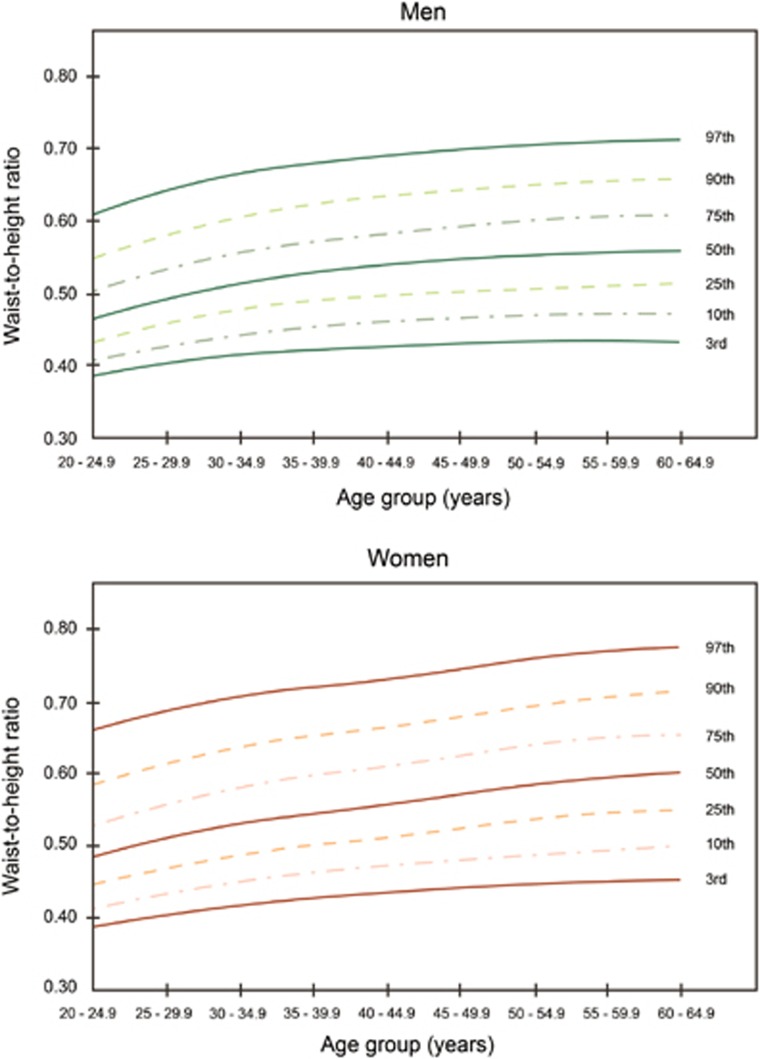
Descriptive statistics for weight, Ht, BMI, WC and WHtR by age group are presented in Table 1. The corresponding percentiles are listed in Table 2 (WC) and Table 3 (WHtR). The corresponding smoothed percentile curves are listed in Figure 1 (WC) and Figure 2 (WHtR). Mean BMI was highly comparable in both sexes, and the prevalence of overweight was 35.8% (95% confidence of interval (CI): 35.4–36.3%) in women and 36.2% (95% CI: 35.7–36.7 5%) in men and that of obesity was 21.9% (95% CI: 21.6–22.3%) and 12.8% (95% CI: 12.5–13.2%), respectively. Mean WC and WHtR increased with age in both sexes, but men had statistically significantly higher values for all ages (P<0.0001). In both sexes, we found a strong positive correlation between WC and BMI (r=0.847, P<0.01) and WHtR and BMI (r=0.878, P<0.01).
Table 1. Mean values (s.d.) for BW, Ht, BMI, WC and WHtR for Colombian adults aged 18–64 years.
