Abstract
Purpose
To describe the clinical manifestations and treatment outcomes of ocular syphilis in patients without human immunodeficiency virus (HIV) infection.
Methods
A total of 45 eyes from 39 patients with ocular syphilis confirmed by serologic tests were reviewed retrospectively. The included cases were all non-HIV-infected patients presenting with intraocular inflammation from 2002 to 2014 at Kyung Hee University Hospital. Medical records of 45 eyes were analyzed and included best-corrected visual acuity and ophthalmologic examination findings of the anterior and posterior segments to determine the focus of inflammation. Optical coherence tomography and fluorescein angiography findings as well as both medical and surgical management were also analyzed.
Results
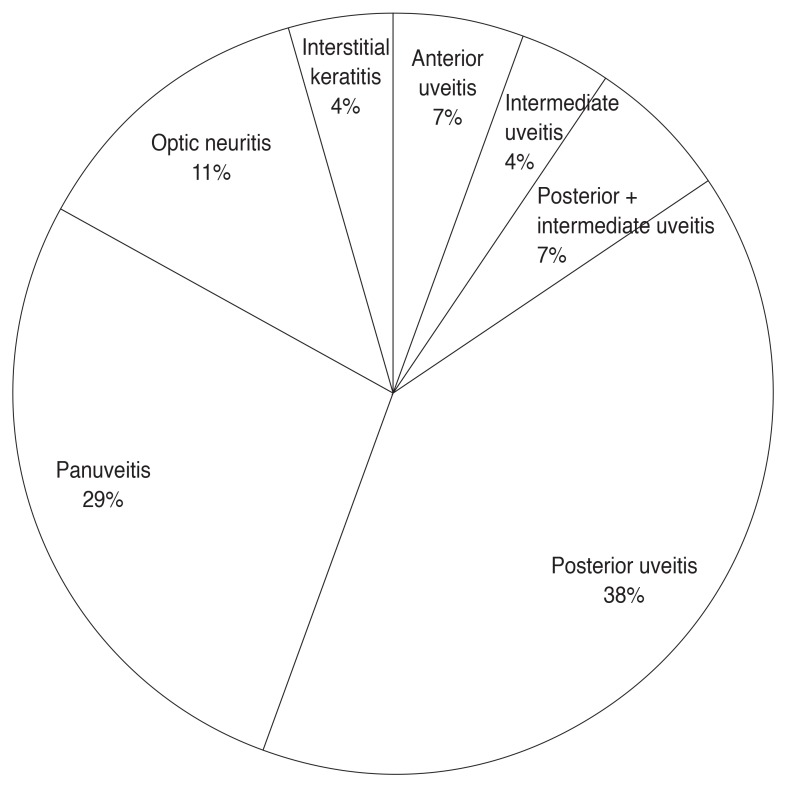
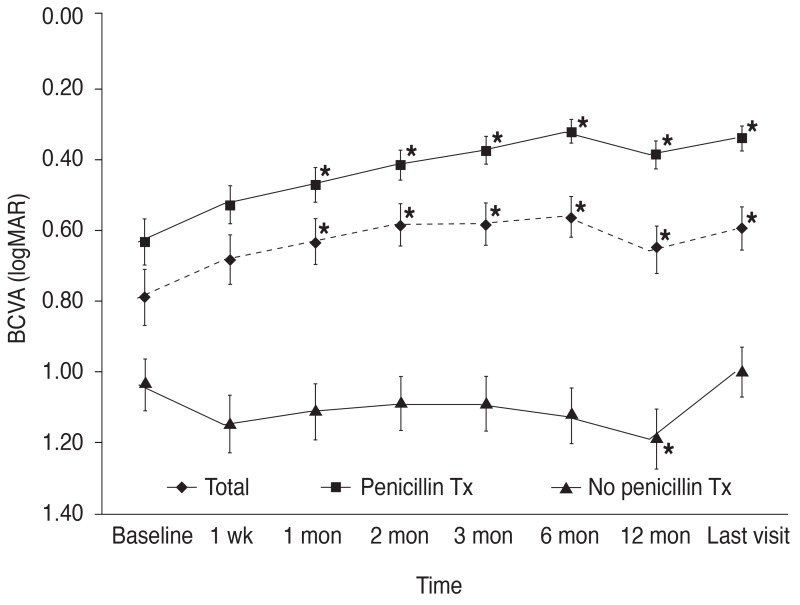
The mean patient age was 61.0 years (range, 37 to 89 years). Bilateral ocular involvement occurred in 6 patients (15.4%), and diagnoses at presentation were most frequently related to posterior uveitis (38%), followed by panuveitis (29%) and optic neuritis (11%). Isolated interstitial keratitis and intermediate uveitis were uncommon (4%, both). Twenty-eight eyes (62.2%) were treated with penicillin, and 11 eyes (24.4%) underwent surgical treatment. The mean baseline best corrected visual acuity was 0.79 ± 0.59 (mean ± standard deviation, logarithm of the minimum angle of resolution) and significantly improved to 0.60 ± 0.63 at the final follow-up after treatment (p = 0.019). Mean visual improvement was significantly greater in the penicillin-treated group (p = 0.001). Visual impairment at the final visit occurred in 11 eyes (24.4%). Among the visual impairment group, 10 eyes (90.1%) had posterior segment-involving uveitis.
Conclusions
Visual outcomes of treated, non-HIV-related ocular syphilis were favorable regardless of time to presentation. Posterior segment-involving uveitis at presentation was associated with poor visual outcome.
