Abstract
Introduction
Urothelium is a highly specialized type of epithelium covering the interior of the urinary tract. One of the structures responsible for its unique features are urothelial plaques formed from glycoprotein heteropolymers, the uroplakins. Four types of uroplakins are known – UPIa, UPIb, UPII, UPIII. Herein we review the current status of knowledge about uroplakins and discuss their potential clinical applications.
Material and methods
A PubMed search was conducted to find original and review papers about uroplakins.
Results
Uroplakins can be detected in tissue, urine and blood. The process of urothelial plaque formation is complex and its disturbances resulting in incorrect plaque formation might be responsible for some pathological states. Additionally, uroplakins might be associated with other pathological processes i.e. urothelial cancer or infections of the urinary tract.
Conclusions
Uroplakins as the end-product of urothelial cells have unique features and a complex structure. These glycoproteins can be involved in some diseases of the urinary tract and as such can be used as potential targets for intervention and markers of the disease.
Keywords: uroplakin, urothelium, urothelial cancer, interstitial cystitis, vesicoureteral reflux, urinary tract infection
INTRODUCTION
Urothelium is a highly specialized structure, which primary function is to protect against penetration of toxic substances from the urine back into the body. It lines the renal pelvis, ureter, bladder and partially the urethra – the structures that are in constant contact with urine. Urothelium is considered to be transitional epithelium, despite the fact that superficial layers of the epithelium are not connected with the basal membrane. This epithelium is unique in its properties (e.g., electrical resistance of 75000 Ω/cm2, which is higher than the epidermis, which separates the organism from the external environment), and that is mainly attributable to uroplakins [1]. The aim of this article is to show possible clinical applications of uroplakins.
MATERIAL AND METHODS
A PubMed search was performed using the keyword ‘uroplakin’. The database of articles was closed on 01 Apr 2015. 443 records were retrieved and all publications were read and assessed for significance. References of selected articles were also analyzed for significance.
Structure and functions of uroplakins
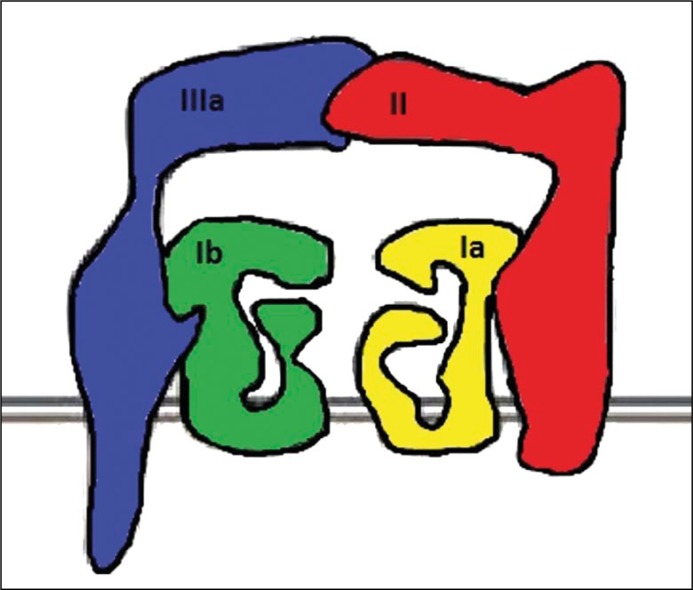
Uroplakins are cell membrane proteins, which form urothelial plaques on the surface of each urothelial cell. Four types of uroplakins are known in humans – UPIa, UPIb, UPII, UPIII. Uroplakins Ia, Ib and III are glycoproteins and their sugar residues are very important elements in the process of synthesis and are necessary for their proper function. Mature form of uroplakin II is deprived of a sugar residue. Uroplakins Ia (27kDa) and Ib (28kDa) are transmembrane proteins with four transmembrane chains coupled with two hydrophilic fragments on the inner side of the bladder and with one fragment localized in the cell plasma. Because of this structure, they are classified as tetraspanins; a superfamily of transmembrane scaffolding proteins responsible for cell adhesion, motility, activation and proliferation [2]. Uroplakin II (15kDa) and UPIII have one transmembrane domain with the C-terminus in the cell plasma and the N-terminus in the intravesical space. There are several isoforms of UPIII. UPIIIa (47kDa) is a dominant form, the most common in humans and the most studied. There are also UPIIIb (35kDa) and the recently found UPIIIc [3]. Synthesis of uroplakins is complex and partially takes place in the endoplasmatic reticulum (ER). In the ER, monomers of uroplakins form heterodimers – UPIa with UPII and UPIb with UPIIIA. These pairs of uroplakins are than embedded into the lipid membrane and further heterotetramerization takes place in the follicles in the area of the Golgi apparatus. Uroplakins heterotetramers then undergo association into hexamers, which are the mature form of urothelial plaques and are about 16 nm in size [1, 4].
