Abstract
Objective To describe the evidence about factors influencing breast cancer patients’ surgery choices and the implications for designing decision support in reference to an extended Theory of Planned Behaviour (TPB) and the Common Sense Model of Illness Representations (CSM).
Background A wide range of factors are known to influence the surgery choices of women diagnosed with early breast cancer facing the choice of mastectomy or breast conservation surgery with radiotherapy. However, research does not always reflect the complexities of decision making and is often atheoretical. A theoretical approach, as provided by the CSM and the TPB, could help to identify and tailor support by focusing on patients’ representations of their breast cancer and predicting surgery choices.
Design Literature search and narrative synthesis of data.
Synthesis Twenty‐six studies reported women’s surgery choices to be influenced by perceived clinical outcomes of surgery, appearance and body image, treatment concerns, involvement in decision making and preferences of clinicians. These factors can be mapped onto the key constructs of both the TPB and CSM and used to inform the design and development of decision support interventions to ensure accurate information is provided in areas most important to patients.
Conclusions The TPB and CSM have the potential to inform the design of decision support for breast cancer patients, with accurate and clear information that avoids leading patients to make decisions they may come to regret. Further research is needed examining how the components of the extended TPB and CSM account for patients’ surgery choices.
Keywords: breast cancer surgery, common sense model of illness representations, decision aids, decision support interventions, decision making, theory of planned behaviour
Background
Women diagnosed with early breast cancer (stage I or II) are typically offered the choice between two surgical treatments: mastectomy or breast conservation surgery with radiotherapy (BCS). Survival rates are equivalent, 1 , 2 although BCS is associated with higher local recurrence, 3 leading to the assumption that, when offered the choice, women would elect BCS. 4 However, uptake has not been consistent, with wide variation in surgical management. 5 , 6 This variation indicates the need for further research into the potential patient and professional causative factors and ways of supporting patients in making this complex and difficult decision. 5 Research in this area does not always reflect the complexities of decision making 7 and is often atheoretical, 8 despite there being theories, which have been effectively used to predict other health‐related behaviours. 22 , 23 , 24 A theoretical analysis of the factors influencing breast cancer patients’ surgery choices could provide a more structured way of exploring these factors, thereby enhancing understanding of the variation in treatment uptake. Identifying these factors would help to identify and tailor ways of supporting women facing this decision.
The period between diagnosis and treatment for breast cancer is particularly stressful because of uncertainty about the disease and pressure to make rapid treatment decisions. 9 Newly diagnosed breast cancer patients display high levels of distress, with a loss of effectiveness in key cognitive activities, 10 raising concern over the psychological impact of being offered a role in decision making for surgery. 9 The extent to which patients are affected by their emotional reaction to their diagnosis may be closely related to their ability to plan their medical care. 11 Fear, intense emotional reactions to diagnosis and time pressures can leave women feeling overwhelmed, unable to process the information or take on the responsibility in decision making. 11 This may be further compounded by the fact that to make an informed choice, patients have to digest a lot of information, and the way in which it is presented may impact on the decision they make. 12 Some, however, may find the decision making process a challenge 9 and a useful psychological distraction, emotionally preparing them for surgery. 13
A range of factors are reported to influence the surgical choices of early breast cancer patients. These include concerns about breast loss and local tumour recurrence, perceived surgeon preferences, 14 patient involvement in decision making, 15 media reports, 16 body image, 17 perceived chance of survival, 18 avoidance of radiation treatments, 19 patient–professional communication, 19 surgeon’s input and clinical guidance. 16 , 20 , 21
Two key theoretical frameworks that have been applied to health‐related decision making are the Theory of Planned Behaviour (TPB) 22 , 23 and the Common Sense Model of Illness Representations (CSM). 24 With its roots in rational models of decision making, the TPB has been extensively used to predict and explain a range of behaviours, including health behaviours. Social cognitive approaches such as the TPB are based on the assumption that a rational and methodical decision making process can predict health behaviours. 25 However, given the potential impact of a breast cancer diagnosis on well‐being, decision making in this context may not be as rational as the TPB implies. The CSM provides a complementary framework for understanding how patients make sense of their condition and their perceptions of the treatments available to them, placing greater emphasis on emotional and coping responses when accounting for illness‐related behaviour. While the CSM examines how the broader representation of an illness helps a patient deal with that illness, the TPB looks to predict what the patient decides to do. The predictive ability of both the TPB and CSM have been applied to intentions to attend prostate specific antigen screening, 26 cervical screening attendance 27 and to women’s perceptions of breast cancer symptoms and help‐seeking intentions. 28 , 29 While the TPB has been found to be a better predictor of intentions, it is the combination of the two models that provides a better understanding of the observed health behaviours, 27 , 28 , 29 although evidence of this with regard to breast cancer patients’ surgery choices is lacking.
Objective
To describe the evidence concerning factors influencing breast cancer patients’ surgery choices and to interpret and discuss this with reference to the constructs of the extended TPB and the CSM. This will provide a basis for examining the implications for practice, more specifically the ways in which early breast cancer patients can be supported when choosing their surgery.
Search strategy
Ten electronic databases (Medline, CINAHL, EBM Reviews, EMBASE, PsycINFO, ASSIA, Social Science Citation Index, ISI Science Citation Index, SIGLE and ZETOC) were searched up to November 2007. The reference lists of key review articles 7 , 9 , 13 , 18 were also searched. The key search terms were ‘breast cancer’, ‘surgery’, ‘mastectomy’, ‘breast conservation surgery’, ‘treatment choice’, ‘psychological theory’, ‘models of health behaviour’, ‘TPB’/’Theory of Planned Behaviour’, ‘CSM’/’Common Sense Model’ and Self‐Regulatory Model.
Inclusion criteria
Studies reporting data concerning factors influencing the surgery choices of women diagnosed with early breast cancer.
Exclusion criteria
Studies that did not include women diagnosed with early breast cancer and/or provide data on the reasons for their surgery choices.
Results
Our search strategy yielded 1818 articles; 149 were put forward for inclusion in this review of which 123 were excluded. Summaries of the 26 included articles are provided in Table S1.