Keywords: Human immunodeficiency virus, Penicillins, Syphilis, Uveitis
Syphilis is a sexually-transmitted disease that can result in multiple organ involvement and demonstrates various disease progressions [1,2]. In recent years, syphilis infection has become a significant public health problem and there has been an increase in the incidence in the Republic of Korea, China, United States, and Europe [3]. In Korea, the incidence of syphilis increased about eight-fold between 2002 and 2008, with a peak in 2008 of 1,561 new stage 1 or 2 cases [4]. The rate increase occurred exclusively among men, particularly gay and bisexual men, who accounted for approximately two-thirds of all syphilis infections during this period [3,4]. Although ocular syphilis is reported to be associated with less than 1% of all syphilis cases [5], the case reports and series in the literature suggest that ocular syphilis is increasing. Moreover, almost any portion of the eye can be involved in syphilis infection [6,7], and the infection may mimic other ocular inflammatory diseases. Therefore, a high index of clinical suspicion is crucial for appropriate clinical diagnosis [8].
Ocular involvement of syphilis infection may occur in the secondary stage and, more frequently, in the later stage of disease [1,6,9]. Ocular manifestations of syphilis are characterized by non-specific involvement of the eye. Ocular syphilis can present as anterior uveitis, intermediate uveitis, interstitial keratitis, chorioretinitis, retinal vasculitis, neuroretinitis, or serous detachment of the retina [10,11,12]. Moreover, other types of infectious or non-infectious uveitis with defined causes including toxoplasmosis, herpetic retinitis, and human immunodeficiency virus (HIV) are common in ocular syphilis [13,14,15]. However, ocular syphilis can also occur in immunocompetent subjects.
HIV status and ocular syphilis treatment outcomes have not been clearly elucidated. The ophthalmic features are reported to be similar according to HIV status, in terms of proportion of bilateral cases, presenting visual acuity, and final visual outcome [3,16,17]. However, HIV-positive patients are more likely to have uveitis associated with the anterior or intermediate segment [18]. Moreover, despite the higher rates of panuveitis and optic nerve involvement in HIV-positive patients [17,19,20], macular edema was more frequently found in HIV-negative patients [3]. Visual loss and ocular complications were also common among HIV-negative patients [21].
Therefore, this study was designed to conduct a review of cases diagnosed with ocular syphilis without HIV co-infection in order to describe the clinical manifestations and to evaluate the visual outcomes following appropriate treatment. In addition, we aim to report demographics and presenting ophthalmic features of ocular syphilis in a Korean population.
Materials and Methods
A retrospective medical record review was performed on patients with ocular syphilis who presented to the Department of Ophthalmology at Kyung Hee University Hospital between January 1, 2002 and December 31, 2014. The diagnosis of ocular syphilis was made by a uveitis specialist based on clinical history, ophthalmic findings, imaging, and positive serologic testing. To confirm the diagnosis and exclude other causes of uveitis, all patients underwent laboratory examination and ocular imaging evaluations, which included chest and lumbar spine X-ray, blood rapid plasma regain test, venereal disease research laboratory (VDRL) test, fluorescent treponemal antibody absorption (FTA-ABS) test, Treponema pallidum particle hemagglutination assay (TPHA), and lumbar puncture for cerebrospinal fluid (CSF) analysis for VDRL, if indicated. Additional diagnostic testing, including serologies for toxoplasmosis, toxocariasis, immunoglobulin assay, and human leukocyte antibody typing of B27 and B51, rheumatoid factor, and other viral markers were performed in all patients. This retrospective study was conducted with the approval of the institutional review board of Kyung Hee University Hospital and in accordance with the principles of the Declaration of Helsinki.
The data of all patients were collected from a medical records database for subsequent statistical analysis. The data collected by chart review included demographic features (including age, sex, sexual behavior, and intravenous drug use); history of syphilis infection (including duration of infection); history of ocular syphilis (including duration of ocular infection) at the time of presentation; and co-morbidity history (including diabetes mellitus and hypertension). Complete ophthalmic examinations were performed at every visit including best-corrected visual acuity (BCVA) using a decimal visual acuity chart, intraocular pressure (IOP), slit-lamp examinations, grade of inflammation in the anterior chamber, and vitreous and fundus findings. The decimal visual acuity was converted to logarithm of the minimum angle of resolution (logMAR) units for statistical analysis, and the Standardization of Uveitis Nomenclature guidelines were used to classify ocular inflammation. Optical coherence tomography and color fundus photography were also performed at every visit. Fluorescein angiography was conducted for initial evaluation of uveitis except for isolated interstitial keratitis. Data on ocular surgeries and medical procedures were obtained. The route and dose of systemic antibiotics, topical antibiotics, use of topical or intraocular corticosteroids, and other intravitreal administration of medications were also reviewed.
The primary outcome variable was change in visual acuity. Visual impairment was defined as a decrease in BCVA compared to that of baseline. Change in visual acuity was designated based on the gain or loss of at least three Snellen lines and was categorized into a visual improvement group and visual impairment group. The secondary outcome variable was incidence of ocular structural complications that were confirmed by a complete ophthalmic examination and appropriate ocular imaging modalities. For secondary glaucoma, ocular hypertension was defined as an IOP higher than 21 mmHg.
Statistical analyses were performed using a licensed version of PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Numerical and categorical variables were compared among penicillin-treated and non-penicillin-treated eyes. The p-values were calculated using Pearson's correlation test, the Kruskal-Wallis test, and Student's t-test. The level of significance was set to a p-value less than 0.05.