| Sex | n | BW (kg) | Ht (cm) | BMI (kg/m2) | WC (cm) | WHtR |
|---|---|---|---|---|---|---|
| Men | ||||||
| 20–24.9 | 5794 | 66.5 (11.8)** | 168.8 (7.0)** | 23.3 (3.6)** | 80.1 (9.3)** | 0.475 (0.055)** |
| 25–29.9 | 5127 | 70.6 (13.4)** | 168.4 (7.0)** | 24.8 (4.1)* | 85.0 (11.0)** | 0.505 (0.064)** |
| 30–34.9 | 4675 | 72.5 (13.4)** | 168.1 (7.1)** | 25.7 (4.9)** | 88.0 (10.9)** | 0.524 (0.065)** |
| 35–39.9 | 4243 | 72.8 (13.2)** | 167.4 (7.0)** | 25.9 (4.2)** | 89.6 (11.0)** | 0.536 (0.065)** |
| 40–44.9 | 4364 | 73.4 (13.1)** | 167.3 (6.9)** | 26.2 (4.3)** | 91.2 (11.0)** | 0.545 (0.065)** |
| 45–49.9 | 3995 | 72.7 (13.3)** | 166.6 (6.9)** | 26.2 (4.2)** | 91.9 (11.5)** | 0.552 (0.069)** |
| 50–54.9 | 3214 | 71.7 (13.3)** | 165.7 (6.9)** | 26.0 (4.2)** | 92.5 (11.7)** | 0.558 (0.069)** |
| 55–59.9 | 2658 | 71.0 (13.1)** | 165.1 (7.0)** | 26.0 (4.2)** | 93.2 (11.9)** | 0.565 (0.073)** |
| 60–64.9 | 2194 | 69.4 (12.7)** | 164.3 (6.9)** | 25.7 (4.0)** | 93.0 (11.6)** | 0.567 (0.068)** |
| Total | 36 264 | 71.1 (13.2)** | 167.3 (7.1)** | 25.4 (4.3)** | 88.4 (11.8)** | 0.529 (0.072)** |
| Women | ||||||
| 20.0–24.9 | 6703 | 58.0 (11.2) | 156.4 (6.2) | 23.7 (4.3) | 77.4 (10.5) | 0.496 (0.068) |
| 25–29.9 | 6476 | 61.1 (12.1) | 156.1 (6.3) | 25.1 (4.6) | 81.2 (11.1) | 0.521 (0.072) |
| 30–34.9 | 6010 | 63.2 (12.5) | 155.3 (6.3) | 26.2 (4.8) | 84.1 (11.4) | 0.542 (0.074) |
| 35–39.9 | 5742 | 64.4 (12.6) | 155.1 (6.2) | 26.8 (4.9) | 85.7 (11.1) | 0.553 (0.073) |
| 40–44.9 | 5900 | 65.4 (13.0) | 154.7 (6.4) | 27.3 (5.1) | 87.3 (11.4) | 0.565 (0.075) |
| 45–49.9 | 5417 | 66.1 (12.6) | 154.2 (6.2) | 27.8 (5.0) | 88.9 (11.1) | 0.577 (0.074) |
| 50–54.9 | 4544 | 66.3 (12.9) | 153.4 (6.3) | 28.2 (5.1) | 90.8 (11.7) | 0.593 (0.078) |
| 55–59.9 | 3462 | 65.7 (13.0) | 152.5 (6.4) | 28.2 (5.1) | 91.8 (12.0) | 0.603 (0.079) |
| 60–64.9 | 2702 | 64.2 (13.2) | 151.5 (6.3) | 28.0 (5.3) | 91.8 (12.2) | 0.607 (0.082) |
| Total | 46 956 | 63.5 (12.8) | 154.7 (6.4) | 26.5 (5.1) | 85.6 (12.2) | 0.554 (0.082) |
Significant difference between men and women within the same age group: *P<0.01; **P<0.0001.
Table 2. Smoothed age- and sex-specific percentile of WC (cm) for Colombian adults aged 18–64 years.
| n | M | s.d. | P3 | P10 | P25 | P50 | P75 | P90 | P97 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Men | ||||||||||
| 20–24.9 | 5794 | 80.1 | 9.3 | 67.0 | 70.3 | 73.7 | 78.2 | 84.5 | 93.0 | 102.0 |
| 25–29.9 | 5127 | 85.0 | 11.0 | 69.2 | 72.8 | 77.0 | 83.5 | 91.5 | 99.5 | 107.5 |
| 30–34.9 | 4675 | 88.0 | 10.9 | 71.0 | 75.0 | 80.0 | 86.9 | 94.7 | 102.4 | 111.0 |
| 35–39.9 | 4243 | 89.6 | 11.0 | 71.9 | 76.6 | 81.5 | 88.8 | 96.2 | 103.6 | 112.0 |
| 40–44.9 | 4364 | 91.2 | 11.0 | 72.6 | 77.4 | 83.4 | 90.9 | 97.9 | 105.4 | 113.3 |
| 45–49.9 | 3995 | 91.9 | 11.5 | 72.7 | 77.5 | 83.5 | 91.5 | 98.8 | 106.4 | 114.7 |
| 50–54.9 | 3214 | 92.5 | 11.7 | 72.4 | 77.6 | 84.2 | 92.4 | 99.8 | 107.1 | 115.6 |
| 55–59.9 | 2658 | 93.2 | 11.9 | 73.2 | 78.0 | 85.0 | 93.1 | 100.5 | 107.8 | 116.1 |
| 60–64.9 | 2194 | 93.0 | 11.6 | 73.0 | 77.8 | 84.4 | 93.0 | 100.9 | 108.0 | 114.6 |
| Total | 36 264 | 88.4 | 11.8 | 70.0 | 74.1 | 79.4 | 87.4 | 96.0 | 103.9 | 112.2 |
| Women | ||||||||||
| 20.0–24.9 | 6703 | 77.4 | 10.5 | 62.8 | 66.0 | 70.2 | 75.8 | 82.5 | 90.7 | 100.5 |
| 25–29.9 | 6476 | 81.2 | 11.1 | 64.8 | 68.8 | 73.5 | 79.5 | 87.2 | 95.8 | 104.7 |
| 30–34.9 | 6010 | 84.1 | 11.4 | 66.5 | 71.2 | 76.2 | 82.8 | 90.1 | 98.7 | 108.0 |
| 35–39.9 | 5742 | 85.7 | 11.1 | 67.8 | 72.5 | 78.1 | 84.5 | 92.2 | 100.2 | 109.5 |
| 40–44.9 | 5900 | 87.3 | 11.4 | 68.5 | 73.9 | 79.5 | 86.5 | 94.1 | 101.5 | 111.3 |
| 45–49.9 | 5417 | 88.9 | 11.1 | 70.0 | 75.4 | 81.2 | 88.2 | 95.8 | 103.2 | 112.0 |
| 50–54.9 | 4544 | 90.8 | 11.7 | 70.8 | 76.6 | 82.8 | 90.1 | 98.2 | 105.9 | 113.9 |
| 55–59.9 | 3462 | 91.8 | 12.0 | 70.6 | 77.5 | 83.7 | 91.4 | 99.1 | 106.6 | 114.9 |
| 60–64.9 | 2702 | 91.8 | 12.2 | 69.8 | 76.5 | 83.7 | 91.3 | 99.0 | 107.1 | 115.5 |
| Total | 46 956 | 85.6 | 12.2 | 65.9 | 70.9 | 76.8 | 84.5 | 93.1 | 101.4 | 110.6 |
Abbreviations: M, mean; s.d., standard deviation; P, percentile.