The main part of this complex is extracellular and is turned with its external part toward the urinary system. For this reason they are called asymmetric unit membrane (AUM – Figure 1) [4]. Similar AUMs are found in all mammals, despite some differences in the structure of the urothelium. As much as 90% of urothelium is covered with uroplakins. The remaining 10% of urothelium constitutes uncovered cellular membrane surface which form flexible regions. These regions together with the elements of the cytoskeleton take part in folding and the changing of the bladder capacity. After emptying the bladder the excess uroplakins are dragged into the cell, which causes reduction of uroplakin covered surface. Uroplakins come to the urothelial surface again in response to the rising volume of bladder – filling the bladder with urine [4, 5].
Figure 1.
Schematic drawing of a uroplakin heterotetramer.
Uroplakins are detectable in fetal life. Research on animals suggests that uroplakins are not only the final products of urothelial cells but they also play a role in organogenesis, particularly in nephrogenesis. The presence of UPII and UPIII has been confirmed in the renal pelvis and urogenital sinus already in the 7-week-old fetus [6, 7]. The role of UPKs is still a matter of intensive research but several facts have come into light. Deletion of the UPII gene leads to total absence of urothelial plaques. This causes penetration of water and substances dissolved in urine into deeper layers [1, 8]. The absence of UPII and UPIIIa results in the inappropriate development of superficial urothelial cells. Abnormal urothelium undergoes hypertrophy followed by urine outflow and vesicoureteral reflux (VUR) [2, 6, 8, 9, 10]. Deletion of uroplakin genes or changes in reading frames, results in death within the first year of life or even in the prenatal period [11].
Uroplakins in urinary tract infections
Infections of urinary tract (UTIs) are the second most common group of systemic infections – after infections of respiratory tract – which constitute a considerable problem for the health care system [12, 13]. Uropathogenic strains of E. coli (UPEC) are responsible for approximately 85% of these infections. They are able to colonize urinary tracts through the interaction between bacterial molecules like: type I-fimbrias, P-fimbrias, lectins, and urothelial glycoprotein fragments containing mannose [14, 15, 16]. Expression of these mannose-rich fragments is a more important factor in infection occurrence than pathogenicity of E. coli strains itself [17]. Bacterial adhesion to the urothelium is possible through the interaction between adhesion molecules of FimH and mannose fragments of subunit UPIa of urothelial plaques. UPII and UPIII do not participate in this reaction. This mechanism may be responsible for ascending infections as UPI is present in all urothelial plaques as well as in the ureter and renal pelvis [1]. Similarly, in the upper urinary tract P-fimbria of E. coli participate in pathogenesis of pyelonephritis [18]. Except for adhesion, connection of UPEC fimbriae with UPIa/Ib starts reactions which allow E. coli to invade and create an intercellular population of bacteria. This population is able to proliferate and to form intercellular bacterial communities (IBCs), which are probably responsible for recurrent urinary tract infections because of their antibiotic resistance [19, 20]. Moreover, the increased amount of mannose rich membrane glycoproteins in diabetes mellitus patients is significantly associated with greater sensitivity to E. coli infections due to the adherence of FimH to mannose [21]. The recurrence rate of UTI in diabetic women is about 1.4 times higher than in groups of non-diabetic women [22].