Results
There were a total of 45 eyes from 39 patients included in this study, of which 24 patients (61.5%) were men with a mean age of 61.0 years (range, 37 to 89 years). All patients showed negative serology for HIV infection. Demographics and clinical characteristics at presentation are demonstrated in Table 1. The annual distribution of incidence was found not to increase since 2009, as shown in Fig. 1. Lens status was no aphakic, 14 pseudophakic (31.1%), and 31 phakic (68.9%) eyes at baseline. Posterior subcapsular cataract was found in 14 of the phakic eyes (45.2%). The activity of uveitis at presentation was found with anterior chamber cells in 27 eyes (60.0%), vitreous cells in 22 eyes (48.9%), and vitreous opacity in 16 eyes (35.6%). In total, 21 patients (53.8%) reported their sexual behavior, and 18 patients (46.2%) did not report sexual orientation. Of the 18 patients with a reported sexual orientation, three (16.7%) were men who have sex with men, 11 (61.1%) were heterosexual, and four (22.2%) were bisexual. The systemic manifestation of syphilis presented with oral or genital ulcers in four patients (10.3%) and skin rash in five patients (12.8%). None of the cases were related to intravenous drug use.
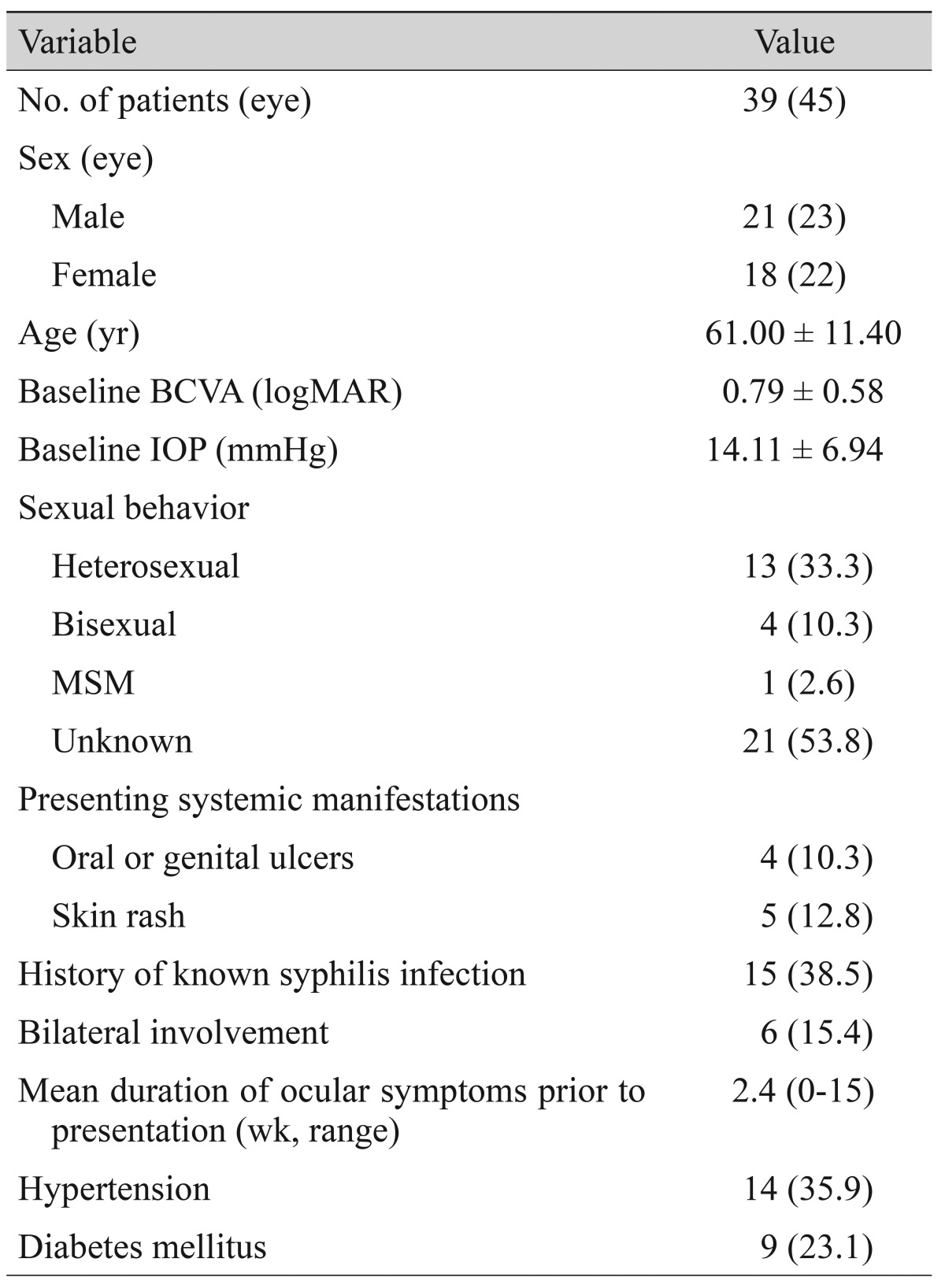
Table 1. Demographics and baseline characteristics.
Values are presented as mean ± standard deviation or number (%) unless otherwise indicated.
BCVA = best-corrected visual acuity; logMAR = logarithm of the minimum angle of resolution; IOP = intraocular pressure; MSM = men who have sex with men.
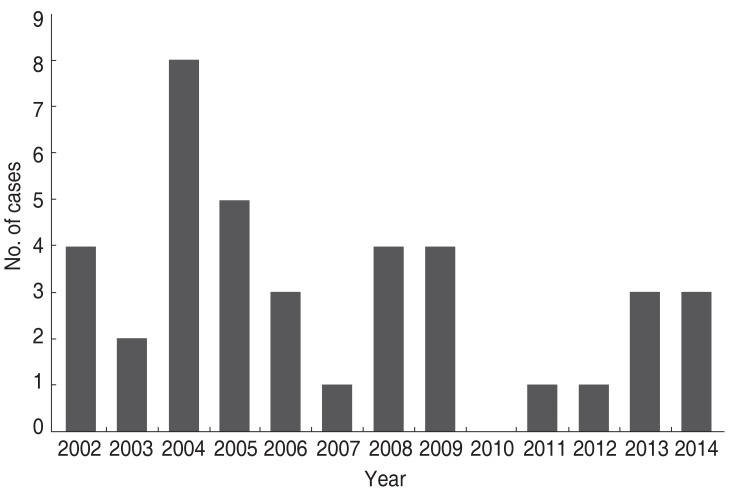
Fig. 1. The annual distribution of ocular syphilis cases. The peak incidence was found in 2004, after which the number of cases decreased.