Table 3. Smoothed age- and sex-specific percentile values of WHtR for Colombian adults aged 18–64 years.
| n | M | s.d. | P3 | P10 | P25 | P50 | P75 | P90 | P97 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Men | ||||||||||
| 20–24.9 | 5794 | 0.475 | 0.055 | 0.394 | 0.414 | 0.436 | 0.466 | 0.503 | 0.548 | 0.598 |
| 25–29.9 | 5127 | 0.505 | 0.064 | 0.408 | 0.432 | 0.460 | 0.498 | 0.545 | 0.585 | 0.635 |
| 30–34.9 | 4675 | 0.524 | 0.065 | 0.420 | 0.447 | 0.479 | 0.518 | 0.562 | 0.606 | 0.654 |
| 35–39.9 | 4243 | 0.536 | 0.065 | 0.429 | 0.457 | 0.489 | 0.531 | 0.575 | 0.617 | 0.664 |
| 40–44.9 | 4364 | 0.545 | 0.065 | 0.434 | 0.465 | 0.501 | 0.544 | 0.585 | 0.628 | 0.675 |
| 45–49.9 | 3995 | 0.552 | 0.069 | 0.435 | 0.468 | 0.506 | 0.548 | 0.594 | 0.637 | 0.685 |
| 50–54.9 | 3214 | 0.558 | 0.069 | 0.436 | 0.469 | 0.510 | 0.558 | 0.601 | 0.647 | 0.698 |
| 55–59.9 | 2658 | 0.565 | 0.073 | 0.443 | 0.478 | 0.515 | 0.564 | 0.607 | 0.653 | 0.697 |
| 60–64.9 | 2194 | 0.567 | 0.068 | 0.442 | 0.477 | 0.518 | 0.568 | 0.612 | 0.654 | 0.696 |
| Total | 36 264 | 0.529 | 0.072 | 0.414 | 0.441 | 0.476 | 0.525 | 0.575 | 0.621 | 0.670 |
| Women | ||||||||||
| 20–24.9 | 6703 | 0.496 | 0.068 | 0.397 | 0.421 | 0.448 | 0.486 | 0.531 | 0.584 | 0.643 |
| 25–29.9 | 6476 | 0.521 | 0.072 | 0.412 | 0.439 | 0.470 | 0.511 | 0.563 | 0.614 | 0.671 |
| 30–34.9 | 6010 | 0.542 | 0.074 | 0.427 | 0.456 | 0.491 | 0.534 | 0.585 | 0.637 | 0.696 |
| 35–39.9 | 5742 | 0.553 | 0.073 | 0.435 | 0.466 | 0.503 | 0.547 | 0.595 | 0.649 | 0.706 |
| 40–44.9 | 5900 | 0.565 | 0.075 | 0.440 | 0.476 | 0.514 | 0.560 | 0.609 | 0.658 | 0.721 |
| 45–49.9 | 5417 | 0.577 | 0.074 | 0.448 | 0.489 | 0.527 | 0.573 | 0.623 | 0.672 | 0.727 |
| 50–54.9 | 4544 | 0.593 | 0.078 | 0.457 | 0.498 | 0.539 | 0.589 | 0.641 | 0.693 | 0.749 |
| 55–59.9 | 3462 | 0.603 | 0.079 | 0.463 | 0.507 | 0.551 | 0.599 | 0.651 | 0.699 | 0.757 |
| 60–64.9 | 2702 | 0.607 | 0.082 | 0.462 | 0.504 | 0.554 | 0.603 | 0.656 | 0.708 | 0.763 |
| Total | 46 956 | 0.554 | 0.082 | 0.421 | 0.455 | 0.495 | 0.547 | 0.605 | 0.660 | 0.722 |
Abbreviations: M, mean; s.d., standard deviation; P, percentile.