Perceived influences on patients’ surgery choices
Surgery outcomes: clinical benefits and risks
Ten studies reported the clinical benefits and risks of surgery to be important factors considered by breast cancer patients, with the possibility of curing their breast cancer and the chance of it recurring among the most significant issues. 11 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 Three studies reported fears of cancer recurrence and worries about the effects of radiation following BCS to be key concerns of patients opting for mastectomy. 14 , 31 , 36 Patients choosing BCS are reported to want to keep their breast if chances of survival are equivalent with mastectomy. 33 , 35 However, decisions to undergo mastectomy may be based on inaccurate perceptions of the risks, with five studies reporting patients who opted for mastectomy perceiving this procedure to be the most effective and definitive treatment, offering a better chance of survival than BCS. 14 , 32 , 34 , 37 , 39
Surgery outcomes: appearance and body image
Seven studies reported concerns about appearance post‐surgery to influence choices. 8 , 11 , 14 , 30 , 36 , 39 , 40 Two studies reported attitudes to body image and sexuality to also influence choice. 11 , 14 Patients opting for BCS place a greater emphasis on these factors, 39 perceiving the outcome to be less disfiguring, 36 allowing them to conserve their femininity, physical appearance and sexuality. 40 Older women may not attach the same importance to these factors, with some feeling that their breast is no longer important to them in terms of sexual attractiveness or appearance. 8
Treatment concerns
Three studies 14 , 35 , 41 reported on the practicalities of likely treatment following surgery and the implications of these for patients’ surgery choices. Some patients are concerned about restrictions in travel if they were to undergo radiation treatment, more common following BCS, 14 , 41 with anecdotal evidence that breast cancer patients in rural areas of Western Australia tended to choose mastectomy rather than BCS. 35 Concerns about the duration of the treatment itself have also been found to influence surgery choices. 41
Involvement in decision making process
Six studies reported that involvement in the decision making process influenced patients. 11 , 15 , 36 , 39 , 42 , 43 Some patients prefer to make their own choice, or to make treatment decisions in collaboration with their clinician, 44 particularly when they realise they have options, 45 whereas others prefer the surgeon to make that decision for them. 37 The degree to which the clinician allows or encourages patient participation in the decision making process is often reflected in the choice of surgery, such that the decision reflects the preferences of the person with greater control over the process. 11 Not all patients perceived that they were offered a choice, despite being eligible. 39 The extent to which patients are involved in the decision making process may also be influential, although the evidence is inconsistent; three studies found that patients more involved in the decision making process were more likely to opt for mastectomy 15 , 36 , 39 with another study reporting that women opting for BCS preferred a more active decision making role than those opting for mastectomy. 35
Perceived preferences of clinicians, as perceived by patients
Eleven studies found patients’ perceptions of their surgeon’s treatment preference to be one of the most influential factors on treatment choice. 14 , 31 , 32 , 34 , 35 , 40 , 44 , 46 , 47 , 48 , 49 Even where patients perceive there to be an option, they are likely to comply with perceived recommendation of their surgeon, often overriding other factors important to them. 14 , 31 , 32 , 34 , 40 , 44 , 46 , 47 , 48 As a primary and specialist source of information, 32 , 46 surgeons are viewed as experts and patients often do not feel qualified to question them. 37 One study found that women who underwent BCS rated their surgeon’s preferences as a more important factor influencing their decision making than women who underwent mastectomy. 35 Another study found the surgeon to be the most significant factor in patients’ decision to choose BCS; 49 however, where patients wanted mastectomy, their fear of cancer overshadowed their surgeon’s input. In the absence of a recommendation, patients may attempt to ascertain what their surgeon’s preference would be. 44
Preferences of patients, as perceived by clinicians
Surgeons may not perceive the decision making in the same way as their patients, 50 or realise that they are highly influential in their patients’ decision making. 41 The discipline of the health care professional can also influence choice. Where BCS is standard care, consultation with the medical oncologist was found to be unrelated to type of surgery, although it was associated with satisfaction with treatment choice. 51 Where BCS is not the standard care, consultation with a medical oncologist is associated with increased likelihood of BCS and satisfaction with the treatment decision. 51 Surgeons may also integrate their perceptions of patients’ attitudes and concerns into their recommendations. For patients reporting that their feelings about losing a breast are of particular importance, surgeons have been found to be less likely to recommend mastectomy than they would for patients who are more afraid of dying from their cancer. 52
Causes of breast cancer, as perceived by patients
One study suggested that newly diagnosed breast cancer patients at an increased risk of carrying the BRCA1/2 genetic mutation for breast cancer and who opt for bilateral mastectomy, do so because of the potential genetic cause of their cancer. 40
Applying theory to surgical treatment decision making for patients with early stage breast cancer
Social cognition models: theory of planned behaviour
The TPB is a model used to predict a wide range of behaviours, accounting for significant variation in intentions and actions. 23 The TPB has its roots in expectancy‐value models, models that posit that decisions concerning a course of action are informed by both subjective probabilities that a given action will lead to a set of expected outcomes and the evaluation of these action outcomes. 53 The TPB proposes that behaviour is predicted by intention to engage in a behaviour and the extent of perceived control over that behaviour. 22 , 23 Intention, in turn, is predicted by attitudes towards that behaviour (a function of the perceived consequences of the behaviour and a personal evaluation of those consequences), subjective norm (a function of the perceived expectations of others and the motivation to comply with those expectations), and perceived control over the behaviour. 23
One study used the TPB prospectively to examine the decision making process in a cohort of women eligible for either modified radical mastectomy or BCS. 38 Most patients in the sample (71.3%) intended to undergo BCS. As proposed by the TPB, surgery intentions were found to be predicted by subjective norm (the surgeon and their contributions to the choice of surgery), perceived behavioural control (self‐efficacy) and attitudes towards the surgery options (concerns or beliefs about cancer recurrence). Beliefs about the importance of breasts to sexuality were also identified as a predictor of surgery intentions. Beliefs about the possibility of cure and complications of chemotherapy and radiotherapy were also factors that patients perceived would be important in influencing their surgery choice, although they were not found to be associated with surgery intentions. However, no pilot work to identify relevant beliefs 54 was undertaken prior to this study; beliefs were derived from evidence from prior research in which women ranked the factors that they thought would be important when deciding their surgery before making their decision. Nor were these beliefs directly related to the outcome of choosing either BCS or mastectomy.