Diagnoses at presentation
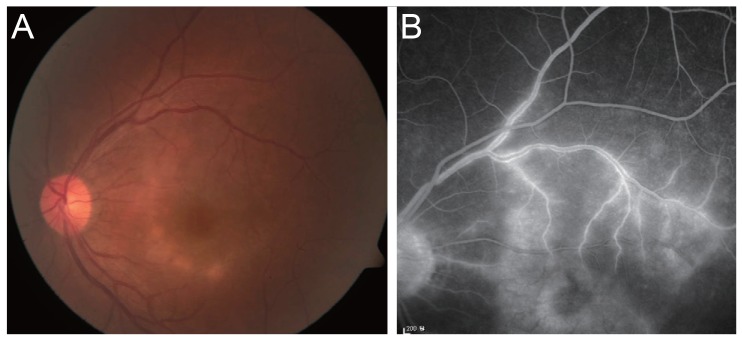
The mean duration of ocular symptoms at presentation was 2.4 weeks (range, 0 to 15). Bilateral ocular involvement occurred in six patients (15.4%). In those with unilateral manifestations, disease progression to the other eye was not seen during follow-up in any patient. The overall frequencies of presenting manifestations are summarized in Table 2. Posterior uveitis was the most frequently diagnosed, noted in 17 of the affected eyes (37.8%) (Fig. 2A and 2B). Panuveitis was the second most frequent diagnosis in 13 affected eyes (28.9%), followed by optic neuropathy (five eyes, 11.1%), combined intermediate and posterior uveitis (three eyes, 6.7%), and isolated anterior uveitis (three eyes, 6.7%). Overall posterior segment involvement was found in 38 affected eyes (84.4%), with findings including macular edema due to retinal vascular occlusion, vitritis, vitreous hemorrhage, chorioretinitis, and optic neuritis. However, isolated interstitial keratitis and intermediate uveitis were not commonly found in the affected eyes (two eyes, 4.4%, both). The overall frequency of presented diagnoses are shown in Fig. 3.
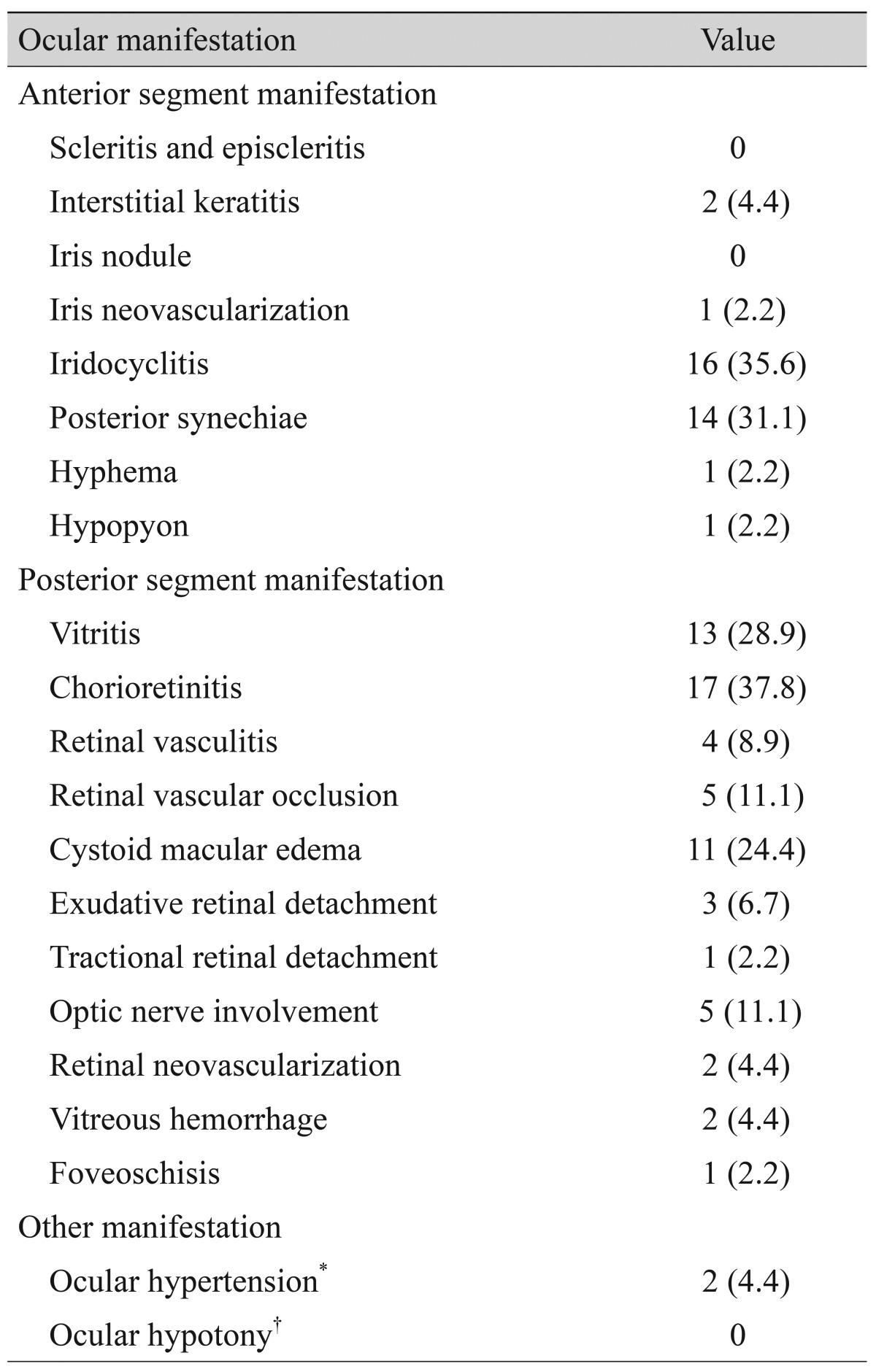
Table 2. The frequencies of clinical manifestations at presentation in patients with ocular syphilis.