Those observations lead to the conclusion that uroplakins might be a potential target for urinary tract infection prevention and treatment. Firstly, by disrupting the interaction between E. coli and urothelium one might try to lower the chance of developing an infection especially in patients with elevated risk. Secondly, one might speculate that in patients with urinary tract infection, disruption of bacteria-urothelium interaction might lead to spontaneous healing and prevention of ascending infection. Thirdly, disruption of UPK-bacteria interaction could theoretically prevent the development of intracellular bacterial communities leading to decreasing the number of patients with recurrent UTIs.
Uroplakins in urothelial cancer diagnostics and treatment
Urothelium lines the renal pelvis, ureter, bladder and partially the urethra. Functions of uroplakins in malignancies are not well understood. Research on UPII has shown that it is a histochemical marker of high specificity and moderate sensitivity in detection of primary and metastatic urothelial cancers [23]. The presence of UPIII is confirmed in about 60–66% of primary cancers and in 53% of cases of metastatic disease. The amount of detectable uroplakin is not correlated with cancer stage [24].
Due to specificity of uroplakins for urinary urothelium, detection of uroplakins in cancer tissue points with high probability to a urothelial origin of cancer. This characteristic is useful in distinguishing anaplastic malignancies, distinguishing metastases to urinary tract from primary urothelial malignancies or identifying urothelial cancer metastases to other organs.
Uroplakin III has also been found and is measurable in urine by enzyme-linked immunosorbent assay (ELISA). Lai et al. showed significantly higher concentration of UPIII in patients with bladder cancer than in those with benign diseases of urinary tract and healthy subjects [25].
Uroplakins and their fragments were also detected in the blood of patients with urothelial cancer. Research on monoclonal antibodies (Ab) anti-uroplakin IIIa and anti-uroplakin II showed, that anti-UPII Ab react with both membranous and intercellular elements, whereas antibodies against UPIIIa react only with membranous elements. It seems possible to use uroplakins as markers of cancer cells, which could be determinants of process activity, treatment response and intangible clinical metastatic disease [26, 27].
Due to the fact that uroplakins are mainly markers of well-differenced urothelial cells, they could also be used as a target for treatment. Currently, new antibodies conjugated with chemotherapeutic agents or radiopharmaceuticals are being investigated. Their aim is selective delivery to cancer cell, omitting healthy cells. Advances in this field have been described by Wang, who has used UP II promoter conjugated with a reporter vector to create a bladder cancer specific vector [28]. Therapy of metastatic urothelial cancer could be improved by to this highly selective therapy. Drug delivery to uroplakin containing tissue reactive with anti-UP antibody would result in therapy effectiveness improvement and reduction of therapy related toxicity.
Research on immunohistochemical markers used in diagnostics of primary and metastatic lung cancer has also shown usefulness of UPIII. Aaron et al. proved that the presence of UPIII, S100P and GATA-3 in lung cancer material was related to urothelial neoplasms. This trial involved 30 patients with pulmonary metastases of urothelial cancer. UPIII was detected in 71% of metastases and histopathological verification was performed [29].
Isotope conjugated antibody could be used in high sensitive and specific medical imaging like positron emitting tomography (PET) and single-photon emission computed tomography (SPECT). The example of such use is girentuximab – chimeric monoclonal antibody against carbonic anhydrase, which is conjugated with In-111 isotope and is used in diagnostics of primary and metastatic foci of renal cell carcinoma (RCC) [30]. Such an approach is also possible when using UPKs as a target for both diagnostic purposes analogically to the mentioned example and for treatment. Antibody conjugated with high-energy emitter could theoretically selectively bind to UPK containing cells and deliver radiation selectively to metastatic foci.
Uroplakins in diagnosis of vesicoureteral reflux
Vesicoureteral reflux (VUR) is a disease in which urine flows in a retrograde direction from the bladder into the ureters and renal pelvises. In normal condition urine flows in one direction – downward from the kidneys. The ureterovesical junction plays a main role in physiological urine flow, as a one way valve. There are two types of VUR, depending on their onset: primary and secondary VUR.