Although we only found one study applying the TPB to decision making in this context, data from other studies provide support for the view that the constructs included in the TPB play an important role in patients’ decision making (see Fig. 1). Extent of perceived control over decision making is reflected in the degree to which patients are involved in the decision making process, which in turn could determine their treatment choices. 11 , 15 , 36 , 39 Attitudes towards mastectomy and BCS are a function of patients’ beliefs about the consequences of choosing either type of surgery and how that will relate to them, in terms of the clinical benefits and risks, 13 , 30 , 32 , 34 , 36 , 37 , 39 and the impact on their appearance and body image. 8 , 11 , 13 , 14 , 36 , 39 , 40 , 55 The influence of patients’ perceptions of what their physician would recommend and their motivation to comply 7 , 13 , 14 , 18 , 32 , 34 , 37 , 39 , 40 , 41 , 44 , 46 , 47 , 48 , 50 , 52 are reflective of the subjective norm construct in the TPB.
Figure 1.
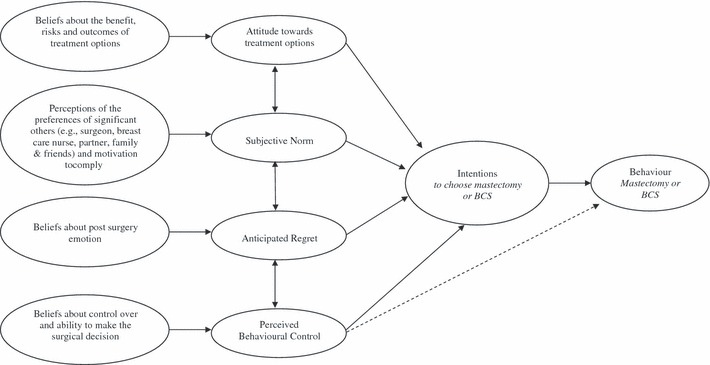
Extended Theory of Planned Behaviour applied to patient deliberation for breast cancer surgery choices (adapted from Ajzen 23 ).
Limitations of the social cognitive approaches Social cognitive approaches have been criticized on the grounds that they sometimes account for limited amounts of statistical variance in predicting health practices. 56 In response to this, the authors of the TPB accept that the predictive power of the model could be improved, but argue that the empirical evidence concerning predictive utility is favourable. 57 A second potential limitation of these approaches is that health behaviours are seen as the result of rational decision making processes based on methodical processing of available information. 25 However, decision making in a medical context tends to occur in a negative affective state, often as a result of receiving an unfavourable diagnosis, 58 and the perception that an important decision needs to be made (i.e. choice of surgery) can also elicit negative emotions. 59 Motivation to cope with such negative emotions could shape decision process patterns and outcomes. 59 Given the potential impact of the breast cancer diagnosis on psychosocial well‐being, decision making in this context may not be as rational as the TPB suggests. Research suggests that affective (emotion‐based) components of the attitude construct may be as important as and possibly more powerful than instrumental (cognitive) components in predicting intention, 60 , 61 , 62 and can be included in an extended version of the TPB.
Extension of the TPB Extended versions of the TPB resulting from the inclusion of additional constructs have been proposed, and these constructs have been found to be key determinants of both attitudes and intentions. 63 , 64 Anticipated regret, for example, is a negative emotion experienced when an individual believes feelings of regret will occur following inaction, or opting for one course of action over another. 63 Distinct from other emotions (e.g. guilt, anger, general affect), 65 anticipated regret may affect decision making and could enhance the TPB’s ability to predict behavioural intentions 63 in relatively ‘high stakes’ situations such as the one confronted by breast cancer patients faced with surgical treatment options. 38 Emotional reactions to a breast cancer diagnosis may be further compounded by the potential loss or altered appearance of a part of the body perceived by many women to be central to feminine identity. 13 Patients who place high importance on their appearance report higher levels of distress before surgery and during the year following surgery than those who attach lower importance to their appearance. 66 Some fear losing a breast more than the life‐threatening repercussions of their diagnosis. 13 Although there is evidence indicating that cancer patients experience post‐decisional regret, further research is needed on the effects of anticipated regret on cancer‐related behaviours and decision making. 67
Illness cognitions: common sense model of illness representations
The CSM 24 emphasizes how cognitive and emotional representations of an illness guide coping and emotional responses to that illness. Thus the CSM has the potential to provide an insight into how patients make sense of their condition and the available treatment options, and has been used to understand the impact of patients’ illness representations on a number of outcomes, 68 including help‐seeking intentions 29 and post‐treatment distress. 69 The CSM identifies the factors involved when patients process information to form a ‘lay perception’ of the illness, which influences coping behaviours and outcomes. This is thought to occur in three stages which continue until the coping strategies adopted are perceived to have been successful and a state of equilibrium is reached:
-
1
Interpretation of the problem, where the patient forms cognitive representations, or a conceptual model, of the illness.
-
2
Action plan/ coping stage, where the patient identifies and develops suitable coping strategies.
-
3
Appraisal stage, where patients evaluate their coping strategies to determine whether to continue with their chosen strategy or develop an alternative.
The emotional state of the individual may change in any of the three stages and additional coping strategies and appraisals may be produced to cope with these responses, both in parallel with, and partially independent of, the cognitive processes.