Values are presented as number (%).
*Intraocular pressure higher than 21 mmHg since initiation of treatment; †Intraocular pressure lower than 5 mmHg since initiation of treatment.
Fig. 2. Fundus photograph (A) and fluorescein angiography (B) of a syphilitic posterior uveitis case at presentation. (A) Uniform distribution of outer retinal and inner choroidal inflammation with opacification in a discrete oval or circular area of the posterior pole presenting as acute syphilitic posterior placoid chorioretinitis. (B) Mid-phase fluorescein angiography showing diffuse vascular leakage in the same area of opacification.
Fig. 3. The frequencies of diagnoses at presentation in patients with ocular syphilis.
Serologic findings
The FTA-ABS and TPHA findings were positive in all patients. However, rapid plasma regain and/or VDRL titer was positive in only 32 patients (82.1%). The baseline median VDRL titer was 1 : 64 (range, 1 : 4 to 1 : 256), and mean pretreatment treponema antibody titer for TPHA was 322.11 units per milliliter (range, 30.86 to 441.85). Serologic testing for toxoplasmosis, toxocariasis, and other viral markers was negative in all patients, while HLA-B27 was positive in three patients (7.7%) and HLA-B51 in one patient (2.6%). There were six patients who underwent lumbar puncture for CSF analysis, and none had positive VDRL or FTA-ABS titer. All of the six patients showed a mild increase in CSF glucose level without significant leukocytosis.
Treatments
Of the 24 patients (61.5%) who underwent penicillin treatment, 10 (41.7%) were treated with a total of 24 million units of intravenous penicillin G benzathine for 14 days followed by intramuscular injection of 2.4 million units per week for 3 weeks. Fourteen patients (58.3%) were treated only with three intramuscular injections of 2.4 million units of penicillin G benzathine for 3 weeks. In addition to systemic antibiotic treatments, topical antibiotics, glucocorticoids, cycloplegics, and IOP-lowering agents were also prescribed.
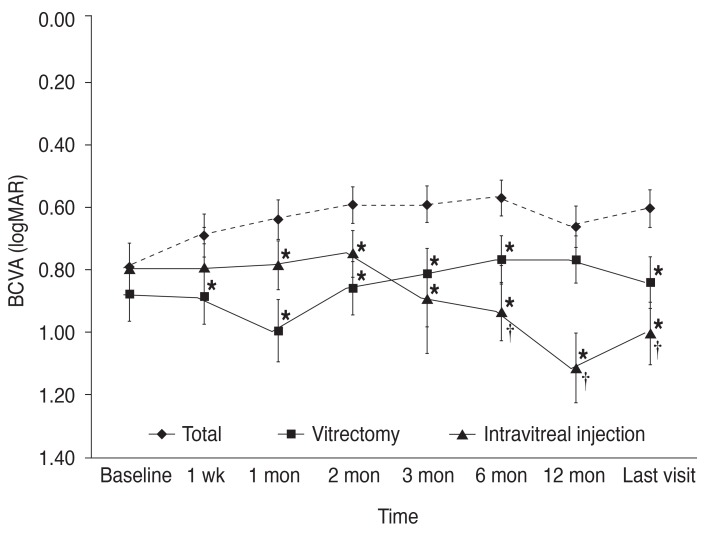
Eleven eyes (24.4%) underwent 23-gauge pars plana vitrectomy due to severe vitreous haze with opacity (eight eyes, 17.8%) and conjunction with Ahmed valve implantation for secondary glaucoma surgery (three eyes, 6.7%). In cases of combined severe macular edema, intravitreal anti-vascular endothelial growth factor (VEGF) was administered in 11 eyes (24.4%). Triamcinolone acetate was combined with anti-VEGF in four eyes with posterior uveitis. Of the 11 anti-VEGF treated eyes, five had retinal vascular occlusion, four had posterior uveitis or panuveitis, and two had vitreous hemorrhage with opacity.
Visual outcomes
A total of 45 eyes were enrolled in the study, and the mean baseline BCVA was 0.79 ± 0.59 (mean ± standard deviation, logMAR) and significantly improved to 0.60 ± 0.63 at final follow-up after treatment (p = 0.019). The average BCVA improvement at final visit was 0.19 ± 0.52 and showed significant correlation with baseline and final BCVA (p = 0.018, p = 0.001; r = 0.554, r = -0.492, respectively).
The final visual acuity was significantly greater in penicillin-treated eyes than non-penicillin-treated eyes (0.35 ± 0.42 and 1.00 ± 0.72, respectively; p = 0.001). Eyes receiving penicillin treatment showed a significant visual improvement compared to baseline visual acuity (p = 0.004), while eyes that were not treated with penicillin showed no improvement (Fig. 4). Both the intravitreal injection group and vitrectomy group showed no improvement in visual acuity at the final visit. Moreover, the intravitreal injection group showed a significant decrease in visual acuity from 0.79 ± 0.69 at baseline to 1.00 ± 0.72 at the final visit (p = 0.008) (Fig. 5).