The possibility of improvement of VUR diagnostics was proposed by Iwaki et al. who has detected an increased expression of uroplakin III mRNA, measured by quantitative methods in urine and bladder tissue of patients with VUR [31]. Specificity and sensitivity of this method in detecting VUR reached 77.8%, and 76.3% respectively. These results, however, are strictly dependent on the patient’s clinical status. In a group of patients without past infections of the urinary tract, specificity was 100%, but sensitivity only 50%. The authors of this work tried to explain higher expression of UP III mRNA, by the defect in product of this gene (UP III protein), which occurs in patients with VUR. It is clear that these results need to be confirmed in larger groups, but this correlation could be a basis for creation of a non-invasive diagnostic test.
There is a possibility of using a urine uroplakin test in combination with ultrasound in early childhood as a non-invasive screening method for VUR detection and possibly follow-up. This method would be less invasive than voiding cystourethrogram (VCUG) in children and better in follow-up.
Presently, only radiological examinations are able to detect congenital disorders of the urinary system during foetal life. Creation of diagnostic tests could improve prenatal diagnosis in these disorders, which occur in 3% of pregnancies (remembering about the significant numer of non-significant VURs). There is the possibility of testing uroplakin concentration in amniotic fluid due to the large amount of foetal urine in it. The research of Kong et al. showed the presence of UPII in stem cells of amniotic fluid [8]. Additional research is needed to investigate whether amount changes of these and other uroplakin-containing cells are connected with congenital disorders of the urinary system.
Interstitial cystitis
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a disease of uncertain etiology which is represented by numerous unspecific symptoms. Frequent and painful urination are the most common representations and women constitute about 90% of patients [32].
There are many theories of etiology and pathophysiology of this disease. Many of them tried to explain it by post infectious, neurogenic or autoimmunologic causes. Damage of the superficial glycosaminoglycan layer of urothelium is probably a consequence of the listed causes. This damage can increase permeability of the urothelium (‘leaky urothelium’), which is suggested by Parsons [33]. Irritating substances contained within urine permeate into deeper layers and affect bladder tissue and local nerves. In healthy persons the bladder protective and sealing function is mainly determined by the superficial layer of glycosaminoglycans where uroplakins are the central glycoproteins. Damage to this layer increases permeability of urothelium. The most damaging factors are: bacteria, foreign bodies, and chemicals. Decreased amount of glycosaminoglycans in the urine of patients with IC/PBS confirms this theory. Research on animal models has also confirmed it. For example, Altuntas et al. has shown that mice immunized to UPIII by intravesical infusion have demonstrated typical symptoms of interstitial cystitis (experimental autoimmune cystitis – EAC) [34]. Also, research by Keay et al. proved impaired repair and thinning of the glycosaminoglycan layer in mouse model with IC/PBS [35].
Hauser et al. examined tissue from bladder biopsies of IC.PBS patients. The largest abnormalities were observed in the amount of keratin – 18 (80%), keratin – 20 (87.5%) and uroplakins (56%) [36]. Likewise, other researchers have shown lower expression of urothelial surface proteins and their inappropriate arrangement in rodents with IC/PBS [37] and damage of tight junctions seen in the electron microscope [38]. Abnormalities in the amount and location of uroplakins have been also confirmed in 50% of cats with IC/PBS (FIC – feline interstitial cystitis) [39].
Lower amount of uroplakins detected in bladder tissue in patients with nonulcerative IC/PBS is connected with lower expression of mRNa of UPIa, UPIb and UPII with the exception of UPIII mRNA, especially UP III-delta4 [40]. Due to this reason UP III-delta4 is a potential marker of IC/PBS.
Especially interesting for further research would be comparing the amount of urinary uroplakins between patients with IC, other pathologies of urinary tract and healthy persons. This research might shed some light into whether those glycoproteins play a role in this disease. Additionally, one might imagine rebuilding the layer of glycosaminoglycans by restoring normal uroplakin function.