Figure 1.
Smoothed WC (in cm) percentile curves for Colombian adults.
Figure 2.
Smoothed WHtR percentile curves for Colombian adults.
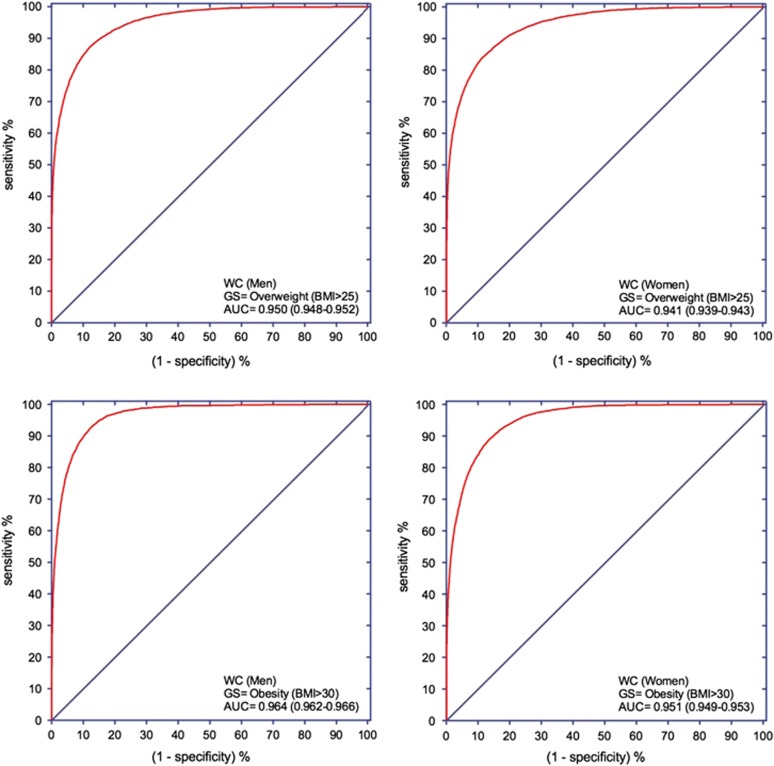
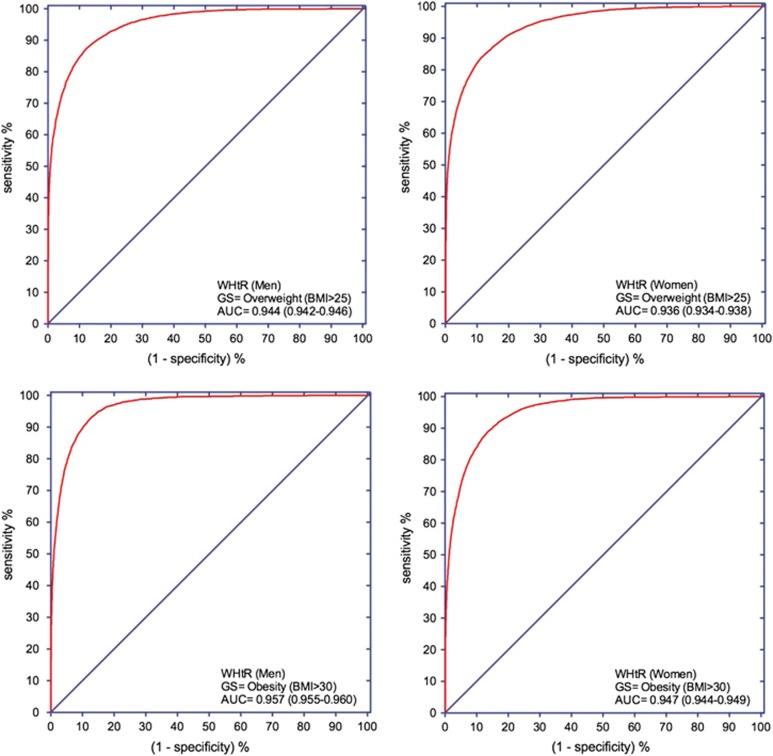
Receiver operating characteristic analysis showed that both WC and WHtR had a high discriminating power to detect WHO overweight and obesity (Figures 3 and 4).
Figure 3.
ROC curve of the WC to detect overweight (up) or obesity (down) according to the WHO criteria for Colombian adults. GS, gold standard; AUC, area under the curve (95% CI).
Figure 4.
ROC curve of the WHtC to detect overweight (up) or obesity (down) according to the WHO criteria for Colombian adults. GS, gold standard; AUC, area under the curve (95% CI).
In the overweight category in men, the cutoff point value of 87.6 cm for the WC provided a sensitivity of 87.6%, a LR (+)value of 7.01, specificity of 87.5% and LR (−) value of 0.14. In women, the cutoff point value of 84.0 cm for the WC provided a sensitivity of 84.0%, a LR (+) value of 7.30, specificity of 88.5% and LR (−) value of 0.18.