Fig. 4. Changes in mean best-corrected visual acuity (BCVA) according to penicillin treatment (Tx). Mean BCVA was significantly increased from baseline acuity 1 month after treatment in both penicillin-treated and total eyes. Eyes without penicillin treatment showed no significant improvement in BCVA throughout the follow up visits. logMAR = logarithm of the minimum angle of resolution. *Significantly different from baseline, p < 0.05.
Fig. 5. Changes in mean best-corrected visual acuity (BCVA) according to treatment other than administration of penicillin. Mean BCVA in both vitrectomy and intravitreal injection groups was significantly worse than the BCVA of the eyes after treatment. Mean BCVA of the intravitreal injection group showed a significant decrease 6 months after treatment. logMAR = logarithm of the minimum angle of resolution. *Significantly worse than the BCVA of all eyes; †Significantly worse than baseline BCVA, p < 0.05.
Despite antibiotic or anti-VEGF treatment, 11 eyes (24.4%) had a final visual acuity worse than baseline. The presented diagnoses of visual impairment eyes were posterior segment-involving uveitis (seven eyes, 63.6%), uveitis combined with retinal vascular occlusion (three eyes, 27.3%), and vitreous hemorrhage with opacity (one eye, 9.1%). The causes of vision loss were chorioretinitis involving the fovea (five eyes, 45.4%), optic disc pallor and atrophy (three eyes, 27.3%), recurrent macular edema associated with retinal vascular occlusion (two eyes, 18.2%), and retinal atrophy associated with central retinal artery occlusion (one eye, 9.1%).
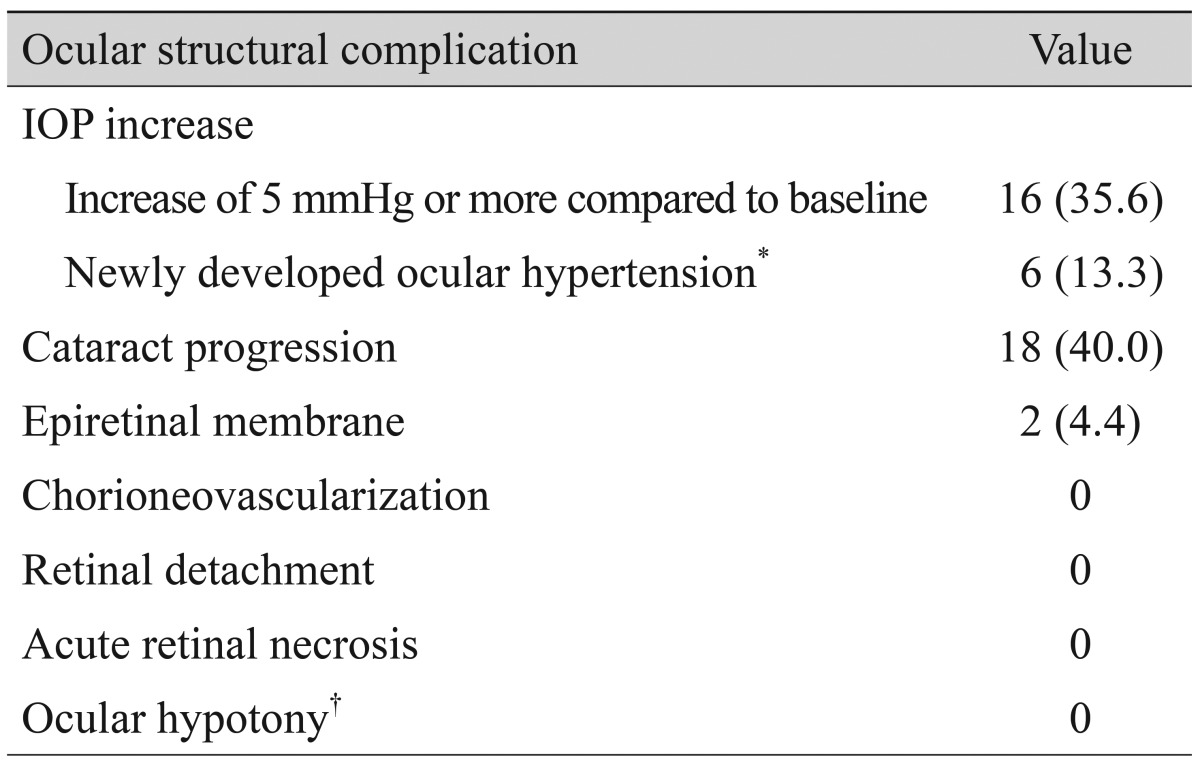
Ocular complications
The incidence of structural ocular complications after initiating treatment is shown in Table 3. A total of 16 eyes (35.6%) experienced an IOP increase of more than 5 mmHg compared to baseline at least once during the follow-up, in spite of administration of topical IOP-lowering agents. New onset ocular hypertension developed in six eyes (13.3%), and four eyes underwent glaucoma surgery due to uncontrolled increase in IOP.
Table 3. Incidence of ocular structural complications following initiation of treatment.
Values are presented as number (%).
IOP = intraocular pressure.
*IOP higher than 21 mmHg since initiation of treatment; †IOP lower than 5 mmHg since initiation of treatment.
Among the 31 phakic eyes, cataract progression occurred in 18 (58.1%), characterized by posterior subcapsular opacity, and three eyes (9.7%) underwent cataract surgery during the follow-up period. Epiretinal membrane developed in two eyes (4.4%), but no surgical procedure was performed. Treatment failure of ocular syphilis occurred in one eye (2.2%) with no four-fold titer decline at 12 months and persisting ocular inflammation. Retreatment with intramuscular penicillin injection was successful. No cases of retinal detachment, chorioneovascularization, acute retinal necrosis, or hypotony (IOP lower than 5 mmHg) were observed.