Cognitive representations of illness are structured around five key areas: cause (perceptions of causal factors); identity (statements patients make about the signs, symptoms and illness label); timeline (beliefs about the duration of the illness, e.g. chronic or acute); cure/ controllability (beliefs concerning the effectiveness of the coping behaviours or the treatment); and consequences (beliefs concerning the impact of the illness on quality of life, or on functional capacity). 24 These components are not independent of each other. For example, the belief that an illness will be long‐term with a number of symptoms tends to be associated with more severe consequences and a more negative perception of the ability to cure/control the illness. 24 Illness representations are influenced by a range of factors such as personal experience of the illness, knowing someone else with experience of the illness, information from friends and relatives, and the media. 24
The CSM may provide a useful framework for understanding how a patient’s representation of their breast cancer influences their surgery choices (see Fig. 2). We did not find any studies applying the CSM to breast cancer surgery decision making, although the results of several studies provide evidence that constructs included in the CSM play a role in women’s treatment decisions. The consequences patients consider when making their decision include chances of survival, cancer recurrence 13 , 30 , 32 , 34 , 36 , 37 , 39 and cosmetic outcome. 11 , 13 , 14 , 30 , 36 , 39 , 55 Other consequences of treatment may be considered by patients when making their decision, such as whether or not they will need radiation treatment (were they to opt for BCS) and the practical implications of this, such as restrictions in travel. 41 The extent to which illness can be controlled or cured is particularly relevant in this clinical context. As noted above, perceptions of cancer recurrence and survival are influential, 30 , 36 with concerns that inaccurate beliefs about superior survival rates for mastectomy lead patients to favour this option. 13 , 32 , 34 , 37 , 39 To our knowledge there is no evidence of the impact of patients’ representations of duration of their breast cancer on their surgery choices. A separate but related issue is the duration of the treatment itself, concerns about which have been found to influence surgery choices. 41 There is a limited degree of evidence that perceptions of the causes of breast cancer influences surgery choices. 40 More recently, research has looked to measure the emotional representation concept of the model, 70 , 71 particularly in the context of screening, where emotions are reported to be associated with the cognitive information processing of the health threat in people with abnormal screening results. 71
Figure 2.
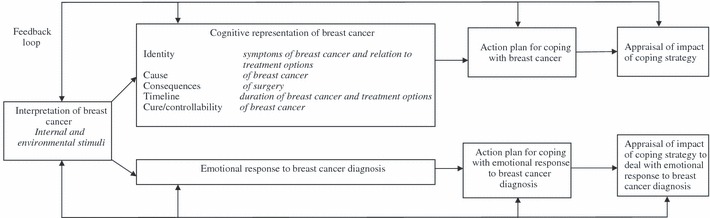
The Common Sense Model of Illness Representations applied to patient deliberation for breast cancer surgery choices (adapted from Hagger & Orbell 62 ).
Synthesis
There is considerable evidence of the factors that shape breast cancer patients’ surgical treatment choices. Factors include beliefs about clinical risks and benefits; the duration of treatment, and of any subsequent treatment; and the impact on appearance and effects on feelings about body image and sexuality. There is extensive evidence of the impact of patients’ perceptions of their surgeons’ preferences, whether or not such preferences are explicit. Although prior research provides evidence concerning a multitude of factors, only 11 studies 8 , 11 , 31 , 33 , 36 , 37 , 38 , 41 , 44 , 49 , 52 examined procedural, disease status and health outcomes simultaneously. Research suggests that it is the combination of these factors that determines patients’ choices.
We are not aware of any studies examining the influence of other clinicians, such as specialist breast nurses, who – in the UK, at least – are recognized as key members of the breast care team, 72 providing patients with information and support when making a decision. 72 , 73 Furthermore, the literature lacks theoretically guided research that considers these various factors in an integrated fashion. Such research would help to provide a more complete understanding of patients’ surgery choices.
Despite the paucity of studies specifically testing the applicability of the TPB and CSM to the study of women’s surgery choices for early breast cancer, it is evident from our review that core elements of these theories do play an important role in decision making. The theories thus provide a useful framework for further analysis, providing different, yet complementary perspectives. The TPB focuses on the impact of attitudes towards the available treatment options and motivation to comply with the perceived preferences of significant others (e.g. surgeon) on the choice of mastectomy or BCS. The CSM provides a framework for understanding how cognitive representations of breast cancer influence the choice of mastectomy or BCS as part of a coping strategy to deal with the threat of breast cancer. Although other models, such as the Conflict Theory of Decision Making 74 and Subjective Utility Theory, 75 have been used, these are older models that have to some extent been superseded by the TPB and CSM and do not offer the same scope for developing a more detailed understanding of the influential factors.
There is evidence that patients form a cognitive representation of their breast cancer using key constructs of the CSM. The perceived timeline of cancer has been found to predict global and disease‐specific forms of distress: patients conceptualising their cancer as chronic (long‐lasting) or cyclic (recurring) were found to be more depressed, anxious and worried than those conceptualising their cancer as acute (short‐term). 69 Patients’ perceptions of the timeline of their breast cancer and the impact of symptoms have also been found to predict psychological morbidity in the year after surgery. 76 Illness representations were more predictive of psychological distress than objective indicators, such as the likelihood of cancer recurrence. 69 Both the TPB and the cognitive component of the CSM have been applied to perceptions of breast cancer symptoms and help‐seeking intentions across the life‐span, 28 and to symptom perceptions and health beliefs as predictors of help‐seeking intentions for breast cancer symptoms. 29 Cognitive representations of the identity and consequences of breast cancer, along with components of the TPB (attitudes towards help‐seeking and perceived behavioural control), partly predicted intention to seek medical help for potential breast cancer symptoms. 29 However, less than one‐third of the variance was accounted for, and of that third, 22% was attributable to the CSM. 29 Missing from these studies was the assessment of the emotional component of the decision making, which might have helped to account for a higher proportion of the variance in help‐seeking intentions. 28 , 29
Designing decision support for patients
A more complete understanding of the factors influencing breast cancer patients’ surgery choices would help in tailoring effective decision support. Interventions such as counselling or formalized ‘decision aids’ 77 , 78 also known as ‘decision support technologies,’ can directly support patients in making ‘good’ decisions at a difficult time, 77 although there is no consensus on what constitutes a good decision when choices depend on the perceived benefits vs. harms. 79 Decision aids are “designed to help people make specific and deliberative choices among options…by providing (at the minimum) information on the options and outcomes relevant to a person’s health status”. 79 These interventions build on the ‘shared decision making’ paradigm which enables patients’ preferences to be incorporated into clinical decisions, particularly where there is more than one option which may impact on their quality of life in different ways. 80 A recent consultation conducted by the UK Department of Health found that citizens wish to be more involved in decisions concerning their care, with appropriate information to support them in making treatment choices. 81 To be able to make an informed choice, i.e. “based on relevant knowledge, consistent with… values and behaviourally implemented”, 82 breast cancer patients need to assimilate a large amount of information in a short space of time. 12 To be sure of meeting their preferences and needs, the information patients receive should be presented in a form that is acceptable to them, understandable and provide a balanced view of the available options. 79
Several decision support interventions have been developed to help early breast cancer patients to make informed choices about surgical treatment, leading to significant improvements in knowledge about treatment options and increases in satisfaction with the decision making process. 83 However, there is a lack of theoretical underpinning to existing decision support interventions in both their design and development. 83 , 84 A more comprehensive and theoretically guided understanding of the factors influencing breast cancer patients’ treatment choices would not only go some way to understanding variation in treatment uptake, but would also help to identify and tailor ways of supporting women in making these choices. The extended TPB and the CSM can be used to inform the design of decision support for patients choosing surgery. More specifically, the theories can guide those areas where balanced, accurate and clear information is vital to avoid decision making based on inaccurate representations, for example beliefs about the likelihood of survival and cancer recurrence.