In the obesity category in men, the cutoff point value of 96.6 cm for the WC provided a sensitivity of 92.9%, a LR (+) value of 7.31, specificity of 87.3% and LR (−) value of 0.08. In women, the cutoff point value of 91.0 cm for the WC provided a sensitivity of 89.2%, a LR (+) value of 6.42, specificity of 86.1% and LR (−) value of 0.13 (Figure 3 and Table 4).
Table 4. Area under the AUC for WC and WHtR indices.
| WC | WHtC | |||||||
|---|---|---|---|---|---|---|---|---|
|
Overweight (BMI >25 kg/m2) |
Obesity (BMI >30 kg/m2) |
Overweight (BMI >25 kg/m2) |
Obesity (BMI >30 kg/m2) |
|||||
| Men | Women | Men | Women | Men | Women | Men | Women | |
| AUC (95% CI) | 0.950 (0.948–0.952) | 0.941(0.939–0.943) | 0.964 (0.962–0.966) | 0.951 (0.949–0.953) | 0.944 (0.942–0.946) | 0.936 (0.934–0.938) | 0.957 (0.955–0.960) | 0.947 (0.944–0.949) |
| Optimal cutoffs | 87.6 | 83.4 | 96.6 | 91.0 | 0.521 | 0.536 | 0.579 | 0.587 |
| J-Youden | 0.751 | 0.725 | 0.802 | 0.753 | 0.735 | 0.712 | 0.777 | 0.744 |
| Sensitivity (%) | 87.6 | 84.0 | 92.9 | 89.2 | 88.8 | 85.4 | 90.7 | 89.9 |
| Specificity (%) | 87.5 | 88.5 | 87.3 | 86.1 | 84.7 | 85.8 | 87.0 | 84.5 |
| LR (+) | 7.01 | 7.30 | 7.31 | 6.42 | 5.80 | 6.01 | 6.98 | 5.80 |
| LR (−) | 0.14 | 0.18 | 0.08 | 0.13 | 0.13 | 0.17 | 0.11 | 0.12 |
Abbreviations: AUC, area under curve; LR (+), positive likelihood ratio; LR (−), negative likelihood ratio.
ROC curve for WHtR was also obtained (Figure 4 and Table 4), and the cutoff point value of 0.521 was used. In the overweight category considering this cutoff point, in men sensitivity was 88.8%, LR (+) value of 5.80, specificity 84.7% and LR (−) 0.13. In women, the cutoff point value was 0.536, sensitivity 85.8%, LR (+) value of 6.01, specificity 85.8% and LR (−) 0.17. In the obesity category in men, the cutoff point value of 0.579 was used. The sensitivity was 90.7%, LR (+) value of 6.98, specificity 87.0% and LR (−) 0.11. In women, the cutoff point value was 0.587 with sensitivity 84.5%, LR (+) value of 5.80, specificity 84.5% and LR (−) 0.12 (Figure 3 and Table 4).
Discussion
This paper presents the first sex- and age-specific WC and WHtR percentiles for Colombian adults, 20–64 years of age. In the case of the male subjects, the mean BW tended to increase until the age of 40, after which it steadily decreased. This contrasted with the findings for women, whose mean BW increased for all of the ages studied. This coincided with previous research.31, 32 In regard to Ht, the values for both men and women tended to decrease as they became older. We agree with Minaker,33 who states that this loss of Ht is most likely due to changes related to ageing. Similar results were obtained in other studies.34, 35
The mean BMI values for both men and women steadily increased until roughly the age of 60. However, after 60, the values for men decreased, whereas those for women remained at the same level with little variation. Our results differ from Zaher et al.36 who studied 1833 adults in Malaysia and reported lower mean BMI values for women and higher BMI values for men.
As reflected in our results, the prevalence of overweight in both men and women was higher than the results obtained in other research such as Ouyang et al.,37 who reported that 31.3% of the adult population in China was overweight and 2% was obese. This could be explained by the fact that the sample populations in the two studies belong to very different cultural and nutritional contexts.
Our results for the WC and WHtR parameters agreed with those obtained in previous research.10, 26, 38 In our study, values for both genders tended to increase as the subjects grew older, although this increase was more pronounced in men. Although our data are not longitudinal (thus making it impossible to confirm a progressive increase in waist perimeter with age), the literature provides ample evidence that age modifies the pattern of subcutaneous fat distribution. As people grow older, fat tends to move from the periphery and to accumulate in the trunk region, which increases the risk of cardiovascular disease.39, 40 Furthermore, in consonance with Balkau et al.41 in their study of 168 000 adult patients in 63 countries, a positive correlation between WC and BMI values was found for both sexes. Nevertheless, despite the strong correlation observed between WC and BMI values,42 it would be helpful to know that the WC values considered normal for each BMI level. Corrective measures could then be applied to those patients with anomalous WC values and thus reducing their risk of cardiometabolic disease.
The results of our study also showed a positive correlation between WHtR and BMI values for both gender groups. This coincides with the results of previous studies43, 44, 45 in which the WHtR is described as a more accurate indicator than the WHtR for the prediction of cardiometabolic risk in adults of both sexes.