Discussion
Syphilis-related ocular inflammation is not common and has a reported incidence range from 1% to 5% of cases in the United States and Europe [5]. However, a dramatic increase in infectious syphilis has been documented in Korea, United States, and Europe over the past decade [3,21]. The majority of the rate increase can be attributed to men who practice unsafe sexual behaviors and have a higher prevalence of co-infection with HIV. Despite the approximately six-fold increase in HIV infection in Korea over the last decade, a recent report by Kwak et al. [22] revealed that HIV-related ocular syphilis was not common in a Korean population. This result was also supported by a study by Anshu et al. [23], who reported 22 Singapore patients with syphilitic uveitis and a negative HIV serology. In the present paper, we elucidated the various non-specific presenting features of ocular syphilis in patients without HIV co-infection. In addition to key elements guiding the diagnosis of ocular syphilis, such as high-risk sexual behaviors and HIV co-infection, our results emphasize that a high index of suspicion and serological testing are crucial for diagnosing ocular syphilis even if the patients are HIV-negative.
The annual distribution of incidence in our study population (Fig. 1) did not exactly reflect the exponential increase seen in syphilis infection over the years. The reason for this outcome is unclear, but it might be due to the higher prevalence of ocular involvement of syphilis during the latent or tertiary disease phases. The natural course of syphilis indicates that latent syphilis occurs 12 months after exposure to Treponema pallidum. Latent syphilis can be maintained for 10 years and progress to persistent latent phase (30%), tertiary syphilis (40%), or spontaneous resolution (30%) [24].
In a report by Moradi et al. [21], the most common presenting feature of ocular syphilis in a U.S. population was panuveitis, regardless of HIV co-infection. In addition, isolated anterior segment inflammation was not common in HIV-negative patients. Our study revealed that posterior uveitis and panuveitis were frequent presenting features of non-HIV-related ocular syphilis, while isolated anterior inflammation was only found in 6.7% of the study population. These results were consistent with a report by Hong et al. [25], which showed panuveitis in 78.6% of all study eyes.
The recommended standard regimen for ocular syphilis is intramuscular injection of penicillin G benzathine or oral administration of doxycycline in cases of penicillin allergy. Even though our results showed no significant difference in final visual acuity between intramuscular and intravenous administration of penicillin, the intravenous aqueous penicillin G seems to decrease the recurrence of ocular inflammation. Our one recurrent case was initially treated with intramuscular injection, followed by repeated injections after confirmation of treatment failure. This supports a study by Puech et al. [26], who reported that a 10-day course of aqueous penicillin was more suitable for reduced recurrence. The overall treatment outcome following penicillin therapy was prevailing non-penicillin-treated eyes in our study. An outstanding antibiotic response and visual outcome of syphilitic uveitis have been reported in many previous studies.
According to a 2-year report from the British Ocular Syphilis Study, uveitis-related macular edema was more frequently found in HIV-negative patients, which accounted for 24% of our study population [3]. The visual outcome was particularly worse among the intravitreal injection eyes due to combined macular edema and posterior involving-uveitis in our study. More than half of those eyes (54.5%) showed visual impairment at the final visit. The greatest visual loss was 0.20 (logMAR) at baseline to 2.00 at the final visit in a patient who presented with posterior uveitis with massive retinal exudates and non-perfusion areas as well as severe macular edema. Moreover, according to the British Ocular Syphilis Study, HIV status did not significantly affect the final visual outcome, and visual impairment cases were all related to posterior segment involvement, which also showed concordance with the main outcome.
The majority of ocular structural complications was increased IOP secondary to intraocular inflammation. Approximately one-fifth of patients with syphilitic uveitis have been reported to be associated with elevated IOP [27]. According to our results, about one-third of patients (35.6%) experienced an elevated IOP, and 6 eyes (13.3%) had ocular hypertension. Among the six eyes with ocular hypertension, two responded well to topical IOP-lowering medications, while four eyes underwent glaucoma surgery. This finding is further supported by previously published studies, which revealed ocular hypertension as the most common complication among non-HIV-related cases [21,27].
While our study reveals the clinical manifestations and outcomes of non-HIV-related ocular syphilis following accurate treatment with certain clinical backgrounds, the design of the study has several limitations. Particularly due to the retrospective design, we were unable to derive results from multiple statistical analyses and failed to control confounding factors that might influence the results. Other limitations of the study include a relatively small number of patients, variety of follow-up periods, a large number of patients with no reported sexual orientation, treatment differences that may have introduced a potential for selection bias, and limited data for CSF analysis. With regard to CSF analysis, we were only able to conduct an examination in six patients due to referral to the infection internal medicine department and patient refusal to undergo the procedure. However, if ocular syphilis is highly suspected with positive serologic evaluation, a CSF analysis should be performed in every patient. Disease of the central nervous system can occur during any stage of syphilis, and CSF abnormalities have been noted in 13% of untreated primary syphilis and 25% to 40% of untreated secondary syphilis cases. Therefore, we suggest that CSF examination is indicated in patients with syphilis who demonstrate any of the following criteria: neurologic or ophthalmic signs or symptoms, evidence of active tertiary syphilis, or treatment failure.