Figure 3 maps the constructs of the extended TPB and the CSM onto the different elements one would expect to find in a decision support intervention for breast cancer surgical decision making.
Figure 3.
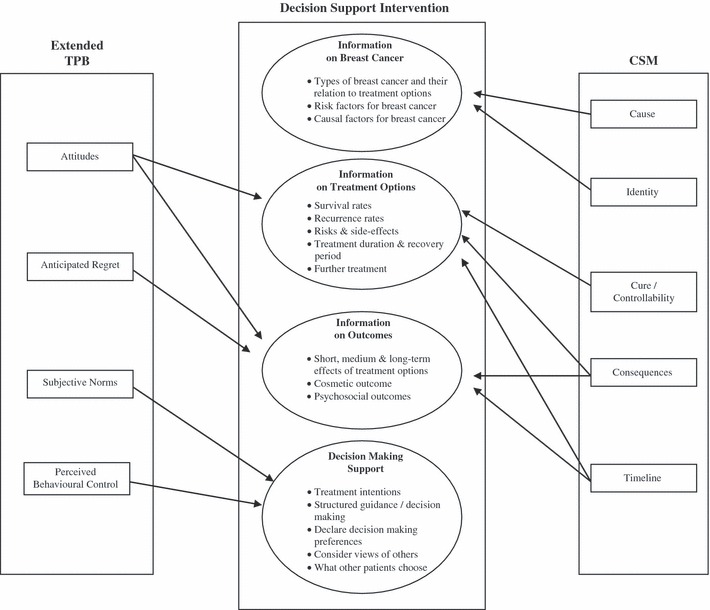
Application of an extended TPB and the CSM to the design of decision support for early stage breast cancer.
Decision support based on the extended TPB Beliefs about the clinical benefits and risks of each surgical option, fears of cancer recurrence, concerns about appearance and psychosocial outcomes, which in turn shape attitudes towards the treatment options, could be addressed in information about the available treatment options and their outcomes. Information about outcomes may also help patients to personalize the information and help them to imagine how they would feel in the future, in particular thinking about any feelings of regret they might experience. Specific support in decision making could also help to address the perceived behavioural control and subjective norm constructs by actively involving the patient in decision making, helping her to consider her own preferences, whether or not she perceives them to be consistent with what others think. Patients may make decisions based on perceptions of their surgeon’s preferences, 85 but the concern is that they might come to regret this later. Some patients may not perceive themselves as having a real choice or control over the decision making process. The availability of an intervention such as a decision aid may help to alter this perception. As noted earlier, some evidence suggests that increased control over the decision making process leads to decisions to undergo mastectomy, whereas less control leads to decisions to undergo BCS. 15 , 36 , 39 However, the evidence is inconsistent, with one study suggesting that increased control leads to decisions to undergo BCS. 35 Furthermore, a meta‐analysis of decision aids for surgery for early breast cancer found women who used them were 25% more likely to choose BCS. 76 This apparent discrepancy highlights the need for more empirical work in this area.
Decision support based on the CSM Patients’ cognitive representations of the causes of breast cancer could be addressed through the provision of information about the genetic and other known risk factors for breast cancer. These beliefs, which are not included in the TPB, could influence which surgery women choose. There is no available evidence concerning the CSM’s construct of illness identity in this clinical context, but providing information about the different types of breast cancer and their relation to the different treatment options would address this, again an area of a decision support intervention the TPB would not inform. Patients’ representations of the timeline of their disease, and in particular the duration of their treatment, could be addressed by providing information about recurrence and survival rates, along with specific details of each treatment option. As with the attitude component of the TPB, patients’ representations of the cure or controllability of their breast cancer and the consequences of the different surgical options could be addressed by providing information about the options and their outcomes. Unlike the TPB, the CSM would not be able to inform the specific decision making support element to the intervention.
Conclusions and future directions
The extended TPB and the CSM provide a useful basis for predicting and understanding the surgery choices of women diagnosed with early breast cancer. While both the extended TPB and CSM provide insight into the beliefs patients hold about the benefits and risks of surgery, the chances of their cancer being cured or recurring and the impact on their body image, they also offer distinct perspectives that need to be considered. Using theory to understand factors influencing women’s choices should inform the design and development of decision support interventions in such a way as to provide clear and accurate information in those areas important to patients. This would be of particular benefit if patients’ misconceptions have the potential to bias them to make a decision they would not make if they had a more complete understanding, and which they might later regret. While there is evidence supporting the utility of applying the extended TPB and CSM in this context, further research is needed to examine the extent to which they account for breast cancer patients’ surgery choices. Research into the distinction between affective and instrumental components of the attitudes construct applied to this clinical context would also help to provide a more detailed account of the complexities of breast cancer patients’ deliberations. Finally, the TPB and CSM are likely to be useful in the design of evaluations of decision support interventions to facilitate patients’ decision making in this context.
Conflicts of interest
There are no conflicts of interest.
Sources of funding
Funds from Cancer Research UK support Stephanie Sivell.
Supporting information
Table S1 Summary of included studies.