Regarding WC percentiles, the 50th percentile showed higher values for men than for women. These gender-related differences were less pronounced for the 97th percentile. Once again, our results point to sexual dimorphism in regard to the body composition of both sexes.46 The WHtR results obtained show marked differences for both men and women in the ages studied. Higher values were obtained in all percentiles for women than for men, which coincides with the results of previous research.47, 48
The ROC shows that both WC and WHtR parameters had a high level of discriminating power when it came to detecting overweight and obesity in the adult population studied. In the male overweight category, we obtained an optimal cutoff value of 87.6 cm, which was higher than the 83 cm reported by Zaher et al.36 for Asian men. In contrast, in regard to women, our optimal cutoff value was 84 cm, which is similar to the cutoff value of 83 cm in Zaher et al.36 for Asian women. However, it is somewhat lower than the cutoff specified by the WHO49 for Caucasian women.
Regarding WC, in the category of male obesity, the optimal cutoff value was 96.6 cm, which was considerably higher than the 89.05 cm reported by Liu et al.34 for the male Chinese population. As for the WC results for female obesity, the cutoff was 91.0 cm, which is very similar to the value of 90.90 cm reported by Liu et al.34 Other studies such as Miyawaki et al.50 of Japanese adults obtained optimal WC cutoff values of 86 cm for men and 77 cm for women, which were much lower than the ones obtained in our study. In line with this, in a study of Korean adults, Baik51 proposes cutoff values of 84-86 cm for men and 78–80 cm for women.
The ROC analysis for the WHtR in the male overweight category provided an optimal cutoff value of 0.521, which was slightly higher than the value of 0.51 in Liu et al.34 In the female overweight category, the cutoff value was 0.536, which was somewhat lower than the value of 0.54 reported by Liu et al.34 In the male obesity category, the WHtR cutoff was 0.570, which was lower than the value of 0.64 established in Lee et al.13 In the female obesity category, the optimal cutoff value was 0.58, which is considerably lower than the value of 0.70 reported in Lee for obese women. Nonetheless, apart from the differences between the cutoffs in our study and those reported in other research on populations at other geographic locations, the WC and WHtR values obtained for overweight and obesity in both sexes constitute the first cutoff values ever reported for a Colombian adult population. This signifies that our research results will be an important reference for future studies.
Our study had several strengths such as the fact that similar studies have not been previously performed in Colombian adults.19, 52, 53 The strength of the present research is that we studied WC and WHtR between different age groups of a large sample in Colombian adults, which could be used as a reference for our population. In addition, anthropometric data were collected by appropriately trained health professionals who used the same anatomic sites of measurements.
Limitations include the lack of information such as socio-economic, dietary and physical activity patterns, and ethnic factors that modulate growth and levels of adiposity. Another point is the cross-sectional design of the study based on data collection in 2010 with a high prevalence of overweight/obesity. Recently, Parra et al.53 using data from the 2000, 2005 and 2010 Colombian Demographic and Health Survey (ENDS) and 2005–2010 National Nutrition Survey (ENSIN), which were conducted concomitantly in the years 2005 and 2010, observed that the prevalence of overweight/obese household increased between 2000 (38.2%) and 2010 (43.1%) (P<0.05), whereas undernourished and dual burden household significantly decreased between 2005 (13.7 and 10.6%, respectively) and 2010 (3.5 and 5.1%, respectively) (P<0.05). Nevertheless, such limitations did not compromise the results obtained here, as they were similar regarding total score by gender and similar to that reported in studies carried out in Colombian.19, 52, 53
In conclusion, by providing LMS tables for WC and WHtR in adults based on Colombian reference data, we hope to provide quantitative tools for the study of obesity and its complications. Public health interventions and a national strategy to tackle the contributors to excess weight gain and its cardiometabolic consequences at the population level and in different age groups should become a national health priority in Colombia.
Acknowledgments
The ENSIN was funded by the Colombian Institute of Family Welfare (ICBF, for its initials in Spanish) and conducted during the years 2008–2010.
The authors declare no conflict of interest.
Footnotes
Author contributions
The authors' contributions are as follows: RR-V and JM-T have made a contribution to the conception of this study. EG-J, JFM-E, JS-RV, KG-R, RR-V, JFM-E, FL and JEC-B drafted the protocol and manuscript. All authors read and approved the final manuscript.