CONCLUSIONS
Urothelium is a highly specialized structure with special characteristic features. Uroplakins as end-product of urothelial cells have unique features and a complex structure. They are necessary for the urinary tract to function properly. Knowledge about them provides us with a new viewpoint for well known diseases. Uroplakins could become a clinically significant diagnostic or therapeutic aim of many urinary tract disorders. However, more studies are needed to gain better knowledge about uroplakins.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Wu XR, Kong XP, Pellicer A, Kreibich G, Sun TT. Uroplakins in urothelial biology, function, and disease. Kidney Int. 2009;75:1153–1165. doi: 10.1038/ki.2009.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee G. Uroplakins in the lower urinary tract. Int Neurourol J. 2011;15:4–12. doi: 10.5213/inj.2011.15.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desalle R, Chicote JU, Sun TT, Garcia-España A. Generation of divergent uroplakin tetraspanins and their partners during vertebrate evolution: identification of novel uroplakins. BMC Evol Biol. 2014;14:13. doi: 10.1186/1471-2148-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lis J, Kątnik-Prastowska I, Tupikowski K, Matejuk A. Uroplakins as markers of diseases of the urinary system. Postepy Hig Med Dosw. 2015;69:98–113. [PubMed] [Google Scholar]
- 5.Lewis S.A. Everything you wanted to know about the bladder epithelium but were afraid to ask. Am J Physiol Renal Physiol. 2000;278:F867–874. doi: 10.1152/ajprenal.2000.278.6.F867. [DOI] [PubMed] [Google Scholar]
- 6.Jenkins D, Bitner-Glindzicz M, Malcolm S, Hu C.C, Allison J, Winyard PJ, et al. De novo uroplakin IIIa heterozygous mutations cause human renal adysplasia leading to severe kidney failure. J Am Soc Nephrol. 2005;16:2141–2149. doi: 10.1681/ASN.2004090776. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins D, Woolf AS. Uroplakins: new molecular players in the biology of urinary tract malformations. Kidney Int. 2007;71:195–200. doi: 10.1038/sj.ki.5002053. [DOI] [PubMed] [Google Scholar]
- 8.Kong XT, Deng FM, Hu P, et al. Roles of uroplakins in plaque formation, umbrella cell enlargement, and urinary tract diseases. J Cell Biol. 2004;167:1195–1204. doi: 10.1083/jcb.200406025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu P, Deng FM, Liang FX, et al. Ablation of uroplakin III gene results in small urothelial plaques, urothelial leakage, and vesicoureteral reflux. J Cell Biol. 2000;151:961–972. doi: 10.1083/jcb.151.5.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu P, Meyers S, Liang FX, et al. Role of membrane proteins in permeability barrier function: uroplakin ablation elevates urothelial permeability. Am J Physiol. Renal Physiol. 2002;283:F1200–1207. doi: 10.1152/ajprenal.00043.2002. [DOI] [PubMed] [Google Scholar]
- 11.Scott JE. Fetal, perinatal, and infant death with congenital renal anomaly. Arch Dis Child. 2002;87:114–117. doi: 10.1136/adc.87.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown P. Epidemiology of urinary tract infections: transmission and risk factors, incidence, and costs. Infect Dis Clin North Am. 2003;17:227–241. doi: 10.1016/s0891-5520(03)00005-9. [DOI] [PubMed] [Google Scholar]
- 13.Ali AB, Bagnis AC. Urinary tract infections in adults. Rev Prat. 2014;64:1358. [PubMed] [Google Scholar]
- 14.Langermann S, Palaszynski S, Barnhart M, et al. Prevention of mucosal Escherichia coli infection by FimH-adhesin-based systemic vaccination. Science. 1997;276:607–611. doi: 10.1126/science.276.5312.607. [DOI] [PubMed] [Google Scholar]