Supporting info item
References
- 1. Fisher B, Anderson S, Bryant J et al. Twenty‐year follow‐up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. New England Journal of Medicine, 2002; 347: 1233–1241. [DOI] [PubMed] [Google Scholar]
- 2. Jacobson JA, Danforth DN, Cowan KH et al. Ten‐year results of a comparison of breast conservation with mastectomy in the treatment of stage I and II breast cancer. New England Journal of Medicine, 1995; 332: 907–911. [DOI] [PubMed] [Google Scholar]
- 3. van Dongen JA, Voogd AC, Fentiman IS et al. Long‐term results of a randomized trial comparing breast‐conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 Trial. Journal of the National Cancer Institute, 2000; 92: 1143–1150. [DOI] [PubMed] [Google Scholar]
- 4. Fallowfield L. Offering choice of surgical treatment to women with breast cancer. Patient Education & Counseling, 1997; 30: 209–214. [DOI] [PubMed] [Google Scholar]
- 5. Caldon LJ, Walters SJ, Reed JA, Murphy A, Worley A, Reed MW. Case‐mix fails to explain variation in mastectomy rates: management of screen‐detected breast cancer in a UK region 1997–2003. British Journal of Cancer, 2005; 92: 55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nattinger AB, Gottlieb MS, Veum J, Yahnke D, Goodwin JS. Geographic variation in the use of breast‐conserving treatment for breast cancer. New England Journal of Medicine, 1992; 326: 1102–1107. [DOI] [PubMed] [Google Scholar]
- 7. Balneaves LG, Long B. An embedded decisional model of stress and coping: implications for exploring treatment decision making by women with breast cancer. Journal of Advanced Nursing, 1999; 30: 1321–1331. [DOI] [PubMed] [Google Scholar]
- 8. Stanton AL, Estes MA, Estes NC, Cameron CL, Danoff‐Burg S, Irving LM. Treatment decision making and adjustment to breast cancer: a longitudinal study. Journal of Consulting & Clinical Psychology, 1998; 66: 313–322. [DOI] [PubMed] [Google Scholar]
- 9. Franks HM, Roesch SC. Appraisals and coping in people living with cancer: a meta‐analysis. Psycho-Oncology, 2006; 15: 1027–1037. [DOI] [PubMed] [Google Scholar]
- 10. Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nursing, 1999; 22: 185–194. [DOI] [PubMed] [Google Scholar]
- 11. McVea KLSP, Minier WC, Palensky Johnson JJ. Low‐income women with early‐stage breast cancer: physician and patient decision making styles. Psycho-Oncology, 2001; 10: 137–146. [DOI] [PubMed] [Google Scholar]
- 12. Dixon JM, Mak C. Predictors of mastectomy in a certified breast center – the surgeon is an independent risk factor. Breast Journal, 2008; 14: 321–323. [DOI] [PubMed] [Google Scholar]
- 13. Roberts CS, Cox CE. Medical and psychosocial treatment issues in breast cancer in older women. Journal of Gerontological Social Work, 1997; 28: 63–74. [Google Scholar]
- 14. Molenaar S, Oort F, Sprangers M et al. Predictors of patients’ choices for breast‐conserving therapy or mastectomy: a prospective study. British Journal of Cancer, 2004; 90: 2123–2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lantz P, Janz N, Fagerlin A et al. Satisfaction with surgery outcomes and the decision process in a population‐based sample of women with breast cancer. Health Services Research, 2005; 40: 745–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nattinger AB, Hoffmann RG, Howell‐Pelz A, Goodwin JS. Effect of Nancy Reagan’s mastectomy on choice of surgery for breast cancer by US women. JAMA, 1998; 279: 762–766. [DOI] [PubMed] [Google Scholar]
- 17. Wei JP, Sherry RM, Baisden BL, Peckel J, Lala G. Prospective hospital‐based survey of attitudes of Southern women toward surgical treatment of breast cancer. Annals of Surgical Oncology, 1995; 2: 360–364. [DOI] [PubMed] [Google Scholar]
- 18. Halkett GKB, Arbon P, Scutter SD, Borg M. The experience of making treatment decisions for women with early stage breast cancer. European Journal of Cancer Care, 2005; 14: 249–255. [DOI] [PubMed] [Google Scholar]
- 19. McKinlay J, Burns R, Durante R et al. Patient, physician and presentational influences on clinical decision making for breast cancer: results from a factorial experiment. Journal of Evaluation in Clinical Practice, 1997; 3: 23–57. [DOI] [PubMed] [Google Scholar]
- 20. Hughes K. Decision making by patients with breast cancer: the role of information in treatment selection. Oncology Nursing Forum, 1993; 20: 623–628. [PubMed] [Google Scholar]
- 21. Smitt MC, Heltzel M. Women’s use of resources in decision making for early‐stage breast cancer: results of a community‐based survey. Annals of Surgical Oncology, 1997; 4: 564–569. [DOI] [PubMed] [Google Scholar]
- 22. Ajzen I. From intention to actions: a theory of planned behaviour In: Kuhl J, Beckmann J. (eds) Action‐control: From Cognition to Behavior. Heidelberg: Spring, 1985: 11–39. [Google Scholar]
- 23. Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes, 1991; 50: 179–211. [Google Scholar]
- 24. Leventhal H, Meyer D, Nerenz D. The common‐sense representation of illness danger In: Rachman S. (ed.) Medical Psychology. Vol 2. New York: Pergamon Press, 1980: 7–30. [Google Scholar]
- 25. Conner M, Norman P. Predicting health behaviour: a social cognition approach In: Conner M, Norman P. (eds) Predicting Health Behaviour: Research Practice with Social Cognition Models. 2nd edn Maidenhead: Open University Press, 2005: 1–27. [Google Scholar]
- 26. Hevey D, Pertl M, Thomas K et al. The relationship between prostate cancer knowledge and beliefs and intentions to attend PSA screening among at‐risk men. Patient Education and Counseling, 2009; 74: 244–249. [DOI] [PubMed] [Google Scholar]
- 27. Orbell S, Hagger M, Brown V, Tidy J. Comparing two theories of health behaviours: a prospective study of noncompletion of treatment following cervical cancer screening. Health Psychology, 2006; 25: 604–615. [DOI] [PubMed] [Google Scholar]