References
- Selassie M, Sinha AC. The epidemiology and aetiology of obesity: a global challenge. Best Pract Res Clin Anaesthesiol 2011; 25: 1–9. [DOI] [PubMed] [Google Scholar]
- Von Eyben FE, Mouritsen E, Holm J, Montvilas P, Dimcevski G, Suciu G et al. Intra-abdominal obesity and metabolic risk factors: a study of young adults. Int J Obes 2003; 27: 941–949. [DOI] [PubMed] [Google Scholar]
- Kagawa M, Byrne NM, Hills AP. Comparison of body fat estimation using waist:height ratio using different ‘waist' measurements in Australian adults. Br J Nutr 2008; 100: 1135–1141. [DOI] [PubMed] [Google Scholar]
- Despres JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation 2012; 126: 1301–1313. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity, 3–5 June 1997, WHO/ NUT/NCD/98.1 1997. WHO: Geneva, 1997. [PubMed] [Google Scholar]
- Kaur JA. Comprehensive review on metabolic syndrome. Cardiol Res Pract 2014; 2014: 943162. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Ashwell M, Mayhew L, Richardson J, Rickayzen B. Waist-to-height ratio is more predictive of years of life lost than body mass index. PLoS One 2014; 9: e103483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Ruíz K, Correa-Bautista JE, Ramírez-Vélez R. Evaluation of the body adiposity index in predicting percentage body fat among colombian adults. Nutr Hosp 2015; 32: 55–60. [DOI] [PubMed] [Google Scholar]
- Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 2012; 13: 275–286. [DOI] [PubMed] [Google Scholar]
- Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H et al. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr 2013; 67: 573–585. [DOI] [PubMed] [Google Scholar]
- Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0•5 could be a suitable global boundary value. Nutr Res Rev 2010; 23: 247–269. [DOI] [PubMed] [Google Scholar]
- Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 2008; 61: 646–653. [DOI] [PubMed] [Google Scholar]
- Alberti KGMM, Zimmet P, Shaw J. The metabolic syndrome – a new worldwide definition. Lancet 2005; 366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes 2003; 27: 610–616. [DOI] [PubMed] [Google Scholar]
- Bosy-Westphal A, Geisler C, Onur S, Korth O, Selberg O, Schrezenmeir J et al. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes (Lond) 2006; 30: 475–483. [DOI] [PubMed] [Google Scholar]
- Sakurai M, Miura K, Takamura T, Ota T, Ishizaki M, Morikawa Y et al. Gender differences in the association between anthropometric indices of obesity and blood pressure in Japanese. Hypertens Res 2006; 29: 75–80. [DOI] [PubMed] [Google Scholar]
- García AI, Niño-Silva LA, González-Ruíz K, Ramírez-Vélez R. Body adiposity index as marker of obesity and cardiovascular risk in adults from Bogotá, Colombia. Endocrinol Nutr 2015; 62: 130–137. [DOI] [PubMed] [Google Scholar]
- Sarmiento OL, Ramirez A, Kutschbach BS, Pinzón PL, García S, Olarte AC et al. Nutrition in Colombian pregnant women. Public Health Nutr 2012; 15: 955–963. [DOI] [PubMed] [Google Scholar]
- Ramírez-Vélez R, Rodrigues-Bezerra D, Correa-Bautista JE, Izquierdo M, Lobelo F. Reliability of health-related physical fitness tests among colombian children and adolescents: The FUPRECOL Study. PLoS One 2015; 10: e0140875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JS, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL et al. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes 2002; 26: 1232–1238. [DOI] [PubMed] [Google Scholar]
- Ho SY, Lam TH, Janus ED. Waist to stature ratio is more strongly associated with cardiovascular risk factors than other simple anthropometric indices. Ann Epidemiol 2003; 13: 683–691. [DOI] [PubMed] [Google Scholar]
- Hsieh SD, Muto T. Metabolic syndrome in Japanese men and women with special reference to the anthropometric criteria for the assessment of obesity: proposal to use the waist-to-height ratio. Prev Med 2006; 42: 135–139. [DOI] [PubMed] [Google Scholar]
- Park SH, Choi SJ, Lee KS, Park HY. Waist circumference and waist-to-height ratio as predictors of cardiovascular disease risk in Korean adults. Circ J 2009; 73: 1643–1650. [DOI] [PubMed] [Google Scholar]
- Can AS, Yildiz EA, Samur G, Rakicioğlu N, Pekcan G, Ozbayrakçi S et al. Optimal waist:height ratio cut-off point for cardiometabolic risk factors in Turkish adults. Public Health Nutr 2010; 13: 488–495. [DOI] [PubMed] [Google Scholar]
- Zeng Q, He Y, Dong S, Zhao X, Chen Z, Song Z et al. Optimal cut-off values of BMI, waist circumference and waist:height ratio for defining obesity in Chinese adults. Br J Nutr 2014; 112: 1735–1744. [DOI] [PubMed] [Google Scholar]
- ICBF. Instituto Colombiano de Bienestar Familiar. Encuesta Nacional de la Situación Nutricional en Colombia. Instituto Colombiano de Bienestar Familiar ICBF: Bogotá, 2010. Available at http://www.icbf.gov.co/portal/page/portal/portalicbf/normatividadc/ensin1/ensin2010/libroensin2010.pdf.