- 15.Ofek I, Hasty DL, Abraham S.N, Sharon N. Role of bacterial lectins in urinary tract infections. Molecular mechanisms for diversification of bacterial surface lectins. Adv Exp Med Biol. 2000;485:183–192. doi: 10.1007/0-306-46840-9_25. [DOI] [PubMed] [Google Scholar]
- 16.Sokurenko EV, Chesnokova V, Dykhuizen DE, et al. Pathogenic adaptation of Escherichia coli by natural variation of the FimH adhesin. Proc Natl Acad Sci USA. 1998;95:8922–8926. doi: 10.1073/pnas.95.15.8922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouckaert J, Mackenzie J, de Paz JL, et al. The affinity of the FimH fimbrial adhesin is receptor-driven and quasi-independent of Escherichia coli pathotypes. Mol Microbiol. 2006;61:1556–1568. doi: 10.1111/j.1365-2958.2006.05352.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts JA, Marklund BI, Ilver D, et al. The Gal(α 1-4) Gal-specific tip adhesin of Escherichia coli P-fimbriae is needed for pyelonephritis to occur in the normal urinary tract. Proc Natl Acad Sci USA. 1994;91:11889–11893. doi: 10.1073/pnas.91.25.11889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson GG, Dodson KW, Hooton TM, Hultgren SJ. Intracellular bacterial communities of uropathogenic Escherichia coli in urinary tract pathogenesis. Trends Microbiol. 2004;12:424–430. doi: 10.1016/j.tim.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Anderson GG, Palermo JJ, Schilling JD, Roth R, Heuser J, Hultgren SJ. Intracellular bacterial biofilm-like pods in urinary tract infections. Science. 2003;301:105–107. doi: 10.1126/science.1084550. [DOI] [PubMed] [Google Scholar]
- 21.Taganna J, de Boer AR, Wuhrer M, Bouckaert J. Glycosylation changes as important factors for the susceptibility to urinary tract infection. Biochem Soc Trans. 2011;39:349–354. doi: 10.1042/BST0390349. [DOI] [PubMed] [Google Scholar]
- 22.Geerlings SE. Urinary tract infections in patients with diabetes mellitus: epidemiology, pathogenesis and treatment. Int J Antimicrob Agents. 2008;(Suppl 1):S54–57. doi: 10.1016/j.ijantimicag.2007.07.042. [DOI] [PubMed] [Google Scholar]
- 23.Moll R, Wu XR, Lin JH, Sun TT. Uroplakins, specific membrane proteins of urothelial umbrella cells, as histological markers of metastatic transitional cell carcinomas. Am J Pathol. 1995;147:1383–1397. [PMC free article] [PubMed] [Google Scholar]
- 24.Kaufmann O, Volmerig J, Dietel M. Uroplakin III is a highly specific and moderately sensitive immunohistochemical marker for primary and metastatic urothelial carcinomas. Am J Clin Pathol. 2000;113:683–687. doi: 10.1309/PYQC-17CB-063T-Q07J. [DOI] [PubMed] [Google Scholar]
- 25.Lai Y, Ye J, Chen J, et al. UPK3A: a promising novel urinary marker for the detection of bladder cancer. Urology. 2010;76:514. doi: 10.1016/j.urology.2009.11.045. [DOI] [PubMed] [Google Scholar]
- 26.Li SM, Zhang ZT, Chan S, et al. Detection of circulating uroplakin-positive cells in patients with transitional cell carcinoma of the bladder. J Urol. 1999;162:931–935. doi: 10.1097/00005392-199909010-00093. [DOI] [PubMed] [Google Scholar]
- 27.Yuasa T, Yoshiki T, Isono T, Tanaka T, Hayashida H, Okada Y. Expression of transitional cell-specific genes, uroplakin Ia and II, in bladder cancer: detection of circulating cancer cells in the peripheral blood of metastatic patients. Int J Urol. 1999;6:286–292. doi: 10.1046/j.1442-2042.1999.00064.x. [DOI] [PubMed] [Google Scholar]