In conclusion, non-HIV-related ocular syphilis is not common but is an important diagnosis to make, as it responds extremely well to treatment and can cause serious morbidity if untreated. Moreover, this condition may present with a variety of ocular symptoms and signs with non-specified sites of inflammation. A high index of suspicion is crucial for all ocular inflammation cases, and the evaluation of systemic signs with serologic testing is required to aid diagnosis. Even after appropriate antibiotic treatment, visual impairment and uncontrolled secondary glaucoma occurred in some cases. Posterior segment-involving uveitis at presentation was common in non-HIV-related ocular syphilis and was associated with poor visual outcome.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Aldave AJ, King JA, Cunningham ET., Jr Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433–441. doi: 10.1097/00055735-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005;20:161–167. doi: 10.1080/08820530500232092. [DOI] [PubMed] [Google Scholar]
- 3.Mathew RG, Goh BT, Westcott MC. British Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394–5400. doi: 10.1167/iovs.14-14559. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Disease web statistics system 2014 [Internet] Cheongju: Centers for Disease Control and Prevention; 2014. [cited 2014 Dec 30]. Available from: http://is.cdc.go.kr/dstat/jsp/stat/stat0001.jsp?disgun=3&discode=67,68,69. [Google Scholar]
- 5.Jones NP. The Manchester Uveitis Clinic: the first 3000 patients: epidemiology and casemix. Ocul Immunol Inflamm. 2015;23:118–126. doi: 10.3109/09273948.2013.855799. [DOI] [PubMed] [Google Scholar]
- 6.Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology. 1990;97:1281–1287. doi: 10.1016/s0161-6420(90)32419-3. [DOI] [PubMed] [Google Scholar]
- 7.Jones NP. The Manchester Uveitis Clinic: the first 3000 patients, 2: uveitis manifestations, complications, medical and surgical management. Ocul Immunol Inflamm. 2015;23:127–134. doi: 10.3109/09273948.2014.968671. [DOI] [PubMed] [Google Scholar]
- 8.Cunningham ET, Jr, Eandi CM, Pichi F. Syphilitic uveitis. Ocul Immunol Inflamm. 2014;22:2–3. doi: 10.3109/09273948.2014.883236. [DOI] [PubMed] [Google Scholar]
- 9.Barile GR, Flynn TE. Syphilis exposure in patients with uveitis. Ophthalmology. 1997;104:1605–1609. doi: 10.1016/s0161-6420(97)30089-x. [DOI] [PubMed] [Google Scholar]
- 10.Davis JL. Ocular syphilis. Curr Opin Ophthalmol. 2014;25:513–518. doi: 10.1097/ICU.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 11.Jumper JM, Machemer R, Gallemore RP, Jaffe GJ. Exudative retinal detachment and retinitis associated with acquired syphilitic uveitis. Retina. 2000;20:190–194. [PubMed] [Google Scholar]
- 12.Browning DJ. Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy, and the influence of human immunodeficiency virus status on response. Ophthalmology. 2000;107:2015–2023. doi: 10.1016/s0161-6420(00)00457-7. [DOI] [PubMed] [Google Scholar]
- 13.Margo CE, Hamed LM. Ocular syphilis. Surv Ophthalmol. 1992;37:203–220. doi: 10.1016/0039-6257(92)90138-j. [DOI] [PubMed] [Google Scholar]
- 14.Doris JP, Saha K, Jones NP, Sukthankar A. Ocular syphilis: the new epidemic. Eye (Lond) 2006;20:703–705. doi: 10.1038/sj.eye.6701954. [DOI] [PubMed] [Google Scholar]
- 15.Ghanem KG, Moore RD, Rompalo AM, et al. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS. 2008;22:1145–1151. doi: 10.1097/QAD.0b013e32830184df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eandi CM, Neri P, Adelman RA, et al. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012;32:1915–1941. doi: 10.1097/IAE.0b013e31825f3851. [DOI] [PubMed] [Google Scholar]
- 17.Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Transm Infect. 2011;87:4–8. doi: 10.1136/sti.2010.043042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaratunge BC, Camuglia JE, Hall AJ. Syphilitic uveitis: a review of clinical manifestations and treatment outcomes of syphilitic uveitis in human immunodeficiency virus-positive and negative patients. Clin Experiment Ophthalmol. 2010;38:68–74. doi: 10.1111/j.1442-9071.2010.02203.x. [DOI] [PubMed] [Google Scholar]
- 19.Shalaby IA, Dunn JP, Semba RD, Jabs DA. Syphilitic uveitis in human immunodeficiency virus-infected patients. Arch Ophthalmol. 1997;115:469–473. doi: 10.1001/archopht.1997.01100150471003. [DOI] [PubMed] [Google Scholar]
- 20.Li JZ, Tucker JD, Lobo AM, et al. Ocular syphilis among HIV-infected individuals. Clin Infect Dis. 2010;51:468–471. doi: 10.1086/654797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moradi A, Salek S, Daniel E, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334–343.e1. doi: 10.1016/j.ajo.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 22.Kwak HD, Kim HW, Lee JE, et al. Clinical manifestations of syphilitic uveitis in the Korean population. J Korean Ophthalmol Soc. 2014;55:555–562. [Google Scholar]
- 23.Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008;92:594–597. doi: 10.1136/bjo.2007.133843. [DOI] [PubMed] [Google Scholar]
- 24.Lautenschlager S. Diagnosis of syphilis: clinical and laboratory problems. J Dtsch Dermatol Ges. 2006;4:1058–1075. doi: 10.1111/j.1610-0387.2006.06072.x. [DOI] [PubMed] [Google Scholar]
- 25.Hong MC, Sheu SJ, Wu TT, Chuang CT. Ocular uveitis as the initial presentation of syphilis. J Chin Med Assoc. 2007;70:274–280. doi: 10.1016/S1726-4901(07)70004-7. [DOI] [PubMed] [Google Scholar]
- 26.Puech C, Gennai S, Pavese P, et al. Ocular manifestations of syphilis: recent cases over a 2.5-year period. Graefes Arch Clin Exp Ophthalmol. 2010;248:1623–1629. doi: 10.1007/s00417-010-1481-z. [DOI] [PubMed] [Google Scholar]
- 27.Reddy S, Cubillan LD, Hovakimyan A, Cunningham ET., Jr Inflammatory ocular hypertension syndrome (IOHS) in patients with syphilitic uveitis. Br J Ophthalmol. 2007;91:1610–1612. doi: 10.1136/bjo.2007.123174. [DOI] [PMC free article] [PubMed] [Google Scholar]