- 28. Grunfeld EA, Hunter MS, Ramirez AJ, Richards MA. Perceptions of breast cancer across the lifespan. Journal of Psychosomatic Research, 2003; 54: 141–146. [DOI] [PubMed] [Google Scholar]
- 29. Hunter S, Grunfeld EA, Ramirez AJ. Help seeking intentions for breast‐cancer symptoms: a comparison of the self‐regulation model and the theory of planned behaviour. British Journal of Health Psychology, 2003; 8: 319–333. [DOI] [PubMed] [Google Scholar]
- 30. Adachi K, Ueno T, Fujioka T, Fujitomi Y, Ueo H. Psychosocial factors affecting the therapeutic decision making and postoperative mood states in Japanese breast cancer patients who underwent various types of surgery: body image and sexuality. Japanese Journal of Clinical Oncology, 2007; 37: 412–418. [DOI] [PubMed] [Google Scholar]
- 31. Katz SJ, Lantz PM, Zemencuk JK. Correlates of surgical treatment type for women with noninvasive and invasive breast cancer. Journal of Women’s Health & Gender-Based Medicine, 2001; 10: 659–670. [DOI] [PubMed] [Google Scholar]
- 32. Kotwall CA, Maxwell JG, Covington DL, Churchill P, Smith SE, Covan EK. Clinicopathologic factors and patient perceptions associated with surgical breast‐conserving treatment. Annals of Surgical Oncology, 1996; 3: 169–175. [DOI] [PubMed] [Google Scholar]
- 33. Kraus PL. Body image, decision making, and breast cancer treatment. Cancer Nursing, 1999; 22: 421–427. [DOI] [PubMed] [Google Scholar]
- 34. Lam WW, Fielding R, Ho EY, Chan M, Or A. Surgeon’s recommendation, perceived operative efficacy and age dictate treatment choice by Chinese women facing breast cancer surgery. Psycho-Oncology, 2005; 14: 585–593. [DOI] [PubMed] [Google Scholar]
- 35. Mastaglia B, Kristjanson LJ. Factors influencing women’s decisions for choice of surgery for Stage I and Stage II breast cancer in Western Australia. Journal of Advanced Nursing, 2001; 35: 836–847. [DOI] [PubMed] [Google Scholar]
- 36. Osborn GD, Hodin M, Drew PJ, Fielder H, Vaughan‐Williams E, Sweetland HM. Patient demographics and treatment for early breast cancer: an observational study. Breast, 2006; 15: 377–381. [DOI] [PubMed] [Google Scholar]
- 37. Reaby LL. The quality and coping patterns of women’s decision making regarding breast cancer surgery. Psycho-Oncology, 1998; 7: 252–262. [DOI] [PubMed] [Google Scholar]
- 38. Temple WJ, Russell ML, Parsons LL et al. Conservation surgery for breast cancer as the preferred choice: a prospective analysis. Journal of Clinical Oncology, 2006; 24: 3367–3373. [DOI] [PubMed] [Google Scholar]
- 39. Katz SJ, Lantz PM, Janz NK et al. Patient involvement in surgery treatment decisions for breast cancer. Journal of Clinical Oncology, 2005; 23: 5526–5533. [DOI] [PubMed] [Google Scholar]
- 40. Schwartz MD, Lerman C, Brogan B et al. Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. Journal of Clinical Oncology, 2004; 22: 1823–1829. [DOI] [PubMed] [Google Scholar]
- 41. Stafford D, Szczys R, Becker R, Anderson J, Bushfield S. How breast cancer treatment decisions are made by women in North Dakota. American Journal of Surgery, 1998; 176: 515–519. [DOI] [PubMed] [Google Scholar]
- 42. Liang W, Burnett CB, Rowland JH et al. Communication between physicians and older women with localized breast cancer: implications for treatment and patient satisfaction. Journal of Clinical Oncology, 2002; 20: 1008–1016. [DOI] [PubMed] [Google Scholar]
- 43. Maly RC, Leake B, Silliman RA. Breast cancer treatment in older women: impact of the patient‐physician interaction. Journal of the American Geriatrics Society, 2004; 52: 1138–1145. [DOI] [PubMed] [Google Scholar]
- 44. Lam W, Fielding R, Chan M, Chow L, Ho E. Participation and satisfaction with surgical treatment decision making in breast cancer among Chinese women. Breast Cancer Research & Treatment, 2003; 80: 171–180. [DOI] [PubMed] [Google Scholar]
- 45. Vogel DA, Helmes AW, Hasenburg A. Concordance between patients’ desired and actual decision making roles in breast cancer care. Psycho-Oncology, 2008; 17: 182–189. [DOI] [PubMed] [Google Scholar]
- 46. Hokanson P, Seshadri R, Miller KD. Underutilization of breast‐conserving therapy in a predominantly rural population: need for improved surgeon and public education. Clinical Breast Cancer, 2000; 1: 72–76. [DOI] [PubMed] [Google Scholar]
- 47. Johnson JD, Roberts CS, Cox CE, Reintgen DS, Levine JS, Parsons M. Breast cancer patients’ personality style, age, and treatment decision making. Journal of Surgical Oncology, 1996; 63: 183–186. [DOI] [PubMed] [Google Scholar]
- 48. Sandison AJ, Gold DM, Wright P, Jones PA. Breast conservation or mastectomy: treatment choice of women aged 70 years and older. British Journal of Surgery, 1996; 83: 994–996. [DOI] [PubMed] [Google Scholar]
- 49. Nold RJ, Beamer RL, Helmer SD, McBoyle MF. Factors influencing a woman’s choice to undergo breast‐conserving surgery versus modified radical mastectomy. American Journal of Surgery, 2000; 180: 413–418. [DOI] [PubMed] [Google Scholar]
- 50. Keating NL, Weeks JC, Borbas C, Guadagnoli E. Treatment of early stage breast cancer: do surgeons and patients agree regarding whether treatment alternatives were discussed? Breast Cancer Research & Treatment, 2003; 79: 225–231. [DOI] [PubMed] [Google Scholar]
- 51. Keating NL, Weeks JC, Landrum MB, Borbas C, Guadagnoli E. Discussion of treatment options for early‐stage breast cancer: effect of provider specialty on type of surgery and satisfaction. Medical Care, 2001; 39: 681–691. [DOI] [PubMed] [Google Scholar]
- 52. Wu ZH, Freeman JL, Greer AL, Freeman DH, Goodman JS. The influence of patients’ concerns on surgeons’ recommendations for early breast cancer. European Journal of Cancer Care, 2001; 10: 100–106. [DOI] [PubMed] [Google Scholar]
- 53. Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Reading, MA: Addison‐Wesley, 1975. [Google Scholar]
- 54. Ajzen I. Perceived behavioral control, self‐efficacy, locus of control, and the Theory of Planned Behavior. Journal of Applied Social Psychology, 2002; 32: 1–20. [Google Scholar]