- 28.Wang D, Wang Z, Tian J, et al. Prostate stem cell antigen enhancer and uroplakin II promoter based bladder cancer targeted tissue-specific vector. Urol Oncol. 2010;28:164–169. doi: 10.1016/j.urolonc.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Gruver AM, Amin MB, Luthringer DJ, et al. Selective immunohistochemical markers to distinguish between metastatic high-grade urothelial carcinoma and primary poorly differentiated invasive squamous cell carcinoma of the lung. Arch Pathol Lab Med. 2012;136:1339–1346. doi: 10.5858/arpa.2011-0575-OA. [DOI] [PubMed] [Google Scholar]
- 30.Muselaers CH, Boerman OC, Oosterwijk E, Langenhuijsen JF, Oyen WJ, Mulders PF. Indium-111-labeled girentuximab immunoSPECT as a diagnostic tool in clear cell renal cell carcinoma. Eur Urol. 2013;63:1101–1106. doi: 10.1016/j.eururo.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 31.Iwaki H, Johnin K, Kageyama S, Kim CJ, Isono T, Yoshiki T. Up-regulation of urinary UPIII mRNA levels in vesicoureteral reflux patients: potential application as a screening test for vesicoureteral reflux. Int J Urol. 2007;14:918–923. doi: 10.1111/j.1442-2042.2007.01861.x. [DOI] [PubMed] [Google Scholar]
- 32.Curhan GC, Speizer FE, Hunter DJ, Curhan SG, Stampfer MJ. Epidemiology of interstitial cystitis: a population based study. J Urol. 1999;161:549–552. [PubMed] [Google Scholar]
- 33.Teichman JM, Parsons CL. Contemporary clinical presentation of interstitial cystitis. Urology. 2007;(4 Suppl):41–47. doi: 10.1016/j.urology.2006.08.1111. [DOI] [PubMed] [Google Scholar]
- 34.Altuntas CZ, Daneshgari F, Sakalar C, Goksoy E, Gulen MF, et al. Autoimmunity to uroplakin II causes cystitis in mice: a novel model of interstitial cystitis. Eur Urol. 2012;61:193–200. doi: 10.1016/j.eururo.2011.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keay S, Leitzell S, Ochrzcin A, Clements G, Zhan M, Johnson D. A mouse model for interstitial cystitis/painful bladder syndrome based on APF inhibition of bladder epithelial repair: a pilot study. BMC Urol. 2012;12:17. doi: 10.1186/1471-2490-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hauser PJ, Dozmorov MG, Bane BL, Slobodov G, Culkin DJ, Hurst RE. Abnormal expression of differentiation related proteins and proteoglycan core proteins in the urothelium of patients with interstitial cystitis. J Urol. 2008;179:764–769. doi: 10.1016/j.juro.2007.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lv YS, Yao YS, Rong L, et al. Intravesical hyaluronidase causes chronic cystitis in a rat model: A potential model of bladder pain syndrome/interstitial cystitis. Int J Urol. 2014;21:601–607. doi: 10.1111/iju.12358. [DOI] [PubMed] [Google Scholar]
- 38.Funahashi Y, Yoshida M, Yamamoto T, Majima T, Takai S, Gotoh M. Intravesical application of rebamipide promotes urothelial healing in a rat cystitis model. J Urol. 2014;192:1864–1870. doi: 10.1016/j.juro.2014.06.081. [DOI] [PubMed] [Google Scholar]
- 39.Hauser PJ, VanGordon SB, Seavey J, et al. Abnormalities in Expression of Structural, Barrier, and Differentiation Related Proteins and Chondroitin Sulfate in the Urothelium of Cats with Feline Interstitial Cystitis Mimic Those Seen in Human Interstitial Cystitis. J Urol. 2015;194:571–577. doi: 10.1016/j.juro.2015.01.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zeng Y, Wu XX, Homma Y, et al. Uroplakin III-delta4 messenger RNA as a promising marker to identify nonulcerative interstitial cystitis. J Urol. 2007;178:1322–1327. doi: 10.1016/j.juro.2007.05.125. [DOI] [PubMed] [Google Scholar]