- Herrán OF, Ward JB, Villamor E. Vitamin B12 serostatus in Colombian children and adult women: results from a nationally representative survey. Public Health Nutr 2015; 18: 836–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 1992; 11: 1305–1319. [DOI] [PubMed] [Google Scholar]
- Royston P, Wright EM. Goodness-of-fit statistics for age-specific reference intervals. Stat Med 2000; 19: 2943–2962. [DOI] [PubMed] [Google Scholar]
- Al-Odat AZ, Ahmad MN, Haddad FH. References of anthropometric indices of central obesity and metabolic syndrome in Jordanian men and women. Diabetes Metab Syndr 2000; 6: 15–21. [DOI] [PubMed] [Google Scholar]
- He YH, Chen YC, Jiang GX, Huang HE, Li R, Li XY et al. Evaluation of anthropometric indices for metabolic syndrome in Chinese adults aged 40 years and over. Eur J Nutr 2012; 51: 81–87. [DOI] [PubMed] [Google Scholar]
- Minaker KL. Common clinical sequelae of aging. In: Goldman L, Schafer AI (eds), Goldman's Cecil Medicine, 24th edn. Elsevier Saunders: Philadelphia, PA, USA, 2011. [Google Scholar]
- Liu Y, Tong G, Tong W, Lu L, Qin X. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health 2011; 11: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TD, Goto S, Bhatt DL, Steg PG, Chan JC, Richard AJ et al. Registry Investigators: Ethnic differences in the relationships of anthropometric measures to metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism 2010; 59: 400–408. [DOI] [PubMed] [Google Scholar]
- Zaher ZM, Zambari R, Pheng CS, Muruga V, Ng B, Appannah G et al. Optimal cut-off levels to define obesity: body mass index and waist circumference, and their relationship to cardiovascular disease, dyslipidaemia, hypertension and diabetes in Malaysia. Asia Pac J Clin Nutr 2009; 18: 209–216. [PubMed] [Google Scholar]
- Ouyang X, Lou Q, Gu L, Ko GT, Mo Y, Wu H et al. Anthropometric parameters and their associations with cardio-metabolic risk in Chinese working population. Diabetol Metab Syndr 2015; 24: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, Liu Y, Yang J, Sun Y, Chen L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a Chinese population. Postgrad Med J 2011; 87: 251–256. [DOI] [PubMed] [Google Scholar]
- Wohlfahrt P, Somers VK, Cifkova R, Filipovsky J, Seidlerova J, Krajcoviechova A et al. Relationship between measures of central and general adiposity with aortic stiffness in the general population. Atherosclerosis 2014; 235: 625–631. [DOI] [PubMed] [Google Scholar]
- Khan RJ, Harvey DJ, Leistikow BN, Haque KS, Stewart CP. Relationship between obesity and coronary heart disease among urban Bangladeshi men and women. Integr Obes Diabetes 2015; 1: 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkau B, Deanfield JE, Després JP, Bassand JP, Fox KA, Smith SC Jr et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation 2007; 116: 1942–1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SC, Haslam D. Abdominal obesity, waist circumference and cardio-metabolic risk: awareness among primary care physicians, the general population and patients at risk—the Shape of the Nations survey. Curr Med Res Opin 2007; 23: 29–47. [DOI] [PubMed] [Google Scholar]
- Rosales Ricardo Y. Anthropometry in the diagnosis of obese patients: a review. Nutr Hosp 2012; 27: 1803–1809. [DOI] [PubMed] [Google Scholar]
- Shao J, Yu L. Waist-to-height ratio, an optimal predictor for obesity and metabolic syndrome in Chinese adults. J Nutr Health Aging 2010; 14: 782–785. [DOI] [PubMed] [Google Scholar]
- Lin CH, Chou CY. Waist-to-height ratio is the best index of obesity in association with chronic kidney disease. Nutrition 2007; 23: 788–793. [DOI] [PubMed] [Google Scholar]
- Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol 2015; 15: 113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X, Tabák AG, Zethelius B, Yudkin JS, Söderberg S, Laatikainen T et al. Obesity attenuates gender differences in cardiovascular mortality. Cardiovasc Diabetol 2014; 19, 13 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn HS, Bullard KM, Barker LE, Imperatore G. Differences between adiposity indicators for predicting all-cause mortality in a representative sample of United States non-elderly adults. PLoS One 2012; 7: e50428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. WHO: Geneva, 1995. [PubMed] [Google Scholar]
- Miyawaki T, Hirata M, Moriyama K, Sasaki Yutaka, Aono Hideshi, Nobuo Saito et al. Metabolic syndrome in Japanese diagnosed with visceral fat measurement by computed tomography. Proc Japan Acad 2005; 81: 471–479. [Google Scholar]
- Baik I. Optimal cutoff points of waist circumference for the criteria of abdominal obesity: comparison with the criteria of the International Diabetes Federation. Circ J 2009; 73: 2068–2075. [DOI] [PubMed] [Google Scholar]
- Sarmiento OL, Parra DC, González SA, González-Casanova I, Forero AY, Garcia J. The dual burden of malnutrition in Colombia. Am J Clin Nutr 2014; 100: 1628S–1635S. [DOI] [PubMed] [Google Scholar]
- Parra DC, Iannotti L, Gomez LF, Pachón H, Haire-Joshu D, Sarmiento OL et al. The nutrition transition in Colombia over a decade: a novel household classification system of anthropometric measures. Arch Public Health 2015; 73: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]