- 55. Keith DJ, Walker MB, Walker LG et al. Women who wish breast reconstruction: characteristics, fears, and hopes. Plastic & Reconstructive Surgery, 2003; 111: 1051–1056. [DOI] [PubMed] [Google Scholar]
- 56. Ogden J. Some problems with social cognition models: a pragmatic and conceptual analysis. Health Psychology, 2003; 22: 424–428. [DOI] [PubMed] [Google Scholar]
- 57. Ajzen I, Fishbein M. Questions raised by a reasoned action approach: comment on Ogden (2003). Health Psychology, 2003; 23: 431–434. [DOI] [PubMed] [Google Scholar]
- 58. Lowenstein G. Hot‐cold empathy gaps and medical decision making. Health Psychology, 2005; 24 (Suppl. 4): S49–S56. [DOI] [PubMed] [Google Scholar]
- 59. Luce MF. Decision making as coping. Health Psychology, 2005; 24 (Suppl. 4): S23–S28. [DOI] [PubMed] [Google Scholar]
- 60. Trafimow D, Sheeran P. Some tests of the distinction between cognitive and affective beliefs. Journal of Experimental and Social Psychology, 1998; 34: 378–397. [Google Scholar]
- 61. Hagger MS, Chatzisarantis NLD. First‐ and higher‐order models of attitudes, normative influence, and perceived behavioural control in the theory of planned behaviour. British Journal of Social Psychology, 2005; 44: 513–535. [DOI] [PubMed] [Google Scholar]
- 62. Lowe R, Eves F, Carroll D. The influence of affective and instrumental beliefs on exercise intentions and behavior: a longitudinal analysis. Journal of Applied Social Psychology, 2002; 32: 1241–1252. [Google Scholar]
- 63. Abraham C, Sheeran P. Acting on intentions: the role of anticipated regret. British Journal of Social Psychology, 2003; 42: 495–511. [DOI] [PubMed] [Google Scholar]
- 64. Triandis HC. Interpersonal Behavior. CA: Brookes‐Cole, 1977. [Google Scholar]
- 65. Zeelenberg M, Pieters R. A theory of regret regulation 1.0. Journal of Consumer Psychology, 2007; 17: 3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Carver CS, Pozo‐Kaderman C, Price AA et al. Concern about aspects of body image and adjustment to early stage breast cancer. Psychosomatic Medicine, 1998; 60: 168–174. [DOI] [PubMed] [Google Scholar]
- 67. Connolly T, Reb J. Regret in cancer‐related decisions. Health Psychology, 2005; 24 (Suppl. 4): S29–S34. [DOI] [PubMed] [Google Scholar]
- 68. Hagger M, Orbell S. A meta‐analytic review of the common‐sense model of illness representations. Psychology and Health, 2003; 18: 141–184. [Google Scholar]
- 69. Rabin C, Leventhal H, Goodin S. Conceptualization of disease timeline predicts post treatment distress in breast cancer patients. Health Psychology, 2004; 23: 407–412. [DOI] [PubMed] [Google Scholar]
- 70. Moss‐Morris R, Weinman J, Petrie KJ et al. The revised illness perception questionnaire (IPQ‐R). Psychology and Health, 2002; 17: 1–16. [Google Scholar]
- 71. Hagger MS, Orbell S. Illness representations and emotion in people with abnormal screening results. Psychology and Health, 2006; 21: 183–209. [DOI] [PubMed] [Google Scholar]
- 72. Ambler N, Rumsey N, Harcourt D, Khan F, Cawthorn S, Barker J. Specialist nurse counsellor interventions at the time of diagnosis of breast cancer: comparing ‘advocacy’ with a conventional approach. Journal of Advanced Nursing, 1999; 29: 445–453. [DOI] [PubMed] [Google Scholar]
- 73. Monson MA, Harwood KV. Helping women select primary breast cancer treatment. American Journal of Nursing, 1998; Apr; Suppl.: 3–7. [PubMed] [Google Scholar]
- 74. Janis IL, Mann L. Decision‐Making: A Psychological Analysis of Conflict, Choice and Commitment. New York: Free Press, 1977. [Google Scholar]
- 75. Edwards W. The theory of decision making. Psychological Bulletin, 1954; 51: 380–417. [DOI] [PubMed] [Google Scholar]
- 76. Millar K, Purushotham AD, McLatchie E, George WD, Murray GD. A 1‐year prospective study of individual variation in distress, and illness perceptions, after treatment for breast cancer. Journal of Psychosomatic Research, 2005; 58: 335–342. [DOI] [PubMed] [Google Scholar]
- 77. Barnato AE, Llewellyn‐Thomas HA, Peters EM et al. Communication and decision making in cancer care: setting up research priorities for decision support/patients’ decision aids. Medical Decision Making, 2007; 27: 626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Elwyn G, O’Connor A, Stacey D et al. Developing a quality criteria framework for patient decision aids: online international Delphi process. BMJ, 2006; 333: 417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. O’Connor AM, Stacey D, Entwistle V et al. Decision aids for people facing health treatment or screening decisions (review). Cochrane Database of Systematic Reviews, 2003; 2: CD001431. [DOI] [PubMed] [Google Scholar]
- 80. Coulter A, Entwistle V, Gilbert D. Sharing decisions with patients: is the information good enough? BMJ, 1999; 318: 318–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Lawrence Z. Building on the best – choice, responsiveness and equity in the NHS. Health Expectations, 2004; 7: 176–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. O’Connor A, O’Brien‐Pallas LL. Decisional conflict In: McFarlane GK, McFarlane EA. (eds). Nursing Diagnosis and Intervention, Toronto: Mosby, 1989: 486–496. [Google Scholar]
- 83. Waljee JF, Rogers MA, Alderman AK. Decision aids and breast cancer: do they influence choice for surgery and knowledge of treatment options? Journal of Clinical Oncology, 2007; 25: 1067–1073. [DOI] [PubMed] [Google Scholar]
- 84. Durand M‐A, Stiel M, Boivin J, Elwyn G. Where is the theory? Evaluating the theoretical frameworks described in decision support technologies Patient Education & Counseling, 2008; 71: 125–135. [DOI] [PubMed] [Google Scholar]
- 85. Masood S. Why most women with breast cancer still undergo mastectomy. Breast Journal, 2003; 9: 69–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Summary of included studies.
Supporting info item


